Abstract
Objective/Background:
Insufficient and/or poor-quality sleep may contribute to poor social emotional well-being, and vice versa, among young children who have experienced maltreatment. This study examined longitudinal associations between sleep and social emotional functioning among a sample of infants and toddlers from families involved with Child Protective Services (CPS) for maltreatment.
Participants:
Participants were 123 parents and their infant or toddler (baseline age 10 to 24 months) from families referred to CPS for maltreatment.
Methods:
Data were collected at baseline and at 3, 6 and 9 months post-baseline. At all time points, parents completed a questionnaire about their child’s social emotional functioning including internalizing behavior, externalizing behavior, and competence in social emotional skills and social relatedness. At 3 months post-baseline, parents reported about their child’s sleep problems and daily napping behavior.
Results:
Higher baseline externalizing behavior was associated with a greater propensity for sleep problems at 3 months post-baseline. Sleep problems at 3 months post-baseline were associated with higher internalizing and higher externalizing behavior at 9 months post-baseline. Daily napping at 3 months post-baseline was associated with lower internalizing behavior, lower externalizing behavior, and higher competence at 9 months post-baseline.
Conclusions:
Among this sample of young children from families involved with CPS for maltreatment, parents’ concerns about their child having a sleep problem longitudinally associated with children’s internalizing and externalizing behavior. Children’s daily napping behavior longitudinally associated with later internalizing behavior, externalizing behavior, and competence.
Keywords: napping, sleep problems, social emotional development, Child Protective Services, early childhood
Obtaining insufficient and/or poor-quality sleep may contribute to poorer social emotional well-being in children, and vice versa. Longitudinally, experiencing more social emotional challenges including greater depressive symptoms is associated with children’s later sleep problems including lower sleep quality and quantity (Kelly & El-Sheikh, 2014). Conversely, children’s sleep problems including difficulties falling asleep, difficulties staying asleep, and/or obtaining insufficient sleep are longitudinally associated with later social emotional challenges including greater internalizing (e.g., anxiety, depression) and/or externalizing (e.g., aggression, inattention) behavior (Jansen et al., 2011; Mindell, Leichman, DuMond, & Sadeh, 2016; Sadeh et al., 2015; Sivertsen et al., 2015; Touchette et al., 2007). In young children (ages 30 to 36 months), missing a usual nap also contributes to greater emotional and behavioral self-regulation difficulties (Berger, Miller, Seifer, Cares, & LeBourgeois, 2012; Miller, Seifer, Crossin, & Lebourgeois, 2014). Obtaining adequate, good-quality sleep – including daytime sleep in young children – is thus likely an important factor contributing to children’s social emotional functioning, and vice versa.
Experiencing maltreatment, including abuse and neglect, can negatively impact children’s sleep and social emotional functioning, however. Compared to children without maltreatment experiences, those with maltreatment experiences take longer to fall asleep at night (Glod, Teicher, Hartman, & Harakal, 1997) and have poorer quality sleep (Glod et al., 1997; Sadeh et al., 1995). Experiencing maltreatment is also a risk factor for lower emotion regulation and greater internalizing and externalizing behavior (Kim & Cicchetti, 2010). Studies examining longitudinal associations between sleep and social emotional functioning among young children who have experienced maltreatment are lacking, however. This is an important gap in knowledge, as there is a consensus that maltreatment negatively impacts children across multiple developmental domains (Cicchetti & Toth, 2015; Shonkoff & Phillips, 2000; Jones Harden & Klein, 2011; Stahmer et al., 2005), but just how poor sleep could be associated with poor social emotional functioning over time among children who have experienced maltreatment is poorly understood.
The purpose of this study was to address this gap in knowledge by examining longitudinal associations between sleep (parent-perceived sleep problems and daily napping behavior) and social emotional functioning (internalizing behavior, externalizing behavior, and competence in social emotional skills and social relatedness) in young children (baseline age 10 to 24 months) from families involved with Child Protective Services (CPS) for maltreatment. We were specifically interested in whether children’s initial social emotional functioning would be associated with later sleep and, if so, whether sleep would then, in turn, be associated with children’s later developmental trajectories of social emotional functioning, while controlling for child age and sex. It was hypothesized that lower baseline levels of internalizing and externalizing behavior would be associated with decreased parent-perceived sleep problems and increased daily napping which, in turn, would be associated with more favorable developmental trajectories (e.g., slower rates of increase, lower final levels) of internalizing and externalizing behavior. It was also hypothesized that higher baseline levels of competence would be associated with decreased parent-perceived sleep problems and increased daily napping which, in turn, would be associated with more favorable developmental trajectories (e.g., faster rates of increase, higher final levels) of competence.
Methods
Design and Participants
This was a secondary analysis of data from a larger longitudinal randomized controlled trial testing a parenting intervention among biological parents and their 10- to 24-month-old child (Oxford, Spieker, Lohr, & Fleming, 2016). Dyads were invited to participate if a recent, open case of maltreatment for a child in their family had been recorded at one of five Washington State CPS offices. Inclusion criteria were: Parents were English-speaking, had a child between the ages of 10 and 24 months, and resided in the target study area (greater Seattle, WA area). Only one child per family was enrolled in this study. In most cases (87%), the enrolled child was the victim of the maltreatment report. In the remaining cases (13%), the enrolled child was a sibling of the reported victim.
Parents who agreed to participate provided written informed consent and were randomized to receive either the parenting intervention (the treatment group) or a resource and referral service (the control group). The parenting intervention, which has been described in detail elsewhere (Kelly, Sandoval, Zuckerman, & Buehlman, 2003, 2008; Kelly, Zuckerman, & Rosenblatt, 2008; Kelly, Zuckerman, Sandoval, & Buehlman, 2016), has been shown to be associated with improvements in children’s sleep problems (Hash et al., 2019; Oxford, Fleming, Nelson, Kelly, & Spieker, 2013; Spieker, Oxford, Kelly, Nelson, & Fleming, 2012). Therefore, only those assigned to the resource and referral group (N = 123) were included in the present study. Parents in the resource and referral group received three brief telephone calls from a social service provider to identify and discuss their family’s needs. Housing, education, financial support, household items, and parenting support were the primary needs identified among the families in this study. Parents in the resource and referral group also received a mailed packet of information about local resources.
Baseline demographic characteristics for the resource and referral group have been reported in detail elsewhere (see Oxford and colleagues, 2016). Briefly, children were, on average, 16.8 months of age (SD = 4.6 months) and 42% female. Of the children, 59% were White or Caucasian, 35% mixed or other, 4% Black or African American, 2% American Indian or Alaska Native, and 1% Asian. Between birth and enrollment, 0.8% of the children had experienced at least one allegation of abandonment, 80% had experienced at least one allegation of neglect, 24% had experienced at least one allegation of physical abuse, and 4% had experienced at least one allegation of sexual abuse. Parents were, on average, 27.0 years of age (SD = 6.3 years) and 91% female. Of the parents, 77% were White or Caucasian, 11% mixed or other, 6% Black or African American, 3% Asian, and 2% American Indian or Alaska Native. The majority of families received food stamps (81%). Average yearly household income was $24,174 (SD = $25,468).
Procedure
Data were collected by trained in-home research visitors masked to treatment assignment. Four visits were conducted at approximately 3-month intervals including baseline (T1), 3 months post-baseline (T2), 6 months post-baseline (T3), and 9 months post-baseline (T4). At all time points, parents were given a questionnaire about their child’s social emotional functioning. At T2, parents were also given a questionnaire about their child’s sleep.
Some children experienced a caregiver change over the course of the study, and their new caregiver was invited to enroll in the study and provide data on the study child. A total of n = 3, n = 6, and n = 8 children had another caregiver participating in this study with them at T2, T3, and T4, respectively. Data were not collected from birth parents if the child was living with another caregiver. For the purposes of this secondary analysis, we include data reported by birth parents only. We do not mix birth parent reports with that of new caregiver reports.
This study was conducted in accordance with Washington State IRB approval.
Measures
Parent-perceived sleep problems
Parent-perceived sleep problems were measured using one item from the Sadeh (2004) Brief Infant Sleep Questionnaire (BISQ). This item asked whether parents thought their child’s sleep was a problem over the past 2 weeks (0 = not a problem at all, 1 = a small problem and 2 = a very serious problem). For the purposes of this study, responses were dichotomized (0 = not a problem v. 1 = a small or very serious problem), as only 2.8% (n = 3) indicated a very serious problem. Prior studies have used a similar single-item approach to measuring parent-perceived sleep problems (Covington, Armstrong, & Black, 2018; Sadeh, Mindell, & Rivera, 2011).
Daily napping behavior
Daily napping behavior was measured with one parent-reported item asking, “Does your child take a nap every day?” (0 = no, 1 = yes).
Social emotional functioning
The Infant-Toddler Social Emotional Assessment (ITSEA; Carter & Briggs-Gowan, 2006) and the Brief Infant-Toddler Social Emotional Assessment (BITSEA; Briggs-Gowan & Carter, 2002) questionnaires were used to measure children’s social emotional functioning including internalizing behavior, externalizing behavior and competence. Parents were asked to indicate, on a three-point rating scale (from 0 = not true/rarely to 2 = very true/often), how well statements described their child’s feelings and behaviors (Briggs-Gowan & Carter, 2002; Carter & Briggs-Gowan, 2006). The ITSEA yields a raw domain score for children’s internalizing behavior (composed of four subscales including depression/withdrawal, general anxiety, separation distress, and inhibition to novelty) and externalizing behavior (composed of three subscales including activity/impulsivity, aggression/defiance, and peer aggression; Carter & Briggs-Gowan, 2006). For the purposes of this study, one item addressing sleep was excluded from the calculation of the internalizing domain score. The BITSEA yields a competence total score indicating age-expected proficiency in social emotional skills, such as prosocial behavior and empathy, as well as social relatedness (composed of the sum of 11 items; Briggs-Gowan & Carter, 2002). Validity and reliability of the ITSEA and BITSEA are well established (Briggs-Gowan & Carter, 1998; Briggs-Gowan, Carter, Irwin, Wachtel, & Cicchetti, 2004; Carter, Briggs-Gowan, Jones, & Little, 2003). Internal consistency for the internalizing domain, externalizing domain, and competence total scores in this study ranged from α = .66 - .79, α = .85 - .87, and α = .61 - .71, respectively.
Control variables
T1 child age (months) and sex (0 = female, 1 = male) were included as control variables.
Analytic Approach
First, descriptives and correlations among study variables (parent-perceived sleep problems, daily napping behavior, internalizing behavior, externalizing behavior, competence, and the control variables) were examined. Next, preliminary analyses of unconditional two-factor (intercept and slope) latent growth models were conducted each for internalizing behavior, externalizing behavior, and competence. The observed T2 - T4 raw ITSEA/BITSEA scores were used to define the latent growth factors, and time was coded to define the intercept at T4 with equal spacing between assessments. This coding scheme made the intercept interpretable as average social emotional functioning at T4 and the slope interpretable as average rate of change in social emotional functioning every 3 months from T2 to T4. In the case of the unconditional internalizing and externalizing behavior models (see Supplemental Table) the means of the intercepts were significant, indicating that the T4 levels of internalizing and externalizing behavior were, on average, significantly different from zero. The unconditional internalizing and externalizing behavior models also showed non-significant means of the slopes, indicating that there was no significant increase or decrease, on average, in internalizing or externalizing behavior over time. However, variance on the intercept and slope factors in the internalizing and externalizing behavior models was significant, indicating significant variance could be predicted in the conditional models. In the case of the competence model, variance on the slope factor was close to zero and nonsignificant (p = .826). We therefore specified an alternative model in lieu of a growth model in our main analyses for competence (discussed in greater detail below).
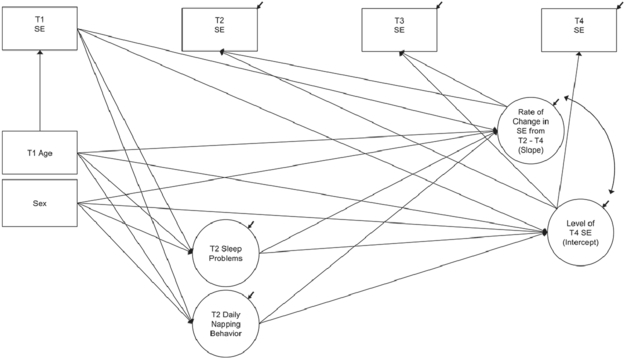
Next, we conducted our main analyses. We first examined a conditional latent growth path model each for internalizing and externalizing behavior, controlling for age and sex. Paths were specified as shown in Figure 1. Weighted least squares means and variances adjusted estimation with the theta parameterization was used, which treated the binary mediators as continuous latent response variables (Muthén, Muthén, & Asparouhov, 2016). Second, we conducted a multiple linear regression with standard predictor entry predicting T4 competence (in lieu of a conditional latent growth path model). T1 competence, the T2 sleep variables (parent-perceived sleep problems and daily napping behavior), and the control variables (T1 age and sex) were entered as predictors into the regression model. Parameter estimates were obtained using maximum likelihood estimation.
Figure 1.
Statistical representation of the conditional latent growth path model examining relations between sleep and social emotional functioning, controlling for child age and sex. T1 = baseline, T2 = 3 months post-baseline, T3 = 6 months post-baseline, T4 = 9 months post-baseline. SE = social emotional functioning (internalizing or externalizing behavior).
Descriptives and correlations among study variables were examined in IBM SPSS Version 19 using default missing data procedures, which included listwise treatment of missing data in descriptive analyses and pairwise treatment in correlation analyses. All other analyses were conducted in Mplus Version 7.31 (Muthén & Muthén, 1998-2015) using data from all cases, including those with partially missing data. We requested that Mplus include all cases by: (a) regressing T1 behavior on T1 age in the conditional latent growth path models as shown in Figure 1 and (b) modeling covariate missingness in the regression model. Missing data were then estimated by default Mplus procedures (Muthén & Muthén, 1998-2015).
Results
Descriptives and Correlations
Table 1 shows means, standard deviations, and zero-order correlations among the study variables. Of the parents, 26% reported concern that their child had a sleep problem. Eighty-four percent of parents reported that their child took a daily nap. Having a parent-perceived sleep problem was correlated significantly with higher T2 - T4 internalizing and externalizing behavior. Taking a daily nap was correlated significantly with lower T3 - T4 internalizing behavior, lower T4 externalizing behavior, and higher T4 competence.
Table 1.
Descriptives and Zero-Order Correlations Among Study Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 internalizing | -- | |||||||||||||||
| 2. T2 internalizing | .58** | -- | ||||||||||||||
| 3. T3 internalizing | .52** | .69** | -- | |||||||||||||
| 4. T4 internalizing | .39** | .51** | .67** | -- | ||||||||||||
| 5. T1 externalizing | .28** | .18 | .13 | .14 | -- | |||||||||||
| 6. T2 externalizing | .33** | .41** | .27** | .34** | .59** | -- | ||||||||||
| 7. T3 externalizing | .18 | .29** | .42** | .41** | .42** | .64** | -- | |||||||||
| 8. T4 externalizing | .18 | .20 | .25* | .44** | .42** | .59** | .73** | -- | ||||||||
| 9. T1 competence | .19* | .12 | .03 | −.01 | −.10 | −.15 | −.23* | −.28 | -- | |||||||
| 10. T2 competence | −.04 | .05 | .00 | −.04 | −.16 | −.27** | −.32** | −.33** | .61** | -- | ||||||
| 11. T3 competence | .08 | .06 | −.10 | −.13 | −.09 | −.19 | −.34** | −.28** | .57** | .59** | -- | |||||
| 12. T4 competence | −.09 | −.11 | −.23* | −.38** | −.32** | −.35** | −.47** | −.59** | .49** | .55** | .48** | -- | ||||
| 13. T2 sleep problems | .16 | .24* | .33** | .27** | .18 | .28** | .32** | .30** | −.07 | −.05 | −.02 | −.16 | -- | |||
| 14. T2 naps | −.14 | −.15 | −.22* | −.26* | −.08 | −.19 | −.13 | −.22* | −.05 | .07 | .05 | .22* | −.11 | -- | ||
| 15. T1 child age | .39** | .16 | .12 | .10 | .08 | −.06 | −.16 | −.09 | .54** | .29** | .34** | .17 | .02 | −.34** | -- | |
| 16. Child sex | −.05 | −.12 | .00 | .04 | .02 | .11 | .14 | .16 | −.05 | −.20* | −.16 | −.20* | .05 | −.15 | −.04 | -- |
| Mean | 0.49 | 0.53 | 0.49 | 0.49 | 0.59 | 0.62 | 0.64 | 0.64 | 16.30 | 17.37 | 17.41 | 17.78 | 0.26 | 0.84 | 16.78 | 0.58 |
| (SD) | 0.21 | 0.23 | 0.22 | 0.30 | 0.31 | 0.30 | 0.35 | 0.36 | 3.56 | 2.93 | 2.93 | 2.95 | 0.44 | 0.36 | 4.55 | 0.50 |
Note. T1 = baseline, T2 = 3 months post-baseline, T3 = 6 months post-baseline, T4 = 9 months post-baseline. Internalizing and externalizing = Infant-Toddler Social and Emotional Assessment raw domain scores. Competence = Brief Infant-Toddler Social and Emotional Assessment raw total scores. Sleep problems dummy coded 0 = no parent-perceived sleep problem, 1 = a small or very serious parent-perceived sleep problem. Naps dummy coded 0 = does not nap daily, 1 = naps daily. Child age = months. Child sex dummy coded 0 = female, 1 = male.
p < .05
p < .01.
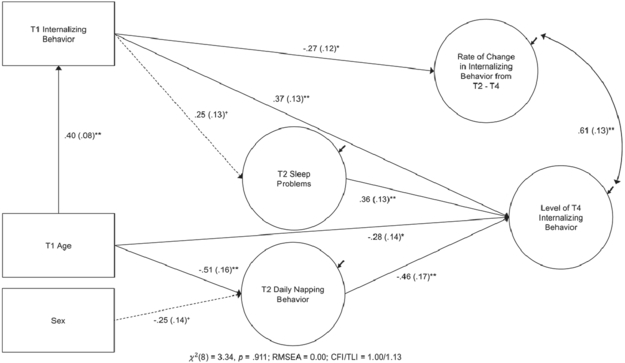
Relations Between Sleep and Internalizing Behavior
Figure 2 shows the results for the conditional two-factor latent growth path model examining parent-perceived sleep problems, daily napping behavior, and internalizing behavior while controlling for age and sex. Higher T1 internalizing behavior was associated with higher T4 levels of internalizing behavior. Higher T1 internalizing behavior was also associated with lower T2 - T4 rates of change in internalizing behavior (a decrease, on average, in internalizing behavior over time). T2 parent-perceived sleep problems was associated with more T4 internalizing behavior. T2 daily napping was associated with lower T4 internalizing behavior.
Figure 2.
Results for the conditional latent growth path model with sleep problems, daily napping behavior, and internalizing behavior while controlling for child age and sex. N = 123. Only paths with a p-value of < .10 shown. Solid arrows indicate paths significant at p < .05. Dashed arrows indicate paths trending toward significance at p < .10. Path coefficients standardized, standard errors in parentheses. T1 = baseline, T2 = 3 months post-baseline, T3 = 6 months post-baseline, T4 = 9 months post-baseline. Age = age in months. Sex dummy coded 0 = female, 1 = male. RMSEA = Root Mean Square Error. CFI = Comparative Fit Index. TLI = Tucker-Lewis Index. Observed T2 - T4 internalizing behavior variables omitted for clearer presentation.
+p < .10, *p < .05, **p < .01.
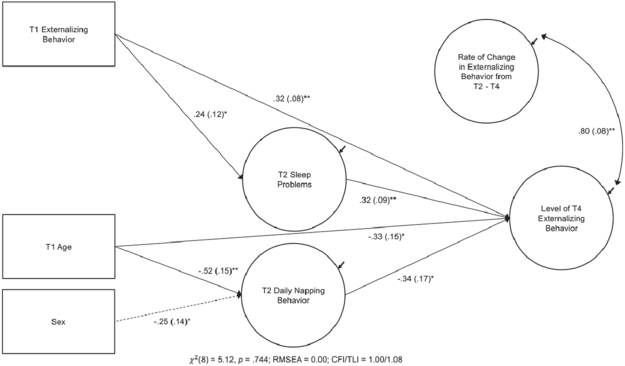
Relations Between Sleep and Externalizing Behavior
Figure 3 shows the results for the conditional two-factor latent growth path model examining parent-perceived sleep problems, daily napping behavior, and externalizing behavior while controlling for age and sex. Higher T1 externalizing behavior was associated with higher levels of T4 externalizing behavior. Higher T1 externalizing behavior was also associated with greater T2 parent-perceived sleep problems. T2 parent-perceived sleep problems was associated with greater T4 levels of externalizing behavior. T2 daily napping was associated with lower T4 externalizing behavior.
Figure 3.
Results for the conditional latent growth path model with sleep problems, daily napping behavior, and externalizing behavior while controlling for child age and sex. N = 123. Only paths with a p-value of < .10 shown. Solid arrows indicate paths significant at p < .05. Dashed arrow indicates path trending toward significance at p < .10. Path coefficients standardized, standard errors in parentheses. T1 = baseline, T2 = 3 months post-baseline, T3 = 6 months post-baseline, T4 = 9 months post-baseline. Age = age in months. Sex dummy coded 0 = female, 1 = male. RMSEA = Root Mean Square Error. CFI = Comparative Fit Index. TLI = Tucker-Lewis Index. Observed T2 - T4 externalizing behavior variables omitted for clearer presentation.
+p < .10, *p < .05, **p < .01.
Relations Between Sleep and Competence
Table 2 shows the results for the multiple linear regression predicting children’s T4 competence. Taking a T2 daily nap was associated with higher T4 competence.
Table 2.
Multiple Linear Regression with Standard Predictor Entry Predicting T4 Competence
| R2 | p | β | (SE) | p | |
|---|---|---|---|---|---|
| .30 | <.001 | ||||
| Intercept | 3.64 | (0.68) | <.001 | ||
| T2 sleep problems | −.10 | (.09) | .293 | ||
| T2 napping behavior | .20 | (.09) | .027 | ||
| T1 competence | .49 | (.09) | <.001 | ||
| T1 child age | −.01 | (.10) | .894 | ||
| Child sex | −.12 | (.09) | .163 |
Note. N = 123. T1 = baseline, T2 = 3 months post-baseline, T4 = 9 months post-baseline. Competence = Infant-Toddler Social and Emotional Assessment raw total score. Sleep problems dummy coded 0 = no parent-perceived sleep problem, 1 = a small or very serious parent-perceived sleep problem. Daily napping behavior dummy coded 0 = does not nap daily, 1 = naps daily. Child age = months. Child sex dummy coded 0 = female, 1 = male.
Discussion
This study fills an important gap in knowledge about longitudinal associations between sleep and social emotional functioning among young children from families involved with CPS for maltreatment. There were two key findings from this study. First, we found that parent-perceived sleep problems longitudinally associated with children’s internalizing and externalizing behavior, but not competence. Second, we found that children’s daily napping behavior longitudinally associated with later internalizing behavior, externalizing behavior, and competence.
Regarding the first finding about children’s parent-perceived sleep problems, our results specifically showed that externalizing behavior at baseline associated with parent-perceived sleep problems 3 months later. In turn, parent-perceived sleep problems associated with externalizing behavior another 6 months later, even while controlling for baseline externalizing behavior. This pattern suggests that children’s sleep problems, as perceived by their parents, may indicate new, enduring or worsening externalizing behavior challenges over time. A similar pattern was evidenced between children’s parent-perceived sleep problems and internalizing behavior, although the association between baseline internalizing behavior and T2 parent-perceived sleep problems did not reach significance at the p < .05 level. It may be that inadequate and/or poor-quality sleep plays a larger role in contributing to internalizing behavior problems than internalizing behavior problems do of sleep problems. This interpretation is consistent with prior work showing that children’s sleep more strongly predicts internalizing behavior than internalizing behavior does of sleep (Jansen et al., 2011; Mindell et al., 2016). In contrast, we found no relation between children’s parent-perceived sleep problems and competence, suggesting that parents’ general concerns about their child having a sleep problem related more strongly to internalizing and externalizing behavior challenges than to difficulties in social emotional skill proficiency and social relatedness.
Findings about naps indicated that children’s daily napping behavior longitudinally associated with all three domains of social emotional functioning 6 months later including internalizing behavior, externalizing behavior, and competence, even while controlling for baseline social emotional functioning. Interestingly, our findings also show that, although there was this longitudinal association, the concurrent correlation between daily napping behavior and T2 social emotional functioning was not significant. What is interesting about this finding is, presumably, if acutely tired toddlers have more trouble regulating their emotions (Berger et al., 2012), then concurrent associations between children’s daily napping behavior and social emotional functioning should be just as strong, if not stronger, than longitudinal associations. Why significant associations between daily napping and social emotional functioning evidenced a time delay in this study is therefore intriguing. It may be that daily napping played a role in setting the stage for later, but not immediate, social emotional functioning among these children. It may also be that the daily napping variable in this study functioned as a proxy indicator for other important factors. For instance, it may have been that children who napped daily also experienced factors such as greater structure and organization in the home, or different parenting strategies. These other factors may help explain why daily napping related to later social emotional functioning in this study. Further research is needed to better understand this phenomenon of a delay in the association between daily napping behavior and social emotional functioning.
Children also vary in their need for daytime naps. Some children respond more poorly to missing naps than others (Berger et al., 2012), and not all children stop napping at the same age (Iglowstein, Jenni, Molinari, & Largo, 2003; Weissbluth, 1995). Among children in this study, some may have been less inclined to nap daily because they were developmentally ready to give up daily naps. Others may have been less likely to nap for reasons other than a natural readiness to stop daily napping, such as life stressors that place demands on families and disrupt children’s sleep routines (Weissbluth, 1995). Families involved with CPS encounter higher rates of stressors including poverty and domestic violence compared to the general population (Campbell, Thomas, Cook, & Keenan, 2012). An interesting hypothesis, therefore, is that the association between daily napping behavior and later social emotional functioning was stronger among the children in this study who needed a daily nap and didn’t get it but weaker or nonsignificant among those who did not need daily naps. It may be that missing daily naps for reasons other than a developmental readiness to stop napping (such as competing life stressors) could, much like a canary in a coal mine, be an early sign of risk for later social emotional problems.
Regarding naps, it is also important to recognize that there is a strong developmental trend in early childhood napping behavior. Prior work has indicated that 100% of 12-month-olds take one (or more) naps per day, but by age 36 months, only 50% of children still take one nap per day (Iglowstein et al., 2003). Our data show a similar developmental trend. Among the children in this study (who ranged in age from 13 to 33 months at the T2 time point, when daily napping behavior was measured), there was a negative association between daily napping behavior and child age. This is in line with the tendency for children to drop naps as they get older.
We found no relation between children’s sleep, including parent-perceived sleep problems and daily napping behavior, and rate of change (the slope factor) in T2 - T4 internalizing and externalizing behavior. Neither a slowing nor a hastening of growth over time in these domains of social emotional functioning thus associated with children’s sleep. Although both parent-perceived sleep problems and daily napping behavior were uniquely associated with T4 levels of internalization and externalization (the intercept factor), neither of these variables associated with rate of change.
This study has potential clinical and service implications. Findings from this study point to the possibility that sleep health promotion could be an integral component in the promotion of social emotional well-being, and vice versa, among young children from families involved with CPS for maltreatment. For example, some families involved with CPS may benefit from help in initiating and maintaining healthy sleep routines. These routines could have immediate and long-term benefits to the child, reduce parental distress, and provide an early parenting success that becomes a foundation for more intensive parenting interventions that may be needed (see Mindell and Williamson, 2018, and Mindell, Li, Sadeh, Kwon, and Goh, 2015, for the benefits of bedtime routines). Home visiting services may also provide support to families. As noted earlier, prior research with the Promoting First Relationships home visiting program suggests that a home visiting model could be a feasible and effective way of reducing parent-perceived sleep problems among young children involved with CPS (Hash et al., 2019) and child welfare (Oxford et al., 2013; Spieker et al., 2012). Further research into programs that promote sleep health among young children with maltreatment experiences is needed.
Strengths and Limitations
There are some limitations of this study that deserve comment. First, we were unable to control for baseline parent-perceived sleep problems and daily napping behavior, as children’s sleep was not measured at baseline in this study. Second, parent-perceived sleep problems, daily napping behavior, and social emotional functioning were all measured by parent report, which may have been biased and may have produced shared variance. For the daily napping behavior variable, however, the lack of correlation with concurrent social emotional functioning (but significant correlation with later social emotional functioning) suggests minimal shared variance between these reports. Third, we did not control for all possible confounders. Future studies including additional potential confounders, such as type and/or degree of maltreatment, would help address this limitation. Fourth, parent-perceived sleep problems and daily napping behavior were measured using one dichotomized item each, not by multiple indictors. These items did not capture nuances (e.g., sleep behaviors that parents had concerns about, timing and/or duration of naps). Future studies including subjective measures (e.g., parent-reported concerns) and objective measures (e.g., actigraphy) would help shed light on this limitation. Finally, we did not have a comparison group of children from families without a CPS maltreatment referral.
This study also has a number of strengths. First, the longitudinal design allowed for the examination of relations between sleep and the development of social emotional functioning over time. Repeated measures of social emotional functioning also allowed for the assessment of developmental trajectories of behavior over time. Second, the ITSEA/BITSEA was designed specifically for use among infants and toddlers (Briggs-Gowan & Carter, 1998) and, as such, was developmentally appropriate for this population. Third, the vulnerable population of infants and toddlers from families with a CPS maltreatment report was also a strength of this study, as it addressed an important gap in knowledge about the interdependence of sleep and social emotional functioning in this population. Finally, parent-reported sleep is clinically meaningful, as parents’ perceptions are integral to the clinical evaluation of pediatric sleep problems (Mindell & Owens, 2015).
Conclusion
This study addressed an important gap in knowledge about longitudinal associations between sleep and social emotional functioning in a sample of infants and toddlers from families involved with CPS for maltreatment. Findings show that parents’ general concerns about their child having a sleep problem longitudinally associated with two domains of social emotional functioning including internalizing and externalizing behavior. Findings also show that children’s daily napping behavior longitudinally associated with three domains of later social emotional functioning including internalizing behavior, externalizing behavior, and competence.
Supplementary Material
Acknowledgements
We thank the parents and children who participated in this study, and their families. We also thank editor David Preston for his assistance.
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development under Grant R01 HD061362; the Eunice Kennedy Shriver National Institute of Child Health and Human Development under Grant U54HD083091; the National Institutes of Health, National Institute of Nursing Research Omics and Symptom Science Training Program at the University of Washington under Grant T32NR016913; the National Institutes of Health, National Institute of Nursing Research, Center for Innovation in Sleep Self-Management under grant P30NR016585; and the University of Washington Warren G. Magnuson Scholarship Award. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development under Grant R01 HD061362; the Eunice Kennedy Shriver National Institute of Child Health and Human Development under Grant U54HD083091; the National Institute of Nursing Research under Grant T32016913; and the University of Washington Warren G. Magnuson Scholarship Award.
Footnotes
Disclosure Statement
The authors have no conflicts of interest to disclose.
Contributor Information
Jonika B. Hash, Department of Biobehavioral Nursing & Health Informatics, University of Washington
Monica L. Oxford, Department of Family & Child Nursing, University of Washington
Charles B. Fleming, Department of Psychiatry & Behavioral Sciences, University of Washington
Teresa M. Ward, Department of Psychosocial & Community Health, University of Washington
Susan J. Spieker, Department of Family & Child Nursing, University of Washington
References
- Berger RH, Miller AL, Seifer R, Cares SR, & LeBourgeois MK (2012). Acute sleep restriction effects on emotion responses in 30- to 36-month-old children. Journal of Sleep Research, 21, 235–246. doi: 10.1111/j.1365-2869.2011.00962.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan M, & Carter AS (2002). Brief Infant-Toddler Social and Emotional Assessment (BITSEA) manual (version 2.0 ed.). New Haven, CT: Yale University. [Google Scholar]
- Briggs-Gowan MJ, & Carter AS (1998). Preliminary acceptability and psychometrics of the Infant-Toddler Social and Emotional Assessment (ITSEA): A new adult-report questionnaire. Infant Mental Health Journal, 19, 422–445. doi: [DOI] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, & Cicchetti DV (2004). The Brief Infant-Toddler Social and Emotional Assessment: Screening for social-emotional problems and delays in competence. Journal of Pediatric Psychology, 29, 143–155. doi: 10.1093/jpepsy/jsh017 [DOI] [PubMed] [Google Scholar]
- Campbell KA, Thomas AM, Cook LJ, & Keenan HT (2012). Longitudinal experiences of children remaining at home after a first-time investigation for suspected maltreatment. The Journal of Pediatrics, 161, 340–347. doi: 10.1016/j.jpeds.2012.02.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter AS, & Briggs-Gowan M (2006). ITSEA: Infant-Toddler Social and Emotional Assessment Examiner’s Manual. San Antonio, TX: Pearson. [Google Scholar]
- Carter AS, Briggs-Gowan MJ, Jones SM, & Little TD (2003). The Infant-Toddler Social and Emotional Assessment (ITSEA): Factor structure, reliability, and validity. Journal of Abnormal Child Psychology, 31, 495–514. doi: 10.1023/A:1025449031360 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2015). Multilevel developmental perspectives on child maltreatment. Development and Psychopathology, 27, 1385–1386. doi: 10.1017/s0954579415000814 [DOI] [PubMed] [Google Scholar]
- Covington LB, Armstrong B, & Black MM (2018). Perceived Toddler Sleep Problems, Co-sleeping, and Maternal Sleep and Mental Health. Journal of Developmental & Behavioral Pediatrics, 39, 238–245. doi: 10.1097/dbp.0000000000000535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glod CA, Teicher MH, Hartman CR, & Harakal T (1997). Increased nocturnal activity and impaired sleep maintenance in abused children. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 1236–1243. doi: 10.1097/00004583-199709000-00016 [DOI] [PubMed] [Google Scholar]
- Hash JB, Oxford ML, Fleming CB, Ward TM, Spieker SJ, & Lohr MJ (2019). Impact of a home visiting program on sleep problems among young children experiencing adversity. Child Abuse & Neglect, 89, 143–154. doi: 10.1016/j.chiabu.2018.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iglowstein I, Jenni OG, Molinari L, & Largo RH (2003). Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics, 111, 302–307. doi: 10.1542/peds.111.2.302 [DOI] [PubMed] [Google Scholar]
- Jansen PW, Saridjan NS, Hofman A, Jaddoe VW, Verhulst FC, & Tiemeier H (2011). Does disturbed sleeping precede symptoms of anxiety or depression in toddlers? The Generation R study. Psychosomatic Medicine, 73, 242–249. doi: 10.1097/PSY.0b013e31820a4abb [DOI] [PubMed] [Google Scholar]
- Jones Harden B, & Klein S (2011). Infants/toddlers in child welfare: What have we learned and where do we go from here? Children and Youth Services Review, 33, 1464–1468. doi: 10.1016/j.childyouth.2011.04.021 [DOI] [Google Scholar]
- Kelly JF, Sandoval D, Zuckerman TG, & Buehlman MA (2003). Promoting First Relationships: A program for service providers to help parents and other caregivers nurture young children’s social and emotional development. Seattle, WA: NCAST Programs. [Google Scholar]
- Kelly JF, Sandoval D, Zuckerman TG, & Buehlman MA (2008). Promoting First Relationships: A program for service providers to help parents and other caregivers nurture young children’s social and emotional development (2nd Ed ed.). Seattle, WA: NCAST Programs. [Google Scholar]
- Kelly JF, Zuckerman T, & Rosenblatt S (2008). Promoting First Relationships: A relationship-focused early intervention approach. Infants & Young Children, 21, 285–295. doi: 10.1097/01.IYC.0000336541.37379.0e [DOI] [Google Scholar]
- Kelly JF, Zuckerman TG, Sandoval D, & Buehlman MA (2016). Promoting First Relationships: A program for service providers to help parents and other caregivers nurture young children’s social and emotional development (3rd ed.). Seattle, WA: NCAST Programs. [Google Scholar]
- Kelly RJ, & El-Sheikh M (2014). Reciprocal relations between children’s sleep and their adjustment over time. Developmenal Psychology, 50, 1137–1147. doi: 10.1037/a0034501 [DOI] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry, 51, 706–716. doi: 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AL, Seifer R, Crossin R, & Lebourgeois MK (2014). Toddler’s self-regulation strategies in a challenge context are nap-dependent. Journal of Sleep Research, 24, 279–287. doi: 10.1111/jsr.12260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell JA, Leichman ES, DuMond C, & Sadeh A (2016). Sleep and social-emotional development in infants and toddlers. Journal of Clinical Child & Adolescsent Psychology, 46, 236–246. doi: 10.1080/15374416.2016.1188701 [DOI] [PubMed] [Google Scholar]
- Mindell JA, Li AM, Sadeh A, Kwon R, & Goh DY (2015). Bedtime routines for young children: A dose-dependent association with sleep outcomes. SLEEP, 38, 717–722. doi: 10.5665/sleep.4662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell JA, & Owens JA (2015). A clinical guide to pediatric sleep: Diagnosis and management of sleep problems (3rd ed.). Philadelphia, PA: Wolters Kluwer. [Google Scholar]
- Mindell JA, & Williamson AA (2018). Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Medicine Reviews, 40, 93–108. doi: 10.1016/j.smrv.2017.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK, & Asparouhov T (2016). Regression and mediation analysis using Mplus. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Muthén LK, & Muthén BO (1998-2015). Mplus user’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Oxford ML, Fleming CB, Nelson EM, Kelly JF, & Spieker SJ (2013). Randomized trial of Promoting First Relationships: Effects on maltreated toddlers’ separation distress and sleep regulation after reunification. Children and Youth Services Review, 35, 1988–1992. doi: 10.1016/j.childyouth.2013.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford ML, Spieker SJ, Lohr MJ, & Fleming CB (2016). Promoting First Relationships®: Randomized trial of a 10-week home visiting program with families referred to Child Protective Services. Child Maltreatment, 21, 267–277. doi: 10.1177/1077559516668274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh A (2004). A brief screening questionnaire for infant sleep problems: Validation and findings for an Internet sample. Pediatrics, 113, e570–e577. doi: 10.1542/peds.113.6.e570 [DOI] [PubMed] [Google Scholar]
- Sadeh A, De Marcas G, Guri Y, Berger A, Tikotzky L, & Bar-Haim Y (2015). Infant sleep predicts attention regulation and behavior problems at 3-4 years of age. Developmental Neuropsychology, 40, 122–137. doi: 10.1080/87565641.2014.973498 [DOI] [PubMed] [Google Scholar]
- Sadeh A, McGuire JP, Sachs H, Seifer R, Tremblay A, Civita R, & Hayden RM (1995). Sleep and psychological characteristics of children on a psychiatric inpatient unit. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 813–819. doi: 10.1097/00004583-199506000-00023 [DOI] [PubMed] [Google Scholar]
- Sadeh A, Mindell J, & Rivera L (2011). “My child has a sleep problem”: A cross-cultural comparison of parental definitions. Sleep Medicine, 12, 478–482. doi: 10.1016/j.sleep.2010.10.008 [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, & Phillips DA (Eds.). (2000). From neurons to neighborhoods: The science of early childhood development. Washington, D.C.: National Academy Press. [PubMed] [Google Scholar]
- Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen L, Ystrom E, & Hysing M (2015). Later emotional and behavioral problems associated with sleep problems in toddlers: A longitudinal study. JAMA Pediatrics, 169, 575–582. doi: 10.1001/jamapediatrics.2015.0187 [DOI] [PubMed] [Google Scholar]
- Spieker SJ, Oxford ML, Kelly JF, Nelson EM, & Fleming CB (2012). Promoting First Relationships: Randomized trial of a relationship-based intervention for toddlers in child welfare. Child Maltreatment, 17, 271–286. doi: 10.1177/1077559512458176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer AC, Leslie LK, Hurlburt M, Barth RP, Webb MB, Landsverk J, & Zhang J (2005). Developmental and behavioral needs and service use for young children in child welfare. Pediatrics, 116, 891–900. doi: 10.1542/peds.2004-2135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touchette E, Petit D, Séguin JR, Boivin M, Tremblay RE, & Montplaisir JY (2007). Associations between sleep duration patterns and behavioral/cognitive functioning at school entry. SLEEP, 30, 1213–1219. doi: 10.1093/sleep/30.9.1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissbluth M (1995). Naps in children: 6 months-7 years. Sleep, 18, 82–87. doi: 10.1093/sleep/18.2.82 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.