Abstract
Day care is a potential alternative to inpatient care of cancer patients. Using day care reduces medical costs substantially compared to inpatient care, which is driving the transfer of many inpatient chemotherapy protocols to day care hospitals (DCHs). However, in contrast to inpatient management, day care provides limited observation time, which could increase the risk of renal toxicity when using these protocols. We present a case report of acute kidney injury following high-dose methotrexate administration in a DCH. Based on a review of the current literature on acid-base balance, we also discuss appropriate patient selection and judicious hydration and urine alkalinization so as to prevent toxicity in the day care setting.
Key Points
| There is serious concern about the administration of high-dose methotrexate in hematology day care hospitals due to the increased risk of renal toxicity. |
| It is possible to achieve a good outcome through stringent selection of patients and the application of an appropriate urine alkalinization strategy. |
Introduction
Day care hospitals (DCHs) play a pivotal role in cancer care. Treating a cancer patient at a DCH reduces medical costs by two-thirds compared to treatment as an inpatient [1]. Although there are strict inpatient and outpatient chemotherapy protocols, the dividing line between them is becoming increasingly blurred. Some regimens, such as high-dose methotrexate (HD-MTX), are rapidly shifting to the day care setting. There is, however, concern about the potential for increased regimen toxicity due to the limited time available to observe patients in day care, in contrast to inpatient care. It is therefore essential to adjust the chemotherapeutic strategy accordingly. HD-MTX is a common pediatric and adult protocol for different malignancies such as osteosarcoma, acute lymphoblastic leukemia, and high-grade lymphoma (including CNS lymphoma). Here we report a case of acute kidney injury (AKI) due to HD MTX toxicity following infusion in a DCH. The optimal strategy for HD-MTX administration in a DCH is not described in the current literature, but it is likely to involve the careful selection of patients and appropriate management to prevent HD MTX toxicity in this changing landscape of patient care.
Case Report
An 81-year-old male patient was diagnosed with a stage IV diffuse large B-cell lymphoma (DLBCL). He had a history of myocardial infarction with two stents, essential hypertension, type 2 diabetes treated with metformin, and renal colic due to urinary stones. He was on bactrim prophylaxis. In view of his age, the multidisciplinary team (MDT) decided on eight courses of rituximab and mini-CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), and planned for two courses of consolidation with methotrexate (MTX) at 1 g/m2 body surface area (BSA). Before the first course of HD MTX, the patient’s baseline creatinine was normal (79 μmol/L), with a calculated clearance of 86.89 mL/min. His hemoglobin level was 9.1 g/dL. The patient had a body surface area of 1.82 m2, a height of 171 cm, and a weight of 71 kg. He received a total dose of 1800 mg of MTX infused over 4 h. Alkaline hydration was begun 4 h prior to MTX infusion; this consisted of normal saline and 1.4% sodium bicarbonate solution at an infusion rate of 125 mL/h, which was continued until the end of MTX administration. The patient’s pre-MTX urine pH was 7.5. The course was uneventful. His plasma MTX level at 24 h was 8.15 μmol/L, which was acceptable. At the same time, his creatinine level started to rise, indicating the onset of AKI and reaching a peak of 261 μmol/L (normal level: 40–120 μmol/L). His urea level was 8.1 mmol/L (normal level: 3.0–7.0 mmol/L). Levels of liver transaminases were normal. Renal ultrasound was normal. The diuresis was preserved. The patient had a mild pulmonary edema, and was treated with the antidote: intravenous glucarpidase at a dose of 2900 UI along with oral folinic acid rescue. A parallel treatment consisted of furosemide for fluid overload and acetazolamide for urine alkalinization. Although the blood MTX level was missing from the records for days 2 to 4 following MTX administration, the MTX level was 1.9 on the fifth day and 0.3 on the sixth day. The patient gradually improved, and presented creatinine and urea values of 128 μmol/L and 4 mmol/L, respectively, after 12 days.
Discussion
Methotrexate is an antimetabolite that interferes with the metabolism of folic acid. After entering cells, methotrexate binds to dihydrofolate reductase (DHFR) with an affinity that is 1000-fold greater than that of folate, and thus competitively inhibits the conversion of dihydrofolate to tetrahydrofolate, which is essential for the biosynthesis of thymidine and purines for DNA synthesis. The blockade of tetrahydrofolate synthesis by methotrexate leads to an inability of cells to divide and produce proteins. Hence, after 24 h of HD-MTX administration, rescue folinic acid is given for 48–72 h to prevent toxicity.
Although HD-MTX administration is commonly associated with moderate asymptomatic transaminasemia, renal toxicity is a major concern, as it occurs in 2–12% of patients [2]. Since these percentages relate to hospitalized inpatients, they may underestimate the incidence of renal toxicity in the day care setting. Obstructive uropathy due to the precipitation of metabolites of methotrexate (such as 7-hydroxymethotrexate and 2,4-diamino-N10-methylpteroic acid) within renal tubules in the presence of acidic urine results in acute tubular necrosis [3]. This precipitation occurs when the pH is lower than 5.7, so it is recommended that the urine pH should maintained at ≥ 7.0 until plasma MTX levels decline to < 0.1 μM [4]. Adequate hydration and urine alkalinization are therefore crucial to avoiding renal toxicity due to highly soluble metabolites. More than 90% of the administered methotrexate is eliminated by the kidneys. Many antineoplastics and antibiotics as well as low molecular weight heparin (LMWH) are relatively or absolutely contraindicated in the presence of renal toxicity, so compromised renal function further complicates patient care.
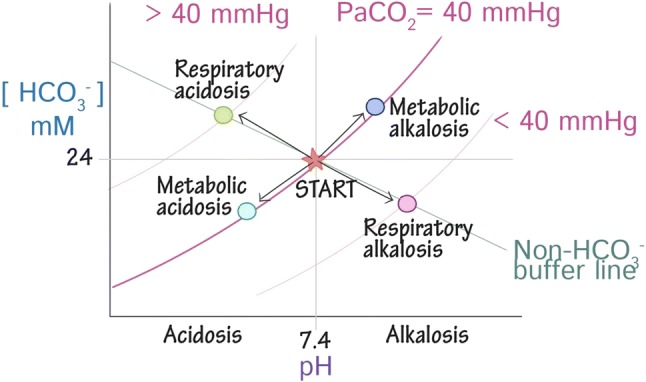
Before we propose a strategy for the management of HD-MTX in the day care setting, it is worth discussing the acid-base balance with the aid of a Davenport diagram. The acid-base balance is largely maintained by the kidney and lungs. The principal acid involved in this balance is carbon dioxide (CO2), which is a weak volatile acid. There are also fixed acids such as those liberated during metabolism (e.g., lactate). The principal buffers are open system buffers such as bicarbonate (HCO3) and closed system buffers such as phosphate and hemoglobin. Respiratory acidosis and alkalosis are compensated for by metabolic alkalosis and acidosis, respectively, and vice versa, with the exception that metabolic alkalosis cannot be compensated for by respiratory acidosis (to ensure that hypopnea-induced tissue hypoxia does not occur). Most of our patients are anemic and thus have reduced hemoglobin (closed system buffer) levels, which could compromise the acid-base balance.
A study by Kintzel et al. found that patients who received oral sodium bicarbonate preadmission showed reduced urine alkalinization (pH > 7) times and were administered HD MTX earlier [5]. In a prospective open-label trial by Cohen et al. [6], 4 g of sodium bicarbonate were administered orally three times daily to nine healthy volunteers for 24 h. Serial blood and urine samples were collected, and urine pH was evaluated. Plasma electrolytes and pH were also measured for safety purposes. All participants had a urine pH of at least 7 after 10 h; at 20 h, the pH was at least 8. No adverse effects or abnormal blood results were documented during the 24-h follow-up.
During the administration of HD-MTX, it is advisable to check the pH of urine in each void or hourly to ensure that the pH does not drop to 6.5. Sodium bicarbonate (NaHCO3) 12.5 mEq/m2 or 25 mEq/m2 is administered. It should be noted that NaHCO3 has the same equivalent weight and molecular weight (84), and that 25 mEq corresponds to 2.1 g. NaHCO3 induces a transient increase in plasma osmolality by increasing the bicarbonate level. The excess bicarbonate reacts with H+ to give H2CO3, increasing the pH. The kidney responds to the alkaline plasma environment by inhibiting renal H+ secretion and stimulating bicarbonate secretion. The H2CO3 dissociates to CO2 and water under the influence of carbonic anhydrase.
The earliest observation by Shamash et al. [7] describes the use of Acetazolamide 500 mg 6-hourly to alkalinize the urine in patients receiving high-dose methotrexate. A urinary pH of greater than 7.5 was achieved in every cycle (13 cycles in 10 patients). A single supplementary dose of sodium bicarbonate was necessary in six cycles. Plasma methotrexate had decreased to satisfactory levels at 24 and 48 h. Acetazolamide is a simple and effective method of achieving urinary alkalinization, with advantages over oral and intravenous bicarbonate. Carbonic anhydrase (mainly located at the luminal proximal tubule membrane) catalyzes the dehydration of carbonic acid, H2CO3, which is required for bicarbonate reabsorption, and the blockade of carbonic anhydrase activity by acetazolamide induces sodium bicarbonate diuresis, reducing body bicarbonate levels.
Folinic acid (a reduced form of folate) works via competitive cellular uptake, thus providing normal tissues with a mechanism to bypass normal tetrahydrofolate synthesis pathways, which circumvents the inhibition of DHFR. This is, however, insufficient to reduce the toxic plasma level of MTX. On the contrary, glucarpidase (also known as carboxypeptidase-G2 or CPDG2) is an enzyme that rapidly metabolizes circulating (not intracellular) MTX to two inactive metabolites: glutamate and 2,4-diamino-N10-methylpteroic acid (which undergoes biliary excretion following glucoronide conjugation in the liver) [8]. In the event of toxicity, glucarpidase should be used in association with folinic acid rescue to combat the intracellular and plasmatic effects of MTX.
Our patient scored 8 on the Naranjo Adverse Drug Reaction (ADR) Probability Scale. Although the score for definite ADR is at least 9, our patient’s score is actually an underestimation, as there was no rechallenge nor any previous exposure to MTX. The patient, who was elderly and was receiving concurrent bactrim and metformin, had recurrent nephrolithiasis, probably due to a serious renal pH disturbance. Although HD MTX was not contraindicated for our patient, he was not an ideal candidate for day care management. He was a better candidate for inpatient care, as prolonged monitoring was required. Nevertheless, a satisfactory 24-h residual methotrexate level does not totally exclude the potential for renal toxicity.
Based on the above review of the current literature regarding this issue, we now specify some steps that should be performed before administering HD MTX in a DCH:
In patients with a massive pleural effusion or ascites, any third-space fluid must be evacuated before administration, as MTX accumulates in third spaces, and there is no appropriate elimination route for MTX from these spaces [9].
Avoid administering drugs that interfere with MTX clearance. Drugs such as sulfamethoxazole trimethoprim and proton pump inhibitors must be stopped for 48–72 h starting from day −1 of MTX administration. Delayed clearance of MTX is also seen with aminoglycosides, probenecid, macrolides, mezlocillin, piperacillin, amphotericin B, and ciprofloxacin, which merits consideration.
If hemoglobin levels are low prior to treatment, blood transfusion should be completed prior to high-dose methotrexate administration (transfusing after high-dose methotrexate has been given will delay the clearance of methotrexate).
The hydration and urine alkalinization can be achieved in successive steps.
The Day Before HD-MTX Administration (Day −1)
There is no need for excessive oral hydration. Fluid intake is adequate if there is normal thirst and colorless or light yellow urine.
Sodium bicarbonate 1300 mg should be administered orally every 4 h while awake. This requires the ingestion of 8–10 tablets, each containing 650 mg of sodium bicarbonate, during the course of the day [5].
The Day of HD-MTX Administration (Day 0)
Introduce at least 2.5–3.5 L/m2/day of intravenous fluid 2–4 h before HD-MTX administration.
Provide sodium bicarbonate (NaHCO3) 12 mEq/m2 IV (slow) if pH is between 6.5 and 7, or 25 mEq/m2 if the pH is 7.
Use carbonic anhydrase inhibitor (acetazolamide) 500 mg IV (slow) if the pH is less than 7.
Perform hourly urinary pH measurements.
Day 1
Folinic acid rescue must be started 24 h after and continued until 48 h after the initiation of HD MTX administration. The dose used and the duration vary according to the local protocol. Commonly, it is 10–15 mg/m2 every 6 h until the MTX level falls to less than 0.2 μmol/L.
Days 2 and 3
The plasma MTX level must be measured 24, 48, and 72 h after starting the MTX infusion until it is less than 0.1 μM/L.
Administration of Glucarpidase for Renal Toxicity
The standard dose of glucarpidase is a single IV bolus injection of 50 units/kg administered over a period of 5 min. Patients should receive hydration and urine alkalinization as required. In addition, folinic acid therapy should be provided 2 h before or after a dose of glucarpidase, as folinic acid and its metabolite are substrates of the enzyme glucarpidase.
Conclusion
This is an old problem that we have revisited because of growing concern over acute kidney injury attributable to HD MTX administration in DCHs. Nevertheless, it is possible to avoid toxicity when administering HD MTX in the DCH setting through the appropriate selection of patients and careful management.
Compliance with Ethical Standards
Funding
No funding was received for the preparation of this manuscript.
Conflict of interest
The authors, SCM, AS, GD, and LBF, declare that they have no conflict of interest that might be relevant to the contents of this manuscript.
Consent to participate
Written informed consent was obtained from the patient.
References
- 1.Mor V, Stalker MZ, Gralla R, Scher HI, Cimma C, Park D, Flaherty AM, Kiss M, Nelson P, Laliberte L, et al. Day hospital as an alternative to inpatient care for cancer patients: a random assignment trial. J Clin Epidemiol. 1988;41(8):771–785. doi: 10.1016/0895-4356(88)90164-3. [DOI] [PubMed] [Google Scholar]
- 2.Howard SC, McCormick J, Pui C-H, Randall K, Buddington RK, Harvey RD. Preventing and managing toxicities of high-dose methotrexate. Oncologist. 2016;21(12):1471–1482. doi: 10.1634/theoncologist.2015-0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fox RM. Methotrexate nephrotoxicity. Clin Exp Pharmacol Physiol Suppl. 1979;5:43–45. [PubMed] [Google Scholar]
- 4.Al-Quteimat OM, Al-Badaineh MA. Practical issues with high dose methotrexate therapy. Saudi Pharm J. 2014;22(4):385–387. doi: 10.1016/j.jsps.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kintzel PE, Campbell AD, Yost KJ, Brinker BT, Arradaza NV, Frobish D, Wehr AM, O’Rourke TJ. Reduced time for urinary alkalinization before high-dose methotrexate with preadmission oral bicarbonate. J Oncol Pharm Pract. 2011;18(2):239–244. doi: 10.1177/1078155211426913. [DOI] [PubMed] [Google Scholar]
- 6.Cohen B, Laish I, Brosh-Nissimov T, Hoffman A, Katz LH, Braunstein R, Sagi R, Michael G. Efficacy of urine alkalinization by oral administration of sodium bicarbonate: a prospective open-label trial. Am J Emerg Med. 2013;31(12):1703–1706. doi: 10.1016/j.ajem.2013.08.031. [DOI] [PubMed] [Google Scholar]
- 7.Shamash J, Earl H, Souhami R. Acetazolamide for alkalinisation of urine in patients receiving high-dose methotrexate. Cancer Chemother Pharmacol. 1991;28(2):150–151. doi: 10.1007/BF00689708. [DOI] [PubMed] [Google Scholar]
- 8.Buchen S, Ngampolo D, Melton RG, et al. Carboxypeptidase G2 rescue in patients with methotrexate intoxication and renal failure. Br J Cancer. 2005;92(3):480–487. doi: 10.1038/sj.bjc.6602337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaies E, Jebabli N, Trabelsi S, Salouage I, Charfi R. Methotrexate side effects: review article. J Drug Metab Toxicol. 2012;3:125. doi: 10.4172/2157-7609.1000125. [DOI] [Google Scholar]