Abstract
Background
Self-Medication with antibiotics is a human practice and attitude in which an individual uses antibiotics to treat self-diagnosed symptoms. The self-medication with antibiotics is a common practice among residents in the UAE.
Purpose
The present study aimed to determine the prevalence of self-medication of antibiotics among residents in the UAE population to determine its associated risk factors and to increase awareness regarding the abuse of antibiotics.
Patients and methods
Three hundred and fifteen participants from different public places in Abu Dhabi, Dubai and Sharjah,UAE received the validated questionnaire over the five-month study period. Collected data were analyzed using SPSS statistical software and the Chi-square test to assess the relationships between categorical variables.
Results
Of 315 participants, 31.7% (n=100) of the respondents reported the use of non-prescription antibiotics within a three-month study period. Self-medication with antibiotics was significantly associated with ethnicity and employment. The participants reported their previous experience with the disease (69; 21.9%), as the main reason for self-medication with antibiotics. The primary sources of antibiotics were those purchased from community pharmacies (70; 22.2%) and household (21; 6.7%).
Conclusion
Our study showed a high prevalence of self-medication behaviour even with the enforcement of the new legislation regarding the prohibition of selling antibiotics without a prescription. Therefore, there is a need to raise public awareness towards the safe use of antibiotics in our community.
Keywords: antibiotics, dispensing, self-medication, Arab, prescription, UAE
Introduction
Prescription of the appropriate antibiotic would improve the patients’ outcomes as well as reduce the development of bacterial resistance.1,2 In developing countries, the prevalence of difficult-to-treat bacterial infections is escalating daily, and they have become a serious threat to public health, leading to an increased mortality rate and decreased quality of life.3,4 Due to the regulatory environment and financial risks, pharmaceutical companies are not participating in the development of new antibiotics. Therefore, they are not able to keep up with the steady developments in antibiotic resistance.5
The World Health Organization (WHO) emphasised the problem of over and inappropriate utilisation of antibiotic that led them to announce their global action plan against antibiotics resistance. The global actions planned to reach such objectives include; improving the awareness and understanding of antimicrobial resistance, strengthening surveillance and research, reducing the infection incidence, optimizing the use of antimicrobial medicines, and ensuring sustainable investment in combating antimicrobial resistance.
Self-medication with antibiotics is a common practice among residents in the United Arab Emirate (UAE); which has an estimated population of 9.68 millions of different ethnic groups in 2019.6 Therefore, the Ministry of Health (MOH) issued a new health legislation prohibiting the dispensing of antibiotics without a medical prescription.7 The self-medication of antibiotics is a human practice and attitude in which an individual uses antibiotics to treat self-diagnosed symptoms.8,9 Moreover, self-medication is a grave threat to health as it increases the risk of antibiotics resistance development.10–12 According to a study commissioned by the UK government in 2014, approximately 700,000 people would die annually from drug-resistant bacteria, and by 2050, it could well soar to 10 million, which exceed the worldwide deaths from cancer.13 This represents a warning sign for physicians who constantly overprescribe antibiotics. For nearly eighty years, the agriculture industry has been giving sub-therapeutic doses of antibiotics to livestock. Many antimicrobials known as growth promoters are used to increase the weight of animals. Humans are at high risk of acquiring infections due to resistant pathogens from livestock production system or food chain animals.14,15 Ensuring sanitation and clean water for everyone are fundamentals to avoid the need for antibiotics and excessive antibiotic use. Accessibilty to the medications when people demand them also contributes to antimicrobial resistance issue.
Moreover, several worldwide websites allow patients to access antibiotics without medical diagnosis and a prescription.9
Many physicians face significant pressure from patients who want rapid relief from their pain and symptoms. Worried parents put pressure on the physician to prescribe antibiotics for their children, especially if high fever is present. Since the physician may be concerned about the possibility of losing a patient, by going to another physician, he would be willing to prescribe antibiotics to please the patient even if the patient has a viral infection.16 In addition, physician’s belief regarding antibiotic use in primary care may be considered. A study published in Australia reported that the majority of physicians did not consider that the patients’ resistance to antibiotics was due to their regular prescription of antibiotics in primary care. They also believe that their inappropriate prescribing would not affect many people as their harmful effect is minor compared to hospital prescribing.17,18
In the UAE, community pharmacists frequently allow access to antibiotics without the presence of a prescription. Health authorities did not enforce dispensing prescription-only medicine (POM) to many pharmacies for a long time. Pharmacists do not have access to the list of medications designated as POM and are not mandated to keep a copy of antibiotics that they dispense in their pharmacies. The MOH and health authorities do not monitor the sale of antibiotics between distributors and pharmacies to check which pharmacies buy the majority of antibiotics and therefore selling them without prescriptions. Different factors encourage the pharmacists to sell antibiotics for patients, even for mild symptoms of cold or flu, lack of strict rules and penalty for dispensing antibiotics without prescriptions, lack of knowledge, patient demand, and high profitability of some antibiotics.19 An earlier study in Egypt reported that 54% of the antibiotics recommended by community pharmacists were inappropriate.20 In addition, antibiotic access without prescription was reported from other neighbouring countries in the Gulf region.9 In the UAE, data on the use of antibiotics without prescription are available before the implementation of the new rules to curb the misuse of antibiotics. The present study is the first conducted investigation following the implementation of the new rule. The study aimed to estimate the prevalence of antibiotics self-medication among UAE population, to understand the factors that allow the people to obtain antibiotics without a prescription and to raise awareness regarding the appropriate use of antibiotics.
Materials And Methods
A descriptive, cross-sectional study carried out in Abu Dhabi, Dubai, and Sharjah, UAE over the period of four months, from January to May 2018.
Questionnaire Development
A validated, well-organized, self-administered questionnaire was developed as a version of that in a study done in Jordon.21 The questionnaires were randomly distributed in public places of Abu Dhabi, Dubai, and Sharjah; to collect the data. The questionnaires were prepared in two languages: English and Arabic. The researchers clarified the aim of the study in the information sheet provided and obtained signed informed consents from all participants except those below the age of 18 years, who their birth mother or father signed the informed consent on their behalf. The questionnaire consisted of two sections: The first section included the demographic data such as age, gender, number of family members, socio-economic factors, and the relation of their job/education to the medical field. The second section included questions about the participant’s medication behaviour; the purpose for taken the antibiotic, whether it was obtained from a friend/relative, a pharmacy, or household, reasons for self-medication with antibiotics, and other questions. The survey included some questions with multiple options (Appendix 1). The researchers provided a short awareness briefing about the use of antibiotics to the participants after they have completed the survey. The sample size was calculated using Raosoft online sample size calculator (Raosoft Inc., Seattle, WA USA), to choose a convenient sample of the population from the targeted three emirates, resulting in 350 questionnaires. The confidence interval of 95%, 5% margin of error, and 50% for the expected response distribution were determined. The inclusion criteria were UAE residents who took antibiotics within the last three months. Exclusion cirteria included; non-UAE residents, respondents who did not take an antibiotic in the last three months, and those who failed to identify antibiotics correctly (for example, confusing antibiotics with pain relievers). A period of three months was selected to obtain more accurate responses about the use of the antibiotics and to remove the possible bias upon recalling events.22
Validity And Reliability Testing
The survey questions were obtained from a validated previous study.21 To assess test–retest reliability, we asked ten participants from the academic members of the University of Sharjah to answer and comment on the questionnaire on two separate occasions with two weeks in-between. The participants reported no changes or comments and we calculated the test–retest reliability using Spearman correlation coefficient (r). The rho value obtained was 0.87, implying an acceptable level of test–retest reliability.
Statistical Analysis
Collected data were analysed using Statistical Package for the Social Sciences (SPSS version 20). Whenever applicable, we used descriptive statistics and we applied the chi-square test to assess the relationship between the independent variable (Demographic Data) and the dependent variable (The population opinion about self-medication). As a cut-off point for significance, we used the level P < 0.05. We calculated both the Chi-square and P values using STATA V.12.0 software (Software for Statistics and Data Science, StataCorp LLC, TX, USA.
Results
Out of 350 distributed surveys, 315 respondents reported that they had used antibiotics within the last three months, giving a response rate of 90%. Among the total participants, 64.4% were females. Table 1 shows the participants’ age, job/education level, ethnicity, and medical insurance coverage.
Table 1.
Demographic Characteristics of the Participants in this Study
| Variables | N (%) |
|---|---|
| Age (Years) | |
| <18 years | 8 (2.5%) |
| 18–29 years | 135 (42.9%) |
| 30–39 years | 89 (28.3%) |
| 40–49 years | 52 (16.5%) |
| 50–59 years | 23 (7.3%) |
| >60 years | 8 (2.5%) |
| Gender | |
| Male | 112 (35.6%) |
| Female | 203 (64.5%) |
| Education | |
| None | 0 |
| Secondary School | 8 (2.5%) |
| Bachelor Degree or Higher | 307 (97.5%) |
| Job/Education Related To The Medical Field: | |
| Yes | 233 (74%) |
| No | 82 (26%) |
| Ethnicity: | |
| Arab | 204 (64.8%) |
| Non-Arab | 111 (35.2%) |
| Employment: | |
| Employed | Employed=232 (73.7%) |
| Not-employed | Non-Employed=83 (26.3%) |
| Residential Area: | |
| Abu Dhabi | 149 (47.3%) |
| Dubai | 83 (26.2%) |
| Sharjah | 83 (26.2%) |
| Medical Insurance: | |
| Yes | 280 (88.9%) |
| No | 35 (11.1%) |
Participants were divided into two groups, self-medicating and non-self-medicating. Penicillins were the most commonly used class of antibiotics by respondents (42.7%), among which amoxicillin-clavulanate recorded the highest (30%) use. Moreover, sulfonamides, nitrofurans, and lincosamides showed the lowest numbers in the same order (Table 2).
Table 2.
The Frequency Of Specific Antibitotics Use
| Antimicrobial Agents | N (%) |
|---|---|
| Penicillins | 135 (42.7%) |
| Macrolides | 47 (14.8%) |
| Quinolones | 46 (14.6%) |
| Cephalosporins | 24 (7.5%) |
| Tetracyclines | 11 (3.5%) |
| Nitroimidazoles | 10 (3.1%) |
| Sulfonamides | 2 (0.6%) |
| Nitrofurans | 1 (0.3%) |
| Lincosamides | 1 (0.3%) |
| Total without missing | 277 (87.4%) |
| Total with missing | 315 (100%) |
| Missing | 38 (12.6%) |
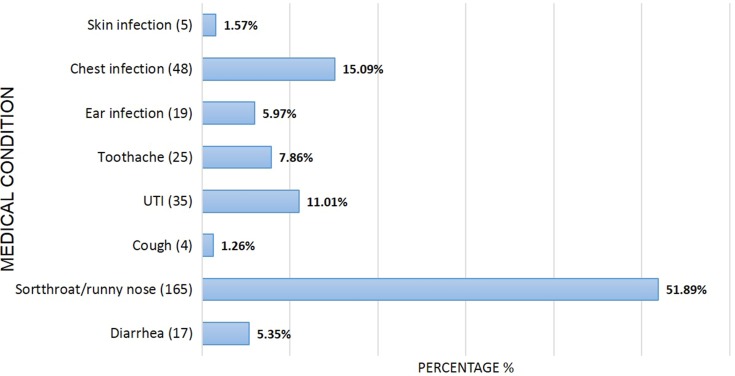
According to the findings, 68.2% of the respondents reported that their physicians prescribed the antibiotic used. Interestingly, 21.9% of the respondents reported that they used antibiotics based on their previous personal experience. Furthermore, 5.7% and 4.4% reported their use of antibiotics was based on advice from a friend/relative or a community pharmacist. Most participants reported that they used an antibiotic for the treatment of a sore throat and runny nose (Figure 1).
Figure 1.
Medical Condition for which Antibiotics were Used by the Participants in this Study.
About 20% of participants reported that the reason for self-medication with antibiotics was their thought that it was unnecessary to visit a physician because of their personal previous experience with the medication. Other reasons include cost-saving (7.6%), time-wasting (10.5%), and inconvenience to keep on visiting the physician (5.1%). Self-medicating participants were requested to provide information about how they accessed their antibiotics and it was found that the highest percentage (69.3%) of participants reported community pharmacy as the source of their purchased antibiotic, whereas 20.8% of the participants used leftover medications from their household.
Moreover, participants were asked about what they do if they have any side effects occur during their use of antibiotics and it was found that 47.6% of the participants reported that they would discontinue the use of antibiotics, 4.4% stated that they would switch to another type, 5.4% reported that they will continue the use of antibiotics and 56.4% asserted that they would consult a health professional.
Furthermore, the findings of the present study demonstrated that the participants depended mainly on the physician and pharmacist as the most accessible source of information to know about the accurate antibiotic use. On the other hand, respondents referred to the medication leaflet, acquired instructions from their relatives or friends and browsed to the internet (Table 3). Nevertheless, more than half of the participants (62.3%) mentioned their ability to treat themselves effectively if they have any common diseases, out of which 28.4% were from non-medical profession.
Table 3.
Sources Of Information Used By Participants
| Information Sources | N (%) |
|---|---|
| Physician | 164 (52.1%) |
| Pharmacist | 160 (51.1%) |
| Relatives/Friends | 21 (6.7%) |
| Leaflet | 61 (19.4%) |
| Internet | 10 (3.2%) |
Respondents reported that they used the antibiotic for 4–7 days (65.7%). However, 20% reported using the antibiotic for only 1–3 days and only 14.3% stated that they administered it for more than seven days.
Remarkably, when asked about when they stopped their antibiotics, almost three quarters (74.9%) of participants recorded stopping antibiotic use at the completion of the course. However, 22.2% reported that they would stop the use of antibiotics as soon as they feel better.
Job/education (P<0.001), and Medical insurance (P <0.001) significantly influenced the participant’s response to the discontinuation of antibiotic (P <0.001) significantly influenced the participant’s response to the discontinuation of antibiotic (Table 4). Of the participants whose job/education is not related to the medical field, 13.3% reported that they stop the antibiotic as soon as they feel better, besides 12.1% stated that they stop the antibiotic at the completion of the course. The relationship between the demographic characteristics and participants’ opinion to treat common disease efficiently by themselves is summarised in Table 5.
Table 4.
The Relationship Between The Demographic Data And Discontinuation Of Antibiotic
| Demographic Data | Grouping | When Do You Usually Discontinue Antibiotic Administration | P Value | |||||
|---|---|---|---|---|---|---|---|---|
| After I Feel Better | Insufficient Supply | At The Completion Of The Course | After Consulting A Doctor/Pharmacist | I Felt It Was Not Effective | I Faced Some Adverse Effects | |||
| Age | <(18) (18–29) (30–39) (40–49) (50–59) (>60) |
5 (1.59%) 27 (8.57%) 11 (3.49%) 16 (5.08%) 9 (2.86%) 2 (0.63%) |
0 0 0 1 (0.32%) 0 0 |
3 (0.95%) 105 (33.33%) 76 (24.13%) 32 (10.16%) 14 (4.44%) 6 (1.90%) |
0 2 (0.63%) 1 (0.32%) 3 (0.95%) 0 0 |
0 0 1 (0.32%) 0 0 0 |
0 1 (0.32%) 0 0 0 0 |
0.115 |
| Gender | Male Female |
26 (8.25%) 44 (13.97%) |
0 1 (0.32%) |
84 (26.67%) 152 (48.25%) |
2 (0.63%) 4 (1.27%) |
0 1 (0.32%) |
0 1 (0.32%) |
0.883 |
| Ethnicity | Arab Non-Arab |
55 (17.46%) 15 (4.76%) |
1 (0.32%) 0 |
141 (44.76%) 95 (30.16%) |
5 (1.59%) 1 (0.32%) |
1 (0.32%) 0 |
1 (0.32%) 0 |
0.052 |
| Job/Education Related To The Medical Field |
Yes No |
28 (8.89%) 42 (13.33%) |
1 (0.32%) 0 |
198 (62.86%) 38 (12.06%) |
5 (1.59%) 1 (0.32%) |
1 (0.32%) 0 |
0 1 (0.32%) |
<0.001 |
| Employment | Employed Unemployed | 32 (10.16%) 28 (8.89%) |
1 (0.32%) 0 |
183 (58.09%) 53 (16.82%) |
5 (1.59%) 1 (0.32%) |
1 (0.32%) 0 |
0 1 (0.32%) |
0.121 |
| Medical Insurance | Yes No |
54 (17.14%) 16 (5.08%) |
1 (0.32%) 0 |
218 (69.21%) 18 (5.71%) |
6 (1.90%) 0 |
1 (0.32%) 0 |
0 1 (0.32%) |
<0.001 |
Note: Bold values represent significant P values.
Table 5.
The Relationship Between The Demographic Characteristics And Participants’ Opinion on Self-Treatment of Common Diseseas
| Demographic Characteristic | Self-Treatment Of Common Diseases (n(%)) | Chi-Square | P Value |
|---|---|---|---|
| Job/Education | Medical field=156 (71.6%) Non-medical field=62 (28.4%) |
5.07 | 0.079 |
| Gender | Male=84 (38.5) Female=134 (61.5) |
4.08 | 0.130 |
| Ethnicity | Arab=150 (68.8%) Non-Arab=68 (31.2%) |
6.37 | 0.041 |
| Employment | Employed=157 (72%) Non-Employed=61(28%) |
11.96 | 0.003 |
| Medical insurance | Insurance=192 (88.1%) Without insurance=26 (11.9%) |
1.35 | 0.510 |
| Number of participants who reported “Yes’’ they can treat common disease efficiently by themselves=218 (69.2%) | |||
Discussion
Despite the implementation by the UAE Ministry of Health of the new legislation to curb the misuse and abuse of non-prescribed antibiotics, the present study found that still 31.7% of the participants reported that they had used an antibiotic without a prescription from a physician, which was either obtained from a community pharmacy, relative/friends or households. Most of the respondents (21%) reported that they had previous experience with the antibiotic, thinking that they were able to effectively diagnose and treat themselves every time they experienced the same symptoms, similar findings were observed in a study conducted in Portugal.23
In Jordan and Saudi Arabia,21,24 females used antibiotics more than males did; this is in agreement with the results of our study, however; inconsistent with a study in Yemen.25 In comparison with previous studies conducted in UAE and Jordan,21,26 the use of self-medication with antibiotics was affected by age and gender. In the present study, we did not find similar association between demographics and responses to questions. The opinion of the respondents about treating themselves was notably affected by ethnicity (P Value=0.041), where 68.8% where Arabs, and by employment (P Value=0.003), where 72% were employed (Table 5).
This association demonstrates that different ethnic groups may affect the use of antibiotics without a prescription, despite being POM.27,28 Another study also indicated that the difference in cultural beliefs and attitudes about illnesses may influence the use of self-medication.27
It was observed that people who were employed had higher level of antibiotics/self-medication use (P Value=0.003) (Table 5), this might be for the reason that employed adults had higher perceptivity because of work-related exposure and sleep disorders.29 Similar results were shown in a study done in Brazil.30
As shown in Table 5, the majority (71.6%) of participants were related to the medical field, and hence may have an easier access to antibiotics. Long working hours and to avoid the long waiting time at clinics and hospitals have been reported as contributing factors for use of antibiotics for self-medications.31–33 However, our study did not show high significance in relation to job/education related to medical field (P Value=0.079).
Community pharmacy was one of the most referred sources for participants to obtain their antibiotics without prescription (22.2%), which is comparable to other studies in the UAE, Jordan and Sudan,8,21,34 this is quite presumed since pharmacies are the primary source of drugs. Therefore, it is fundamental for community pharmacists to have sufficient competence and knowledge to provide rational drug use to patients and should be closely monitored by the health authorities.
In addition, due to the mandatory health insurance and high co-pay for physician visits, participants reported that it was easier and cheaper to access community pharmacies and to seek treatment including antibiotics than to seek physician consultation. Many pharmacists have set sales targets to reach, and antibiotics constitute a large percentage of the sales for the pharmacies.
Due to cultural attitudes, residents remined to rely on having easy access to antibiotics regardless of the new law. Unfortunately, leftover medications from household as an alternative source were also prevalent in our study and another study in UAE.26 Some patients might directly run to their medicine cabinets for immediate relief of nagging symptoms. Others might take expired medications which may cause some risks including lack of efficacy of the product; rare kidney disease called renal tubular damage, which was previousely reported as a result of Tetracycline.35 A study done in Spain also concluded the storage of antibiotics reduced the efficacy and quality of the treatment at the community level.36
Leftover medications might be stored inappropriately, which could cause defects in the medication leading to ineffective treatment. Therefore, proper storage is extremely critical for the efficiency, efficacy, and safety of medicines.
In the present study, participants reported that amoxicillin-clavulanate was the most commonly used antibiotic. This finding may seem reasonable considering the fact that it rarely leads to the emergence of bacterial resistance. Lack of infection control measures, irrational antibiotic use and the continuous noncompliance to the safe use of antibiotics will contribute to the emergence of bacterial resistance. Other antibiotics included macrolides, quinolones, and cephalosporins in correlation with results from studies conducted in Jordan, UAE, and Saudi Arabia.21,24,26
Slightly more than 50% of the respondents used antibiotics to relieve symptoms of a sore throat and runny nose (52.4%); these symptoms are common with flu caused by viruses and do not require antibacterial medications since most viral infections are self-limiting. Therefore, a correct diagnosis, advice, and education are necessary from the physician to prevent risk of self-medication and taking of an inappropriate medication.37 The pharmacist may not have the appropriate diagnostic measures to differentiate if the patient suffers from a bacterial or a viral infection.
Asking participants about instructions of the medication use, most of them reported that pharmacists and doctors were their sources of information. This response is in agreement with similar previous studies.21,25 Pharmacists were one of the leading sources of information. This is an expected result since pharmacists are frontline health-care providers and the most familiar with drugs use. Other sources of information included medication leaflets, advice from friends/relatives and the internet. These sources were found to be common in other studies as well.21
Health-care professionals, including pharmacists, are reliable, trustworthy source of medical advice to the population and can play an essential role in the prevention of irrational antibiotic use. Responsible use of antibiotics by the public can be achieved by means of providing them with information and improving their knowledge about the possible risks associated with antibiotics misuse/overuse, stressing on the relation between an incomplete course of antibiotic and ineffectiveness of the treatment. Altogether, this will reduce the bacterial resistance issues worldwide.10
According to our results, the majority of the respondents used antibiotics for four to seven days, and a significant number of participants used antibiotics for one to three days. Similar findings were previously reported.21
It is most likely to be a result of stopping the antibiotic when the patient feels better or when the symptoms disappear; being unaware of the health risks associated with non-compliance to the complete specified period of medication use such as the development of bacterial resistance. This occurs when the therapeutic levels of the drug are insufficient in eliminating the infecting bacteria. A smaller group of participants reported using the antibiotic for more than 7 days, depending on the condition treated.
Jobs/education of participants, who reported that they stopped the antibiotic after the completion of the course were related to the medical field. For this reason, they might be aware of the health risk associated with stopping the medication without consultation from a health-care provider. On the other hand, 12% of the participants from non-medical field reported that they stopped the use of antibiotic as soon as they feel better. Proper health education and adopting a regular education attitude may have a direct positive influence on people’s attitude toward self-medication.38
Prior to implementation of the strict legislation prohibiting dispensing antibiotics without a medical prescription, pharmacists dispensing antibiotics without a medical prescription from a licensed physician were not subjected to any specific action. According to a study done in the UAE in 2009, 44% of the participants reported that they obtained antibiotics without prescriptions.26 However, despite the strict new law implemented which includes punishing pharmacists who violate the rules, 31.7% of the participants reported that they have obtained an antibiotic without a prescription. Since the legislaton was recently implemented, a small regression may be expected.
Limitation
In our study, the majority of the participants were with medical profession background. On the other hand, general public participation was much less. We, therefore, recommend that a further trial with a more robust design to be conducted and studied.
Conclusion
The findings of the present study showed a high prevalence of self-medication of antibiotics in the presence of implementation of the authority’s new health legislation regarding the ban of selling antibiotics without a prescription. Self-medication is a leading cause of emergence of antibiotic resistance globally. Therefore, there is a need for collaborative efforts to raise awareness regarding the safe use of antibiotic drugs to reduce the incidence of antibiotic resistance crisis from occurring in our community.
Acknowledgments
The authors would like to thank the participants for their contribution to this study.
Ethics Statement
We obtained ethical approval (Reference Number: REC-18-03-12-01-S) to conduct the study from The Research and Ethics Committee of the Colleges of Medicine and Health Sciences, University of Sharjah, UAE.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bell BG, Schellevis F, Stobberingh E, Goossens H, Pringle M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis. 2014;14(1):13. doi: 10.1186/1471-2334-14-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schuts EC, Hulscher MEJL, Mouton JW, et al. Current evidence on hospital antimicrobial stewardship objectives: a systematic review and meta-analysis. Lancet Infect Dis. 2016;16(7):847–856. doi: 10.1016/S1473-3099(16)00065-7 [DOI] [PubMed] [Google Scholar]
- 3.Garofalo L, Di Giuseppe G, Angelillo IF. Self-medication practices among parents in Italy. Biomed Res Int. 2015;2015:1–8. doi: 10.1155/2015/580650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grigoryan L, Burgerhof JGM, Degener JE, et al. Determinants of self-medication with antibiotics in Europe: the impact of beliefs, country wealth and the healthcare system. J Antimicrob Chemother. 2008;61(5):1172–1179. doi: 10.1093/jac/dkn054 [DOI] [PubMed] [Google Scholar]
- 5.Gajdács M. The concept of an ideal antibiotic: implications for drug design. Molecules. 2019;24(5):892. doi: 10.3390/molecules24050892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Population Review. United Arab Emirates Population. Available from: http://worldpopulationreview.com/countries/united-arab-emirates-population/ Published 2019. Accessed April1, 2019.
- 7.UAE Ministry of Health. Ministry of Health and Prevention issues warning against dispensing antibiotics without medical prescription. Available from: http://www.mohap.gov.ae/en/MediaCenter/News/Pages/1921.aspx Published 2017. Accessed April3, 2019.
- 8.Awad AI, Eltayeb IB, Capps PA. Self-medication practices in Khartoum State, Sudan. Eur J Clin Pharmacol. 2006;62(4):317–324. doi: 10.1007/s00228-006-0107-1 [DOI] [PubMed] [Google Scholar]
- 9.El Zowalaty ME, Belkina T, Bahashwan SA, et al. Knowledge, awareness, and attitudes toward antibiotic use and antimicrobial resistance among Saudi population. Int J Clin Pharm. 2016;38(5):1261–1268. doi: 10.1007/s11096-016-0362-x [DOI] [PubMed] [Google Scholar]
- 10.Rather IA, Kim B-C, Bajpai VK, Park Y-H. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci. 2017;24(4):808. doi: 10.1016/J.SJBS.2017.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World health organization. Guidelines for the regulatory assessment of medicinal products for use in self-medication. Available from: https://apps.who.int/medicinedocs/en/d/Js2218e/ Published 2000. Accessed April3, 2019.
- 12.Gajdács M, Paulik E, Szabó A, Andrea S. The opinions of community pharmacists related to antibiotic use and resistance | G. Mario | request PDF. January Available from: https://www.researchgate.net/publication/332167826_The_opinions_of_community_pharmacists_related_to_antibiotic_use_and_resistance Published 2018. Accessed September2, 2019.
- 13.Piddock LJV. Reflecting on the final report of the O’Neill review on antimicrobial resistance. Lancet Infect Dis. 2016;16(7):767–768. doi: 10.1016/S1473-3099(16)30127-X [DOI] [PubMed] [Google Scholar]
- 14.Chang Q, Wang W, Regev-Yochay G, Lipsitch M, Hanage WP. Antibiotics in agriculture and the risk to human health: how worried should we be? Evol Appl. 2015;8(3):240–247. doi: 10.1111/eva.12185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dweba CC, Zishiri O, El Zowalaty M. Methicillin-resistant Staphylococcus aureus: livestock-associated, antimicrobial, and heavy metal resistance. Infect Drug Resist. 2018;11:2497–2509. doi: 10.2147/IDR.S175967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linder JA, Singer DE. Desire for antibiotics and antibiotic prescribing for adults with upper respiratory tract infections. J Gen Intern Med. 2003;18(10):795–801. doi: 10.1046/j.1525-1497.2003.21101.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fletcher-Lartey S, Yee M, Gaarslev C, Khan R. Why do general practitioners prescribe antibiotics for upper respiratory tract infections to meet patient expectations: a mixed methods study. BMJ Open. 2016;6(10):e012244. doi: 10.1136/bmjopen-2016-012244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gajdács M, Edit P, Szabó A. The attitude of community pharmacists towards their widening roles in the prevention and treatment of infectious diseases in the southeast region of Hungary. Gyógyszerészet. 2019;63:26–30. [Google Scholar]
- 19.Mahmoud MA, Aldhaeefi M, Sheikh A, Aljadhey H. Community pharmacists perspectives about reasons behind antibiotics dispensing without prescription: a qualitative study. Biomed Res. 2018;29(21):3792–3796. doi: 10.4066/biomedicalresearch.29-18-1112 [DOI] [Google Scholar]
- 20.Sabry NA, Farid SF, Dawoud DM. Antibiotic dispensing in Egyptian community pharmacies: an observational study. Res Soc Adm Pharm. 2014;10(1):168–184. doi: 10.1016/j.sapharm.2013.03.004 [DOI] [PubMed] [Google Scholar]
- 21.Al-Azzam S, Al-Husein B, Alzoubi F, Masadeh M, Al-Horani MAS. Self-medication with antibiotics in jordanian population. Int J Occup Med Environ Health. 2007;20(4):373–380. doi: 10.2478/v10001-007-0038-9 [DOI] [PubMed] [Google Scholar]
- 22.Bradburn N, Rips L, Shevell S. Answering autobiographical questions: the impact of memory and inference on surveys. Science (80- ). 1987;236(4798):157–161. doi: 10.1126/science.3563494 [DOI] [PubMed] [Google Scholar]
- 23.Ramalhinho I, Cordeiro C, Cavaco A, Cabrita J. Assessing determinants of self-medication with antibiotics among Portuguese people in the Algarve Region. Int J Clin Pharm. 2014;36(5):1039–1047. doi: 10.1007/s11096-014-9992-z [DOI] [PubMed] [Google Scholar]
- 24.Alghadeer S, Aljuaydi K, Babelghaith S, Alhammad A, Alarifi MN. Self-medication with antibiotics in Saudi Arabia. Saudi Pharm J SPJ Off Publ Saudi Pharm Soc. 2018;26(5):719–724. doi: 10.1016/j.jsps.2018.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Albawani SM, B. Hassan Y, Abd-Aziz N, Gnanasan S. Self-medication with antibiotics in Sana’a City, Yemen. Trop J Pharm Res. 2017;16(5):1195. doi: 10.4314/tjpr.v16i5.30 [DOI] [Google Scholar]
- 26.Abasaeed A, Vlcek J, Abuelkhair M, Kubena A. Self-medication with antibiotics by the community of Abu Dhabi Emirate, United Arab Emirates. J Infect Dev Ctries. 2009;3(7):491–497. doi: 10.3855/jidc.466 [DOI] [PubMed] [Google Scholar]
- 27.Dawood OT, Hassali MA, Saleem F, Ibrahim IR, Abdulameer AH, Jasim HH. Assessment of health seeking behaviour and self-medication among general public in the state of Penang, Malaysia. Pharm Pract (Granada). 2017;15(3):991. doi: 10.18549/PharmPract.2017.03.991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Azmi M, Fahad S. A National Survey on the use of medicines III (NSUM III) by Malaysian consumers 2015 | Pharmaceutical services programme. Available from: https://www.pharmacy.gov.my/v2/en/documents/national-survey-use-medicines-iii-nsum-iii-malaysian-consumers-2015.html Accessed September12, 2019.
- 29.Fischer FM, Oliveira DC, Teixeira LR, Teixeira MCTV, do Amaral MA. Effects of work on the health of adolescents. Cien Saude Colet. 2003;8(4):973–984. doi: 10.1590/S1413-81232003000400019 [DOI] [Google Scholar]
- 30.de Moraes ACF, Delaporte TRM, Molena-Fernandes CA, Falcão MC. Factors associated with medicine use and self medication are different in adolescents. Clinics (Sao Paulo). 2011;66(7):1149–1155. doi: 10.1590/s1807-59322011000700005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ali AN, Kai JTTK, Keat CC, Dhanaraj S. Self-medication practices among health care professionals in a Private University, Malaysia. Int Curr Pharm J. 2012;1(10):302–310. doi: 10.3329/icpj.v1i10.11846 [DOI] [Google Scholar]
- 32.Rosen IM, Christie JD, Bellini LM, Asch DA. Health and health care among housestaff in four U.S. internal medicine residency programs. J Gen Intern Med. 2000;15(2):116–121. doi: 10.1046/j.1525-1497.2000.11218.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Allibone A, Oakes D, Shannon HS. The health and health care of doctors. J R Coll Gen Pract. 1981;31(233):728–734. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7338866 Accessed September 15, 2019. [PMC free article] [PubMed] [Google Scholar]
- 34.Sharif SI, Bugaighis LMT. Sharif RS. Self-Medication Practice among Pharmacists in UAE. Pharmacology & Pharmacy 2015; 6: 428–435. doi: 10.4236/pp.2015.69044 [DOI] [Google Scholar]
- 35.Perrone D, Afridi F, King-Morris K, Komarla A, Kar P. Proximal renal tubular acidosis (fanconi syndrome) induced by apremilast: a case report. Am J Kidney Dis. 2017;70(5):729–731. doi: 10.1053/J.AJKD.2017.06.021 [DOI] [PubMed] [Google Scholar]
- 36.Orero A, González J, Prieto J. Antibiotics in Spanish households. Medical and socioeconomic implications. URANO Study Group. Med Clin (Barc). 1997;109(20):782–785. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9493156 Accessed September 15, 2019. [PubMed] [Google Scholar]
- 37.Hernandez-Juyol M, Job-Quesada JR. Dentistry and self-medication: a current challenge. Med Oral. 2002;7(5):344–347. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12415218 Accessed September 14, 2019. [PubMed] [Google Scholar]
- 38.Bennadi D. Self-medication: A current challenge. J Basic Clin Pharm. 2013;5(1):19–23. doi: 10.4103/0976-0105.128253 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- World Population Review. United Arab Emirates Population. Available from: http://worldpopulationreview.com/countries/united-arab-emirates-population/ Published 2019. Accessed April1, 2019.