Abstract
Alpha-synuclein is an intrinsically disordered, highly dynamic protein that pathogenically aggregates into inclusion structures called Lewy bodies, in several neurogenerative diseases termed synucleinopathies. Despite its importance for understanding disease, the oligomerization status of alpha-synuclein in healthy cells remains unclear. Alpha-synuclein may exist predominantly as either a monomer or a variety of oligomers of different molecular weights. There is solid evidence to support both theories. Detection of apparent endogenous oligomers are intimately dependent on vesicle and lipid interactions. Here we consider the possibility that apparent endogenous alpha-synuclein oligomers are in fact conformations of membrane-bound alpha-synuclein and not a bona fide stable soluble species. This perspective posits that the formation of any alpha-synuclein oligomers within the cell is likely toxic and interconversion between monomer and oligomer is tightly controlled. This differs from the hypothesis that there is a continuum of endogenous non-toxic oligomers and they convert, through unclear mechanisms, to toxic oligomers. The distinction is important, because it clarifies the biological origin of synucleinopathy. We suggest that a monomer-only, lipid-centric view of endogenous alpha-synuclein aggregation can explain how alpha-synuclein pathology is triggered, and that the interactions between alpha-synuclein and lipids can represent a target for therapeutic intervention. This discussion is well-timed due to recent studies that show lipids are a significant component of Lewy pathology.
Subject terms: Neuroscience, Molecular biology
Introduction
Alpha-synuclein (αSyn) is an intrinsically disordered, highly flexible protein, which plays an important role in the pathogenesis of several neurodegenerative diseases cumulatively referred to as synucleinopathies. In different synucleinopathies, neurons and/or glia bare the hallmark intracellular deposits of filamentous αsyn1 but the origin of this pathology remains unclear. αSyn oligomers with β-sheet structure (αsynO-β) are toxic to cells, possibly through physical disruption of cellular membranes.2,3 αSynO-β/preformed fibrils (PFFs) generated in vitro or isolated from the brains of patients developing synucleinopathies can “seed” aggregates, especially in transgenic rodent models overexpressing αsyn,4 and initiate a toxic cascade reminiscent of that seen in disease.5–7 However, not all oligomers are believed to be bad actors, as evidence suggests that various oligomers may not only exist in the cell but also have normal cellular functions.8–10 Indeed, some conformers of αsynO-β do not seed pathology and are non-toxic.11–13 Functional endogenous oligomers have been controversial, as their existence has been both confirmed and refuted by carefully executed studies.8,14,15
Are there benign αsyn oligomers that have normal cellular functions, and if so, how do they transition to toxic αsynO-β? Here, in this short review, we discuss how lipid–αsyn interactions might help explain the observation of apparent endogenous non-toxic oligomers and highlight alternative models that are monomer-centric. Furthermore, we will extend this viewpoint to consider its implications for synucleinopathy pathogenesis. There has been substantial work done in this area and several exhaustive reviews on lipid–αsyn interactions16–21 and oligomerization22,23 are available; hence, for the sake of clarity, we will not comprehensively discuss the literature.
Biology of lipids in neurodegenerative disease
The brain is ~60% lipids by weight.24 Lipids have diverse cellular functions in biology including cell signaling, energy storage, and structural partitioning.25 Phospholipids contain amphipathic characteristics with a charged hydrophilic phosphate group and a carbon chain of varying lengths.25 Phospholipids spontaneously form bilayer structures in aqueous solutions that are the basis of cellular membranes. Lipids have not been as extensively studied as proteins in vivo, possibly because of their hydrophobicity, chemical complexity, and the fact that they are not gene products.25 However, lipids are crucial for cellular function and are implicated in several neurodegenerative diseases including synulceinopathies.26 Recent technological advances with lipodomic analysis have furthered the study of lipids.27–30 Current lipodomic analyses, however, are focused on whole-cell lysates and therefore insensitive to cellular spatial and temporal dimensions, which are crucial for understanding lipid function.25
αSyn–vesicle membrane interactions
Shortly following the discovery of αsyn in Lewy pathology,31 the lipid-binding properties of asyn were documented and the significance of disease-causing point mutations in lipid-binding domains was recognized.32 Indeed, one of the earliest histochemical descriptions of Lewy bodies noted that they stain positively for phospholipids, particularly sphingomyelin.33 Since then, interactions between αsyn and vesicle lipids have been implicated in the initial generation of synucleinopathy.16–19,34–36 The hypothesis that lipids control pathological αsyn aggregation primarily stems from observations that lipids/vesicles influence aggregation kinetics in vitro,34,37–40 and that disease-related missense mutations of SNCA alter residues within the N-terminal lipid-binding domain of αsyn.41–46 αSyn may redistribute to lipid compartments early in disease pathogenesis.36 Several disease-causing αsyn mutants abnormally associate with intracellular vesicles and lipid droplets,47,48 and dyshomeostasis of intracellular lipids are likely an early molecular event preceding pathology formation.49 The key to pathogenesis lies within the lipid-binding domain of αsyn.
αSyn binding to vesicular membranes is important, because it influences oligomerization and pathological aggregation. Evidence suggests that non-pathological αsyn is involved with vesicular dynamics in cells9,18,50–55 and regulation of the presynaptic vesicle pool.56,57 αSyn–lipid interactions may have a vesicle tethering function. It has been proposed that the broken α-helical N-terminus can function to tether intracellular vesicles via a “double-anchor” mechanism.58–61 The biological significance of αsyn-mediated clustering is unknown; however, it could serve to promote the exchange of lipids between adjacent vesicles62 and possibly promote vesicle fusion.56–58,62–64 αSyn preferentially binds to membranes with lipid-packing defects65–68 and high curvature.69–72 In the neurons, αsyn is densely clustered around intracellular vesicles and vesicular tubule structures, most prominently at the nerve terminal.73 When incubated with small (~10–30 nm) unilamaller vesicles, the N-terminal of αsyn adopts an extended α-helical conformation as it coats the vesicular surface and a broken α-helical conformation when interacting with micelles.59,74–80 The interaction between the N-terminus of αsyn with lipid membranes is driven by electrostatic interactions between positively charged residues and lipid phosphate head group.81 When membrane bound, the N-terminus residues (1–26) of αsyn rigidly bind to the membrane and the internal segment (residues 26–97) acts to sense lipid properties and regulates binding affinity.82 Interestingly, the hydrophobic stretch of residues 71–82 are required for pathological aggregation of αsyn83 and, therefore, lipid-sensing properties of αsyn and pathological aggregation occur through the same functional domain. It is not clear whether mutation of the N-terminus results in a toxic gain of function or loss of function.
Many cellular functions have been attributed to αsyn and membrane interactions, including soluble N‐ethylmaleimide sensitive factor attachment protein receptor (SNARE) complex assembly and exocytosis; however, the exact cellular function of αsyn remains unclear.9,50,84 αSyn interacts with SNARE proteins at the vesicle surface.85–88 αSyn binding to membranes promotes SNARE complex formation and may function as a SNARE chaperone protein.9,88,89 Vesicular membrane-binding promotes the oligomerization of αsyn.9 In vitro phospholipids can also increase the rate of pathological aggregation (i.e., β-sheet confirmations) by decreasing lag time of primary nucleation.37,90 The effect of lipids on αsyn aggregation is dependent on lipid to protein ratio, with a low ratio promoting aggregation and higher ratio being inhibitory.74,91 This bimodal phenomenon probably results from a lack of monomer available for oligomer elongation when the lipid ratio is too high. Interestingly, increasing αsyn expression, presumably shifting the intracellular lipid to protein ratio, promotes aggregation of αsyn in cells. Notably, it has been hypothesized that reducing monomeric αsyn is an important therapeutic target.92–94
A confusing aspect to the literature is that binding of αsyn to membranes has been reported to both inhibit95–97 and to promote αsyn aggregation.39,47 This may be due to differences in assay conditions between studies, such as membrane lipid composition and αsyn concentration. Indeed, recent studies using lipodomics implicated specific fatty acid oleic acid in the pathogenesis of Parkinson’s disease.49 In the model proposed by Fanning and colleagues49, soluble αsyn binds to oleic acid, effectively sequestering the monomer to lipid membranes and ultimately culminating in pathological aggregate formation. As they also observed an increase in oleic acid in response to αsyn overexpression, there may be a toxic lipid dyshomeostatis that preceeds aggregate formation. Their results suggest a complex origin of synucleinopathy where both lipid metabolism and αsyn are central players.
αSyn may have a more generalized cellular function as an effector of lipid dynamics, and not as a factor of a specific subprocess or pathway. To highlight this concept, consider the curious relationship between αsyn and erythropoiesis (i.e., red blood cell differentiation) for which others have hypothesized αsyn that may have an underlying redundant mechanism in the two cells of different linage.98 αSyn is highly expressed in erythrocytes under the control of transcription factor GATA1.99,100 During the terminal step of erythropoiesis, α-syn expression dramatically increases and remains elevated in the mature erythrocyte.98 αSyn is then found associated with phospholipids and vesicle membranes in the mature erythrocyte.101 Thus, which of the proposed cellular functions does αsyn perform during erythropoiesis? One likely explanation is that αsyn plays a role in the dramatic intracellular lipid organization, analogous to asymmetric cytokinesis, which occurs prior to the phenomenon of enucleation. Enucleation is the process by which organelles are condensed and extruded from the cell to form a mature erythrocyte. Indeed, just prior to enucleation αsyn can be found associated with lipids of the cell, particularly the nucleus and ER, which are key players in enucleation. αSyn accumulates at the site of nuclear extrusion,102 suggesting it is directly involved with enucleation lipid dynamics. Concurrently, SNARE machinery is decreased in the erythrocyte, suggesting that the potential involvement of αsyn in lipid dynamics during enucleation is independent of hypothesized SNARE functions.103 However, if αsyn is involved in this cellular phenomenon, it is non-essential or interchangeable with beta or gamma synucleins, as only minor phenotypic abnormalities of erythrocytes are observed in α-syn-knockout models.99
Soluble oligomers devoid of lipid
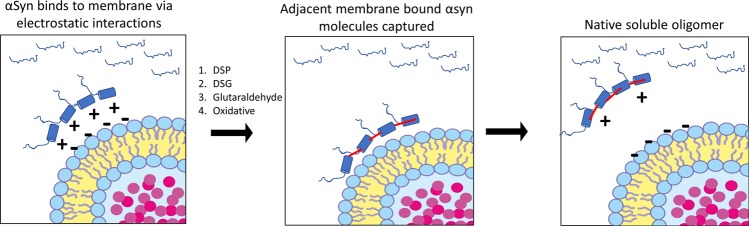
There is good evidence of a naturally occurring metastable soluble αsyn oligomer (i.e., tetramer) that is devoid of vesicle/lipid binding.8 However, the existence of a soluble αsyn tetramer is based mostly on results from crosslinking experiments.8,48,104–106 The interpretation of crosslinking experiments is non-trivial. αSyn tetramers are captured when using a permissive chemical cross-linker with spacer arm length (DSG spacer arm length 7.7 Å) and perhaps not with a shorter spacer arm (formalin spacer arm length ~2 Å).107 A milieu of progressively larger oligomers are formed and captured even when purified recombinant αsyn is incubated with glutaraldehyde.108 The successful detection of an αsyn tetramer in tissues and cells is dependent on sample preparation conditions and can be detected when cells remain intact prior to crosslinking or when tissue lysates are kept highly concentrated.107 Indeed, purification of αsyn prevents the detection of a soluble tetramer further suggesting a cofactor is required and this factor is likely of lipid origin.109 Although the question remains which lipid cofactor might be responsible for the tetramer formation, the tetramer and αsyn–lipid interactions are inextricably linked. This is highlighted when recently a transgenic mouse model (called “3K”) of tetramer deficiency was generated by introducing 3E– > K mutations in αsyn’s lipid-binding N-terminus.48 These 3K mice exhibit aggressive αsyn aggregation, loss of an apparent tetramer, and a motor phenotype that has some semblance to Parkinson’s disease. The lipid-binding domain was mutated in the 3K mice and correspondingly lipid interactions were enhanced48 and similar to what was observed with similar mutations in cells.110 In both mice and cells, mutated 3K αsyn clustered around vesicles and intact tissue crosslinking captured less soluble tetramer.48,106,110 Was this due to less tetramer or alternatively less soluble tetramer? The results could be explained either way, but if the captured αsyn species is truly an insoluble tetramer, one would expect less detection in the soluble fraction, as the authors observed. Indeed, the results appear to fit a scenario where folding on the vesicular membrane is driving αsyn pathology without the need for a soluble tetramer. (Fig. 1)
Fig. 1.
Endogenous soluble oligomers are inextricably associated with lipid/vesicle binding. Depicted is an possible explanation for the detection of a soluble αsyn oligomer. In the cytoplasm, αsyn exists in an equilibrium between a disordered slightly compact monomer and membrane-bound α-helix confirmation. The N-terminus of αsyn binds to vesicle membranes via electrostatic interactions and adopts an α-helix structure. αSyn most likely binds to localized areas of vesicle surfaces with lipid-packing defects. Normally, in the cell ~5–10% of αsyn is interacting with vesicle surfaces. The same percentage is also proposed for soluble oligomers. Covalent bonds between adjacent αsyn molecules capture the confirmations bound to the vesicle surface. Covalent modification of amino-acid residue side chains, especially lysine, following chemical crosslinking neutralizes a portion of αsyn charge required for membrane binding. The captured species could then retain the membrane-bound confirmation and enter the aqueous phase for subsequent detection. Thus, endogenous soluble functional oligomers are unlikely, in agreement with several studies. Instead, endogenous oligomers may represent confirmations of membrane-bound αsyn. This hypothesis makes lipid-syn interactions at the membrane a crucial mediator of pathology initiation. DSP dithiobis(succinimidyl propionate), DSG disuccinimidyl glutarate
Detection of endogenous oligomers, including the tetramer, could be explained by compartmentalized αsyn residing on the vesical membrane (Fig. 1). Membrane interactions occur through electrostatic forces between positively charged lysine residues of αsyn and negatively charge phosphate group of lipids.41,75,81,111 Interestingly, the same crosslinking chemicals used to capture tetramers chemically modify lysine side chains of αsyn and neutralize their charge.112 Chemically modifying the lysine side chains during tissue crosslinking would presumably disrupt membrane binding, because it neutralizes the required electrostatic charge of lysine residues. Therefore, captured oligomers would dissociate from the membrane and would be detected in the soluble fraction, producing the characteristic gel-shift of the αsyn tetramer.106 To highlight this concept, the neutralization of αsyn charge by chemical cross-linkers is routinely used to enhance the retention of αsyn on polyvinylidene difluoride membranes during western blotting protocols.112 Together, adjacent αsyn molecules bound to intracellular vesicle surfaces (i.e., compartmentalized) might disassociate into the soluble fraction once chemically modified by the crosslinking reagent. This phenomenon would also help explain why the soluble tetramer has similar intermolecular n-terminal structure as the membrane-bound form.
The apparent soluble tetramer may be stabilized by covalent bonds formed in the oxidative environment of the erythrocyte (i.e., the source from which it was originally isolated). Biochemical characterization of a putative αsyn tetramer was mostly done using erythrocyte derived αsyn.8 Erythrocytes have millimolar concentrations of hemoglobin. Hemoglobin oxidatively catalyzes the formation of intramolecular dityrosine bonds resulting in a mixture of αsyn dimers and tetramers.113 Dityrosine crosslink formation occurs rapidly113,114 and would likely occur to some extent during αsyn purification from erythrocytes. αSyn in erythrocytes associates with vesicles101,102 and stable dityrosine αsyn occurs in clinical blood samples.115 Together, it is probable that stable αsyn oligomers isolated from erythrocytes are due to oxidative crosslinking of adjacent αsyn molecules bound to vesicle membranes. Heat denaturation irreversibly abolished the tetramers α-helix structure, indicating that the captured configuration was not in equilibrium but instead was a stabilized structure originating from the tissue (i.e., vesicle bound). Lipid binding of the tetramer was enhanced when compared with the monomer, further suggesting it retained a lipid-binding confirmation.8 Removal of lipids with Lipodex 1000 did not affect the tetramer detection, suggesting the tetramer was not associated with any stabilizing lipid structure. Stabilization of small oligomers via oxidative crosslinking can prevent progressive aggregation and might explain why the stable tetramer appears to resist aggregation.8,116 Together, it is likely to be that the stable soluble αsyn tetramer purified from erythrocyte is a covalently stabilized membrane-bound confirmation similar to that captured using exogenous crosslinking agents.
Soluble αsyn oligomers have been detected using several imaging techniques. Förster resonance energy transfer (FRET) is a powerful technique used to determine intermolecular distances between molecules with 1–2 nm spatial resolution.117 FRET has been employed to study various aspects of αsyn oligomerization mostly in vitro9,77,118–120 but also ex vivo121 and in vivo.122 In vitro, purified αsyn forms distinct oligomer conformers, which then can spontaneously convert to protease resistant and toxic αsynO-β.12 Biomolecular fluorescence complementation (BiFC) technique uses fluorescent constructs to determine protein–protein interaction. BiFC constructs have been used to study αsyn aggregation in vivo;123,124 however, the resolution of this technique cannot differentiate between small oligomers and complex formation (i.e., membrane bound). The method detects diffuse staining in neurons lacking pathology, suggesting either small aggregates or close association of αsyn molecules normally within the cytosol.124 αSyn comes into close proximity around synaptic vesicles and possibly forms multimers on the membrane.15 Other BiFC techniques employing photoactivatable fluorescent molecules can increase the spatial resolution to several nanometers,125 but this type of imaging has yet to be done with αsyn.
Soluble disordered monomer devoid of lipid
There is also good evidence that αsyn exists predominantly as an intrinsically disordered monomer in the cytosol.10,14,126–130 αSyn purified from Escherichia coli behaves as an intrinsically disordered protein with a large stokes radius,129 which may be why monomeric αsyn appears to have greater mass in some assays.126 Non-denaturing purification procedures from several tissue sources also produce a disordered monomeric αsyn.126 A disordered soluble monomer has been observed directly using in-cell nuclear magnetic resonance (NMR) imaging techniques.14 Specifically, investigators transfected cells with recombinant αsyn labeled with 15N isotope to monitor individual αsyn molecules within the living cells. Results showed that the majority of monomeric αsyn maintained a disordered confirmation in the cell, while becoming slightly more compact than in free solution, probably due to molecular crowding.14 The compact structure observed in vivo likely prevents spontaneous aggregation in the cytosol.131 Although this is compelling evidence that the majority of αsyn in the cell occurs as a disordered monomer, the result does not rule out the existence of a tetramer. A tetramer that existed at low concentration would not be detected and it is possible that the recombinant αsyn behaved dissimilarly to endogenous αsyn. Importantly, this study demonstrated that the majority of αsyn in the cell is cytosolic and monomeric, and suggests that membrane interactions are likely transient and highly dependent on local environment (e.g., nerve terminal). Correspondingly, it would be interesting if αsyn persists as a monomer at axon terminals where it’s vesicle interactions are more prominent than in the cell body.73,132 The α-helix conformation αsyn was recently described in HELA cells using FRET, where it was demonstrated that αsyn assumes several confirmations when interacting with vesicle surfaces.133 Considered together, the majority of αsyn in the cell exists as a relatively compact disordered monomer and adopts an α-helix structure when interacting with vesicle membranes. The native state of αsyn may not include an oligomer, whether free and soluble, or vesicle bound.
Aberrant vesicle binding progresses to pathology
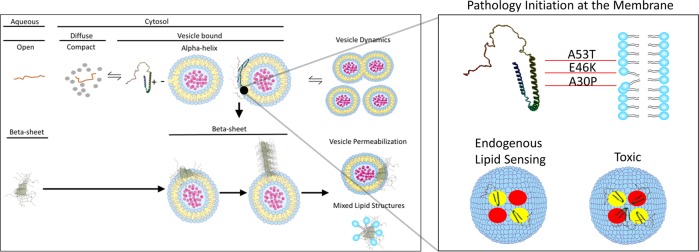
Assuming monomeric αsyn is interacting with vesicle membranes, and remains monomeric at the vesicle surface under normal circumstances, how might pathology begin? (Fig. 2). One possible scenario involves vesicle surfaces acting as two-dimensional (2D) reactors that promote pathogenic intermolecular interactions of αsyn.91,134–136 In the cystosol, αsyn remains monomeric and in a slightly compact configuration. Transient interactions with vesicle surfaces induce a conformational shift, but not necessarily oligomerization, and concentrate αsyn molecules on the vesicle surface. This focal point on the vesicle surface is where opposing αsyn molecules bind and might serve as the molecular origins for Lewy pathology. Numerous cellular and genetic factors converge at this focal point in such a way that creates an environment conducive for the initiation of pathogenic αsyn aggregation. Studies using sonicated αsyn PFFs suggest that once the αsynO-β is present, progressive aggregation and toxicity follow.7,137 Yet, studies that utilize PFF’s to assess pathology are bypassing pathology generation and may be recapitulating downstream pathological events. Therefore, the use of PFF’s to study synucleinopathy is likely to give valuable insight into the progression of these diseases and perhaps are not suitable to study the initiation of the disease.
Fig. 2.
Potential role of lipids in αsyn aggregate pathoetiology. In the cell, αsyn is partitioned between aqueous phase and the lipid phase via transient interactions at the vesicle surface. Endogenous αsyn probably exists in several states, including a compact monomer and a vesicle-bound monomer with an N-terminal α-helix structure. Folding αsyn monomers on the vesicle surfaces likely plays a non-essential or redundant role in vesicle dynamics. β-Sheet confirmation of αsyn may begin at vesicle surfaces. Toxic effects of β-sheet oligomers included vesicle permeabilization or the formation of toxic mixed lipid–protein structures. Pathology initiation might involve specific configurations of αsyn folding onto a variety of membranes. Altered lipid-sensing properties by known disease-causing mutations (e.g., A30P, E46K, and A53T) might alter the affinity of αsyn for certain vesicle lipid components (depicted as yellow and red circles), or change the spatial arrangement of αsyn molecules on the vesicle surface. Resulting β-sheet oligomers may have different toxic or prion-like properties based the physiochemical details of the initial pathology development
At the membrane, αsynO-β might act similar to a “molecular shovel” inserting itself into the membrane with destructive, toxic, consequences.2,138 Together with lipid/vesicle interactions at the center of αsyn function, a route to pathophysiology might be the collapse of clustered lipids/vesicles into a pathological inclusion. Similar to a massive star transitioning to a black hole, at some point pathological αsyn and lipids form a critically dense structure, and compact to form a Lewy body. Interestingly, the architecture of the Lewy pathology supports this interpretation.139–144 Neuropathological examination of patient brains shows a mixture of αsyn staining in neurons that consist of a pale diffuse, punctate irregular shape (i.e., uneven distribution), discrete body (i.e., pale body), and a massive dense structure with a pale core (i.e., Lewy body).139 These structures have been hypothesized to be snapshots of a pathological process with Lewy bodies being the result. Indeed, pale bodies contain a mixture of granular and vesicular structures and are often found near mature LB.141,145 Using a lipid centric view, punctate irregular “early” pathology might represent the initial vesicle clustering48 or lipid droplet formation47 before the characteristic pathology develops. Overexpression of αsyn in yeast models produces lipid only inclusions, lacking the filamentous αsyn that is the hallmark of synucleinopathies.146 Lipids have been identified as a core component of Lewy pathology33,147,148 but this has largely been ignored and the pathology is often considered “proteinaceous.”
Recent work by Shahmoradian and colleagues149 provided substantial evidence that Lewy pathology consists of compacted lipid components from a variety of organelles with αsyn oligomers interspersed. Their work strongly suggests that Lewy pathology is actually an inclusion of fragmented lipids, for which αsyn–lipid interactions play a causative role. Ultrastructural characterization of Lewy pathology showed tubule vesicular, fragmented membranous, and mixed lipid–protein structures, all of which can be formed from αsyn interactions with vesicle membranes. Electron dense structures, consistent with lysosomes, were also observed throughout Lewy pathology.149 Lysosomes are central mediators of lipid metabolism150 and the conspicuous presence of lysosomes surrounded by fragmented membrane structures strongly suggests a deficit in lysosomal/autophagic pathways, specifically the removal of lipid membranes. Large-scale genome-wide association studies have implicated lysosomal/autophagy pathway in several neurodegerative diseases, including synucleinopathies.151,152
A lipid-centric view of Lewy pathology is transformative in that it helps unify and identify disease-causing pathology of several molecular origins. Several neurodegenerative diseases are currently characterized by protein aggregation, when instead we may be missing the lipid components that are the core of the pathology. For example, clinical cases resembling synucleinopathies are documented without the presence of Lewy pathology (e.g., Parkin mutations with early-onset Parkinson’s disease), as measured by αsyn staining.153 The presence of lipid inclusions in the absence of αsyn are not generally considered when examining patient tissues.
Determining αsyn–lipids interactions in living cells
αSyn interactions with lipids and vesicles has been investigated mostly in vitro and needs to be characterized in living cells. There are several promising strategies to start understanding lipid–αsyn interactions. The first strategy uses synthetic bifunctional lipids to directly determine lipid–protein interactions.154,155 This strategy offers flexibility with analysis and offers unambiguous evidence of direct αsyn–lipid interactions in vivo. Captured lipid–αsyn molecules can be subsequently labeled or purified for downstream analysis. Labeling the structures will help determine where αsyn–lipid interactions are most relevant in the cell. Purification of the structures with subsequent analysis by liquid chromatography–mass spectrometry could determine specific αsyn proteoforms involved with pathological lipid interactions, as well as global analysis of other proteins that are involved. However, the drawback to this strategy is the investigator can only assess one specific lipid species at a time and a synthetic bifunctional lipid must be available or developed for application. Recently, a bifunctional analog of glucosylceramide, a lipid implicated in synucleinopathy,156 has become commercially available and could aid in these studies.
A shotgun lipidomic analysis may also be useful, but because of the complexity of whole-cell lipid determination, the data may not give insight into the localized αsyn–lipid interactions that precede pathology formation. Recently, a shotgun lipodomic analysis was conducted on various αsyn mutant models and αsyn was found to have an effect on lipid metabolism.49 However, it is difficult to draw distinct conclusions or find drug targets based on the description of a total lipid species. The resulting information is most useful in implicating lipid metabolism or catabolism pathways, and not the characterization of the specific localized lipids that may be involved with initiating pathology. To find a disease-relevant target, a focused lipodomic approach looking at specific organelles, or better yet, early Lewy pathology, will be the most illuminating. Lipodomic arrays can also be used to screen many lipid–protein interactions; however, they have the disadvantage of not representing in vivo binding conditions.
A key question remains: at what point during its interaction with cytoplasmic membranes and extracellular vesicles does αsyn adopt a pathological confirmation? To answer this question, one needs to consider the membrane as a chemical reactor favoring molecular encounters.134 This is the consequence that restrains monomeric or low-molecular-weight oligomeric αsyn diffusion from a three-dimensional to a 2D space upon interaction with the plasma membrane or extracellular vesicles plane.
Conclusions
Evidence for a soluble αsyn oligomer might be best explained by folding intermediates on the plasma or vesicle membranes that remain soluble for subsequent extraction and detection. This interpretation does not require a soluble functional oligomer and seems to fit much of the experimental data. The distinction between a soluble native oligomer and vesicle-bound oligomers/folding intermediates is important, because it clarifies the origins of pathological aggregation of αsyn. With this perspective, determining the molecular details of αsyn–vesicle/lipid interactions is important for understanding the endogenous origins of synucleinopathy. Although there is consensus that aggregation of αsyn is associated with neurological disease, the precise molecular origin of the aggregate pathology remains a mystery.
Author contributions
B.A.K. and J.H.K. conceived and prepared the manuscript. R.M. and P.B. provided valuable discussion, as well as reviewed and edited the manuscript.
Competing interests
P.B. has received commercial support as a consultant from Axial Biotherapeutics, CuraSen, Fujifilm-Cellular Dynamics International, IOS Press Partners, LifeSci Capital, and Living Cell Technologies Ltd. He has received commercial support for grants/research from Lundbeck A/S and Roche. He has ownership interests in Acousort AB and Axial Biotherapeutics and is on the steering committee of the NILO-PD trial. J.H.K. has received commercial support as a consultant from Cellular Dynamics International, Inc., Michael J. Fox Foundation, Abbvie, Exicure, NSGENE, Guidepoint, Inhibikhase, Axovant, and Seelos B.A.K. and R.M. have no competing interests to disclose.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McCann H, Stevens CH, Cartwright H, Halliday GM. Alpha-synucleinopathy phenotypes. Parkinsonism Relat. Disord. 2014;20:S62–S67. doi: 10.1016/S1353-8020(13)70017-8. [DOI] [PubMed] [Google Scholar]
- 2.Fusco G, et al. Structural basis of membrane disruption and cellular toxicity by alpha-synuclein oligomers. Science. 2017;358:1440–1443. doi: 10.1126/science.aan6160. [DOI] [PubMed] [Google Scholar]
- 3.Froula JM, et al. Defining alpha-synuclein species responsible for Parkinson disease phenotypes in mice. J. Biol. Chem. 2019 doi: 10.1074/jbc.RA119.007743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thakur P, et al. Modeling Parkinson’s disease pathology by combination of fibril seeds and alpha-synuclein overexpression in the rat brain. Proc. Natl Acad. Sci. USA. 2017;114:E8284–E8293. doi: 10.1073/pnas.1710442114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luk KC, et al. Exogenous alpha-synuclein fibrils seed the formation of Lewy body-like intracellular inclusions in cultured cells. Proc. Natl Acad. Sci. USA. 2009;106:20051–20056. doi: 10.1073/pnas.0908005106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Volpicelli-Daley LA, et al. Exogenous alpha-synuclein fibrils induce Lewy body pathology leading to synaptic dysfunction and neuron death. Neuron. 2011;72:57–71. doi: 10.1016/j.neuron.2011.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luk KC, et al. Intracerebral inoculation of pathological alpha-synuclein initiates a rapidly progressive neurodegenerative alpha-synucleinopathy in mice. J. Exp. Med. 2012;209:975–986. doi: 10.1084/jem.20112457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bartels T, Choi JG, Selkoe DJ. Alpha-synuclein occurs physiologically as a helically folded tetramer that resists aggregation. Nature. 2011;477:107–110. doi: 10.1038/nature10324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burre J, Sharma M, Sudhof TC. Alpha-synuclein assembles into higher-order multimers upon membrane binding to promote SNARE complex formation. Proc. Natl Acad. Sci. USA. 2014;111:E4274–4283. doi: 10.1073/pnas.1416598111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burre J, et al. Properties of native brain alpha-synuclein. Nature. 2013;498:E4–E6. doi: 10.1038/nature12125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winner B, et al. In vivo demonstration that alpha-synuclein oligomers are toxic. Proc. Natl Acad. Sci. USA. 2011;108:4194–4199. doi: 10.1073/pnas.1100976108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cremades N, et al. Direct observation of the interconversion of normal and toxic forms of alpha-synuclein. Cell. 2012;149:1048–1059. doi: 10.1016/j.cell.2012.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forloni G, Artuso V, La Vitola P, Balducci C. Oligomeropathies and pathogenesis of Alzheimer and Parkinson’s diseases. Mov. Disord. 2016;31:771–781. doi: 10.1002/mds.26624. [DOI] [PubMed] [Google Scholar]
- 14.Theillet FX, et al. Structural disorder of monomeric alpha-synuclein persists in mammalian cells. Nature. 2016;530:45–50. doi: 10.1038/nature16531. [DOI] [PubMed] [Google Scholar]
- 15.Wang L, et al. alpha-synuclein multimers cluster synaptic vesicles and attenuate recycling. Curr. Biol. 2014;24:2319–2326. doi: 10.1016/j.cub.2014.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Galvagnion C. The role of lipids interacting with alpha-synuclein in the pathogenesis of Parkinson’s disease. J. Parkinsons Dis. 2017;7:433–450. doi: 10.3233/JPD-171103. [DOI] [PubMed] [Google Scholar]
- 17.Suzuki M, Sango K, Wada K, Nagai Y. Pathological role of lipid interaction with alpha-synuclein in Parkinson’s disease. Neurochem. Int. 2018;119:97–106. doi: 10.1016/j.neuint.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 18.Snead D, Eliezer D. Alpha-synuclein function and dysfunction on cellular membranes. Exp. Neurobiol. 2014;23:292–313. doi: 10.5607/en.2014.23.4.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alza NP, Iglesias Gonzalez PA, Conde MA, Uranga RM, Salvador GA. Lipids at the crossroad of alpha-synuclein function and dysfunction: biological and pathological implications. Front. Cell. Neurosci. 2019;13:175. doi: 10.3389/fncel.2019.00175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Leary EI, Lee JC. Interplay between alpha-synuclein amyloid formation and membrane structure. Biochimica et biophysica acta. Biochim. Biphys. Acta Proteins Proteom. 2019;1867:483–491. doi: 10.1016/j.bbapap.2018.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alecu I, Bennett SAL. Dysregulated lipid metabolism and its role in alpha-synucleinopathy in Parkinson’s disease. Front. Neurosci. 2019;13:328. doi: 10.3389/fnins.2019.00328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bengoa-Vergniory N, Roberts RF, Wade-Martins R, Alegre-Abarrategui J. Alpha-synuclein oligomers: a new hope. Acta Neuropathol. 2017;134:819–838. doi: 10.1007/s00401-017-1755-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lashuel HA, Overk CR, Oueslati A, Masliah E. The many faces of alpha-synuclein: from structure and toxicity to therapeutic target. Nat. Rev. Neurosci. 2013;14:38–48. doi: 10.1038/nrn3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Brien JS, Sampson EL. Lipid composition of the normal human brain: gray matter, white matter, and myelin. J. Lipid Res. 1965;6:537–544. [PubMed] [Google Scholar]
- 25.Muro E, Atilla-Gokcumen GE, Eggert US. Lipids in cell biology: how can we understand them better? Mol. Biol. Cell. 2014;25:1819–1823. doi: 10.1091/mbc.e13-09-0516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adibhatla RM, Hatcher JF. Role of lipids in brain injury and diseases. Future Lipidol. 2007;2:403–422. doi: 10.2217/17460875.2.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brugger B. Lipidomics: analysis of the lipid composition of cells and subcellular organelles by electrospray ionization mass spectrometry. Annu. Rev. Biochem. 2014;83:79–98. doi: 10.1146/annurev-biochem-060713-035324. [DOI] [PubMed] [Google Scholar]
- 28.Lydic TA, Goo YH. Lipidomics unveils the complexity of the lipidome in metabolic diseases. Clin. Transl. Med. 2018;7:4. doi: 10.1186/s40169-018-0182-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang K, Han X. Lipidomics: techniques, applications, and outcomes related to biomedical sciences. Trends Biochem. Sci. 2016;41:954–969. doi: 10.1016/j.tibs.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saliba AE, Vonkova I, Gavin AC. The systematic analysis of protein-lipid interactions comes of age. Nat. Rev. Mol. Cell Biol. 2015;16:753–761. doi: 10.1038/nrm4080. [DOI] [PubMed] [Google Scholar]
- 31.Spillantini MG, et al. Alpha-synuclein in Lewy bodies. Nature. 1997;388:839–840. doi: 10.1038/42166. [DOI] [PubMed] [Google Scholar]
- 32.Jensen PH, Nielsen MS, Jakes R, Dotti CG, Goedert M. Binding of alpha-synuclein to brain vesicles is abolished by familial Parkinson’s disease mutation. J. Biol. Chem. 1998;273:26292–26294. doi: 10.1074/jbc.273.41.26292. [DOI] [PubMed] [Google Scholar]
- 33.den Jager WA. Sphingomyelin in Lewy inclusion bodies in Parkinson’s disease. Arch. Neurol. 1969;21:615–619. doi: 10.1001/archneur.1969.00480180071006. [DOI] [PubMed] [Google Scholar]
- 34.Burre J, Sharma M, Sudhof TC. Definition of a molecular pathway mediating alpha-synuclein neurotoxicity. J. Neurosci. 2015;35:5221–5232. doi: 10.1523/JNEUROSCI.4650-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kramer ML, Schulz-Schaeffer WJ. Presynaptic alpha-synuclein aggregates, not Lewy bodies, cause neurodegeneration in dementia with Lewy bodies. J. Neurosci. 2007;27:1405–1410. doi: 10.1523/JNEUROSCI.4564-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Halliday GM, et al. Alpha-synuclein redistributes to neuromelanin lipid in the substantia nigra early in Parkinson’s disease. Brain. 2005;128:2654–2664. doi: 10.1093/brain/awh584. [DOI] [PubMed] [Google Scholar]
- 37.Galvagnion C, et al. Lipid vesicles trigger alpha-synuclein aggregation by stimulating primary nucleation. Nat. Chem. Biol. 2015;11:229–234. doi: 10.1038/nchembio.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhu M, Li J, Fink AL. The association of alpha-synuclein with membranes affects bilayer structure, stability, and fibril formation. J. Biol. Chem. 2003;278:40186–40197. doi: 10.1074/jbc.M305326200. [DOI] [PubMed] [Google Scholar]
- 39.Lee HJ, Choi C, Lee SJ. Membrane-bound alpha-synuclein has a high aggregation propensity and the ability to seed the aggregation of the cytosolic form. J. Biol. Chem. 2002;277:671–678. doi: 10.1074/jbc.M107045200. [DOI] [PubMed] [Google Scholar]
- 40.Grey M, et al. Acceleration of alpha-synuclein aggregation by exosomes. J. Biol. Chem. 2015;290:2969–2982. doi: 10.1074/jbc.M114.585703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jo E, Fuller N, Rand RPSt, George-Hyslop P, Fraser PE. Defective membrane interactions of familial Parkinson’s disease mutant A30P alpha-synuclein. J. Mol. Biol. 2002;315:799–807. doi: 10.1006/jmbi.2001.5269. [DOI] [PubMed] [Google Scholar]
- 42.Fares MB, et al. The novel Parkinson’s disease linked mutation G51D attenuates in vitro aggregation and membrane binding of alpha-synuclein, and enhances its secretion and nuclear localization in cells. Hum. Mol. Genet. 2014;23:4491–4509. doi: 10.1093/hmg/ddu165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ghosh D, et al. The newly discovered Parkinson’s disease associated Finnish mutation (A53E) attenuates alpha-synuclein aggregation and membrane binding. Biochem. 2014;53:6419–6421. doi: 10.1021/bi5010365. [DOI] [PubMed] [Google Scholar]
- 44.Robotta M, Cattani J, Martins JC, Subramaniam V, Drescher M. Alpha-synuclein disease mutations are structurally defective and locally affect membrane binding. J. Am. Chem. Soc. 2017;139:4254–4257. doi: 10.1021/jacs.6b05335. [DOI] [PubMed] [Google Scholar]
- 45.Kara E, et al. alpha-Synuclein mutations cluster around a putative protein loop. Neurosci. Lett. 2013;546:67–70. doi: 10.1016/j.neulet.2013.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Flagmeier P, et al. Mutations associated with familial Parkinson’s disease alter the initiation and amplification steps of alpha-synuclein aggregation. Proc. Natl Acad. Sci. USA. 2016;113:10328–10333. doi: 10.1073/pnas.1604645113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cole NB, et al. Lipid droplet binding and oligomerization properties of the Parkinson’s disease protein alpha-synuclein. J. Biol. Chem. 2002;277:6344–6352. doi: 10.1074/jbc.M108414200. [DOI] [PubMed] [Google Scholar]
- 48.Nuber S, et al. Abrogating native alpha-synuclein tetramers in mice causes a L-DOPA-responsive motor syndrome closely resembling Parkinson’s disease. Neuron. 2018;100:75–90 e75. doi: 10.1016/j.neuron.2018.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fanning S, et al. Lipidomic analysis of alpha-synuclein neurotoxicity identifies stearoyl CoA desaturase as a target for Parkinson treatment. Mol. Cell. 2019;73:1001–1014 e1008. doi: 10.1016/j.molcel.2018.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Burre J. The synaptic function of alpha-synuclein. J. Parkinsons Dis. 2015;5:699–713. doi: 10.3233/JPD-150642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Scott D, Roy S. alpha-Synuclein inhibits intersynaptic vesicle mobility and maintains recycling-pool homeostasis. J. Neurosci. 2012;32:10129–10135. doi: 10.1523/JNEUROSCI.0535-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Larsen KE, et al. Alpha-synuclein overexpression in PC12 and chromaffin cells impairs catecholamine release by interfering with a late step in exocytosis. J. Neurosci. 2006;26:11915–11922. doi: 10.1523/JNEUROSCI.3821-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nemani VM, et al. Increased expression of alpha-synuclein reduces neurotransmitter release by inhibiting synaptic vesicle reclustering after endocytosis. Neuron. 2010;65:66–79. doi: 10.1016/j.neuron.2009.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Busch DJ, et al. Acute increase of alpha-synuclein inhibits synaptic vesicle recycling evoked during intense stimulation. Mol. Biol. Cell. 2014;25:3926–3941. doi: 10.1091/mbc.e14-02-0708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lautenschlager J, Kaminski CF, Kaminski Schierle G. S. alpha-synuclein - regulator of exocytosis, endocytosis, or both? Trends Cell Biol. 2017;27:468–479. doi: 10.1016/j.tcb.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 56.Murphy DD, Rueter SM, Trojanowski JQ, Lee VM. Synucleins are developmentally expressed, and alpha-synuclein regulates the size of the presynaptic vesicular pool in primary hippocampal neurons. J. Neurosci. 2000;20:3214–3220. doi: 10.1523/JNEUROSCI.20-09-03214.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cabin DE, et al. Synaptic vesicle depletion correlates with attenuated synaptic responses to prolonged repetitive stimulation in mice lacking alpha-synuclein. J. Neurosci. 2002;22:8797–8807. doi: 10.1523/JNEUROSCI.22-20-08797.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fusco G, et al. Structural basis of synaptic vesicle assembly promoted by alpha-synuclein. Nat. Commun. 2016;7:12563. doi: 10.1038/ncomms12563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Georgieva ER, Ramlall TF, Borbat PP, Freed JH, Eliezer D. Membrane-bound alpha-synuclein forms an extended helix: long-distance pulsed ESR measurements using vesicles, bicelles, and rodlike micelles. J. Am. Chem. Soc. 2008;130:12856–12857. doi: 10.1021/ja804517m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nass, R. a. P., S. Parkinson’s Disease: Molecular and Therapeutic Insights from Model Systems (Elsevier, 2008).
- 61.Georgieva ER, Ramlall TF, Borbat PP, Freed JH, Eliezer D. The lipid-binding domain of wild type and mutant alpha-synuclein: compactness and interconversion between the broken and extended helix forms. J. Biol. Chem. 2010;285:28261–28274. doi: 10.1074/jbc.M110.157214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sharon R, et al. alpha-Synuclein occurs in lipid-rich high molecular weight complexes, binds fatty acids, and shows homology to the fatty acid-binding proteins. Proc. Natl Acad. Sci. USA. 2001;98:9110–9115. doi: 10.1073/pnas.171300598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mesmin B, et al. A four-step cycle driven by PI(4)P hydrolysis directs sterol/PI(4)P exchange by the ER-Golgi tether OSBP. Cell. 2013;155:830–843. doi: 10.1016/j.cell.2013.09.056. [DOI] [PubMed] [Google Scholar]
- 64.Lev S. Non-vesicular lipid transport by lipid-transfer proteins and beyond. Nat. Rev. Mol. Cell Biol. 2010;11:739–750. doi: 10.1038/nrm2971. [DOI] [PubMed] [Google Scholar]
- 65.Ouberai MM, et al. alpha-Synuclein senses lipid packing defects and induces lateral expansion of lipids leading to membrane remodeling. J. Biol. Chem. 2013;288:20883–20895. doi: 10.1074/jbc.M113.478297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Garten M, et al. Methyl-branched lipids promote the membrane adsorption of alpha-synuclein by enhancing shallow lipid-packing defects. Phys. Chem. Chem. Phys. 2015;17:15589–15597. doi: 10.1039/C5CP00244C. [DOI] [PubMed] [Google Scholar]
- 67.Nuscher B, et al. Alpha-synuclein has a high affinity for packing defects in a bilayer membrane: a thermodynamics study. J. Biol. Chem. 2004;279:21966–21975. doi: 10.1074/jbc.M401076200. [DOI] [PubMed] [Google Scholar]
- 68.Kamp F, Beyer K. Binding of alpha-synuclein affects the lipid packing in bilayers of small vesicles. J. Biol. Chem. 2006;281:9251–9259. doi: 10.1074/jbc.M512292200. [DOI] [PubMed] [Google Scholar]
- 69.Middleton ER, Rhoades E. Effects of curvature and composition on alpha-synuclein binding to lipid vesicles. Biophys. J. 2010;99:2279–2288. doi: 10.1016/j.bpj.2010.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pranke IM, et al. alpha-Synuclein and ALPS motifs are membrane curvature sensors whose contrasting chemistry mediates selective vesicle binding. J. Cell Biol. 2011;194:89–103. doi: 10.1083/jcb.201011118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kjaer L, Giehm L, Heimburg T, Otzen D. The influence of vesicle size and composition on alpha-synuclein structure and stability. Biophys. J. 2009;96:2857–2870. doi: 10.1016/j.bpj.2008.12.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.O’Leary EI, Jiang Z, Strub MP, Lee JC. Effects of phosphatidylcholine membrane fluidity on the conformation and aggregation of N-terminally acetylated alpha-synuclein. J. Biol. Chem. 2018;293:11195–11205. doi: 10.1074/jbc.RA118.002780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Boassa D, et al. Mapping the subcellular distribution of alpha-synuclein in neurons using genetically encoded probes for correlated light and electron microscopy: implications for Parkinson’s disease pathogenesis. J. Neurosci. 2013;33:2605–2615. doi: 10.1523/JNEUROSCI.2898-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chandra S, Chen X, Rizo J, Jahn R, Sudhof TC. A broken alpha -helix in folded alpha-synuclein. J. Biol. Chem. 2003;278:15313–15318. doi: 10.1074/jbc.M213128200. [DOI] [PubMed] [Google Scholar]
- 75.Davidson WS, Jonas A, Clayton DF, George JM. Stabilization of alpha-synuclein secondary structure upon binding to synthetic membranes. J. Biol. Chem. 1998;273:9443–9449. doi: 10.1074/jbc.273.16.9443. [DOI] [PubMed] [Google Scholar]
- 76.Hellstrand E, et al. Adsorption of alpha-synuclein to supported lipid bilayers: positioning and role of electrostatics. ACS Chem. Neurosci. 2013;4:1339–1351. doi: 10.1021/cn400066t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ferreon AC, Gambin Y, Lemke EA, Deniz AA. Interplay of alpha-synuclein binding and conformational switching probed by single-molecule fluorescence. Proc. Natl Acad. Sci. USA. 2009;106:5645–5650. doi: 10.1073/pnas.0809232106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Trexler AJ, Rhoades E. Alpha-synuclein binds large unilamellar vesicles as an extended helix. Biochem. 2009;48:2304–2306. doi: 10.1021/bi900114z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jao CC, Hegde BG, Chen J, Haworth IS, Langen R. Structure of membrane-bound alpha-synuclein from site-directed spin labeling and computational refinement. Proc. Natl Acad. Sci. USA. 2008;105:19666–19671. doi: 10.1073/pnas.0807826105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bussell R, Jr., Eliezer D. A structural and functional role for 11-mer repeats in alpha-synuclein and other exchangeable lipid binding proteins. J. Mol. Biol. 2003;329:763–778. doi: 10.1016/S0022-2836(03)00520-5. [DOI] [PubMed] [Google Scholar]
- 81.Jo E, McLaurin J, Yip CMSt, George-Hyslop P, Fraser P. E. alpha-Synuclein membrane interactions and lipid specificity. J. Biol. Chem. 2000;275:34328–34334. doi: 10.1074/jbc.M004345200. [DOI] [PubMed] [Google Scholar]
- 82.Fusco G, et al. Direct observation of the three regions in alpha-synuclein that determine its membrane-bound behaviour. Nat. Commun. 2014;5:3827. doi: 10.1038/ncomms4827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Giasson BI, Murray IV, Trojanowski JQ, Lee VM. A hydrophobic stretch of 12 amino acid residues in the middle of alpha-synuclein is essential for filament assembly. J. Biol. Chem. 2001;276:2380–2386. doi: 10.1074/jbc.M008919200. [DOI] [PubMed] [Google Scholar]
- 84.Logan T, Bendor J, Toupin C, Thorn K, Edwards R. H. alpha-Synuclein promotes dilation of the exocytotic fusion pore. Nat. Neurosci. 2017;20:681–689. doi: 10.1038/nn.4529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Almandoz-Gil L, et al. In situ proximity ligation assay reveals co-localization of alpha-synuclein and SNARE proteins in murine primary neurons. Front. Neurol. 2018;9:180. doi: 10.3389/fneur.2018.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lou X, Kim J, Hawk BJ, Shin Y. K. alpha-Synuclein may cross-bridge v-SNARE and acidic phospholipids to facilitate SNARE-dependent vesicle docking. Biochem. J. 2017;474:2039–2049. doi: 10.1042/BCJ20170200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sun J, et al. Functional cooperation of alpha-synuclein and VAMP2 in synaptic vesicle recycling. Proc. Natl Acad. Sci. USA. 2019 doi: 10.1073/pnas.1903049116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Atias M, et al. Synapsins regulate alpha-synuclein functions. Proc. Natl Acad. Sci. USA. 2019 doi: 10.1073/pnas.1903054116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Burre J, et al. Alpha-synuclein promotes SNARE-complex assembly in vivo and in vitro. Science. 2010;329:1663–1667. doi: 10.1126/science.1195227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gaspar R, Pallbo J, Weininger U, Linse S, Sparr E. Reprint of “Ganglioside lipids accelerate alpha-synuclein amyloid formation”. Biochim. Biophys. Acta Proteins Proteom. 2019;1867:508–518. doi: 10.1016/j.bbapap.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 91.Bodner CR, Dobson CM, Bax A. Multiple tight phospholipid-binding modes of alpha-synuclein revealed by solution NMR spectroscopy. J. Mol. Biol. 2009;390:775–790. doi: 10.1016/j.jmb.2009.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mittal S, et al. beta2-Adrenoreceptor is a regulator of the alpha-synuclein gene driving risk of Parkinson’s disease. Science. 2017;357:891–898. doi: 10.1126/science.aaf3934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chu Y, Dodiya H, Aebischer P, Olanow CW, Kordower JH. Alterations in lysosomal and proteasomal markers in Parkinson’s disease: relationship to alpha-synuclein inclusions. Neurobiol. Dis. 2009;35:385–398. doi: 10.1016/j.nbd.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 94.Chatterjee D, et al. Proteasome-targeted nanobodies alleviate pathology and functional decline in an alpha-synuclein-based Parkinson’s disease model. NPJ Parkinsons Dis. 2018;4:25. doi: 10.1038/s41531-018-0062-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Narayanan V, Scarlata S. Membrane binding and self-association of alpha-synucleins. Biochem. 2001;40:9927–9934. doi: 10.1021/bi002952n. [DOI] [PubMed] [Google Scholar]
- 96.Zhu M, Fink AL. Lipid binding inhibits alpha-synuclein fibril formation. J. Biol. Chem. 2003;278:16873–16877. doi: 10.1074/jbc.M210136200. [DOI] [PubMed] [Google Scholar]
- 97.Jo E, et al. Alpha-synuclein-synaptosomal membrane interactions: implications for fibrillogenesis. Eur. J. Biochem. 2004;271:3180–3189. doi: 10.1111/j.1432-1033.2004.04250.x. [DOI] [PubMed] [Google Scholar]
- 98.Nakai M, et al. Expression of alpha-synuclein, a presynaptic protein implicated in Parkinson’s disease, in erythropoietic lineage. Biochem. Biophys. Res. Commun. 2007;358:104–110. doi: 10.1016/j.bbrc.2007.04.108. [DOI] [PubMed] [Google Scholar]
- 99.Renella R, Schlehe JS, Selkoe DJ, Williams DA, LaVoie MJ. Genetic deletion of the GATA1-regulated protein alpha-synuclein reduces oxidative stress and nitric oxide synthase levels in mature erythrocytes. Am. J. Hematol. 2014;89:974–977. doi: 10.1002/ajh.23796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Scherzer CR, et al. GATA transcription factors directly regulate the Parkinson’s disease-linked gene alpha-synuclein. Proc. Natl Acad. Sci. USA. 2008;105:10907–10912. doi: 10.1073/pnas.0802437105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Abd-Elhadi S, et al. Total and proteinase K-resistant alpha-synuclein levels in erythrocytes, determined by their ability to bind phospholipids, associate with Parkinson’s disease. Sci. Rep. 2015;5:11120. doi: 10.1038/srep11120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Araki K, et al. The localization of alpha-synuclein in the process of differentiation of human erythroid cells. Int. J. Hematol. 2018;108:130–138. doi: 10.1007/s12185-018-2457-8. [DOI] [PubMed] [Google Scholar]
- 103.Gautier EF, et al. Comprehensive proteomic analysis of human erythropoiesis. Cell Rep. 2016;16:1470–1484. doi: 10.1016/j.celrep.2016.06.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Imberdis T, Fanning S, Newman A, Ramalingam N, Dettmer U. Studying alpha-synuclein conformation by intact-cell cross-linking. Methods Mol. Biol. 2019;1948:77–91. doi: 10.1007/978-1-4939-9124-2_8. [DOI] [PubMed] [Google Scholar]
- 105.Kim S, et al. GBA1 deficiency negatively affects physiological alpha-synuclein tetramers and related multimers. Proc. Natl Acad. Sci. USA. 2018;115:798–803. doi: 10.1073/pnas.1700465115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dettmer U, Newman AJ, von Saucken VE, Bartels T, Selkoe D. KTKEGV repeat motifs are key mediators of normal alpha-synuclein tetramerization: Their mutation causes excess monomers and neurotoxicity. Proc. Natl Acad. Sci. USA. 2015;112:9596–9601. doi: 10.1073/pnas.1505953112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Killinger BA, Moszczynska A. Characterization of alpha-synuclein multimer stoichiometry in complex biological samples by electrophoresis. Anal. Chem. 2016;88:4071–4084. doi: 10.1021/acs.analchem.6b00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pieri L, Madiona K, Melki R. Structural and functional properties of prefibrillar alpha-synuclein oligomers. Sci. Rep. 2016;6:24526. doi: 10.1038/srep24526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Luth ES, Bartels T, Dettmer U, Kim NC, Selkoe DJ. Purification of alpha-synuclein from human brain reveals an instability of endogenous multimers as the protein approaches purity. Biochem. 2015;54:279–292. doi: 10.1021/bi501188a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Dettmer U, et al. Loss of native alpha-synuclein multimerization by strategically mutating its amphipathic helix causes abnormal vesicle interactions in neuronal cells. Hum. Mol. Genet. 2017;26:3466–3481. doi: 10.1093/hmg/ddx227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rhoades E, Ramlall TF, Webb WW, Eliezer D. Quantification of alpha-synuclein binding to lipid vesicles using fluorescence correlation spectroscopy. Biophys. J. 2006;90:4692–4700. doi: 10.1529/biophysj.105.079251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Newman AJ, Selkoe D, Dettmer U. A new method for quantitative immunoblotting of endogenous alpha-synuclein. PLoS ONE. 2013;8:e81314. doi: 10.1371/journal.pone.0081314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mukherjee S, et al. Characterization and identification of dityrosine cross-linked peptides using tandem mass spectrometry. Anal. Chem. 2017;89:6136–6145. doi: 10.1021/acs.analchem.7b00941. [DOI] [PubMed] [Google Scholar]
- 114.Getoff N. Pulse radiolysis of aromatic amino acids - state of the art. Amino Acids. 1992;2:195–214. doi: 10.1007/BF00805942. [DOI] [PubMed] [Google Scholar]
- 115.Papagiannakis N, et al. Alpha-synuclein dimerization in erythrocytes of patients with genetic and non-genetic forms of Parkinson’s disease. Neurosci. Lett. 2018;672:145–149. doi: 10.1016/j.neulet.2017.11.012. [DOI] [PubMed] [Google Scholar]
- 116.Wordehoff MM, et al. Opposed effects of dityrosine formation in soluble and aggregated alpha-synuclein on fibril growth. J. Mol. Biol. 2017;429:3018–3030. doi: 10.1016/j.jmb.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Stryer L, Haugland RP. Energy transfer: a spectroscopic ruler. Proc. Natl Acad. Sci. USA. 1967;58:719–726. doi: 10.1073/pnas.58.2.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tosatto L, et al. Single-molecule FRET studies on alpha-synuclein oligomerization of Parkinson’s disease genetically related mutants. Sci. Rep. 2015;5:16696. doi: 10.1038/srep16696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Nath S, Meuvis J, Hendrix J, Carl SA, Engelborghs Y. Early aggregation steps in alpha-synuclein as measured by FCS and FRET: evidence for a contagious conformational change. Biophys. J. 2010;98:1302–1311. doi: 10.1016/j.bpj.2009.12.4290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Iljina M, et al. Kinetic model of the aggregation of alpha-synuclein provides insights into prion-like spreading. Proc. Natl Acad. Sci. USA. 2016;113:E1206–E1215. doi: 10.1073/pnas.1524128113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Camacho R, Tauber D, Scheblykin IG. Fluorescence anisotropy reloaded-emerging polarization microscopy methods for assessing chromophores’ organization and excitation energy transfer in single molecules, particles, films, and beyond. Adv. Mater. 2019;31:e1805671. doi: 10.1002/adma.201805671. [DOI] [PubMed] [Google Scholar]
- 122.Yamasaki TR, et al. Parkinson’s disease and multiple system atrophy have distinct alpha-synuclein seed characteristics. J. Biol. Chem. 2019;294:1045–1058. doi: 10.1074/jbc.RA118.004471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dimant H, et al. Direct detection of alpha synuclein oligomers in vivo. Acta Neuropathol. Commun. 2013;1:6. doi: 10.1186/2051-5960-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Roberts RF, Wade-Martins R, Alegre-Abarrategui J. Direct visualization of alpha-synuclein oligomers reveals previously undetected pathology in Parkinson’s disease brain. Brain. 2015;138:1642–1657. doi: 10.1093/brain/awv040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Betzig E, et al. Imaging intracellular fluorescent proteins at nanometer resolution. Science. 2006;313:1642–1645. doi: 10.1126/science.1127344. [DOI] [PubMed] [Google Scholar]
- 126.Fauvet B, et al. alpha-Synuclein in central nervous system and from erythrocytes, mammalian cells, and Escherichia coli exists predominantly as disordered monomer. J. Biol. Chem. 2012;287:15345–15364. doi: 10.1074/jbc.M111.318949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Alderson TR, Markley JL. Biophysical characterization of alpha-synuclein and its controversial structure. Intrinsically Disord. Proteins. 2013;1:18–39. doi: 10.4161/idp.26255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Eliezer D, Kutluay E, Bussell R, Jr., Browne G. Conformational properties of alpha-synuclein in its free and lipid-associated states. J. Mol. Biol. 2001;307:1061–1073. doi: 10.1006/jmbi.2001.4538. [DOI] [PubMed] [Google Scholar]
- 129.Weinreb PH, Zhen W, Poon AW, Conway KA, Lansbury PT., Jr. NACP, a protein implicated in Alzheimer’s disease and learning, is natively unfolded. Biochem. 1996;35:13709–13715. doi: 10.1021/bi961799n. [DOI] [PubMed] [Google Scholar]
- 130.Araki K, et al. A small-angle X-ray scattering study of alpha-synuclein from human red blood cells. Sci. Rep. 2016;6:30473. doi: 10.1038/srep30473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Dedmon MM, Lindorff-Larsen K, Christodoulou J, Vendruscolo M, Dobson CM. Mapping long-range interactions in alpha-synuclein using spin-label NMR and ensemble molecular dynamics simulations. J. Am. Chem. Soc. 2005;127:476–477. doi: 10.1021/ja044834j. [DOI] [PubMed] [Google Scholar]
- 132.Galvin JE, Schuck TM, Lee VM, Trojanowski JQ. Differential expression and distribution of alpha-, beta-, and gamma-synuclein in the developing human substantia nigra. Exp. Neurol. 2001;168:347–355. doi: 10.1006/exnr.2000.7615. [DOI] [PubMed] [Google Scholar]
- 133.Fakhree MAA, Nolten IS, Blum C, Claessens M. Different conformational subensembles of the intrinsically disordered protein alpha-synuclein in cells. J. Phys. Chem. Lett. 2018;9:1249–1253. doi: 10.1021/acs.jpclett.8b00092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Shrivastava AN, Aperia A, Melki R, Triller A. Physico-pathologic mechanisms involved in neurodegeneration: misfolded protein-plasma membrane interactions. Neuron. 2017;95:33–50. doi: 10.1016/j.neuron.2017.05.026. [DOI] [PubMed] [Google Scholar]
- 135.Dikiy I, et al. Semisynthetic and in vitro phosphorylation of alpha-synuclein at Y39 promotes functional partly helical membrane-bound states resembling those induced by PD mutations. ACS Chem. Biol. 2016;11:2428–2437. doi: 10.1021/acschembio.6b00539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Anderson VL, Ramlall TF, Rospigliosi CC, Webb WW, Eliezer D. Identification of a helical intermediate in trifluoroethanol-induced alpha-synuclein aggregation. Proc. Natl Acad. Sci. USA. 2010;107:18850–18855. doi: 10.1073/pnas.1012336107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Patterson JR, et al. Time course and magnitude of alpha-synuclein inclusion formation and nigrostriatal degeneration in the rat model of synucleinopathy triggered by intrastriatal alpha-synuclein preformed fibrils. Neurobiol. Dis. 2019;130:104525. doi: 10.1016/j.nbd.2019.104525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Iyer A, Claessens M. Disruptive membrane interactions of alpha-synuclein aggregates. Biochimica et biophysica acta. Proteins Proteom. 2019;1867:468–482. doi: 10.1016/j.bbapap.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 139.Wakabayashi K, Tanji K, Mori F, Takahashi H. The Lewy body in Parkinson’s disease: molecules implicated in the formation and degradation of alpha-synuclein aggregates. Neuropathol. 2007;27:494–506. doi: 10.1111/j.1440-1789.2007.00803.x. [DOI] [PubMed] [Google Scholar]
- 140.Wakabayashi K, et al. The Lewy body in Parkinson’s disease and related neurodegenerative disorders. Mol. Neurobiol. 2013;47:495–508. doi: 10.1007/s12035-012-8280-y. [DOI] [PubMed] [Google Scholar]
- 141.Dale GE, et al. Relationships between Lewy bodies and pale bodies in Parkinson’s disease. Acta Neuropathol. 1992;83:525–529. doi: 10.1007/BF00310030. [DOI] [PubMed] [Google Scholar]
- 142.Gomez-Tortosa E, Newell K, Irizarry MC, Sanders JL, Hyman B. T. alpha-Synuclein immunoreactivity in dementia with Lewy bodies: morphological staging and comparison with ubiquitin immunostaining. Acta Neuropathol. 2000;99:352–357. doi: 10.1007/s004010051135. [DOI] [PubMed] [Google Scholar]
- 143.Kuusisto E, Parkkinen L, Alafuzoff I. Morphogenesis of Lewy bodies: dissimilar incorporation of alpha-synuclein, ubiquitin, and p62. J. Neuropathol. Exp. Neurol. 2003;62:1241–1253. doi: 10.1093/jnen/62.12.1241. [DOI] [PubMed] [Google Scholar]
- 144.Kanazawa T, et al. Pale neurites, premature alpha-synuclein aggregates with centripetal extension from axon collaterals. Brain Pathol. 2012;22:67–78. doi: 10.1111/j.1750-3639.2011.00509.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Wakabayashi K, et al. Accumulation of alpha-synuclein/NACP is a cytopathological feature common to Lewy body disease and multiple system atrophy. Acta Neuropathol. 1998;96:445–452. doi: 10.1007/s004010050918. [DOI] [PubMed] [Google Scholar]
- 146.Soper JH, et al. Alpha-synuclein-induced aggregation of cytoplasmic vesicles in Saccharomyces cerevisiae. Mol. Biol. cell. 2008;19:1093–1103. doi: 10.1091/mbc.e07-08-0827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Issidorides MR, Panayotacopoulou MT, Tiniacos G. Similarities between neuronal Lewy bodies in parkinsonism and hepatic Mallory bodies in alcoholism. Pathol. Res. Pract. 1990;186:473–478. doi: 10.1016/S0344-0338(11)80466-8. [DOI] [PubMed] [Google Scholar]
- 148.Gai WP, et al. In situ and in vitro study of colocalization and segregation of alpha-synuclein, ubiquitin, and lipids in Lewy bodies. Exp. Neurol. 2000;166:324–333. doi: 10.1006/exnr.2000.7527. [DOI] [PubMed] [Google Scholar]
- 149.Shahmoradian SH, et al. Lewy pathology in Parkinson’s disease consists of crowded organelles and lipid membranes. Nat. Neurosci. 2019;22:1099–1109. doi: 10.1038/s41593-019-0423-2. [DOI] [PubMed] [Google Scholar]
- 150.Thelen AM, Zoncu R. Emerging roles for the lysosome in lipid metabolism. Trends Cell Biol. 2017;27:833–850. doi: 10.1016/j.tcb.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kunkle BW, et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Abeta, tau, immunity and lipid processing. Nat. Genet. 2019;51:414–430. doi: 10.1038/s41588-019-0358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Chang D, et al. A meta-analysis of genome-wide association studies identifies 17 new Parkinson’s disease risk loci. Nat. Genet. 2017;49:1511–1516. doi: 10.1038/ng.3955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Johansen KK, Torp SH, Farrer MJ, Gustavsson EK, Aasly JO. A case of Parkinson’s disease with no Lewy body pathology due to a homozygous exon deletion in Parkin. Case Rep. Neurol. Med. 2018;2018:6838965. doi: 10.1155/2018/6838965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Haberkant P, Holthuis JC. Fat & fabulous: bifunctional lipids in the spotlight. Biochim. Biophys. Acta. 2014;1841:1022–1030. doi: 10.1016/j.bbalip.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 155.Hoglinger D, et al. Trifunctional lipid probes for comprehensive studies of single lipid species in living cells. Proc. Natl Acad. Sci. USA. 2017;114:1566–1571. doi: 10.1073/pnas.1611096114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zunke F, et al. Reversible conformational conversion of alpha-synuclein into toxic assemblies by glucosylceramide. Neuron. 2018;97:92–107 e110. doi: 10.1016/j.neuron.2017.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]