Abstract
Objective:
This study examines whether disparities exist in poor health and depressive symptomatology among older gay/bisexual men (50+) with (n = 371) and without (n = 973) HIV. If so, what risk/promoting factors account for those disparities?
Method:
These cross-sectional analyses used 2014 data from the Aging With Pride: National Health, Aging, and Sexuality/Gender Study.
Results:
Those with HIV reported poorer health and more depressive symptomatology accounted for by lower income, resilience and social support, and more lifetime victimization. Poorer health among those with HIV was associated with more chronic conditions. Higher depressive symptomatology was associated with diagnosed anxiety and drug addiction. Community engagement reduced disparities in poor health and depression.
Implications:
Older gay/bisexual men living with HIV infection are at greater risk for physical and mental health issues. Assessments should be conducted with attention to these risk factors. Interventions for improving social support, resilience, and community engagement are warranted.
Keywords: HIV, sexual minorities, health disparities, older gay and bisexual men, depression, physical health, older adults
Introduction
Older adults are diverse with regard to gender, race, ethnicity, and historical experience. Recently, there is a growing recognition that older adults are diverse with regard to sexual orientation and gender identity (Fredriksen-Goldsen, & Muraco, 2010). Based on population estimates, 2.4% of adults aged 50 and older identify as lesbian, gay, bisexual, or transgender (LGBT), accounting for more than 2.4 million older adults (Fredriksen-Goldsen & Kim, 2017). Compared with heterosexuals of similar age, gay male, lesbian, and bisexual older adults are more likely to experience poor health, disability, and mental distress (Fredriksen-Goldsen et al., 2013; Fredriksen-Goldsen & Kim, 2017; Wallace, Cochran, Durazo, & Ford, 2011).
Since the beginning of the HIV epidemic, gay and bisexual men (also termed men who have sex with men or MSM) have been disproportionally impacted by HIV (Centers for Disease Control and Prevention [CDC], 2016). This pattern has been consistent across time and is relevant to those aging with HIV. Recent data from the CDC indicate that 49.5% of all people living with HIV over the age of 50 in the United States have MSM as their transmission category. In addition, 48% of all new HIV cases in 2016 had MSM as the risk category (CDC, 2018a). Adding to the importance of these patterns is the fact that the number of older adults living with HIV is growing rapidly. This phenomenon is the result of a confluence of new infections of HIV among people above age 50 combined with the aging of those living with HIV who were infected at an earlier age (CDC, 2018a; Heckman & Halkitis, 2014). In a recent HIV surveillance report, the CDC found that in 2012 there were an estimated 357,097 people age 50 and over living with HIV in the United States (CDC, 2018b). By 2016, the number of those 50 and over living with HIV had risen to 477,886 indicating more than a 30% increase in the number of older adults living with HIV in a 4-year span of time.
Compared with their heterosexual counterparts, older gay and bisexual men have an increased risk for poorer physical health and poorer mental health (Fredriksen-Goldsen, Kim, Barkan, Muraco, & Hoy-Ellis, 2013). We also know that older people living with HIV in general are at risk for a variety of physical and mental health conditions. Older adults living with HIV experience health disparities when compared with their HIV-negative counterparts, including “accelerated” aging (Pathai, Bajillan, Landay, & High, 2014), an increase in comorbid health conditions (Wing, 2016), and social isolation and poorer informal social networks (Emlet, 2006; Grodensky et al., 2015). In the Aging and Health Report, Fredriksen-Goldsen and colleagues (2011) documented significant differences between those older, sexual minority adults with and without HIV including domains of health, psychological well-being, and social and personal risks and resources.
Older adults with living with HIV have also been found to have psychological strengths that foster resilience including mastery (Emlet, Shiu, Kim, & Fredriksen-Goldsen, 2017) suggesting the need to examine both risk as well as protective factors when conducting research with this population. An additional component of research focusing on sexual minority individuals must acknowledge the historical and environmental contexts (Fredriksen-Goldsen & Kim, 2017). HIV stigma has been associated with negative psychological states, and data from a large sample of LGBT older adults demonstrate the long-standing impact of lifetime victimization on poorer general heath, disability, and increased depression (Fredriksen-Goldsen et al., 2013). In addition, behavioral elements of lifestyle can also impact health and well-being. For example, adults with HIV have a higher proportion of smokers with serious health consequences than their HIV-negative counterparts (Reddy et al., 2017). Chronic conditions associated with substance use can have negative impacts on health and well-being, whereas older HIV positive adults have found to gain strengths and support from religion and spirituality (Brennan, 2008; Emlet, Harris, Furlotte, Brennan, & Pierpaoli, 2016). Thus, it is important to consider both the health affirming and detrimental behavioral processes for older adults living with HIV. The purpose of this study, therefore, is to assess two research questions using data from the Aging With Pride: National Health, Aging, and Sexuality/Gender Study (NHAS) that allow for a comparison of older gay and bisexual men with and without HIV infection: (a) Are there disparities in poor general health and depressive symptomatology as well as health risk and promoting factors between gay and bisexual older men living with HIV and without HIV? (b) Which health risk and promoting factors account for the disparities in poor general health and depressive symptomatology between gay and bisexual older men living with HIV and without HIV? Based on the literature and previous research, we put forth two directional hypotheses. First, we hypothesize that older gay and bisexual men living with HIV will show heightened rates of poor general health, depressive symptomatology, and more health risk factors and lower rates of health-promoting factors as compared with their counterparts without HIV. Second, we hypothesize that the disparities in poor general health and depressive symptomatology among HIV-positive older gay and bisexual men, compared with their HIV-negative counterparts, will be explained by those with HIV having heightened disadvantages in health risk and promoting factors. The selection of the health risk and promoting factors in the study was guided by existing literature, as stated above, revealing factors associated with HIV infection and/or health and well-being and the following conceptual model.
Conceptual Framework
Because of the multiple components that impact the well-being of older gay and bisexual men and the need to consider historical and environmental impacts on health, we have conceptualized this analysis drawing from the Health Equity and Promotion Model (HEPM), which articulates the determinants of health and well-being in historically disadvantaged populations. The model is unique in that unlike previous models used to examine the mental and physical health of LGBT older adults, the HEPM incorporates an Iridescent Life Course (Fredriksen-Goldsen, Jen, & Muraco, 2019) perspective to better understand the full range of positive and adverse experiences that may influence individual opportunities (Fredriksen-Goldsen & Kim, 2017). As seen in Figure 1, the model takes into account the importance of a historical perspective as well as the individual life events and characteristics that influence health and well-being. In this analysis, we based our conceptualizing of factors associated with health disparities into historical and environmental, psychological, social, behavioral, and biological factors (including chronic conditions), influencing health outcomes. For a full description of the model, see Fredriksen-Goldsen et al., 2014).
Figure 1.
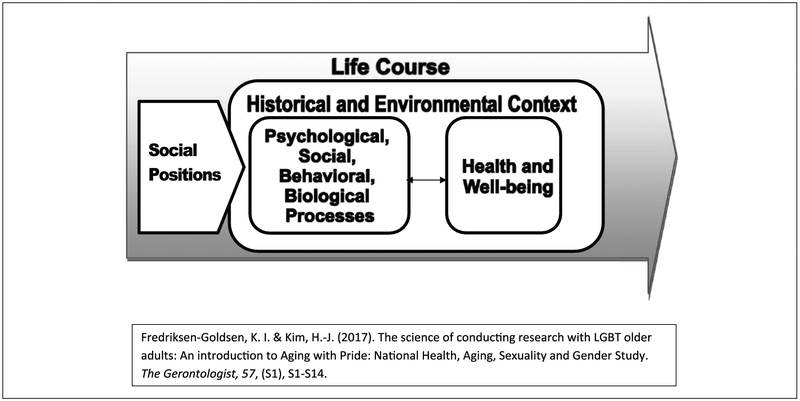
Health equity and promotion model.
Source. Adapted from Fredriksen-Goldsen & Kim (2017).
Method
Conducting research on health disparities among older adults living with HIV creates methodological challenges. Lyons, Pitts, and Grierson (2012) suggest that to conduct a full assessment of the impact of HIV infection on older adults, a comparison between those with and without HIV infection is needed. Similarly, using non HIV-infected individuals from the general population creates other problems. Uninfected adults from the general population are different from persons living with HIV, and demographic, lifestyle, socioeconomic factors, and health outcomes (including comorbidities) must be considered (Wong, Althoff, & Gange, 2014). Sample size is also a concern, as even studies using a nationally representative sample most often have a small number of older adults living with HIV (Beatie, Mackinzie, & Chou, 2015).
To address such concerns, we used our data from the NHAS for this analysis. NHAS is the first longitudinal study of LGBT older adults, aged 50 and older funded by the National Institutes of Health/National Institute on Aging. The sampling strategies for this study was designed to achieve the aims of the research study and also to address the challenges of conducting research with LGBT older adults (Fredrisken-Goldsen & Kim, 2017) including those living with HIV infection. Data from the NHAS allow us to examine potential health disparities associated with HIV infection among a vulnerable and marginalized population similar in age, sex, and sexual orientation while focusing on a population disproportionally impacted by HIV.
Data and Procedures
This current study conducted a cross-sectional analysis using a subsample of gay and bisexual men (n = 1,344), from the NHAS. Data collected from a 2014 survey were analyzed. The NHAS recruited older adults aged 50 or more who self-identified as lesbian, gay, bisexual, transgender, or nonbinary, and/or reported engagement in same-sex sexual behavior or romantic relationship. The sample includes participants from across all U.S. census divisions using contact lists of service organizations for LGBT older adults as well as via social network clustering chain referral to secure sufficient proportions of underrepresented subgroups, including racial/ethnic minorities and the oldest old. Self-administered surveys, either in English or Spanish, were collected after distribution in the fall of 2014 through postal or electronic mail according to participant’s preference. With an initial response rate of 70%, 2,686, out of 3,627 potential participants returned complete surveys. The final sample size was reduced to 2,450 through random selection conducted when the sample size of a particular subgroup exceeded the sampling goals (Fredriksen-Goldsen & Kim, 2017). Research protocols of the study were approved by the Human Subjects Division of the University of Washington. This current study focuses on gay and bisexual men with and without HIV (n = 371 and 973, respectively). Survey weights were applied for postsurvey adjustments that address sampling bias and improve the generalizability. See blinded for review for more information regarding the postsurvey adjustment procedures.
Measures
HIV status.
HIV status indicates whether or not participants reported that they had ever been told by a health care provider that they had HIV and/or AIDS. A dichotomous variable indicating either or both diagnoses (1) versus none (0) was used.
Health outcomes.
Poor general health was measured by a single item, selfrated overall health (1 = excellent; 5 = poor). A single-item measure asking about global self-rating of general health is evidenced to have validity and reliability in measuring overall general health status in addition to its benefits of simplicity and reduced burden on respondents (Bowling, 2005). Depressive symptomatology was measured with the 10-item Center for Epidemiologic Studies Depression Scale (CES-D 10) (Andresen, Malmgren, Carter, & Patrick, 1994). A summed score of the CESD-10 ranged from 0 to 30 with each item measured on a response format of 0 (less than one day) to 3 (five to seven days) with a higher score indicating a higher symptomatology of depression (α = .85).
Health risk and promoting factors
Historical and environmental.
LGBT-related lifetime discrimination and victimization (Fredriksen-Goldsen & Kim, 2017) was assessed for five types of discrimination (e.g., employment, housing, and health care) and nine types of victimization (e.g., verbal and physical threat, verbal, physical, and sexual assault, property damage, threat of being outed). Participants were asked to report on a scale (0 = never to 3 = three or more times) how many times they have experienced each type of event in their life because of their LGBT identities. Each response was summed into a discrimination scale with a possible range from 0 to 15 (α = .77) and a victimization scale with a possible range from 0 to 27 (α = .85). LGBT-related micro-aggression, brief and commonplace daily indignities, intentional or unintentional, that communicate hostility, negativity, and insults, was assessed with eight items (Fredriksen-Goldsen & Kim, 2017). The eight-item measure adopted interpersonal and environmental micro-aggression framework and addressed three domains of micro-aggression including micro-invalidation/insult, micro-assault, and hostile environment (Sue et al., 2007). Participants reported on the frequency of experiences such as “People use derogatory terms to refer to LGBT individuals in your presence” on a scale from never (0) to almost every day (5). An average score was used with a Cronbach’s alpha of .85. Day-to-day discrimination experiences of unfair treatment that may occur on a daily basis were assessed with six items measuring frequency of experiences (Fredriksen-Goldsen & Kim, 2017). Items included, “People do things that devalue and humiliate you” and “People suggest you are inferior to others,” and participants responded on a scale ranging from never (0) to almost every day (5). An average score was used with the Cronbach’s alpha of .91.
Psychological.
LGBT identity affirmation and stigma were the two indicators of identity appraisal (Fredriksen-Goldsen & Kim, 2017). Identity affirmation, the extent to which an LGBT person has positive attitudes and feelings toward their sexual or gender identity (Mayfield, 2001; Mohr & Kendra, 2011), was assessed with a mean of four items (1 = strongly disagree; 6 = strongly agree). Items include “I am proud to be LGBT,” with an α = .81. Identity stigma, negative attitudes, and feelings toward their sexual or gender identity, or personal acceptance of sexual stigma as part of one’s value system and self-concept as defined by Herek, Gillis, and Cogan (2009), was also assessed with a mean of four items (1 = strongly disagree; 6 = strongly agree), including “I feel ashamed of myself for being LGBT, with an α = .83. To assess perceived resilience, the capacity for people to rebound when they experience hardships (Smith et al., 2008), we utilized a three-item scale (Fredriksen-Goldsen & Kim, 2017). Items include “I tend to bounce back quickly after hard times,” and responses were on a 6-point Likert-type scale (1 = strongly disagree; 6 = strongly agree). An average score with higher scores indicating greater perceived resilience was used with the Cronbach’s alpha of .81. Spirituality, spiritual beliefs, meaning, and support, was measured with a 4-item spirituality scale (Fredriksen-Goldsen & Kim, 2017). Items include “I believe in a higher power or God who watches over me,” and participants were asked to rate each item on a 6-point Likert-type scale (1 = strongly disagree; 6 = strongly agree). An average score with higher scores indicating greater spirituality was used with the Cronbach’s alpha of .92. Anxiety was measured dichotomously by a single item asking whether participants have ever been diagnosed with anxiety (1 = yes; 0 = no).
Behavioral.
Current smoking was measured based on two survey questions, whether they had smoked at least 100 cigarettes in their entire lives and, if so, whether they currently smoke cigarettes every day, some days, or not at all. Those who indicated smoking every day or some days were coded as current smokers (1). Those who had smoked fewer than 100 lifetime cigarettes or currently did not smoke at all were coded as nonsmokers (0) (Jamal et al., 2015). Physical activities were measured by asking frequency and quantity of moderate and vigorous physical activity. The variable was dichotomized by determining whether the CDC recommendation of 150 min of moderate or 75 min of vigorous activities per week or an equivalent mix of the two (CDC, 2015) was met (1 = yes; 0 = no).
Social.
Social support was measured with the abbreviated four-item scale (Gjesfjeld, Greeno, & Kim, 2008) of the Medical Outcomes Study (MOS)-Social Support Scale (Sherbourne & Stewart, 1991). Items of this scale capturing perceived instrumental, informational, affectionate, and social interaction support include “Someone to help with daily chores if you were sick,” and participants answered on a scale from never (0) to very often (4). An average score with higher score indicating more support was used with the Cronbach’s alpha of .86. LGBT community engagement was measured by the four-item Community Engagement scale (Fredriksen-Goldsen & Kim, 2017), addressing the sense of belonging, participation in social activity in the community, sense of trust and helpfulness, and making contributions to community. Items included “I feel part of the community,” and the response was on a 6-point Likert-type scale (1 = strongly disagree; 6 = strongly agree). An average score of which the higher indicates higher engagement was used with the Cronbach’s alpha being .86. Being partnered/married in terms of relationship status was measured with a single question where participants selected whether they were single (0) or partnered or married (1). Death of a partner was dichotomously measured by asking whether participants had ever experienced in lifetime the death of a partner or spouse (1 = yes; 0 = no).
Biological/chronic conditions.
The number of chronic conditions was measured by 11 types of chronic conditions ever diagnosed, including back pain, heart attack, high blood pressure, any heart diseases, arthritis, osteoporosis, diabetes, lung and respiratory problems including asthma, cancer, stroke, and dementia including Alzheimer’s. The chronic health conditions assessed have been identified as those leading to disability (Brault, 2008; Freedman, Schoeni, Martin, & Cornman, 2007) and the number was summed with scores ranging from zero to 10. Drug addiction and alcoholism were each measured dichotomously by a single item asking whether the participants have ever been told by health professionals to have drug addiction or and/or alcoholism (1 = yes; 0 = no).
Background characteristics.
Background characteristics included age (in years), sexual orientation (gay vs. bisexual), household income at or below versus above 200% of the federal poverty level according to federal income guidelines (U.S. Department of Health and Human Services, 2013), education (high school graduate or less vs. other), and race/ethnicity (non-Hispanic White vs. other).
Analysis
Analysis was conducted using Stata/SE 14.2 (Stat Corp LP, College Station, TX). First, we examined distributions of background characteristics, health risk and promoting factors, and health outcomes by HIV status. Means for continuous variables and percentage distributions for categorical variables as well as their 95% confidence intervals were computed by HIV status. We further conducted linear or logistic regressions to evaluate statistical significance of the differences by HIV status holding age constant in the significance tests, as those with HIV in the sample were significantly younger than their counterparts without HIV (58.2 vs. 63.4 in years, p < .001). Second, as a step to examine factors that account for HIV status-related disparities in health outcomes, we selected the background characteristics and health-promoting and risk factors that were found to be significantly associated with HIV status in the preceding analyses at p < .10 level and further tested whether they predicted health outcomes. The HIV-associated factors were entered as covariates in the regression models predicting poor general health and depressive symptomatology based on the hypothesis that the association between HIV status and health outcomes would be explained away by these HIV-associated factors. Multicollinearity were checked and no concerns were found with the variance inflation factors (VIFs) ranging from 1.05 to 1.75 indicating weak correlations. Third, we further conducted statistical testing of these hypothesized indirect effects of HIV status on health outcomes. To identify the mediated HIV effect, a bootstrapping procedure was performed for each mediating factor instead of assessing or reduction in direct HIV effects on health outcomes (Zhao, Lynch, & Chen, 2010). Indirect effect coefficients (a product of the coefficient for the effect of HIV on a factor and the coefficient for the effect of the same factor on an outcome) and bias-corrected confidence intervals were computed with 3,000 replications (Preacher & Hayes, 2008). If the confidence interval did not contain zero, the indirect effect is considered statistically significant.
Results
Background Characteristics, Health Risk and Promoting Factors, and Health Outcomes by HIV Status
The HIV prevalence rate among gay and bisexual men aged 50 or older in this study was 32.52%. Table 1 illustrates the findings on differences according to HIV status in background characteristics, health-promoting and risk factors, and health outcomes. Compared with older gay and bisexual men without HIV, those with HIV were younger, more likely to be gay than bisexual (with marginal significance), to have household income at or below 200% of the federal poverty line, to have attained education of high school or less, and to be racial/ethnic minorities.
Table 1.
Background Characteristics, Health Risk and Promoting Factors, and Health Outcomes by HIV Status.
| HIV (unweighted n = 371) |
Non-HIV (unweighted n = 973) |
|
|---|---|---|
| M or % [95% CI] | M or % [95% CI] | |
| Background characteristics | ||
| Age | 58.23 [57.25, 59.21]*** | 63.38 [62.47, 64.28] |
| Sexual orientation: Gay | 86.47% [79.26, 91.45]† | 81.15% [75.58, 85.69] |
| Income: ≤200% Poverty | 48.44% [40.06, 56.91]*** | 21.65% [17.56, 26.39] |
| Education: High school or less | 45.31% [36.89, 54.01]*** | 21.96% [72.30, 82.88] |
| Race/ethnicity: Non-Hispanic White | 59.64% [51.01, 67.72]*** | 87.31% [83.30, 90.47] |
| Health risk and promoting factors | ||
| Historical & environmental | ||
| LGBT-related lifetime discrimination | 2.27 [1.77, 2.78] | 1.69 [1.34, 2.03] |
| LGBT-related lifetime victimization | 7.11 [5.94, 8.28]† | 5.19 [4.59, 5.79] |
| LGBT-related micro-aggressions | 1.42 [1.24, 1.60] | 1.19 [1.10, 1.27] |
| Day-to-day discrimination | 0.95 [0.80, 1.10] | 0.90 [0.79, 1.01] |
| Psychological | ||
| LGBT identity affirmation | 5.09 [4.94, 5.25] | 5.16 [5.06, 5.25] |
| LGBT identity stigma | 1.80 [1.63, 1.97]† | 1.62 [1.52, 1.71] |
| Resilience | 3.94 [3.75, 4.13]* | 4.28 [4.16, 4.40] |
| Spirituality | 3.96 [3.66, 4.26]† | 3.61 [3.44, 3.79] |
| Anxiety: ever | 42.60% [34.45, 51.17]*** | 21.89% [17.69, 26.76] |
| Behavioral | ||
| Current smoking | 21.37% [14.82, 29.80] | 12.27% [8.94, 16.61] |
| Physical activities | 81.78% [74.34, 87.43] | 81.25% [76.83, 84.99] |
| Social | ||
| Social support | 2.42 [2.22, 2.62]* | 2.72 [2.59, 2.84] |
| LGBT community engagement | 4.03 [3.86, 4.21]* | 3.80 [3.68, 3.92] |
| Partnered/married | 34.95% [27.01, 43.82]*** | 52.19% [46.89, 57.44] |
| Death of a partner | 43.77% [35.60, 52.28]*** | 29.76% [25.19, 34.76] |
| Biological | ||
| Number of chronic health conditions | 1.98 [1.66, 2.30]** | 1.66 [1.51, 1.82] |
| Drug addiction diagnosed ever | 11.38% [6.56, 19.02]** | 2.20% [0.94, 5.07] |
| Alcoholism diagnosed ever | 13.46% [8.28, 21.14] | 7.73% [5.10, 11.55] |
| Health outcomes | ||
| Poor general health | 3.15 [2.99, 3.31]*** | 2.62 [2.51, 2.73] |
| Depressive symptomatology | 11.20 [9.90, 12.50]*** | 7.19 [6.44, 7.94] |
Note. Statistical significance was tested with the ordinary least squares regressions and logistic regressions. Each variable was regressed on HIV status and age as a covariate. Age and HIV was analyzed on a bivariate level. LGBT = lesbian, gay, bisexual, and transgender; CI = confidence interval.
p < .10.
p < .05.
p < .01.
p < .001.
We found significant differences in health-promoting and risk factors according to HIV status after controlling for age. Older gay and bisexual men living with HIV experienced more LGBT-related lifetime victimization and reported higher level of LGBT identity stigma with marginal significance. Those with HIV had lower resilience, higher spirituality (marginally significant), and higher prevalence of an anxiety diagnosis. HIV-positive older gay and bisexual men reported lower level of social support and higher levels of LGBT community engagement. They were less likely to have a partner and more likely to have experienced the death of a partner. Those living with HIV had more chronic conditions and were more likely to have had a diagnosis of drug addiction than their HIV-negative counterparts.
Health outcomes were also significantly different according to HIV status. Older gay and bisexual men with HIV rated their general health poorer and had higher scores of depressive symptomatology than those without HIV.
Indirect Effects of HIV on Health Outcomes via Health-Promoting and Risk Factors
As a preliminary step for estimating indirect effects of HIV on health outcomes, we tested whether the health-promoting and risk factors significantly associated with HIV status were predictive of the health outcomes, controlling for HIV status and age. In this regard, only those factors that were significantly (at least at p < .10) associated with HIV status based on the preceding analyses (Table 1) were included. Table 2 shows the findings of the regression models predicting the health outcomes, and Table 3 shows the results of the bootstrapping procedures showing significant mediators of the HIV effects on poor general health and depressive symptomatology.
Table 2.
Regressions of Poor General Health and Depressive Symptomatology on HIV Status and Possible Mediating Factors, b [95% CI].
| Poor general health |
Depressive symptomatology |
|
|---|---|---|
|
F(15, 2,317) = 15.85 R2 = 36.09% |
F(15, 2,298) = 35.34 R2 = 56.29% |
|
| HIV/AIDS | 0.19 [−0.00, 0.38]† | 0.62 [−0.48, 1.72] |
| Age | −0.00 [−0.01, 0.01] | −0.05 [−0.10, −0.00]* |
| Sexual orientation: Gay (vs. Bisexual) | 0.09 [−0.14, 0.32] | −0.42 [−1.86, 1.02] |
| Income: ≤ 200% Poverty | 0.48 [0.28, 0.68]*** | 2.57 [1.19, 3.96]*** |
| Education: High school or less | 0.20 [−0.01, 0.41]† | 0.62 [−0.60, 1.85] |
| Race/ethnicity: Non-Hispanic White | −0.18 [−0.42, 0.06] | 0.37 [−1.01, 1.76] |
| LGBT-related lifetime victimization | 0.02 [0.01, 0.03]** | 0.17 [0.09, 0.25]*** |
| LGBT identity stigma | −0.05 [−0.14, 0.05] | 0.21 [−0.28, 0.70] |
| Resilience | −0.10 [−0.18, −0.01]* | −2.51 [−2.92, −2.09]*** |
| Spirituality | −0.00 [−0.05, 0.05] | 0.05 [−0.19, 0.28] |
| Anxiety: ever | 0.10 [−0.10, 0.30] | 2.48 [1.36, 3.60]*** |
| Social support | −0.10 [−0.18, −0.02]* | −0.76 [−1.29, −0.23]** |
| LGBT community engagement | −0.09 [−0.16, −0.02]* | -0.42 [−0.82, −0.02]* |
| Partnered/married | 0.09 [−0.08, 0.25] | 0.48 [−0.71, 1.66] |
| Death of a partner | −0.01 [−0.19, 0.16] | 0.59 [−0.33, 1.51] |
| Number of chronic health conditions | 0.22 [0.16, 0.28]*** | 0.17 [−0.14, 0.47] |
| Drug addiction diagnosed ever | −0.07 [−0.58, 0.44] | 2.26 [0.23, 4.30]* |
Note. Statistical significance was tested with the ordinary least squares regressions. Poor general health and depressive symptomatology was regressed on the health risk and promoting factors significantly associated with HIV/AIDS on a bivariate level with age held constant. LGBT = lesbian, gay, bisexual, and transgender; CI = confidence interval.
p < .10.
p < .05.
p < .01.
p < .001.
Table 3.
Indirect Effects of HIV-Positive Status on Poor General Health and Depressive Symptomatology: Path Coefficients (Bias-Corrected 95% CI).
| Mediating variables | Poor general health | Depressive symptomatology |
|---|---|---|
| Sexual orientation: Gay (vs. Bisexual) | −0.01 (−0.04, 0.01) | 0.04 (−0.08, 0.22) |
| Income: ≤ 200% Poverty | 0.11 (0.06, 0.19) | 0.58 (0.27, 1.11) |
| Education: High school or less | 0.05 (0.00, 0.11) | 0.15 (−0.13, 0.50) |
| Race/ethnicity: Non-Hispanic White | 0.03 (−0.01, 0.10) | −0.07 (−0.38, 0.18) |
| LGBT-related lifetime victimization | 0.02 (0.00, 0.07) | 0.21 (0.01, 0.56) |
| LGBT identity stigma | −0.01 (−0.05, 0.01) | 0.04 (−0.04, 0.23) |
| Resilience | 0.03 (0.00, 0.07) | 0.66 (0.07, 1.29) |
| Spirituality | −0.00 (−0.02, 0.02) | 0.01 (−0.05, 0.14) |
| Anxiety: ever | 0.02 (−0.01, 0.06) | 0.37 (0.13, 0.78) |
| Social support | 0.04 (0.01, 0.09) | 0.28 (0.07, 0.65) |
| LGBT community engagement | −0.02 (−0.06, −0.00) | −0.09 (−0.30, 0.00) |
| Partnered/married | −0.02 (−0.06, 0.01) | −0.10 (−0.42, 0.11) |
| Death of a partner | −0.00 (−0.04, 0.03) | 0.11 (−0.04, 0.34) |
| Number of chronic health conditions | 0.11 (0.03, 0.18) | 0.08 (−0.07, 0.26) |
| Drug addiction diagnosed ever | −0.01 (−0.05, 0.04) | 0.18 (0.01, 0.53) |
Note. Path coefficient indicating the indirect effect through each mediator was computed by multiplying the two coefficients: one from HIV status to mediator and another from mediator to health outcome. The bias-corrected 95% CIs were calculated from the bootstrap results of 3,000 replications. The CIs that do not contain zero are presented in bold, indicating statistically significant indirect effects at p < .05; CI = confidence interval.
As shown in Table 2, poor general health was associated with income at or below 200% of federal poverty level, education level of high school or less (marginally), more LGBT-related lifetime victimization, lower levels of resilience, social support, and LGBT community engagement, and more chronic conditions. Subsequent bootstrapping procedures confirmed these factors as significant mediators in the link from HIV-positive status to poor general health (see Table 3). Those with HIV were more likely to have poorer general health than their counterparts without HIV because of their lower income and education, more LGBT-related lifetime victimization, lower resilience and social support, and more chronic conditions. The direction of indirect effect via LGBT community engagement was different from the other factors stated above, such that the risk of poorer general health was lower for those with HIV (as indicated by the negative coefficient, −0.02) on account of their level of LGBT community engagement being higher than those without HIV.
Depressive symptomatology was associated with younger age, income at or below 200% of federal poverty line, more LGBT-related lifetime victimization, lower resilience, diagnosis of anxiety and/or drug addiction, lower social support, and lower LGBT community engagement. Subsequent bootstrapping procedures confirmed the significant mediating effects of these factors in the association of HIV and depressive symptomatology. Those with HIV were more likely to have higher depressive symptomatology because of their lower income, more LGBT-related lifetime victimization, lower resilience, higher prevalence of diagnosed anxiety, higher prevalence of drug addiction, and lower social support. LGBT community engagement operated in the opposite direction to the other factors for depressive symptomatology as well. Those with HIV were to have lower scores of depressive symptomatology (coefficient = −0.09) on the account of their level of LGBT community engagement being higher than those without HIV.
Discussion
This study sought to determine whether there are health disparities among older gay and bisexual men with and without HIV infection, and if so, what are the determinants of those disparities? We hypothesize that older gay and bisexual men living with HIV would evidence heightened rates of poor general health, depressive symptomatology, and health risk factors and lower rates of health-promoting factors. For this analysis, we used 2014 data of 1,344 gay and bisexual men from the NHAS for comparison. The analysis was guided by the HEPM. Our initial analysis supported our first hypothesis, as we found significantly higher scores in both health outcomes, poor general health and depressive symptomatology, among those living with HIV compared with those without HIV. Not only the health outcomes but also background characteristics and health-promoting and risk factors were different between those older gay and bisexual men with and without HIV. These findings reinforce Burbank’s (2006) position that specific diverse groups of older adults, even those within an already vulnerable group, may experience increased risk of adverse physical, psychological, and social health outcomes. Our findings, in part, are consistent with a national study of 1,135 Australian gay men age 40 and over. In that study, Lyons et al. (2012) found that individuals living with HIV had significantly lower incomes and were more likely to have experienced depression than their HIV-negative counterparts. Our findings that those men living with HIV infection reported poorer health status, including drug addiction, anxiety, more chronic conditions, poorer general health, and higher depressive symptomatology, are consistent with a study using the Veterans Aging Cohort Study (VACS) in which Goulet and colleagues (2007) found VACS participants with HIV had higher rates of multimorbidity, which included three clusters of medical disease, psychiatric disorders, and substance abuse disorders compared with their HIV-negative counterparts. Our findings reinforce the added vulnerability in both physical health and psychological disorders (in this case depression) among older gay and bisexual men living with HIV compared with their HIV-negative counterparts. Older gay and bisexual men with HIV infection may need additional services and supports from both the HIV and aging sectors to maintain positive physical and mental health outcomes. In addition, our findings also reinforce that older adults of color are overrepresented among people over the age of 50 living with HIV infection (CDC, 2018c), suggesting the intersectionality of race/ethnicity, sexual orientation, and HIV status. These findings are important as many of the methodological concerns expressed in previous HIV research have been addressed in this study including small sample size, particularly among racial and ethnic minorities, and lack of a demographically similar HIV uninfected comparison group (Goulet et al., 2007; Wong et al., 2014).
The second research question this analysis sought to assess was which health risk and promoting factors account for the disparities in poor general health and depressive symptomatology between gay and bisexual older men living with HIV and without HIV infection. We hypothesized that the disparities in poor general health and depressive symptomatology among HIVpositive older gay and bisexual men, compared with their HIV-negative counterparts, would be explained by those with HIV having heightened disadvantages in health risk and promoting factors. The findings from our analysis as to factors accounting for higher poor general health and depressive symptomatology among older gay and bisexual adults living with HIV support our hypothesis and reinforce the predictive value of the HEPM. As seen in Figure 1, the model takes into account not only psychological, social, and behavioral processes but examines them in an environmental and historical context. Our findings provide support for the importance and relevance of LGBT-related lifetime victimization as a risk factor as well as LGBT community engagement as a protective factor against poorer health outcomes. D’Augelli and Grossman (2001) found lifetime victimization had deleterious effects on mental and social health among lesbian, gay, and bisexual older adults, while other research has tied victimization to poorer physical health as well (Kimmel, Rose, & David, 2006). The findings from this analysis uncover the greater impact of lifetime victimization and lowered social support on both depressive symptoms and poor physical health. The finding again points to within-group marginalization, or being multiply disadvantaged within the population of older gay and bisexual men. Compared to older gay and bisexual men without HIV infection, living with HIV has historical, psychological, social, behavioral, and biological impact as our model suggests.
The findings related to protective factors of community involvement are consistent with a recent study by Emlet and colleagues (2017) who found LGBT community engagement was positively associated with both increased resilience and mastery among older gay and bisexual men living with HIV. Resilience and mastery was, in that study, significantly associated with improved psychological health-related quality of life. While older adults living with HIV often cite the importance of the HIV community though associations with AIDS Service Organizations as meaningful (Emlet et al., 2016), these findings reinforce the importance of continued connection to the LGBT community as well, as a source of support and a protective factor against negative health outcomes. It is important to consider the historical impact that community involvement and engagement had on (primarily) gay men in the early days of the HIV epidemic. The history of community engagement surrounding HIV is rich, emanating from a period when serving others with HIV/AIDS was seen as part of the fight to survive. Community engagement, often through volunteerism in the arena of HIV, provided a way for individuals to find meaning (Gaskins & Brown, 1997). The history of community engagement and experiencing its reciprocal benefits may be stronger for those men who lived through the epidemic with HIV, creating an enhanced sense of the importance of community engagement. The reciprocity of such engagement (Emlet & Harris, 2018) may be a reason that macro-level engagement with one’s community is a protective factor.
Of considerable concern are our findings that living with HIV in this sample of older gay and bisexual men was associated with lower levels of resilience and decreased levels of social support. Those men living with HIV were less likely to be married or partnered and more likely to have experienced the death of a partner. Whether less social support was due to a smaller social network because of AIDS-related losses is unknown. We do know from other studies that social support has been associated with lower levels of HIV stigma (specifically anticipated and internalized stigma) among older Canadians living with HIV (Emlet et al., 2013) as well as associated with improved mental health related quality of life, mastery (Emlet, Fredriksen-Goldsen, & Kim, 2013), and resilience (Fang et al., 2015) in older adults with HIV infection. Loneliness has been found to be associated with increased depression among HIV-positive older adults (Greysen et al., 2013; Grov, Golub, Parsons, Brennan, & Karpiak, 2010). These findings remind us of the particular social vulnerability of this population and reinforce the need to continue to create and foster mechanisms for social support for this population. Creating HIV and age sensitive venues through existing AIDS service organizations (ASOs) and Older American Act programs may provide needed support if done properly (Cox & Brennan-Ing, 2017).
Our analysis reveals that the components influencing poorer physical and mental health in this population include individual demographic characteristics such as income, education, and race/ethnicity, as well as intrapersonal and interpersonal influences. Our findings reinforce the impact of multimorbidity which can encompass substance abuse. It is estimated that high as 50% of persons living with HIV have current or past histories of substance use (Durvasula & Miller, 2014) and our data suggest substance use, even past use, is associated with depression. Integrated models of care that address mental health, physical health, and substance abuse histories should be made more widely available. Furthermore, our findings of the impact of anxiety on depression reinforce the need for more comprehensive care and the triple risk of these older gay and bisexual men living with HIV. In addition, historical and environmental impacts including experiences of lifetime victimization, death of partners, as well as sense of community may have lasting impacts on one’s physical and mental health and well-being. The methodology used in this study has considerable strengths including a large sample size and a similar comparison group of non-HIV infected individuals, both of which address concerns in previous comparative studies. This study, however, also has limitations in design and execution that need to be acknowledged. First, even though these survey data are from a longitudinal study, our analysis is cross-sectional and therefore no causal inferences can be made. Second, because the original study focused on LGBT older adults and not specifically those living with HIV infection, other potentially useful variables that are HIV specific were not available, such as detailed information about their use of active antiretroviral therapies (ART) and retention in HIV care. Third, HIV status is selfreport from the study participants and not clinically verified. In an earlier study, we tested self-report of HIV status by gay and bisexual older men compared with HIV status information provided by a primary health care provider and found no significant differences. Thus, we concluded that such self-report data are robust (Fredriksen-Goldsen, Kim, Muraco, & Mincer, 2009). Finally, in the current study we measured discrimination and victimization with retrospective recall. Therefore, the measurement may still be subjective to measurement errors, despite the fine psychometrics properties they displayed. It should be promising for future studies to draw on longitudinal data to determine temporal relationships and if trajectories of health disparities that were found to exist in one point in time accentuate as time progresses.
Conclusion
Older gay and bisexual men are at greater risk for health disparities compared with their heterosexual peers (Fredriksen-Goldsen et al., 2013). The findings from this analysis confirm that those older gay and bisexual men living with HIV infection experience heightened health disparities even compared with their HIV-negative counterparts, in the areas of poor general health, increased depressive symptomatology, and that they differ in demographic characteristics including age, income, education and race ethnicity, as well as in health-promoting and risk factors including victimization, resilience, and social support. Our analysis also reveals important protective factors including engagement within the LGBT community. It is clear from our analysis that older gay and bisexual men living with HIV experience heightened vulnerability and are a hidden and marginalized population within an existing marginalized population. Advocacy and program development can enhance community engagement, social support, and identify and treat mental health concerns to improve the lives of these older men.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG026526 (K. I. Fredriksen-Goldsen, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Andresen EM, Malmgren JA, Carter WB, & Patrick DL (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine, 10, 77–84. [PubMed] [Google Scholar]
- Beatie B, Mackenzie CS, & Chou K-L (2015). Health in HIV-positive middle-aged and older adults: Results from wave 2 of the national epidemiologic survey on alcohol and related conditions. Journal of Therapy and Management in HIV Infection, 3, 7–16. doi: 10.12970/2309-0529.2015.03.01.2 [DOI] [Google Scholar]
- Bowling A (2005). Just one question: If one question works, why ask several. Journal of Epidemiology and Community Health, 59, 342–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brault M (2008). Americans with disabilities: 2005 (Current population reports, P70-P117). Retrieved from https://www.census.gov/library/publications/2008/demo/p70-117.html
- Brennan M (2008). Older men living with HIV: The importance of spirituality. Generations, 32, 54–61. [Google Scholar]
- Burbank PM (2006). Vulnerable older adults: Health care needs and interventions. New York, NY: Springer. [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Physical activity: How much physical activity do older adults need? Retrieved from http://www.cdc.gov/physicalactivity/basics/older_adults/
- Centers for Disease Control and Prevention. (2016). HIV surveillance report, 28 Retrieved from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2016-vol-28.pdf [Google Scholar]
- Centers for Disease Control and Prevention. (2018a). HIV among people aged 50 and over. Retrieved from https://www.cdc.gov/hiv/group/age/olderamericans/index.html
- Centers for Disease Control and Prevention. (2018b). HIV Surveillance Report, 29 Retrieved from http://www.cdc.gov/hiv/library/reports/surveillance/ [Google Scholar]
- Centers for Disease Control and Prevention. (2018c). Diagnosis of HIV infection among adults aged 50 years and older in the United States and dependent areas 2011-2016. HIV Surveillance Supplemental Report, 23(5). Retrieved from http://www.cdc.gov/hiv/library/reports/surveillance/ [Google Scholar]
- Cox LE, & Brennan-Ing M (2017). Medical, social and supportive services for older adults with HIV In Brennan-Ing M & DeMarco R (Eds.), HIV and aging (vol. 42, pp. 204–221). Basel, Switzerland: Krager. [DOI] [PubMed] [Google Scholar]
- D’Augelli AR, & Grossman AH (2001). Disclosure of sexual orientation, victimization, and mental health among lesbian, gay, and bisexual older adults. Journal of Interpersonal Violence, 16, 1008–1027. [Google Scholar]
- Durvasula R, & Miller TR (2014). Substance abuse treatment in persons with HIV/AIDS: Challenges in managing triple diagnosis. Behavioral Medicine, 40, 43–52. doi: 10.1080/08964289.2013.866540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emlet CA (2006). An examination of the social networks and social isolation in older and younger adults living with HIV/AIDS. Health & Social Work, 31, 299–308. [DOI] [PubMed] [Google Scholar]
- Emlet CA, Brennan DJ, Brennenstuhl S, Rueda S, Hart TA, Rourke SB, & the OHTN Cohort Study Team. (2013). Protective and risk factors associated with stigma in a population of older adults living with HIV in Ontario Canada. AIDS Care, 25, 1330–1339. [DOI] [PubMed] [Google Scholar]
- Emlet CA, & Harris L (2018). Giving back is receiving: The role of generativity in successful aging among HIV-positive older adults. Journal of Aging and Health. Advance online publication. doi: 10.1177/0898264318804320 [DOI] [PubMed] [Google Scholar]
- Emlet CA, Harris L, Furlotte C, Brennan DJ, & Pierpaoli C (2016). “I’m happy in my life now, I’m a positive person”: Approaches to successful ageing in older adults living with HIV in Ontario, Canada. Ageing & Society, 37, 2128–2151. doi: 10.1017/S0144686X16000878 [DOI] [Google Scholar]
- Emlet CA, Shiu C-S, Kim H-J, & Fredriksen-Goldsen KI (2017). Bouncing back: Resilience and mastery among HIV-positive gay and bisexual older men. The Gerontologist, 57(S1), S40–S49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang X, Vincent W, Calabrese SK, Heckman TG, Sikkema KJ, Humphries DL, & Hansen NB (2015). Resilience, stress and life quality in older adults living with HIV/AIDS. Aging & Mental Health, 19, 1015–1021. doi: 10.1080/13607863.2014.1003287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Emlet CA, Kim H-J, Muraco A, Erosheva EA, & Goldsen J (2013). The physical and mental health of lesbian, gay male and bisexual (LGB) older adults: The role of key health indicators and risk and protective factors. The Gerontologist, 53, 664–675. doi: 10.1093/geront/gns123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Jen S, & Muraco A (2019). Iridescent life course: Review of LGBTQ aging research and blueprint for the future. Gerontology, 65, 253–274. doi: 10.1159/000493559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, & Kim H-J (2017). The science of conducting research with LGBT older adults: An introduction to Aging With Pride: National Health, Aging, Sexuality and Gender Study. The Gerontologist, 57(S1), S1–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim H-J, Barkan SE, Muraco A, & Hoy-Ellis CP (2013). Health disparities among lesbian, gay, and bisexual older adults: Results from a population-based study. American Journal of Public Health, 103, 1802–1809. doi: 10.2105/AJPH.2012.301110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim H-J, Emlet CA, Muraco A, Erosheva EA, Hoy-Ellis CP, … Petry H (2011). The aging and health report: Disparities and resilience among lesbian, gay, bisexual and transgender older adults. Seattle, WA: Institute for Multigenerational Health. [Google Scholar]
- Fredriksen-Goldsen KI, Kim H-J, Muraco A, & Mincer S (2009). Chronically ill midlife and older lesbians, gay men, and bisexuals and their informal caregivers: The impact of the social context. Journal of Sexuality Research and Social Policy, 6, 52–64. doi: 10.1525/srsp.2009.6.4.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, & Muraco A (2010). Aging and sexual orientation: A 25-year review of the literature. Research on Aging, 32, 372–413. doi: 10.1177/0164027509360355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Simoni JM, Kim H-J, Lehavot K, Walters KL, Yang J, … Muraco A (2014). The health equity promotion model—Reconceptualization of lesbian, gay, bisexual, and transgender (LGBT) health disparities. American Journal of Orthopsychiatry, 84, 653–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, Schoeni RF, Martin LG, & Cornman JC (2007). Chronic conditions and the decline in late-life disability. Demography, 44, 459–477. [DOI] [PubMed] [Google Scholar]
- Gaskins S, & Brown K (1997). Helping others: A response to HIV disease. Journal of the Association of Nurses in AIDS Care, 8(3), 35–39. [DOI] [PubMed] [Google Scholar]
- Gjesfjeld C Greeno C, & Kim K (2008). A confirmatory factor analysis of an abbreviated social support instrument: The MOS-SSS. Research on Social Work Practice, 18, 231–237. doi: 10.1177/1049731507309830 [DOI] [Google Scholar]
- Goulet JL, Fultz SL, Rimland D, Butt A, Gilbert C, & Justice AC (2007). Do patterns of comorbidity vary by HIV status, age and HIV severity? Clinical Infectious Diseases, 45, 1593–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greysen SR, Horwitz LI, Covinsky KE, Gordon K, Ohl M, & Justice AC (2013). Does social isolation predict hospitalization and mortality among HIV+ and uninfected older Veterans? Journal of the American Geriatrics Society, 61, 1456–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grodensky CA, Golin CE, Jones C, Mamo M, Dennis AC, Abernethy MG, & Patterson KB (2015). “I should know better”: The roles of relationships, spirituality, disclosure, stigma, and shame for older women living with HIV seeking support in the South. Journal of the Nurses Association in AIDS Care, 26, 12–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Golub S, Parsons J, Brennan M, & Karpiak S (2010). Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS Care, 22, 630–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman TG, & Halkitis PN (2014). Biopsychosocial aspects of HIV and aging. Behavioral Medicine, 40, 81–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, Gillis JR, & Cogan JC (2009). Internalized stigma among sexual minority adults: Insights from a social psychological perspective. Journal of Counseling Psychology, 56, 32–43. doi: 10.1037/a0014672 [DOI] [Google Scholar]
- Jamal A, Homa DM, O’Connor E, Babb SD, Caraballo RS, Singh T, … King BA (2015). Current cigarette smoking among adults—United States 2005-2014. Morbidity and Mortality Weekly Report, 64, 1233–1240. [DOI] [PubMed] [Google Scholar]
- Kimmel D, Rose T, & David S (2006). Lesbian, gay, bisexual, and transgender aging: Research and clinical perspectives. New York, NY: Columbia University Press. [Google Scholar]
- Lyons A, Pitts M, & Grierson J (2012). Exploring the psychological impact of HIV: Health comparisons of older Australian HIV-positive and HIV-negative gay men. AIDS and Behavior, 16, 2340–2349. [DOI] [PubMed] [Google Scholar]
- Mayfield W (2001). The development of an internalized homonegativity inventory for gay men. Journal of Homosexuality, 41, 53–76. [DOI] [PubMed] [Google Scholar]
- Mohr JJ, & Kendra MS (2011). Revision and extension of a multidimensional measure of sexual minority identity: The lesbian, gay and bisexual identity scale. Journal of Counseling Psychology, 58, 234–245. doi: 10.1037/a0022858 [DOI] [PubMed] [Google Scholar]
- Pathai S, Bajillan H, Landay AL, & High KP (2014). Is HIV a model of accelerated or accentuated aging? Journals of Gerontology: A Biological Sciences Medical Sciences, 69, 833–842. doi: 10.1093/gerona/glt168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Reddy KP, Kong CY, Hyle EP, Baggett T, Huang M, Parker RA, … Walensky P (2017). Lung cancer mortality associated with smoking and smoking cessation among people living with HIV in the United States. JAMA Internal Medicine, 177, 1613–1621. doi: 10.1001/jamainternmed.2017.4349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, & Stewart AL (1991). The MOS social support survey. Social Science & Medicine, 32, 705–714. [DOI] [PubMed] [Google Scholar]
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, & Bernard J (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15, 194–200. doi: 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- Sue DW, Capodilupo CM, Torino GC, Bucceri JM, Holder AM, & Esquilin M (2007). Racial microaggressions in everyday life: Implications for clinical practice. American Psychologist, 62, 271–286. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2013). Annual update of the HHS poverty guidelines. Federal Register, 78, 5182–5183. [Google Scholar]
- Wallace SP, Cochran SD, Durazo EM, & Ford CL (2011). The health of aging lesbian, gay and bisexual adults in California. Los Angeles, CA: UCLA Center for Health Policy Research; Retrieved from http://www.healthpolicy.ucla.edu/pubs/files/aginglgbpb.pdf [PMC free article] [PubMed] [Google Scholar]
- Wing EJ (2016). HIV and aging. International Journal of Infectious Diseases, 53, 61–68. [DOI] [PubMed] [Google Scholar]
- Wong C, Althoff K, & Gange SJ (2014). Identifying an appropriate comparison group for HIV-infected individuals. Current Opinion in HIV and AIDS, 9, 379–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, & Chen Q (2010). Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research, 37, 197–206. doi: 10.1086/651257 [DOI] [Google Scholar]


