Abstract
Objective:
Hypertension is largely asymptomatic and, as a result, patients often fail to sufficiently engage in medication adherence and other health behaviors to control their blood pressure (BP). This study explores the mechanisms by which MyBP, an automated SMS-facilitated home blood pressure monitoring (HBPM) program, helps facilitate healthy behavior changes.
Methods:
A thematic analysis of transcribed audio-recordings from semi-structured post-intervention interviews (n=40) was conducted.
Results:
Three primary themes were identified as contributing most to patients’ decision to initiate a behavior change: 1) increased hypertension literacy attributed to educational videos presented at enrollment, 2) increased day-to-day salience of blood pressure levels as a result of consistent HBPM, and 3) use of BP readings as feedback, with high readings triggering motivations to make behavior changes. These themes and most accompanying sub-themes correspond to constructs in the Health Belief Model and Social Cognitive Theory.
Conclusion:
Patient-centered HBPM interventions such as MyBP appear to promote improvements in hypertension self-management via several mechanisms consistent with recognized models of behavior change.
Practice Implications:
SMS-supported HBPM, paired with video-based education, may provide a simple and scalable way of encouraging health behavior adherence in hypertensive patients.
Keywords: Behavior Change, Hypertension, Qualitative, Text-messaging, Home Blood Pressure Monitoring
1. Introduction
Outpatient management and control of high blood pressure (BP) remains a challenge.[1] Home blood pressure monitoring (HBPM) is now widely recommended and, when combined with additional support such as educational resources or tele-monitoring, is effective in lowering BP.[2-4] However, practitioners lack practical aids to facilitate HBPM. Given the ubiquity of mobile phones, there is great potential to leverage this technology to support HBPM interventions among diverse populations, including underserved groups such as African-Americans and rural patients in whom hypertension is often poorly controlled.[5-7] Intervention studies that employ short message service (SMS, commonly known as text-messaging) to facilitate regular HBPM in hypertensive patients have shown promising results.[8-10] However, existing programs involve additional non-automated communications and healthcare resources that make them difficult to implement in real-world settings. Therefore, a fully automated SMS system providing HBPM support with personalized feedback for patients is desirable.
Based upon these considerations, we developed and tested the feasibility of MyBP. As described in detail elsewhere,[11] multiple stakeholders identified barriers and facilitators to hypertension self-management. One key component was the necessity to address hypertension literacy, which encompasses both patients’ factual knowledge about the disease and the ability to apply that knowledge to guide decision-making.[12] Therefore, MyBP begins with hypertension education delivered at the patient’s convenience via commercially-available videos. In addition, stakeholders noted low patient awareness of their BP and low self-efficacy around BP self-management. Thus, MyBP provides fully automated messaging to assist patients in systematic BP measurement and tracking, including generation of personalized BP reports. To test program fidelity, uptake and engagement, patients from various outpatient settings were invited to use MyBP for 6 weeks. The quantitative analysis of this study revealed a high rate of scheduled BP measurement and 88% of patients reported interest in using the program long-term. In addition, patients frequently reported making changes in diet, exercise, stress reduction, and medication adherence.[11]
The mechanism by which HBPM lowers BP is poorly understood. Routine monitoring may provide patients and physicians with information needed to appropriately titrate medications.[13] Also, increased awareness of one’s BP may lead patients to improve their adherence to medication regimens, recommended lifestyle modifications, or both.[14, 15] Qualitative studies exploring patients’ experiences with HBPM have noted that many patients will attempt to change a health behavior such as diet, exercise, or medication adherence as a consequence of self-monitoring.[16-19] While these studies allude to behavior change, none has focused specifically on exploring the mechanisms by which HBPM interventions can encourage patients to make lifestyle changes.
We have postulated that supporting self-management through MyBP may stimulate patients to make healthy behavior changes through mechanisms articulated within the Health Belief Model, specifically by increasing perceived susceptibility to the complications of hypertension, and by providing a “cue to action” through SMS-prompted BP readings and personalized feedback.[11, 20] In the feasibility study mentioned above, we conducted post-intervention interviews to explore the effects of MyBP on participants’ cognitions related to hypertension, self-monitoring, and the role of health behaviors in BP control. Here, we present an inductive thematic analysis examining how and why the MyBP program impacted participants’ motivation to participate in hypertension self-care activities. We then use this empirical information along with health behavior change theories to revise our conceptual model of the effects of MyBP on hypertension-relevant health behaviors.
2. Methods
2.1. Participants:
Participants were recruited from three sites: an urban emergency department, a primary care clinic, and a clinic which specializes in hypertension management. Participants were eligible if they were 18 years of age or older, had an EMR-confirmed diagnosis of hypertension, an arm circumference <48 cm, and a mobile phone with unlimited text messaging. Those with neuropsychiatric disorders precluding independence in texting and hypertension self-care were not approached. Participants received a $30 debit-card after completing both the six-week study and the exit interview. All participants provided signed, informed consent and the study was approved by the University of Pittsburgh Investigational Review Board (PRO14110100).
2.2. Sample characteristics:
Current clinical BP, BMI, and prescription medications were abstracted from the medical record. Participant socio-demographic characteristics and baseline BP self-monitoring were self-reported.
2.3. MyBP Program and Pilot Study:
Box 1 outlines the design and features of the MyBP program. The primary aim of the pilot study was to determine whether MyBP can be successfully deployed and whether patients would engage with the program. Upon recruitment, patients registered their phone numbers in the MyBP system, and were instructed to watch the six educational videos. Three to five days later, a research assistant called to confirm that the videos had been viewed via a short quiz and finalized system enrollment. Participants then used MyBP for six weeks without routine intervention from the research team. At study completion, a research assistant conducted a semi-structured interview regarding their experiences with MyBP. This qualitative study is a secondary analysis of the interviews.
Box 1. Summary of MyBP Intervention.
The MyBP intervention consisted of two key components: 1) Hypertension education delivered via online videos, and 2) Automated, bidirectional, logic-based text-messages facilitating home blood pressure monitoring with personalized feedback.
At enrollment, participants were provided access and instructed to watch six short videos on hypertension at their convenience (See Appendix A for a summary of video content).
MyBP was initiated on participants’ phones by sending a text to the MyBP phone number.
Automated texting for BP self-monitoring was initiated after a brief phone call with a research assistant, during which the participants selected two mornings and two evenings to receive an HBPM prompt at the days and times of their choosing.
Each text prompt instructed patients to take a BP measurement and reply with the systolic and diastolic values. After submitting a BP, the system sent an automatic reply acknowledging the submission and providing the patient with an updated rolling average of their BP.
Every two weeks, a summary report was sent to participants providing: 1) their adherence to responding to the HBPM prompts, 2) their average systolic & diastolic pressure over the two-week period and a statement as to whether this was above or below the general recommendation of <140/<90, and 3) how much their BP had changed since initiating the program (See Appendix B for example screenshots of the MyBP program).
Following each two-week report, participants received a text message option to continue using the program or suspend monitoring for two weeks.
The program also sent an educational “health tip” once per week.
2.4. Exit Interviews:
Interviews were conducted over the phone by author JE, a male research assistant. The interview, lasting 15-20 minutes on average, consisted of semi-structured questions about the overall experience with the MyBP program and engagement in hypertension self-management, including BP self-monitoring, diet, physical activity, stress reduction, and medication adherence. The interview also explored whether MyBP participants changed their attitudes, beliefs, or behaviors as a result of the program, and if so, what about the program spurred these changes (see Appendix C to view the interview guide). A single interview was conducted with all willing participants, rather than stopping at the point of data saturation, for the purpose of conducting a content analysis with interview data.
2.5. Coding & Thematic Analysis:
The interviews were audiotaped and transcribed verbatim. Organization and coding of transcript data was performed using Atlas.ti 7.5 software. A thematic analysis following the steps outlined by Braun and Clarke[21] was employed. The primary investigator (author MA, a male medical student) used an inductive coding approach with an in depth reading and re-reading of the transcripts and the application of “in vivo” codes from specific text segments pertinent to the research question, as well as categorical codes of behaviors and attitudes expressed by participants.[22] Then, a second researcher (author TI, a female post-doctoral researcher) independently coded each interview, made suggestions for revisions and additions, and confirmed that codes accurately captured the ideas being expressed. Discussions between the two coders continued until consensus was reached.
Once the consensus codes were applied, the two coders collaboratively performed a broader thematic analysis. This step involved arranging codes into wider themes using various iterations of conceptual maps in order to help visualize the potential relationships between codes and themes. This map of themes was then organized into a conceptual model of how the MyBP program may facilitate behavior changes. Finally, participant quotes were selected as illustrative examples to support the analysis.
The second coder, while familiar with the MyBP study, was not involved in its creation or implementation, and thus was chosen to help ensure that the coding was consistent and credible. The two coders were blinded to the primary results of the quantitative study, which focused on differences in participant adherence to SMS-prompts.[11]
2.6. Application to Conceptual Model:
The results of the thematic analysis were then compared to pertinent theories in the health behavior change literature, with the goal of identifying constructs in those models which were analogous to our themes and sub-themes.[20, 23-26] This information was incorporated to revise our conceptual model depicting how use of MyBP affects patients’ health behaviors.
3. Results
3.1. Study Flow and Participants Characteristics
A total of 57 patients signed informed consents to participate in the pilot study, of which 14 decided not to enroll. Of the 43 enrolled, 40 participants completed the exit interview. The three participants who did not complete the interview had withdrawn from the MyBP program and could not be reached by phone. See Table 1 for participants’ characteristics.
Table 1.
Description of participants
| Characteristics | n=40 |
|---|---|
| Age, mean (s.d.) | 55 (8.5) |
| Sex, n (% female) | 23 (58%) |
| Race, n (% black) | 24 (60%) |
| Education, n (%) | |
| High school only | 14 (35%) |
| Some college/technology training | 12 (30%) |
| Bachelors or higher | 14 (35%) |
| Body mass index, kg/m2 (s.d.) | 33 (5.9) |
| Systolic BP, mean (s.d.) | 158 (24) |
| Diastolic BP, mean (s.d.) | 94 (14) |
| Number of antihypertensive medications, mean (s.d.) | 2.1 (1.4) |
| Owned a BP cuff, n (%) | 12 (32 %)a |
| Checked own BP in past month, n (%) | 17 (43%) |
s.d., standard deviation; BP, blood pressure
n=38
3.2. Thematic Analysis
The final thematic analysis includes three overarching themes: Hypertension Literacy, Day-to-Day Salience of BP, and BP Readings as Behavioral Feedback. Each theme and related subthemes are detailed below.
3.3. Theme 1 – Hypertension Literacy
3.3.1. Increased Hypertension Knowledge
Participants watched educational videos on hypertension. For those patients who believed they already knew the content, they felt that the videos had no impact on them. However, many participants had little to no knowledge about hypertension, and cited these videos as an influential part of their decisions to ultimately make a health behavior change.
“When they were describing how your arteries extended themselves widthwise and lengthwise, made that pressured, it makes the blood pressure what it is... I didn’t understand [systolic & diastolic] on the machine until then... [The videos] made me feel like I could have a better understanding of my body and what was going on with it and how I could get into some kind of regimen of improving things.”(63yo F)
Other participants stated that while they felt they had a good working knowledge of hypertension prior to the study, they believed the videos filled gaps in their knowledge.
“They showed a lot of points where I had been negligent in doing, with my blood pressure and what have you, so I thought they were great.”(66yo F)
3.3.2. Increased Awareness of Hypertension as a Risk to Health
In conjunction with increased knowledge, participants often stated that this intervention changed their beliefs about hypertension. The primary change participants noted was that the videos made them more cognizant of how hypertension negatively impacts health and life expectancy.
“[The videos] scared me a little bit, to realize how it works like that. But sometimes being scared about something is good, if you take the appropriate actions to, you know, get yourself together. Scared straight, let’s call it that.”(64yo M)
“Yeah, [the program] sort of made me understand a little bit more how serious my blood pressure is. You know, to keep it on the lower side, you know... Knowing that it can cause other health issues, stroke and all that stuff. I’ve taken it a bit more seriously now.”(53yo F)
3.3.3. Increased Awareness of BP-Behavior Connection
Another key component of hypertension literacy is understanding that health behaviors have a major impact on BP. As expected, many participants stated that the videos increased their knowledge of certain health behaviors and the relationship between those behaviors and BP.
“That’s why I said I took it nonchalant, I was thinking my blood pressure as long as I take my medicine will be fine. I didn’t know that there was a lot more to be added to it.”(54yo M)
3.3.4. Understanding BP Variability
One ancillary goal of the MyBP program is to help patients with hypertension develop a better understanding of the fact that BP varies over time, with the hope that patients would understand this as a natural and relatively benign phenomenon. This was not directly addressed in the educational videos, rather it was assumed that participants might develop this understanding intuitively through the program’s emphasis on showing participants’ their average BP. Indeed, many did state something to this effect during their interviews.
“When you’re doing your blood pressures yourself, you’re just seeing one number at a time. I’m not tracking my averages. I’m just looking at one number at a time. But, having the averages like kind of given to you, it’s like, “Oh, okay,” this is how I’ve been doing the last few weeks. It’s the more significant number, I think.”(48yo F)
In contrast, some participants checked their BP more often than MyBP requested, usually around once or twice per day in addition to the regularly scheduled four times per week. Some did this simply because they were curious, but a couple participants cited some degree of anxiety about the variability of their BP as the reason for excess monitoring.
“I think for most people two days might be good for them. But like for me I wanted to know if my pressure was really high. I really wanted to know where I was.”(51yo F)
3.4. Theme 2 – Day-to-Day Salience of BP
3.4.1. Increased BP Awareness
A central goal of this intervention was to help patients be more cognizant of their BP. The majority of study participants did not routinely check their BP prior to starting the program, and several stated that their BP would only be checked during health care visits.
“[The program] made me more aware of [my blood pressure] because before I wasn’t checking it, I wasn’t thinking about it.”(40yo F)
“[Taking a blood pressure] was something that the doctor did and would tell me, oh it’s high or it’s low and I just, I couldn’t remember the numbers”(67yo F)
3.4.2. Increased Hypertension Relevance
Once participants became more aware of their BP through home monitoring, many found themselves being more conscientious of their hypertension. These participants stated that hypertension became a more relevant part of their day-to-day life and how they think about their health.
“[The program] made me more attentive to what I was doing, it made me think about it more and actually, you know, just doing the day to day—just a lot of times you think about in the day to day, and get busy, you just don’t be conscious of what you’re doing, but it makes you slow down and think about it, I can’t do this, I gotta do this,you know.”(40yo F)
3.4.3. Text Messages as Behavioral Nudge
MyBP was designed to regularly prompt hypertensive patients to check their BP. Intriguingly, a few participants noted that the HBPM-reminder text messages also prompted them to engage in other hypertension self-management behaviors.
“I’m just not a good medicine-taker. So when I got that text I knew to do that. I wish I could get text messages that say take your medicine, you know. That would help.”(46yo F)
“The overall consistency of you guys texting me, letting me know that it’s time, it made [me] more aware—getting up earlier, going to the gym, working out, coming home, eating properly.”(46yo M)
3.5. Theme 3 – BP Readings as Behavioral Feedback
3.5.1. High Readings as Trigger for Change
When participants were asked why they made a behavior change, a large number of participants indicated that seeing a high or up-trending BP reading directly prompted them to change a health behavior in order to lower their BP.
“Because when I’m seeing those high numbers, I’m taking [my BP medication] as prescribed. Before I would just take it any time in the day. Now I take it in the morning, and I take my second one in the afternoon.”(47yo M)
“[I made dietary changes] because I didn’t want my blood pressure to be high. And I wanted to have a good reading every time.”(52yo M)
“Well, when I saw when I used the salt that my pressure was higher... it showed me that you have to let go of some of the things that you’re used to... I don’t know why, but I guess when you’re told not to use something rather than to be shown not to use, it’s a whole different outlook on it.”(62yo F)
3.5.2. Improved Readings as Positive Reinforcement
Conversely, multiple participants discussed how seeing "good" or down-trending BP readings helped reinforce the positive steps they had taken to lower their BP.
“My blood pressure is a little better than I believed that it was, and then being that it was better and I was proud of myself, it made me want to keep it like that, or go a little lower, so I’ve been slowly cutting out a few things.”(51yo F)
“It made me a little more on the excited side to know that I was in compliance. And that the fourteen medicines I’m taking today are working! [laughs] And that, you know, obviously cutting back my salt, and my food choices are also working.”(52yo F)
3.5.3. BP Feedback Prompting Behavioral Experimentation
Some participants experimented with multiple different behavior changes they believed might help lower their BP. These patients tended to look for direct cause-and-effect relationships between certain behaviors and high readings.
“[Taking my BP] at different times let me know the different things I was doing around that time, which would cause me to change what I was doing so it wouldn’t be so high.”(34yo F)
“So, you get an understanding, okay, you’re slowly going up, so you need to, you know, dial back the diet, or push up the exercise, or do something, because it’s going in the wrong direction.”(51yo M]
3.5.4. Increased Confidence in Maintaining Healthy Behavior Changes
Finally, of those participants who attempted to change a health behavior, the majority affirmed that they were now more confident in their ability to adopt and maintain that change.
“[I’m] more confident because I’m doing it, I’m slowly working on it every day.”(51yo F)
“Now that the weather is warmed up, I’ll be doing some walking a little bit and finding out, ‘Oh, well this ain’t so hard and you’re kind of liking it,’ you know?”(67yo F)
3.6. Phenomena Explained Using Models of Behavior Change
The MyBP program’s original conceptual model[11] was informed by the Health Belief Model,[20] and through the current analysis we recognized the additional utility of Social Cognitive Theory (SCT).[23] The themes and sub-themes identified above have analogous constructs in one or both of these theories of health behavior, as displayed in Table 2.
Table 2.
MyBP behavior change themes and related behavior change theories.
| Theme/Subtheme | Construct | Theoretical Framework |
|---|---|---|
| Increased Health Literacy | ||
| Hypertension Knowledge | Perceived Benefits | Health Belief Model |
| Hypertension as Threat to Health | Perceived Susceptibility Perceived Seriousness |
Health Belief Model Health Belief Model |
| Awareness of BP-Behavior Connection | Self-Observation | Social Cognitive Theory |
| Increased Day-to-Day Salience of BP | ||
| BP Awareness | Self-Observation | Social Cognitive Theory |
| BP Relevance | Self-Observation | Social Cognitive Theory |
| Text Messages as “Nudge” | Cues to Action | Health Belief Model |
| BP Readings as Behavioral Feedback | ||
| High Readings as Trigger for Change | Cues to Action Self-Evaluation |
Health Belief Model Social Cognitive Theory |
| Improved Readings as Positive Reinforcement | Self-Evaluation | Social Cognitive Theory |
| Increased Confidence in Making Changes | Self-Efficacy/Perceived Behavioral Control | Multiple theoretical models |
We then used these observations collectively to inform revisions to our conceptual model (Figure 1). Many participants who made behavior changes indicated that the prerequisite videos changed their understanding about risks of high BP and the actions they could take to mitigate those risks, consistent with HBM.[20] The other essential component of HBM is the “Cue to Action”, a concept which aligns well with those who stated that either the SMS reminders or the BP readings themselves nudged them towards making healthier choices.[20] Constructs from SCT, specifically the concepts of self-observation and self-evaluation, accounted for a number of our subthemes not otherwise explained by HBM.[23] Our final subtheme, “increased confidence”, can be correlated to the concept of “self-efficacy” found in both HBM and SCT, along with the construct of “perceived behavioral control” found in the Theory of Planned Behavior.[25, 27]
Figure 1: Conceptual Model of the MyBP Program Impact on Health Behaviors.
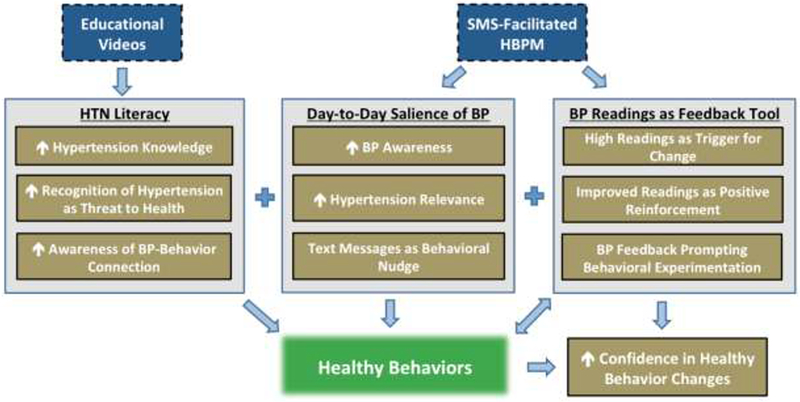
This illustrates the authors’ conception of how the study’s identified themes and subthemes impact health behaviors. MyBP components are depicted in blue tiles, the model’s psychological constructs in tan, and the outcome of interest in green. Educational videos increased participants’ hypertension literacy, a key building block in making health behavior changes. Consistent self-monitoring led to increased day-to-day salience of participants’ BP. Finally, participants used BP readings as self-evaluative feedback, with high readings stimulating a desire to make behavior changes which might lower their BP. Together, these features increased confidence to maintain changes in health behaviors.
4. Discussion and conclusion
4.1. Discussion
In a pilot study of the MyBP program, the presentation of educational videos at baseline, followed by systematic BP self-monitoring, catalyzed efforts to change health behaviors among many participants. To better understand how MyBP impacts patients’ hypertension self-care, we undertook this qualitative study and identified three overarching themes which participants stated encouraged healthy behavior change: increasing hypertension literacy, increasing day-to-day salience of one’s BP, and using BP readings as behavioral feedback. These findings have been arranged into a conceptual model, with the intent of informing the design of both future iterations of MyBP and other hypertension-management interventions.
Other qualitative studies have examined the impact of HBPM interventions. None was a clear analog to MyBP, as these interventions did not rely heavily on automated communication and varied widely in terms of provider oversight and the use of educational materials. While prior studies did not focus on behavior change, some had findings which correlate to ours. Themes related to hypertension literacy such as understanding of health risks, BP-behavior connection, and BP variability were often cited in this literature.[13, 19, 28] Patients using BP readings as feedback on their health behaviors have also been noted.[16, 17] Increasing day-to-day salience of one’s BP appears to be a unique finding derived from our interview data, providing further insight into the mechanisms by which consistent HBPM facilitates health behavior change.
Some qualitative studies note that HBPM can cause anxiety in a minority of patients, while most patients find home monitoring reassuring.[16, 17, 29] This study’s findings appear to be consistent with this literature. More research is warranted both to determine which patients are prone to anxiety with HBPM and to develop ways of mitigating that anxiety. Given the positive impact of MyBP video content, additional videos covering topics such as the benign nature of daily BP fluctuations may improve participant understanding. Such content could also be reinforced over SMS whenever a patient submits a BP reading significantly higher or lower than usual.
We initially hypothesized that MyBP would promote health behavior change by increasing health literacy and providing cues to action, as seen in Health Belief Model. However, our findings suggest that an essential aspect of interventions such as MyBP may be the consistency of self-monitoring, which not only keeps a patient’s BP at the forefront of his or her mind, but also allows the patient to observe trends in readings and gauge “performance.” These concepts fit better with the Social Cognitive Theory.[23] Intrinsically linked to patients’ self-observation of their BP is their personal evaluation of those readings which, according to Social Cognitive Theory, can be inherently motivating.[23] Applied to MyBP, when patients engaged in self-monitoring and noticed that their BP was incongruent with the standard goal, it often triggered a desire to have “better” readings. This, in turn, motivated some participants to achieve this goal through behavior change.
Published research suggests that SMS can be used to help manage and prevent lifestyle diseases such as hypertension in several ways, including medication reminders[30-32] and contextually relevant health education.[33-35] These interventions use text-messages as “cues to action” which directly target a specific health behavior. In contrast, results from this study suggest that prompting patients to measure their BP can indirectly target a range of health behaviors. Several participants mentioned changing more than one behavior, which may have an even greater impact on lowering BP and motivating sustained adherence.[36, 37] Interventions which engage patients through non-directive mechanisms of behavior change such as this may enhance their sense of self-efficacy in managing their own health, ultimately improving outcomes.[38]
The MyBP program utilizes a combination of functionalities commonly used in mobile phone-supported behavior change research: self-monitoring, performance feedback, and personalized messaging.[39] As noted, patients in this study often developed connections between healthy behaviors and BP intuitively based on BP reporting alone. Other research has found that patient-reported variation in health behaviors tracks with daily fluctuations in BP.[40] Therefore, the addition of behavior reporting to MyBP’s functionality might further enhance the role of BP readings as behavior feedback, allowing patients to make more precise and specific connections. In addition, MyBP might benefit from incorporating adaptive algorithms that respond to changes in behavior and outcomes.[41] For example, a participant could receive a decreased frequency of HBPM reminders if BP is below target, or vice-versa. Simple adaptive functions such as these could improve long-term adherence to the program by tailoring the intensity of the intervention to the needs of the patient.
The MyBP program described here lacks integration with the electronic medical record of their providers and associated health care systems. This limitation has been addressed in current versions of MyBP. Another limitation of this study was the use of an exit interview designed to collect both quantitative and qualitative data, requiring the use of some close-ended questions which may have narrowed participant conversations. For the same reason, there were no progressive alterations to the interview questions which may have increased richness of data. Also, participants were involved in the MyBP pilot study for six weeks; a longer duration of program use may reveal different results regarding both the benefits and possible frustrations associated with long-term HBPM.[42]
4.2. Conclusions
This investigation identified three mechanisms by which video education plus SMS-facilitated HBPM may improve hypertension self-management: increasing hypertension literacy, increasing day-to-day salience of one’s BP, and using BP readings as behavioral feedback. Further studies are needed to explore whether this intervention can sustain such changes long term, as well as objective evidence of improved hypertension self-management and related health outcomes.
4.3. Practice Implications
Fully automated hypertension self-management programs such as MyBP appear to increase patient engagement with their own health care. SMS-facilitated HBPM, in conjunction with video-based education, may provide an efficient and easily scalable approach to promote healthy behaviors in hypertensive patients.
Supplementary Material
Highlights.
Automated text-based HBPM program encourages healthy lifestyle choices
Complementary educational videos increase patients’ knowledge of hypertension
SMS-supported HBPM improves awareness of one’s BP
BP readings act as feedback on health behaviors and medication adherence
Acknowledgements:
Special thanks to the following:
Patients from the three clinical study sites for serving as volunteer study participants.
Mr. Jack Doman for designing and programming the automated SMS system.
Kevan C Schultz and his associates at the University of Pittsburgh Center for Social and Urban Research for their assistance with coding the participant interviews.
Emmi Solutions, Inc. for creating the hypertension education videos which were used through a lease agreement with UPMC Health System.
Funding: The UPP Academic Foundation; NIH T32 Training Grant (5 T32 HL 7560-33)
This study’s funding source had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Prior Presentations:
Allen M, Einhorn J, Suffoletto B, Burke L, Kamarck TA, Rollman BL, Muldoon MF. Self-management Support for Patients with Hypertension Using Online Videos and Automated, Bi-directional Text-Messaging. American Psychosomatic Society Annual Meeting. March 15-18, 2017; Seville, Spain.
Allen M, Irizarry T, Einhorn J, Suffoletto B, Kamarck T, Burke L, Rollman B, Muldoon MF. Text-facilitated home blood pressure monitoring: A qualitative analysis of health behavior change. AHA Council on Hypertension Annual Scientific Meeting. September 6-9, 2018; Chicago, IL.
Declarations of Interest: None
Matthew Allen: None
Taya Irizarry: None
Julian Einhorn: None
Thomas Kamarck: None
Brian Suffoletto: None
Lora Burke: None
Bruce Rollman: None
Matthew Muldoon: None
Patient Details: I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
References
- [1].Booth JN 3rd, Li J, Zhang L, Chen L, Muntner P, Egan B, Trends in Prehypertension and Hypertension Risk Factors in US Adults: 1999-2012, Hypertension 70(2) (2017) 275–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM, Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis, Ann. Intern. Med. 159(3) (2013) 185–94. [DOI] [PubMed] [Google Scholar]
- [3].Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr., Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr., Williamson JD, Wright JT Jr., 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, Hypertension 71(6) (2018) 1269–1324. [DOI] [PubMed] [Google Scholar]
- [4].Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, Earle K, George J, Godwin M, Green BB, Hebert P, Hobbs FDR, Kantola I, Kerry SM, Leiva A, Magid DJ, Mant J, Margolis KL, McKinstry B, McLaughlin MA, Omboni S, Ogedegbe O, Parati G, Qamar N, Tabaei BP, Varis J, Verberk WJ, Wakefield BJ, McManus RJ, Self-monitoring of blood pressure in hypertension: A systematic review and individual patient data meta-analysis, PLoS Med. 14(9) (2017) e1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ricciardi L, Mostashari F, Murphy J, Daniel JG, Siminerio EP, A national action plan to support consumer engagement via e-health, Health Aff. (Millwood) 32(2) (2013) 376–84. [DOI] [PubMed] [Google Scholar]
- [6].Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA Jr., Willis M, Yancy CW, Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association, Circulation 136(21) (2017) e393–e423. [DOI] [PubMed] [Google Scholar]
- [7].Bale B, Optimizing hypertension management in underserved rural populations, J. Natl. Med. Assoc. 102(1) (2010) 10–7. [DOI] [PubMed] [Google Scholar]
- [8].Cottrell E, Chambers R, O'Connell P, Using simple telehealth in primary care to reduce blood pressure: a service evaluation, BMJ Open 2(6) (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kiselev AR, Gridnev VI, Shvartz VA, Posnenkova OM, Dovgalevsky PY, Active ambulatory care management supported by short message services and mobile phone technology in patients with arterial hypertension, J. Am. Soc. Hypertens. 6(5) (2012) 346–55. [DOI] [PubMed] [Google Scholar]
- [10].Logan AG, Irvine MJ, McIsaac WJ, Tisler A, Rossos PG, Easty A, Feig DS, Cafazzo JA, Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics, Hypertension 60(1) (2012) 51–7. [DOI] [PubMed] [Google Scholar]
- [11].Irizarry T, Allen M, Suffoletto BP, Einhorn J, Burke LE, Kamarck TW, Rollman BL, Muldoon MF, Development and Preliminary Feasibility of an Automated Hypertension Self-Management System, Am. J. Med. 131(9) (2018) 1125.e1–1125.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H, E. Consortium Health Literacy Project, Health literacy and public health: a systematic review and integration of definitions and models, BMC Public Health 12 (2012) 80–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Jones MI, Greenfield SM, Bray EP, Baral-Grant S, Hobbs FD, Holder R, Little P, Mant J, Virdee SK, Williams B, McManus RJ, Patients' experiences of self-monitoring blood pressure and self-titration of medication: the TASMINH2 trial qualitative study, Br. J. Gen. Pract. 62(595) (2012) e135–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Dickey RA, Janick JJ, Lifestyle modifications in the prevention and treatment of hypertension, Endocr. Pract. 7(5) (2001) 392–9. [DOI] [PubMed] [Google Scholar]
- [15].Fletcher BR, Hartmann-Boyce J, Hinton L, McManus RJ, The Effect of Self-Monitoring of Blood Pressure on Medication Adherence and Lifestyle Factors: A Systematic Review and Meta-Analysis, Am. J. Hypertens. 28(10) (2015) 1209–21. [DOI] [PubMed] [Google Scholar]
- [16].Abdullah A, Othman S, The influence of self-owned home blood pressure monitoring (HBPM) on primary care patients with hypertension: a qualitative study, BMC Fam. Pract. 12 (2011) 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hanley J, Ure J, Pagliari C, Sheikh A, McKinstry B, Experiences of patients and professionals participating in the HITS home blood pressure telemonitoring trial: a qualitative study, BMJ Open 3(5) (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fletcher BR, Hinton L, Hartmann-Boyce J, Roberts NW, Bobrovitz N, McManus RJ, Self-monitoring blood pressure in hypertension, patient and provider perspectives: A systematic review and thematic synthesis, Patient Educ. Couns. 99(2) (2016) 210–219. [DOI] [PubMed] [Google Scholar]
- [19].Lambert-Kerzner A, Havranek EP, Plomondon ME, Albright K, Moore A, Gryniewicz K, Magid DM, Ho PM, Patients' Perspectives of a Multifaceted Intervention With a Focus on Technology: A Qualitative Analysis, Circ. Cardiovasc. Qual. Outcomes 3(6) (2010) 668–674. [DOI] [PubMed] [Google Scholar]
- [20].Rosenstock IM, Historical Origins of the Health Belief Model, Health Educ. Monogr. 2(4) (1974) 328–335. [DOI] [PubMed] [Google Scholar]
- [21].Braun V, Clarke V, Using thematic analysis in psychology, Qual Res Psychol 3(2) (2006) 77–101. [Google Scholar]
- [22].Thomas D, A General Inductive Approach for Qualitative Data Analysis, 2003. [Google Scholar]
- [23].Bandura A, Social cognitive theory of self-regulation, Organ. Behav. Hum. Decis. Process. 50(2) (1991) 248–287. [Google Scholar]
- [24].Prochaska JO, Velicer WF, The Transtheoretical Model of Health Behavior Change, Am. J. Health Promot. 12(1) (1997) 38–48. [DOI] [PubMed] [Google Scholar]
- [25].Ajzen I, The theory of planned behavior, Organ. Behav. Hum. Decis. Process. 50(2) (1991) 179–211. [Google Scholar]
- [26].Winter SJ, Sheats JL, King AC, The Use of Behavior Change Techniques and Theory in Technologies for Cardiovascular Disease Prevention and Treatment in Adults: A Comprehensive Review, Prog. Cardiovasc. Dis. 58(6) (2016) 605–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Rosenstock IM, Strecher VJ, Becker MH, Social Learning Theory and the Health Belief Model, Health Educ. Q. 15(2) (1988) 175–183. [DOI] [PubMed] [Google Scholar]
- [28].Vasileiou K, Barnett J, Young T, Interpreting and acting upon home blood pressure readings: a qualitative study, BMC Fam. Pract. 14 (2013) 97–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Ovaisi S, Ibison J, Leontowitsch M, Cloud G, Oakeshott P, Kerry S, Stroke patients' perceptions of home blood pressure monitoring: a qualitative study, Br. J. Gen. Pract. 61(590) (2011) e604–e610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Bobrow K, Farmer AJ, Springer D, Shanyinde M, Yu LM, Brennan T, Rayner B, Namane M, Steyn K, Tarassenko L, Levitt N, Mobile Phone Text Messages to Support Treatment Adherence in Adults With High Blood Pressure (SMS-Text Adherence Support [StAR]): A Single-Blind, Randomized Trial, Circulation 133(6) (2016) 592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Buis L, Hirzel L, Dawood RM, Dawood KL, Nichols LP, Artinian NT, Schwiebert L, Yarandi HN, Roberson DN, Plegue MA, Mango LC, Levy PD, Text Messaging to Improve Hypertension Medication Adherence in African Americans From Primary Care and Emergency Department Settings: Results From Two Randomized Feasibility Studies, JMIR Mhealth Uhealth 5(2) (2017) e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Kamal AK, Shaikh Q, Pasha O, Azam I, Islam M, Memon AA, Rehman H, Akram MA, Affan M, Nazir S, Aziz S, Jan M, Andani A, Muqeet A, Ahmed B, Khoja S, A randomized controlled behavioral intervention trial to improve medication adherence in adult stroke patients with prescription tailored Short Messaging Service (SMS)-SMS4Stroke study, BMC Neurol. 15 (2015) 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Hacking D, Haricharan HJ, Brittain K, Lau YK, Cassidy T, Heap M, Hypertension Health Promotion via Text Messaging at a Community Health Center in South Africa: A Mixed Methods Study, JMIR Mhealth Uhealth 4(1) (2016) e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Partridge SR, McGeechan K, Hebden L, Balestracci K, Wong AT, Denney-Wilson E, Harris MF, Phongsavan P, Bauman A, Allman-Farinelli M, Effectiveness of a mHealth Lifestyle Program With Telephone Support (TXT2BFiT) to Prevent Unhealthy Weight Gain in Young Adults: Randomized Controlled Trial, JMIR Mhealth Uhealth 3(2) (2015) e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Pfaeffli Dale L, Whittaker R, Jiang Y, Stewart R, Rolleston A, Maddison R, Text Message and Internet Support for Coronary Heart Disease Self-Management: Results From the Text4Heart Randomized Controlled Trial, J. Med. Internet Res. 17(10) (2015) e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Meader N, King K, Wright K, Graham HM, Petticrew M, Power C, White M, Sowden AJ, Multiple Risk Behavior Interventions: Meta-analyses of RCTs, Am. J. Prev. Med. 53(1) (2017) e19–e30. [DOI] [PubMed] [Google Scholar]
- [37].Conn VS, Ruppar TM, Chase JA, Enriquez M, Cooper PS, Interventions to Improve Medication Adherence in Hypertensive Patients: Systematic Review and Meta-analysis, Curr. Hypertens. Rep. 17(12) (2015) 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Patrick H, Williams GC, Self-determination theory: its application to health behavior and complementarity with motivational interviewing, Int. J. Behav. Nutr. Phys. Act. 9 (2012) 18–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Zhao J, Freeman B, Li M, Can Mobile Phone Apps Influence People's Health Behavior Change? An Evidence Review, J. Med. Internet Res. 18(11) (2016) e287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Taft C, Hallberg I, Bengtsson U, Manhem K, Kjellgren K, Links between blood pressure and medication intake, well-being, stress, physical activity and symptoms reported via a mobile phone-based self-management support system: a cohort study in primary care, BMJ open 8(8) (2018) e020849–e020849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R, Health behavior models in the age of mobile interventions: are our theories up to the task?, Transl. Behav. Med. 1(1) (2011) 53–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Morton K, Dennison L, Bradbury K, Band RJ, May C, Raftery J, Little P, McManus RJ, Yardley L, Qualitative process study to explore the perceived burdens and benefits of a digital intervention for self-managing high blood pressure in Primary Care in the UK, BMJ Open 8(5) (2018) e020843. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


