Abstract
Rationale: Clinical and research training opportunities in global health are of increasing interest to medical trainees, but little is known about such opportunities in U.S.-based pulmonary and pulmonary/critical care medicine (PCCM) fellowship programs.
Objectives: Summarize currently available global health–related training opportunities and identify potential barriers to implementing global health curricula among U.S.-based PCCM fellowship programs.
Methods: We sent a confidential, online, targeted needs assessment to PCCM fellowship program directors and associate program directors. Data collected included program demographics, currently available global health–related clinical and research training opportunities, potential barriers to the implementation of global health–related programmatic content, and perceived interest in global health–related training opportunities by current and/or prospective trainees. To evaluate for nonresponse bias, we performed an online search to identify global health–related training opportunities offered by nonresponding programs.
Results: Out of 171 surveyed programs, 63 PCCM fellowship programs (37%) provided survey responses. Most responses (n = 56, 89%) were from combined PCCM training programs; 66% (n = 40) of programs offered at least one component of global health–related clinical or research training. Overall, 27% (n = 17) had a Ruth L. Kirschstein National Research Service Award Institutional Research Training Grant (National Institutes of Health T32), 73% (n = 46) had fewer than 35 faculty members, and 51% (n = 32) had at least one faculty member conducting global health–focused research. Most responding programs (66%, n = 40) offered at least one global health–related educational component. Among programs that would like to offer global health–related training components, the most common barriers included competing priorities for lecture content and a lack of in-division mentors with global health experience, a champion for global health–related activities, and established partnerships outside the United States.
Conclusions: PCCM program leaders are interested in offering global health–related training opportunities, but important barriers include lack of mentorship, dedicated fellowship time, and established global partnerships. Future research is needed to better understand global health–related interests and training needs of incoming fellows and to design creative solutions for providing global health–related training across academic institutions with variable global health–related training capacities.
Keywords: medical education, curriculum, needs assessment, global health
Global health–related training opportunities are of increasing interest to medical trainees (1–10). Although inconsistently defined, global health has been described as “an area for study, research, and practice that places a priority on improving health and achieving health equity for all people worldwide” (11), and this definition has driven various models of global health training across the spectrum of undergraduate and graduate medical education.
With increasing globalization, and as mass migration is occurring on an unprecedented scale (12), future leaders in pulmonary and pulmonary/critical care medicine (PCCM) require broad training and practical, hands-on experience that incorporates an in-depth understanding of health and disease around the world. Respiratory-related conditions including chronic obstructive pulmonary disease, pneumonia, lung cancer, and tuberculosis (TB) are among the top 10 causes of death globally (13–15), and most respiratory-related mortality occurs in low- and middle-income countries (16). Likewise, of the 15 million people worldwide who die annually as a result of severe illness or serious infection, the vast majority live in low- and middle-income countries (17, 18). Several recent infectious disease epidemics, including severe acute respiratory distress syndrome (2002), H1N1 influenza (2009), Middle East respiratory syndrome–related coronavirus (2012), and Ebola (2014), have demonstrated how in a progressively interconnected world, diseases can quickly cross geographic borders with profound social, political, and economic consequences. Expertise from pulmonologists and intensivists in clinical management, education, and research has been instrumental in mitigating the impact of these diseases among vulnerable populations (19–23). Consequently, these specialists are uniquely positioned to lead efforts in global health training.
Global health training can provide tangible benefits that include and extend beyond the commonly cited ability to care for patients in underresourced areas. Although global health is commonly conceptualized as occurring in international locations, the medical conditions and structural challenges experienced by the world’s poor often transcend international boundaries because of similarities in lack of access to reliable health care and diseases of poverty experienced in many U.S. rural locations (24, 25). Simultaneously, trainees exhibit a more cost-conscious approach to medical care and a greater focus on technology-independent diagnoses and gain experience managing diseases that may be more advanced at presentation or are less common in high-income countries, such as TB or severe acute respiratory distress syndrome (26, 27). Furthermore, these trainees increase public awareness of such health conditions and exhibit greater cross-cultural competence as medical practitioners (28). Despite the merits of global health training and growing interest among trainees (1–11, 29–33), little is known about the current global health–related clinical and research training opportunities among PCCM programs. To address this critical knowledge gap, we conducted a targeted needs assessment of U.S.-based PCCM fellowship programs to summarize current global health–related educational opportunities and identify potential barriers to implementing global health–related educational curricula in PCCM fellowship training.
Methods
We conducted a targeted needs assessment via an online survey of program directors (PDs) and associate program directors (APDs) at U.S.-based Accreditation Council for Graduate Medical Education (ACGME)-accredited adult PCCM fellowship programs from August through December 2017. We used purposive sampling to identify PDs and APDs in collaboration with the Association for Pulmonary and Critical Care Medicine Program Directors. PDs and APDs were eligible for participation in the survey if they were employed in an ACGME-accredited fellowship program and their contact information was available through the Association for Pulmonary and Critical Care Medicine Program Directors; they were contacted by e-mail up to four times to invite them to complete the survey. The e-mail invitation included a brief introduction to the purpose of the survey, offer of entry into a drawing for one of two $250 Amazon gift cards on survey completion, and information regarding confidentiality, privacy, and informed consent. Interested participants accessed the online survey through a hyperlink provided in the email. We collected respondent names and e-mail addresses to prevent duplicate program representation but did not link survey responses with individual names or programs. Survey methods were deemed exempt from review by the Partners Healthcare Institutional Review Board, and all survey respondents provided informed consent.
Online Survey
We designed the survey to assess current and ideal components of global health–focused training as well as barriers to and perceptions of the need for such training opportunities in PCCM fellowship programs. Survey components were developed by the study authors and refined through multiple rounds of review and discussion. Once consensus was achieved among study authors, the survey was pretested with select PCCM faculty from different institutions to assess content validity, clarity of concepts, minimization of bias, completeness of response options, and applicability to research goals. After further revision, the survey was then pilot tested to assess for logistical and psychometric performance. Finally, we administered the survey (online supplement) to PDs and APDs using Qualtrics online survey software.
We defined global health–related educational components as any of the following: didactic sessions on global health–related research or clinical care/teaching; global health–related local clinical experiences such as TB, public health, or refugee clinics; clinical experiences based in another country; research in a global health setting; global health–related coursework; or a dedicated track or pathway within the PCCM fellowship. We also examined barriers among programs that would like to but do not currently offer global health–related education curricula and fellowship leaders’ perceptions of trainees’ interests and career plans related to global health. Covariates were selected a priori and included faculty size; presence of faculty involved in global health research, clinical work, or educational activities within the division; and the presence of a National Institutes of Health (NIH) Ruth L. Kirschstein National Research Service Award Institutional Research Training Grant (NIH T32).
To evaluate for nonresponse bias, we identified programs that did not provide survey responses on the basis of the list of PCCM fellowship programs published on the Electronic Residency Application Service website. For nonresponding programs, we examined fellowship program websites to identify global health–related training opportunities by searching for any mention of the phrase “global health” or faculty members who participate in international work. We also searched websites of corresponding hospital- or university-based global health centers for presence of pulmonary or critical care–focused projects or PCCM faculty in a leadership role. We explored whether affiliated Schools of Public Health (SPH) offered global health–related coursework or degree-granting opportunities by querying the Association of Schools and Programs of Public Health SPH list for “global health” (34). Finally, we queried the NIH Research Portfolio Online Reporting Tools website to identify programs funded by an NIH T32.
Statistical Analysis
We summarized program demographics using descriptive statistics. If we received more than one survey response from a program, we included only the PD’s response in our analysis. In instances in which an individual submitted more than one response, we included the first response if responses were concordant overall and excluded that individual’s responses if the first and second response were discordant. Among responding programs, we compared characteristics of programs with global health–related training opportunities to those without global health–related training opportunities using chi-square or Fisher exact testing, as appropriate. We also compared the proportion of programs offering global health–related training opportunities and the presence of NIH T32 support between nonresponding and responding programs using chi-square tests. Analyses were conducted using Stata 13 (StataCorp).
Results
Program Demographics
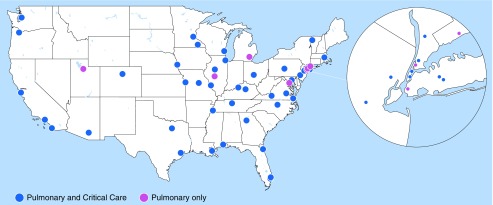
Of a total of 171 surveyed programs, we received 71 survey responses from 68 individuals, representing 63 unique PCCM fellowship programs and 37% of the programs surveyed (Table 1, Figure 1). PDs completed the survey for 53 (84%) of the responding programs, and 56 responses (89%) were from combined pulmonary/critical care training programs. Most divisions (n = 46, 73%) had fewer than 35 faculty members (M.D. and/or Ph.D.), and 32 programs (51%) reported that at least one faculty member was involved in global health–related research. A minority of responding programs (n = 17, 27%) were supported by an NIH T32. Of the 63 unique survey responses, two were from individuals who submitted a discordant set of responses and were excluded from subsequent analyses.
Table 1.
Demographic characteristics of responding programs
| Characteristic | n (%) |
|---|---|
| Program director provided response | 53 (84) |
| Type of training program | |
| Pulmonary and critical care | 56 (89) |
| Pulmonary only | 7 (11) |
| NIH T32 institutional training grant | 17 (27) |
| Approximate number of division faculty (M.D. and/or Ph.D.) | |
| <35 | 46 (73) |
| 35–60 | 9 (14) |
| >60 | 8 (13) |
| Approximate number of division faculty members who conduct research focused on global health | |
| None | 31 (49) |
| 1–3 | 24 (38) |
| >3 | 8 (13) |
Definition of abbreviation: NIH = National Institutes of Health.
n = 63 out of a total of 171 programs.
Figure 1.
National map of responding pulmonary or pulmonary and critical care fellowship programs.
Global Health–related Training Opportunities
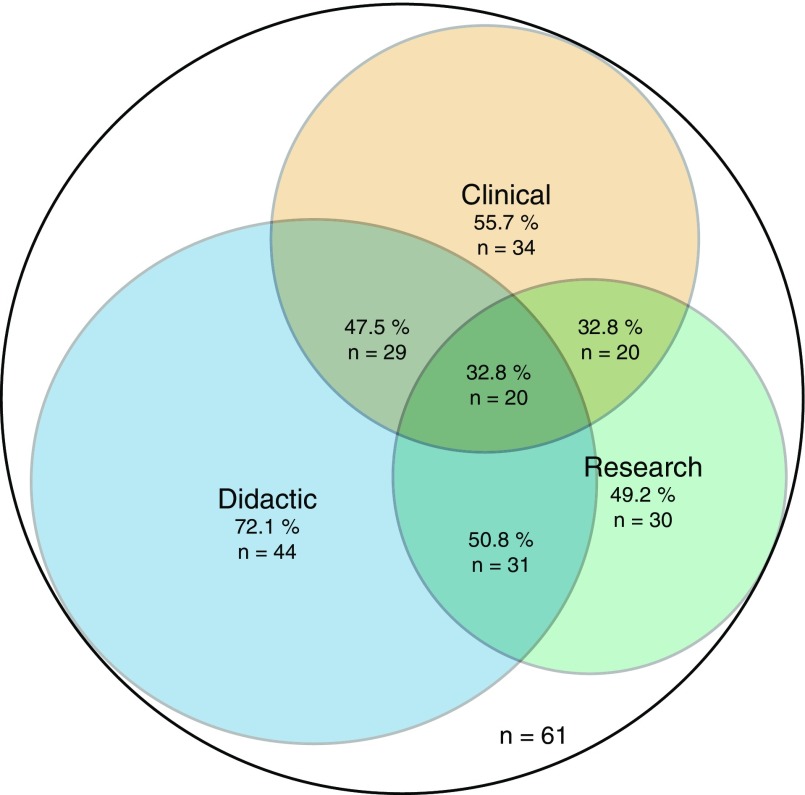
Of the 61 responding programs analyzed further, 66% (n = 40) offered at least one global health–related educational component. The most common components offered were global health–related local clinical experiences (e.g., TB, public health, or refugee clinics) (n = 23, 38%) and global clinical experiences (e.g., patient care–based rotation at clinic or hospital in another country) (n = 18, 30%) (Figure 2; see Table E1 in the online supplement). Only four programs (7%) offered a dedicated global health track or pathway. Although not included in the definition of a global health–related educational component, 30 programs (49%) offered one lecture per year on a global health–related research, clinical, or educational topic, and 24 programs (40%) offered enrollment in a degree-granting program at an SPH. By comparison, among the 108 nonresponding PCCM programs, 24 programs (22%) had websites that indicated global health–related training opportunities (P < 0.001) and 24 (22%) had an NIH T32 (P = 0.48).
Figure 2.
Venn diagram for currently offered global health training opportunities at responding programs. The currently offered training opportunities are grouped into clinical, didactic, and research-focused content areas, and the number of programs that offer aspects of a given content area is reflected by the size of the corresponding circle. Areas where the circles overlap indicate programs that indicated that they offer aspects of several content areas.
Responding programs with an NIH T32 were more likely to offer global health–related coursework at an SPH than those without an NIH T32 (75% vs. 13%, P < 0.001) (Table E2). Compared with programs with fewer faculty (<35 faculty members), those with more faculty (>60 faculty members) were more likely to offer research in a global setting (74% vs. 16%, P = 0.002), as well as global health–related coursework at an SPH (100% vs. 14%, P < 0.001) (Table E3). Programs with at least one faculty member involved in global health–related research were more likely to offer one lecture per year on a global health–related topic (77% vs. 20%, P < 0.001), a series of sessions on global health–related research (32% vs. 3%, P = 0.006), research in a global setting (42% vs. 7%, P = 0.002), or global health–related coursework at an SPH (45% vs. 13%, P = 0.01) (Table E4).
Most common among the educational components that were not currently offered, but desired by program leaders, were a lecture series on global health–related clinical or teaching experience (n = 33, 54%) or research (n = 32, 52%) and local global health–related clinical experiences such as TB, public health, or refugee clinics (n = 31, 51%). The only educational component that the majority of respondents (56%, n = 34) expressed no interest in offering was a dedicated global health track/pathway within fellowship training.
Barriers to Offering Global Health–related Training Opportunities
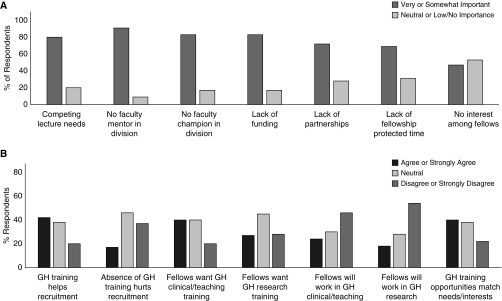
Fifty-five responding programs that would like to offer but do not currently offer certain global health training components provided information on perceived barriers (Figure 3A). Barriers that were considered somewhat or very important by a majority of respondents included competing priorities for lecture content (n = 42, 79%) and the absence of: mentors with global health experience within the division (n = 49, 91%); a faculty champion for global health–related training opportunities within the division (n = 46, 84%); dedicated institutional funding to support global health–related opportunities (n = 46, 84%); established partnerships outside of the United States where fellows can participate in clinical, research, or teaching opportunities (n = 39, 71%); and protected time for fellows to pursue global health–related training opportunities (n = 38, 69%). Although 95% (n = 39) of programs without an NIH T32 cited lack of funding as a very or somewhat important barrier, 50% (n = 7) of programs with an NIH T32 also believed that lack of dedicated funding was a barrier to offering global health–related training opportunities (P = 0.001).
Figure 3.
(A) Barriers to implementation of global health opportunities (n = 55). (B) Program leadership impressions of current and prospective fellows’ opinions about global health–related training opportunities (n = 60). GH = global health.
Program Leadership Impressions of Fellows’ Interest in Global Health–related Training
Most responding programs (n = 60, 95%) provided impressions of current and prospective fellows’ opinions about global health as it pertains to their selection of training programs and/or future career plans (Figure 3B). Many program leaders (n = 25, 42%) believed that the presence of global health–related training opportunities positively impacted their ability to recruit fellowship applicants, although a similar proportion (n = 23, 38%) believed that this neither helped nor hindered recruitment. Overall, 40% of respondents (n = 24) believed that currently offered global health–related training opportunities matched the needs and interests of their fellows. Although 40% of programs (n = 24) believed that their current fellows were interested in engaging in global health–related clinical or teaching opportunities during fellowship, a similar proportion took a neutral stance on whether global health–related opportunities matched the needs/interests of their trainees (n = 23, 38%). Approximately half of program leadership was under the impression that their current fellows did not plan to incorporate global health–related clinical work/teaching (n = 28, 46%) or research (n = 32, 54%) into future careers.
Program leaders of fellowships with at least one faculty member involved in global health–related research were more likely to report that lack of global health–related training opportunities negatively impacted recruitment (31% vs. 3%, P = 0.006), that their current fellows planned to engage in global health–related research during fellowship (43% vs. 10%, P = 0.007), and that current fellows planned to incorporate global health–related clinical work/teaching (37% vs. 10%, P = 0.03) or research (33% vs. 3%, P = 0.006) in their future careers. However, whether program leaders believed that global health–related training opportunities positively impacted recruitment abilities did not differ by presence of at least one faculty member working in global health (53% vs. 30%, P = 0.07) (Table E5).
Discussion
This survey—the first to characterize available global health–related training opportunities in U.S.-based PCCM fellowship programs—highlights important challenges that have limited the expansion of PCCM global health–related training, provides a framework around which a standardized training curriculum and metrics of success can be developed, and characterizes several existing gaps that require formal evaluation before consideration of widespread implementation of global health–related training opportunities nationally. The majority of responding programs offered at least one component of global health–related training opportunities, most commonly global health–related local clinical experiences (e.g., TB, public health, or refugee clinics). The major barriers to offering global health–related training opportunities identified by program leaders were absence of faculty mentors, lack of dedicated institutional funding, lack of partnerships outside of the United States, insufficient protected time for fellows, and competing priorities for lecture content. Although program leaders reported perceived interest in global health–related training among their current fellows, most were under the impression that their fellows would not pursue careers inclusive of global health. Program leadership conveyed limited interest in creating dedicated global health tracks within PCCM fellowship training, but a majority did express interest in exposing fellows to lecture series on global health–related clinical, teaching, or research topics and local global health–related clinical experiences.
Academic institutions that have incorporated global health–related training into their PCCM fellowship curricula have done so through a variety of methods. Although the confidential nature of our survey precludes describing the specific models implemented by responding programs, we have previously summarized the global health–related training models implemented by several PCCM fellowships, which include: global health electives at established domestic or international sites, additional research years contingent on securing mentorship and independent funding, and integrated global health tracks that aim to teach core competencies over the course of fellowship in a curriculum-based manner with domestic and international components (1). Each of these approaches requires varying degrees of human and financial resources that may be prohibitive to some institutions. Programs that provide global health–related training opportunities outside of a dedicated track or pathway are the most common, which is reflective of the ways in which other subspecialty expertise is generally offered to interested trainees. For instance, most programs do not have formalized educational tracks or pathways in pulmonary vascular disease or lung transplant, yet specialized training is possible for interested trainees through a combination of didactic, clinical, and research experiences.
Program leadership expressed interest in providing global health–related training opportunities but not specifically in offering dedicated tracks or pathways within fellowship training. In line with these findings, expansion of global health–related training opportunities to all PCCM fellowship programs through the creation of dedicated tracks or pathways would be an unrealistic use of finite resources. One possible solution to this resource scarcity is to reconsider the structure of global health–related training by creatively leveraging the expertise of centers with existing resources and mentorship across the country. For example, faculty mentors and available clinical and/or research collaborative sites might be organized as a unified network across academic institutions rather than isolated academic silos, any one of which could include a combination of tenets of global health training, akin to what has been accomplished by the NIH Fogarty International Center (35). Accordingly, global health expertise could be regionalized into academic centers of excellence. This approach could feasibly provide interested fellows with access to a broad network of clinical and research curricula and mentorship to support pursuit of their career goals while completing clinical requirements at their home institutions. This approach would also mitigate the anticipated strain of global health training on interested smaller programs, many of which lack funding and/or faculty to support these activities. Resulting academic products, whether clinical or research-focused, would arguably advance the goals of both the fellowship program, through providing the fellow with the training necessary to achieve specified career goals, as well as the center of excellence, through advancing the goals of center-driven global health–focused clinical and/or research initiatives.
A standardized approach to global health training within PCCM fellowship may have additional long-term benefits beyond skills acquisition. A review of online job postings from 48 global health employers found that most postings relevant to physicians required either substantial experience in global health activities that extended beyond clinical practice, masters- or doctoral-level training, or foreign language skills (36). Global health employers identified “understanding public health in an international development context and characteristics like flexibility, creativity, and cultural sensitivity” as highly desired but often lacking among individuals without practical global health experience (37). Furthermore, recent graduates of a global health–focused residency program believed that their training had prepared them to overcome typical barriers to pursing global health–related careers, such as lower salaries, lack of mentorship, and opaque career trajectories (38). Graduates of training programs with carefully considered global health training content would potentially be more prepared to enter the global health work force and to successfully navigate these career challenges.
Importantly, there remains a gap in defining what constitutes necessary global health training in graduate and post-graduate medical programs, including which content areas to define as core competencies. Increasing global health clinical and research activities among PCCM faculty in the last decade has established a rich resource of expertise and leadership. These experts can guide consensus statements on global health–related education (16, 39, 40) that standardize global health–related training among U.S.-based PCCM fellowship programs through a structured approach to developing a shared curriculum that includes a trainee-based needs assessment, identification of goals and objectives, development of educational strategies, implementation, and objective assessment and evaluation. As formalized PCCM fellowship global health training is in its infancy, this is the optimal time to create a structured approach to PCCM global health education. A formalized set of core competencies could also be adapted to training programs in other specialties, such as emergency medicine, infectious diseases, surgery, and obstetrics and gynecology, among others. To accomplish this goal, we can build on the work of the Association of Schools and Programs of Public Health, which is developing a global health competency model (24), and from work to define the goals of global health education within medical school curricula (41). We have previously proposed four core competencies around which to formalize PCCM global health training (1). These four competency areas include: 1) clinical knowledge, 2) research training, 3) cultural competency, and 4) clinical and/or research capacity building (Table 2). We posit that using competencies to design a framework for global health education will produce foundational knowledge for PCCM trainees that can be expanded by specific educational experiences driven by trainee interests. Proposed competencies should align with existing ACGME-mandated programmatic requirements (42), such that their completion simultaneously fulfills both global health and ACGME-related requirements.
Table 2.
Proposed core competency areas for global health education in pulmonary and critical care medicine fellowship training programs
| Core Competency Areas | Objectives |
|---|---|
| Clinical knowledge | Develop a comprehensive understanding of the global burden of respiratory and critical illness, including: |
| Knowledge of the global epidemiologic distribution of major infectious and noncommunicable diseases imparting morbidity and mortality. | |
| Social, environmental, and economic determinants of health, including how host-, environmental-, and health systems–based factors govern health worldwide. | |
| Identification of the clinical presentation and management of complex diseases in resource-limited settings through completing didactic coursework concerning major pathological processes (e.g., malaria, tuberculosis, viral hemorrhagic syndromes, human immunodeficiency virus), their biological alterations, and how they affect specific organ systems. | |
| International research training | Complete didactic coursework and receive mentorship from domestic and international investigators, focused on developing an understanding of the unique cultural, legal, and societal considerations required of research conducted in low- and middle-income countries, including: |
| International research ethics and human subject protection. | |
| Needs assessment, including community-based involvement, to generate locally relevant research. | |
| Study design and implementation. | |
| Cultural competency | Cultivate and develop awareness of the attitudes, beliefs, and processes that facilitate the doctor–patient relationship and allow effective partnership across international clinical and research collaborations by: |
| Actively participating in seminars regarding cultural beliefs and practices of international training sites. | |
| Establishing mechanisms to address conflict resolution in international clinical and research settings. | |
| Clinical and research capacity building | Actively participate in clinical and/or research capacity building with a focus on sustainable, longitudinal partnerships by developing: |
| “Train the trainer” educational models to develop local subspecialty expertise, ultimately aimed at local clinical and research independence. | |
| Multilevel participatory needs assessments with international stakeholders. |
Reprinted by permission from Reference 1.
The main strength of this survey is that it is a nationally representative sample of PCCM program leadership, which allows for the first-ever characterization of global health–related training opportunities in U.S.-based PCCM fellowship programs. Nonetheless, this survey has several limitations. First, although we have attempted to characterize global health training opportunities in PCCM fellowship from a programmatic perspective, notably absent from this discussion is the perspective of current and prospective fellows. It is crucial to evaluate the concordance (or lack thereof) between PCCM leaders’ perspectives and that of current and prospective PCCM fellows. Our data suggest that, from the perspective of program leaders, a portion of prospective PCCM fellows are seeking global health–related training opportunities. A systematic needs assessment among current and prospective PCCM trainees is critical to inform nascent efforts to formalize global health training within the specialty.
Another limitation is that we were unable to evaluate the larger institutional environment within which individual PCCM programs operate, which is likely to influence the presence and extent of global health–related training opportunities. In addition, the response rate of 37% may limit generalizability because of nonresponse bias. Indeed, nonresponding programs were less likely to have global health–related training opportunities than responding programs. Notably, our online search could not identify global health–related educational components of nonresponding programs with the same granularity as our survey, and we may have consequently underestimated the presence of global health–related training opportunities. Nonetheless, this survey provides important insights into the presence and extent of global health–related educational content across PCCM training programs and provides a framework for future efforts on this topic.
Conclusions
Published literature supports that there is interest among medical trainees for global health–related opportunities (1–10), and our survey adds that PCCM fellowship program leadership has interest in providing these opportunities. But, important barriers to offering global health–related opportunities remain. Before dedicating resources to expanding global health–related training in PCCM fellowship, further work is necessary to characterize the interest of current and prospective fellows in global health–related training opportunities, compare the relative importance of global health training with other components of fellowship training, and evaluate the use of existing global health–related training opportunities. Additional unanswered questions include what constitutes global health–related training needs, how to align those training needs with current ACGME-mandated training requirements, and how to design creative solutions for providing access to global health training across academic institutions with limited local global-health training capacity.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank the University of Washington International Respiratory and Severe Illness Center (www.intersectuw.org) for generous support of this survey, the Association of Pulmonary and Critical Care Medicine Program Directors for distribution of the online survey, the program directors who assisted us in pilot testing the questions, and the program directors and associate program directors who provided survey responses.
Footnotes
Gift cards for survey participation were funded by the University of Washington International Respiratory and Severe Illness Center. The views expressed in this article do not communicate an official position of the University of Washington International Respiratory and Severe Illness Center or any of the authors’ affiliated institutions.
Author Contributions: Substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data for the work: C.M.N., E.F.A., K.E.R., T.S., R.E., and T.E.W. Drafting of manuscript: C.M.N., E.F.A., K.E.R., and T.S. Contributed to the content, phrasing, and structure of the questions included in the online survey: A.P., B.Ç., E.J.C., D.C.C., J.B.R., L.H., and W.C. All authors revised the manuscript critically for important intellectual content, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Siddharthan T, North CM, Attia EF, Christiani DC, Checkley W, West TE. Global health education in pulmonary and critical care medicine fellowships. Ann Am Thorac Soc. 2016;13:779–783. doi: 10.1513/AnnalsATS.201601-028PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drain PK, Primack A, Hunt DD, Fawzi WW, Holmes KK, Gardner P. Global health in medical education: a call for more training and opportunities. Acad Med. 2007;82:226–230. doi: 10.1097/ACM.0b013e3180305cf9. [DOI] [PubMed] [Google Scholar]
- 3.Adams LV, Wagner CM, Nutt CT, Binagwaho A. The future of global health education: training for equity in global health. BMC Med Educ. 2016;16:296. doi: 10.1186/s12909-016-0820-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Drain PK, Holmes KK, Skeff KM, Hall TL, Gardner P. Global health training and international clinical rotations during residency: current status, needs, and opportunities. Acad Med. 2009;84:320–325. doi: 10.1097/ACM.0b013e3181970a37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khan OA, Guerrant R, Sanders J, Carpenter C, Spottswood M, Jones DS, et al. Global health education in U.S. medical schools. BMC Med Educ. 2013;13:3. doi: 10.1186/1472-6920-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peluso MJ, Forrestel AK, Hafler JP, Rohrbaugh RM. Structured global health programs in U.S. medical schools: a web-based review of certificates, tracks, and concentrations. Acad Med. 2013;88:124–130. doi: 10.1097/ACM.0b013e3182765768. [DOI] [PubMed] [Google Scholar]
- 7.McCunn M, Speck RM, Chung I, Atkins JH, Raiten JM, Fleisher LA. Global health outreach during anesthesiology residency in the United States: a survey of interest, barriers to participation, and proposed solutions. J Clin Anesth. 2012;24:38–43. doi: 10.1016/j.jclinane.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Kerry VB, Walensky RP, Tsai AC, Bergmark RW, Bergmark BA, Rouse C, et al. US medical specialty global health training and the global burden of disease. J Glob Health. 2013;3:020406. doi: 10.7189/jogh.03.020406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson BD, Lee AC, Newby PK, Chamberlin MR, Huang CC. Global health training in pediatric residency programs. Pediatrics. 2008;122:28–33. doi: 10.1542/peds.2007-2178. [DOI] [PubMed] [Google Scholar]
- 10.Velji A. Global health education consortium: 20 years of leadership in global health and global health education. Infect Dis Clin North Am. 2011;25:323–335. doi: 10.1016/j.idc.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Koplan JP, Bond TC, Merson MH, Reddy KS, Rodriguez MH, Sewankambo NK, et al. Consortium of Universities for Global Health Executive Board. Towards a common definition of global health. Lancet. 2009;373:1993–1995. doi: 10.1016/S0140-6736(09)60332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carballo M, Divino JJ, Zeric D. Migration and health in the European Union. Trop Med Int Health. 1998;3:936–944. doi: 10.1046/j.1365-3156.1998.00337.x. [DOI] [PubMed] [Google Scholar]
- 13.Gakidou E, Afshin A, Abajobir AA, et al. GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1345–1422. doi: 10.1016/S0140-6736(17)32366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Global health estimates 2016: deaths by cause, age, sex, by country and by region. 2000–2016. Geneva: World Health Organization; 2018. [created 2018 May 24; accessed 2018 Nov 12]. Available from: http://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. [Google Scholar]
- 15.Bousquet J, Kiley J, Bateman ED, Viegi G, Cruz AA, Khaltaev N, et al. Prioritised research agenda for prevention and control of chronic respiratory diseases. Eur Respir J. 2010;36:995–1001. doi: 10.1183/09031936.00012610. [DOI] [PubMed] [Google Scholar]
- 16.Ferkol T, Schraufnagel D. The global burden of respiratory disease. Ann Am Thorac Soc. 2014;11:404–406. doi: 10.1513/AnnalsATS.201311-405PS. [DOI] [PubMed] [Google Scholar]
- 17.Adhikari NK, Rubenfeld GD. Worldwide demand for critical care. Curr Opin Crit Care. 2011;17:620–625. doi: 10.1097/MCC.0b013e32834cd39c. [DOI] [PubMed] [Google Scholar]
- 18.Kiwanuka SN, Ekirapa EK, Peterson S, Okui O, Rahman MH, Peters D, et al. Access to and utilisation of health services for the poor in Uganda: a systematic review of available evidence. Trans R Soc Trop Med Hyg. 2008;102:1067–1074. doi: 10.1016/j.trstmh.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 19.Manocha S, Walley KR, Russell JA. Severe acute respiratory distress syndrome (SARS): a critical care perspective. Crit Care Med. 2003;31:2684–2692. doi: 10.1097/01.CCM.0000091929.51288.5F. [DOI] [PubMed] [Google Scholar]
- 20.Kumar A, Zarychanski R, Pinto R, Cook DJ, Marshall J, Lacroix J, et al. Canadian Critical Care Trials Group H1N1 Collaborative. Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA. 2009;302:1872–1879. doi: 10.1001/jama.2009.1496. [DOI] [PubMed] [Google Scholar]
- 21.Arabi YM, Arifi AA, Balkhy HH, Najm H, Aldawood AS, Ghabashi A, et al. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med. 2014;160:389–397. doi: 10.7326/M13-2486. [DOI] [PubMed] [Google Scholar]
- 22.Fowler RA, Fletcher T, Fischer WA, II, Lamontagne F, Jacob S, Brett-Major D, et al. Caring for critically ill patients with Ebola virus disease: perspectives from West Africa. Am J Respir Crit Care Med. 2014;190:733–737. doi: 10.1164/rccm.201408-1514CP. [DOI] [PubMed] [Google Scholar]
- 23.West TE, von Saint André-von Arnim A. Clinical presentation and management of severe Ebola virus disease. Ann Am Thorac Soc. 2014;11:1341–1350. doi: 10.1513/AnnalsATS.201410-481PS. [DOI] [PubMed] [Google Scholar]
- 24.Ablah E, Biberman DA, Weist EM, Buekens P, Bentley ME, Burke D, et al. Improving global health education: development of a Global Health Competency Model. Am J Trop Med Hyg. 2014;90:560–565. doi: 10.4269/ajtmh.13-0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Butteris SM, Schubert CJ, Batra M, Coller RJ, Garfunkel LC, Monticalvo D, et al. Global health education in US pediatric residency programs. Pediatrics. 2015;136:458–465. doi: 10.1542/peds.2015-0792. [DOI] [PubMed] [Google Scholar]
- 26.Bissonette R, Routé C. The educational effect of clinical rotations in nonindustrialized countries. Fam Med. 1994;26:226–231. [PubMed] [Google Scholar]
- 27.Haq C, Rothenberg D, Gjerde C, Bobula J, Wilson C, Bickley L, et al. New world views: preparing physicians in training for global health work. Fam Med. 2000;32:566–572. [PubMed] [Google Scholar]
- 28.Panosian C, Coates TJ. The new medical “missionaries”--grooming the next generation of global health workers. N Engl J Med. 2006;354:1771–1773. doi: 10.1056/NEJMp068035. [DOI] [PubMed] [Google Scholar]
- 29.Bussell SA, Kihlberg CJ, Foderingham NM, Dunlap JA, Aliyu MH. Global health education in general preventive medicine residencies. Am J Prev Med. 2015;48:593–598. doi: 10.1016/j.amepre.2014.12.013. [DOI] [PubMed] [Google Scholar]
- 30.Zink T, Solberg E. Development of a global health curriculum for family medicine based on ACGME competencies. Teach Learn Med. 2014;26:174–183. doi: 10.1080/10401334.2014.883987. [DOI] [PubMed] [Google Scholar]
- 31.Havryliuk T, Bentley S, Hahn S. Global health education in emergency medicine residency programs. J Emerg Med. 2014;46:847–852. doi: 10.1016/j.jemermed.2013.11.101. [DOI] [PubMed] [Google Scholar]
- 32.Bjorklund AB, Cook BA, Hendel-Paterson BR, Walker PF, Stauffer WM, Boulware DR. Impact of global health residency training on medical knowledge of immigrant health. Am J Trop Med Hyg. 2011;85:405–408. doi: 10.4269/ajtmh.2011.10-0732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koplan J, Bond T, Merson M, et al. Towards a common definition of global health. Lancet. 2009;373:1993–1995. doi: 10.1016/S0140-6736(09)60332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Association of Schools and Programs of Public Health. Academic program finder. Washington, D.C.: ASPPH; [accessed 2019 Mar 12]. Available from: https://programfinder.aspph.org/
- 35.Heimburger DC, Carothers CL, Gardner P, Primack A, Warner TL, Vermund SH. Nurturing the global workforce in clinical research: the National Institutes of Health Fogarty International Clinical Scholars and Fellows program. Am J Trop Med Hyg. 2011;85:971–978. doi: 10.4269/ajtmh.2011.11-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown HA, Mulherin P, Ferrara WC, Humphrey ME, Vera A, Hall JW. Using future employers’ expectations to inform global health fellowship curricula. J Grad Med Educ. 2018;10:517–521. doi: 10.4300/JGME-D-18-00348.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rudy S, Wanchek N, Godsted D, Blackburn M, Mann E. The PHI/GHFP-II employers’ study: the hidden barriers between domestic and global health careers and crucial competencies for success. Ann Glob Health. 2016;82:1001–1009. doi: 10.1016/j.aogh.2016.10.012. [DOI] [PubMed] [Google Scholar]
- 38.Palazuelos D, Dhillon R, Nelson AK, Savage KP, Conover R, Katz JT, et al. Training toward a movement: career development insights from the first 7 years of a global health equity residency. J Grad Med Educ. 2018;10:509–516. doi: 10.4300/JGME-D-18-00213.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schultz MJ, Dunser MW, Dondorp AM, Adhikari NK, Iyer S, Kwizera A, et al. Global Intensive Care Working Group of the European Society of Intensive Care Medicine. Current challenges in the management of sepsis in ICUs in resource-poor settings and suggestions for the future. Intensive Care Med. 2017;43:612–624. doi: 10.1007/s00134-017-4750-z. [DOI] [PubMed] [Google Scholar]
- 40.Papali A, Schultz MJ, Dünser MW European Society of Intensive Care Medicine (ESICM) Global Intensive Care working group and The Mahidol–Oxford Research Unit (MORU) in Bangkok, Thailand. Recommendations on infrastructure and organization of adult ICUs in resource-limited settings. Intensive Care Med. 2018;44:1133–1137. doi: 10.1007/s00134-017-4972-0. [DOI] [PubMed] [Google Scholar]
- 41.Arthur MA, Battat R, Brewer TF. Teaching the basics: core competencies in global health. Infect Dis Clin North Am. 2011;25:347–358. doi: 10.1016/j.idc.2011.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in pulmonary disease and critical care medicine. Chicago, IL: ACGME; [revised 2019 Jun 9; accessed 2019 Jun 12]. Available from: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/156_PCCM_2019.pdf?ver=2019-06-13-102121-433 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.