Abstract
Medicinal plants are targeted in the search for new antimicrobial agents. Nowadays, there is an alarmingly increasing antimicrobial resistance to available agents with a very slow development of new antimicrobials. It is, therefore, necessary to extensively search for new agents based on the traditional use of herbal medicines as potential source. The antibacterial activity of 80% methanol extracts of the leaves of Verbena officinalis (Vo-80ME), Myrtus communis (Mc-80ME), and Melilotus elegans (Me-80ME) was tested against 6 bacterial isolates using agar well diffusion technique. In each extract, 3 concentrations of 10, 20, and 40 mg/well were tested for each bacterium. The minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) were also determined. Vo-80ME and Mc-80ME exhibited promising antibacterial activity against Staphylococcus aureus with the highest zone of inhibition being 18.67 and 26.16 mm, respectively at concentration of 40 mg/well. Regarding gram-negative bacteria, Vo-80ME exhibited an appreciable activity against Escherichia coli and Salmonella typhi. Mc-80ME displayed remarkable activity against all isolates including Pseudomonas aeruginosa with the maximum zone of inhibition being 22.83 mm. Me-80ME exhibited better antibacterial activity against E coli, but its secondary metabolites had little or no activity against other gram-negative isolates. The MIC values of Vo-80ME ranged from 0.16 to 4.00 mg/mL. The lowest MIC was observed in Mc-80ME, with the value being 0.032 mg/mL. Mc-80ME had bactericidal activity against all tested bacterial isolates. Mc-80ME showed remarkable zone of inhibitions in all tested bacterial isolates. Besides, Vo-80ME showed good antibacterial activity against S aureus, E coli, and S typhi. Conversely, Me-80ME has shown good activity against E coli only. Generally, M communis L and V officinalis have good MIC and MBC results.
Keywords: antibacterial activity, Verbena officinalis, Myrtus communis, Melilotus elegans
Plants have been used for the treatment of various disorders regardless of their safety and efficacy profiles. Previous studies indicated that approximately 80% of the global population relies on traditional medicine for their primary healthcare.1–4 Nevertheless, the use of traditional plants has been associated with the adulteration of valuable medicinal components, poor cultivation and collection procedures, lack of standardization during preparation, poor storage conditions, and incertitude among traditional medicine practitioners, ultimately affecting the process of drug development.5 Despite challenges, there is great demand for development of new antibacterial agents from traditional medicinal plants. Therefore, it is worthwhile to properly evaluate the safety and efficacy of medicinal plants that are being used in various traditional medical systems. The need for newer, more effective, less expensive, and safer agents has become a paramount issue for overcoming current challenges including antimicrobial resistance.
The antimicrobial activities of medicinal plants is based on their bioactive phytoconstituents called secondary metabolites including alkaloids, terpenoids, flavonoids, tannins, and glycosides, among others.6 The crude extracts of various medicinal plants such as Rhamnus prinoides, Calpurnia aurea, Peterollobium stellatum, Datura stramonium, Croton macrostachyus, and Acokanthera schimperi extracts have been tested and approved for their antimicrobial activity in previous studies.7–10 In addition, a study conducted by Abebe et al on the antibacterial activity of Verbena officinalis L was found inconclusive and very shallow.11 Moreover, there are still several medicinal plants such as Melilotus elegans that have been used traditionally for the treatment of infectious diseases indicating the need for further scientific studies to validate and develop safe and efficacious antibacterial agents.
The anti-inflammatory and analgesic effects of V officinalis extract in different formulations have been studied and confirmed.12 In addition, the extract of aerial parts of V officinalis has traditionally had antipyretic, sedative,13 and anticancer effects.14 Moreover, the plasters of aerial part of V officinalis are used as hemostatics and antirheumatics in knees and elbows.15 Apart from this, the extract or the juice of V officinalis has been used for the treatment of tonsillitis and ascariasis.16 The leaf extract is also used in the treatment of ear disease by applying some drops of the extract through the ear16 and for the control of snake bite poisoning.17 For instance, the extract of the whole plant, after boiling with tea, is given orally for the treatment of dysentery.18,19
Myrtus communis L (family: Myrtaceae) is one of the most important drugs being used in the Unani system of phytomedicine since ancient Greece period. In Ethiopia, common myrtle or M communis has several vernacular names such as Ades (Amharic, Guragegna, Tigregna), Addisaa, coddoo (Afan Oromo), and wobattaa (Welaitigna).20,21 It is a well-known shrub for its therapeutic, cosmetic, and food uses.22 Various parts of the plant have also been used as folkloric repute for the management of several disorders including hemorrhoid, inflammation, pulmonary diseases,23 and wound infections.24 Besides, the decoction of leaf powder has been used for the treatment of eczema and other skin diseases.25 Moreover, the leaves have been traditionally used for the treatment of diarrhea in different traditional medical systems.24,26,27 In addition, it has been used for the treatment of dandruff,28 scabies,18 and headache.29
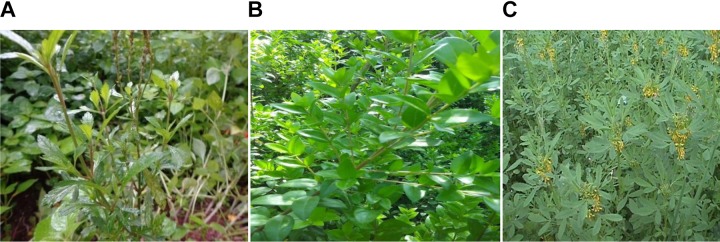
The third medicinal plant selected for this study was Melilotus elegans, which is one of the medicinal plants belonging to the family leguminosae.30 In Ethiopia, it has a wide distribution, particularly in highlands where the altitude ranges between 1700 and 2800 m above sea level. The plant is known by its vernacular names including “Egug” and “Gugi” in Amharic and “Yemamberi” in Tigregna (Figure 1).31,32 In folk medicine, the powdered leaves of M elegans are mixed with butter and applied topically against hemorrhoids and mouth and wound infections.32 The plant can also be taken orally for the management of bronchial asthma. In addition, the leaf of the plant is used in the treatment of various disorders (excavated sore, piles, and ulcers).33 The crude extract and its isolated flavonoids from the leaves of M elegans have been shown to have anti-inflammatory activity in carrageenan-induced paw edema in rodents model.32
Figure 1.
Photographs of medicinal plants: (A) Verbena officinalis, (B) Myrtus communis, and (C) Melilotus elegans.
The slow rate of new antimicrobial development in the area of antimicrobial therapy has become a global issue because antimicrobial research and development are not attractive to venture capitalists leading to an investment rate of less than 5%. Conversely, the high rate of antimicrobial resistance makes the majority of available medications ineffective, leading to a post-antibiotic era. Thus, safe alternatives are sought. In particular, there is a need to intensify research into medicinal plants claimed to be effective in the management of infectious diseases. The alternative and complementary therapies being used in traditional medicine should be integrated into conventional medicine to ensure the safe and efficacious use of drugs. Therefore, there must be a real commitment in commencing preclinical studies based on the folkloric repute to provide a benchmark for further studies. Therefore, this study aimed to investigate the in vitro antibacterial activities of the aforementioned medicinal plants having folkloric repute in different traditional medical systems including Ethiopian traditional medicine.
Methods and Materials
Collection of Plant Materials and Their Authentication
The leaves of V officinalis were collected from Debre Markos town and its surrounding areas, which is 300 km to the northwest of the capital of Ethiopia, Addis Ababa, in November 2017. Likewise, the leaves of M communis and M elegans were collected from Mersa, North Wollo, which is 490 km away from Addis Ababa to the northeast in December 2017. The identification of the plant specimens was undertaken by a taxonomist at the National Herbarium, College of Natural and Computational Sciences, Addis Ababa University, where voucher specimens were deposited for future reference: MS002/2017, MS003/2017, and MS004/2017 for V officinalis, M communis, and M elegans, respectively.
Preparation and Extraction of Plant Materials
The leaves of the aforementioned plants were gently washed with tap water to remove dirt and soil. The leaves of the plants were manually cut into pieces and dried under shade for 2 weeks. The dried plant materials were ground into an appropriate coarse powder using mortar and pestle. Then, 150 g of coarsely powdered leaves of each plant material was separately macerated in 2 L Erlenmeyer flask with 400 mL 80% methanol for 3 days with frequent agitation using mini-orbital shaker at room temperature. The extracts were filtered through double-layered muslin cloth followed by Whatman No. 1 filter paper (Schleicher and Schuell Micro Science Gmbh, Germany). The marcs of leaf extracts of each plant material were re-macerated twice (3 days for each batch) with the same volume of fresh solvent to increase the actual yield of extraction. A similar filtration procedure was undertaken to obtain the final filtrates. The combined filtrates were concentrated to dryness using rotary evaporator (Buchi labortechnik AG, Switzerland). The remaining aqueous residues of each plant material were deep-frozen to form ice and lyophilized (Operan, Korea Vacuum Limited, Korea) to obtain the final dried extract. The percentage yields of the extracts were determined as follows:
Finally, the dried extracts were stored frozen in air-tight container until the day of experimentation.
Preliminary Phytochemical Screening
The presence of secondary metabolites such as alkaloids, flavonoids, saponins, tannins, terpenoids, glycosides, and steroids was evaluated in the crude extracts using standard testing methods.34–36
Standard Laboratory Strains
Standard isolates of different bacteria strains: American Type Culture Collection (ATCC) including Staphylococcus aureus (ATCC 25923), Escherichia coli (ATCC 25922), Salmonella typhi (ATCC 13062), Shigella flexneri (ATCC 12022), Pseudomonas aeruginosa (ATCC 27853), and Proteus mirabilis (ATCC 29906) were obtained from the Ethiopian Public Health Institute (Addis Ababa, Ethiopia). The bacteria were purposely selected for evaluating the spectrum of activity and considering the folkloric repute of the experimental plants.
Inoculum Preparation and Standardization
Nutrient agar was prepared following the manufacturer’s preparation protocol. Then, standard bacterial isolates were inoculated and spread on the prepared agar using inoculating wire loop following aseptic condition in safety cabinet (Bioair Instruments, Eurolone Company, Italy) and incubated for 24 hours at 37°C. The bacterial turbidity of each bacterium was prepared and standardized following the Clinical and Laboratory Standard Institute guideline.37 Having prepared the nutrient broth in distilled water and autoclaved it (Astell Scientific Ltd, England), 3 to 5 well-isolated colonies of the same morphological type of each bacterium were peaked up by wire loop from fresh agar plates of bacterial culture and aseptically transferred into test tubes containing 5 mL of nutrient broth and incubated for about 6 hours. The turbidity of the inoculum tube was adjusted to the already prepared turbidity equivalent of 0.5 McFarland standard, which is assumed to contain a bacterial concentration of 1 × 108 CFU/mL.
Antibacterial Activity Assay
Agar Well Diffusion
The antibacterial agar well diffusion method was conducted by following the method described by previous studies.8–10,38 Bacterial broth culture was prepared equivalent to 0.5 McFarland standard as described previously. An aliquot of inoculum of the respective bacterium was streaked on the sterile Muller Hinton agar plates (prepared according to the manufacturer’s guideline) using a sterile cotton swab to ensure even coverage of the plates with each bacterium following incubation. Then, the plated media were allowed to dry at room temperature for 30 minutes. On each plate, equidistant wells (4 for gram-positive and 5 for gram-negative bacteria having 2 controls) were made with a 6 mm diameter sterilized cork borer.10 The labeled wells were filled with 100 μL of 100, 200, and 400 mg/mL of leaf extracts of each plant material for each bacterium corresponding to 10, 20, and 40 mg/well concentrations. Commercial antibiotic powders (primary standards) of amoxicillin and ciprofloxacin (Ethiopian Pharmaceutical Industry, Epharm) were used as standard drugs. To match the preparation of extract solutions, the concentration of 250 μg/mL (25 μg/well) and 200 μg/mL (20 μg/well) solutions were prepared using sterile water for amoxicillin and ciprofloxacin, respectively. The solvent for dissolving crude extracts was 25% dimethylsulfoxide in sterile water and was treated as a negative control. Then, the plates were allowed to stand on a laboratory bench for approximately 2 hours to permit prediffusion of the extract to agar medium at room temperature.8,39 Finally, the plates were incubated at 37°C for 24 hours. The resulting diameters of zones of inhibition, including the diameter of the well, were measured using a ruler and reported in millimeter. To maintain the consistency of measurements, each zone of inhibition was measured twice (one vertical and one horizontal measurement) and the average value was taken. The experiment was performed in triplicate for each bacterium and plant material and the mean zone of inhibition was calculated for each crude extract and standard antibiotics.
Determination of the Minimum Inhibitory Concentration (MIC)
The extracts having antibacterial activity in agar well diffusion technique were further processed for the quantitative determination of MIC values using serial broth dilution technique. In this method, the first test tube contained stock solutions (100 mg/mL) of each extract for each bacterium. The stock solutions were subjected to serial dilution with nutrient broth with final concentration being 0.032 mg/mL (100, 20, 4, 0.80, 0.16, and 0.032 mg/mL). Standardized microbial suspension of 1 mL was added to each test tube. The last 2 columns were reserved for positive (growth) and negative (sterility) controls. Control I which served as negative control, contained nutrient broth with extract in serial dilutions in the absence of bacterium, whereas control II was regarded as positive control and contained nutrient broth with respective bacterium and without extracts for comparing the turbidity status. The tubes were incubated at 37°C for 24 hours. In a series of test tubes, the lowest concentration of extracts at which no turbidity (growth) occurred was considered as the MIC cutoff point. All the procedures were performed in 3 independent tests, and the average value was taken as a final MIC value.
Determination of Minimum Bactericidal Concentration (MBC)
The determination of MBC values was performed in accordance with previous studies.8,40 In line with the MIC experiment conducted in triplicate, the contents of test tubes above or equal to MIC cutoff points were subjected for aseptic subculturing in Muller Hinton agar free of antimicrobial disks and incubated at 37°C for 24 hours. Following incubation, the lowest concentration of the extract at which no bacterial growth occurred on agar plates was treated as the MBC cutoff point.
Data Analysis
Data were entered and analyzed using IBM Statistical Package for the Social Sciences (SPSS) Version 20.0 software (Armonk, NY). Results were expressed as mean ± standard error of the mean (M ± SEM). The normality of the data distribution was checked using Kolmogorov-Smirnov and Shapiro-Wilk tests. For analyzing zone of inhibition, One-way analysis of variance was performed followed by Tukey’s post-hoc test for multiple comparisons. MIC and MBC values were computed using descriptive statistics. The analysis was performed at 95% confidence level and P value <.05 denoted statistical significant.
Results
Extraction Yields
The percentage yields of the 80% methanol leaf extracts of V officinalis (Vo-80ME), M communis (Mc-80ME), and M elegans (Me-80ME) were found to be 9.25% (w/w), 16.33% (w/w), and 10.60% (w/w), respectively.
Phytochemical Screening
The preliminary phytochemical screening revealed that M communis was found rich in tested secondary metabolites except alkaloids. Only flavonoids and terpenoids were detected in the leaves of V officinalis. The leaves of M elegans are rich in flavonoids and saponins. Generally, the study indicated that flavonoids are common secondary metabolites in all extracts (Table 1).
Table 1.
Preliminary Phytochemical Screening of 80ME of the Leaves of Verbena officinalis, Myrtus communis, and Melilotus elegans
| Constituents | V officinalis | M communis | M elegans |
|---|---|---|---|
| Cardiac glycosides | − | + | − |
| Flavonoids | + | + | + |
| Alkaloids | − | − | − |
| Saponins | − | + | + |
| Steroids | − | + | − |
| Tannins | − | + | − |
| Terpenoids | + | + | − |
Abbreviations: +, present; −, absent.
Antibacterial Activity
Both Vo-80ME and Mc-80ME showed remarkable zone of inhibitions against S aureus in a concentration-dependent manner. With similar concentrations across the extracts, Mc-80ME had the highest zone of inhibitions at all concentrations tested against this bacterium. However, Me-80ME did not have any inhibition at all tested concentrations indicating the absence of antibacterial activity (Table 2).
Table 2.
Zone of Inhibition (mm) of the Hydromethanolic Extracts of the Leaves of Verbena officinalis, Myrtus communis, and Melilotus elegans Against Staphylococcus aureus.*
| Dose | Zone of Inhibition (mm) Against S aureus | ||
|---|---|---|---|
| V officinalis | M communis | M elegans | |
| 10 mg/well | 11.33 ± 0.83a** | 21.83 ± 0.44a**c*d** | NA |
| 20 mg/well | 14.83 ± 1.01a** | 25.5 ± 0.76a** | NA |
| 40 mg/well | 18.67 ± 1.20a** | 26.16 ± 0.60a** | NA |
| 20 μg/well (CIP) | 30.50 ± 2.78 | 31.50 ± 0.87 | 30.67 ± 1.01 |
Abbreviations: CIP, ciprofloxacin; NA, no activity/inhibition at dose(s) tested.
* Values are expressed as mean ± SEM (n = 3), analysis was performed with one-way analysis of variance followed by Tukey post hoc test: acompared positive control (CIP), bcompared to 10 mg/well, ccompared to 20 mg/well, dcompared to 40 mg/well
**P < .01; *P < .05.
Besides, Vo-80ME was endowed with appreciable antibacterial activity against E coli and S typhi at lower and middle concentrations. Likewise, at 40 mg/well dose of Vo-80ME, the most susceptible strain was E coli with the zone of inhibition being 20.33 mm. The antibacterial activity of V officinalis against P aeruginosa was found very modest with the maximum zone of inhibition being 6.67 mm at the concentration of 40 mg/well. The leaf extract of V officinalis has also shown a relatively better antibacterial activity against P mirabilis than that of S flexineri. The leaf extract of M elegans (Me-80ME) exhibited a notable zone of inhibition against E coli at all tested concentrations in a concentration-dependent manner. This plant material was, however, devoid of any antibacterial activity against the 2 gram-negative aerobic bacilli, P aeruginosa and P mirabilis. Moreover, the antibacterial activity of the leaf of this plant material against S typhi and S flexneri was found extremely limited. The leaf extract of M communis showed remarkable antibacterial activities against all strains. Most important, the difficult to treat gram-negative bacterium P aeruginosa has shown the highest level of susceptibility to this plant material. Besides, Mc-80ME showed the highest zone of inhibition against S flexneri, with the maximum value being 26.17 mm corresponding to 40 mg/well concentration (Table 3).
Table 3.
Zone of Inhibition (mm) of the Hydromethanolic Extracts of the Leaves of Verbena officinalis, Myrtus communis, and Melilotus elegans Against Gram-Negative Bacteria*.
| Plant Material | Dose | Zone of Inhibition (mm) | ||||
|---|---|---|---|---|---|---|
| Escherichia coli | Salmonella typhi | Shigella flexneri | Pseudomonas aeruginosa | Proteus mirabilis | ||
| V officinalis | 10 mg/well | 12.00 ± 0.578a**e** | 12.67 ± 1.45a* | 3.33 ± 0.88a**b**e** | NA | 8.67 ± 2.03a**b** |
| 20 mg/well | 14.67 ± 1.45a**e** | 15.00 ± 2.08 | 8.66 ± 0.88a**b** | 4.50 ± 0.29a** | 13.33 ± 1.45a**b** | |
| 40 mg/well | 20.33 ± 0.88a**b** | 16.50 ± 0.28 | 13.00 ± 0.58a** | 6.67 ± 0.88a** | 16.00 ± 1.04a**b** | |
| 25 μg/well (AMOX) | 13.83 ± 0.33a** | 20.33 ± 2.18 | 18.67 ± 2.96a** | NT | 27.67 ± 2.40 | |
| 20 μg/well (CIP) | 30.67 ± 0.93 | 24.17 ± 3.08 | 32.67 ± 0.33 | 18.67 ± 1.76 | 31.67 ± 0.44 | |
| M communis | 10 mg/well | 13.33 ± 0.33a**e* | 13.33 ± 0.33a**b**e** | 20.83 ± 0.93a**e** | 14.83 ± 0.44a** d**e** | 12.17 ± 0.73a**b**e* |
| 20 mg/well | 16.83 ± 1.87a** | 15.83 ± 0.93a**b**e* | 23.83 ± 0.93a** | 20.50 ± 0.50 | 14.50 ± 1.15a**b** | |
| 40 mg/well | 19.16 ± 0.44a**b* | 18.50 ± 0.50a** | 26.17 ± 1.20a**b** | 22.83 ± 0.93a* | 19.33 ± 1.45a**b** | |
| 25 μg/well (AMOX) | 12.16 ± 0.44a** | 20.50 ± 0.289 | 20.00 ± 0.58a** | NT | 26.83 ± 1.59 | |
| 20 μg/well (CIP) | 31.67 ± 1.67 | 22.17 ± 0.44 | 34.83 ± 0.44 | 19.50 ± 0.29 | 31.00 ± 0.58 | |
| M elegans | 10 mg/well | 11.33 ± 0.33a*** | 0.67 ± 0.33a**b** | 1.50 ± 0.29a***b*** | NA | NA |
| 20 mg/well | 17.67 ± 2.40a*** | 1.17 ± 0.17a**b** | 3.33 ± 0.60a***b*** | NA | NA | |
| 40 mg/well | 19.50 ± 1.26a**b* | 2.00 ± 0.29a**b** | 5.00 ± 0.58a***b*** | NA | NA | |
| 25 μg/well (AMOX) | 11.33 ± 0.33a*** | 19.50 ± 1.80 | 20.67 ± 0.33a*** | NT | 25.67 ± 1.45 | |
| 20 μg/well (CIP) | 32.00 ± 2.00 | 20.67 ± 0.67 | 34.83 ± 1.64 | 19.33 ± 0.33 | 31.33 ± 1.45 | |
Abbreviations: AMOX, amoxicillin; CIP, ciprofloxacin; NA, no activity/inhibition at dose(s) tested; NT, not tested for controls.
* Values are expressed as mean ± SEM (n = 3); analysis was performed with one-way analysis of variance followed by Tukey’s post hoc test: acompared with positive control (ciprofloxacin), bcompared with positive control (amoxicillin), ccompared with 10 mg/well, dcompared with 20 mg/well, ecompared with 40 mg/well.
*P < .05; **P < .01; ***P < .001.
MIC of the Leaf Extracts
To quantitatively investigate the antibacterial activity, the MIC cutoff points were determined for each plant extract. Accordingly, lower MICs were recorded against S typhi (0.16 mg/mL) and E coli (0.8 mg/mL) in Vo-80ME. In Mc-80ME, the lowest MIC cutoff point was observed against S typhi (0.032 mg/mL). However, in Me-80ME, relatively higher MIC values were recorded with the lowest value being 4.00 mg/mL against E coli (Table 4).
Table 4.
MIC (in mg/mL) of Hydromethanolic Extracts Using Broth Dilution Techniques (Prepared From 100 mg/mL Stock Solution).
| Bacteria | Plant Materials | ||
|---|---|---|---|
| Verbena officinalis | Myrtus communis | Melilotus elegans | |
| Staphylococcus aureus | 4.00 ± 0.00 | 0.80 ± 0.00 | — |
| Escherichia coli | 0.80 ± 0.00 | 0.16 ± 0.00 | 4.00 ± 0.00 |
| Salmonella typhi | 0.16 ± 0.00 | 0.032 ± 0.00 | 20.00 ± 0.00 |
| Shigella flexneri | 4.00 ± 0.00 | 0.16 ± 0.00 | 20.00 ± 0.00 |
| Pseudomonas aeruginosa | — | 0.80 ± 0.00 | — |
| Proteus mirabilis | 4.00 ± 0.00 | 0.80 ± 0.00 | — |
Abbreviations: MIC, minimum inhibitory concentration; —, no inhibitory effect starting from stock or first dilution.
MBC of the Leaf Extracts
The MBC cutoff points of Vo-80ME ranged from 0.8 mg/mL (against S typhi) to 20 mg/mL (S aureus, S flexneri, and P mirabilis). Relatively lower MBC values were recorded in Mc-80ME with the lowest MBC being 0.8 mg/mL (against strains of E coli and S typhi), whereas the maximum MBC recorded was 4.00 mg/mL against the remaining bacterial strains. In Me-80ME, however, the bactericidal effect was observed against E coli only, with MBC of 20 mg/mL. Generally, Mc-80ME killed the bacterial strains with relatively lower concentration and broader coverage (Table 5).
Table 5.
MBC (in mg/mL) of the Leaf Extract of Verbena officinalis, Myrtus communis, and Melilotus elegans Against Gram-Positive and Gram-Negative Bacteria.
| Bacteria | Plant Materials | ||
|---|---|---|---|
| Verbena officinalis | Myrtus communis | Melilotus elegans | |
| Staphylococcus aureus | 20.00 ± 0.00 | 4.00 ± 0.00 | — |
| Escherichia coli | 4.00 ± 0.00 | 0.80 ± 0.00 | 20.00 ± 0.00 |
| Salmonella typhi | 0.80 ± 0.00 | 0.80 ± 0.00 | — |
| Shigella flexneri | 20.00 ± 0.00 | 4.00 ± 0.00 | — |
| Pseudomonas aeruginosa | — | 4.00 ± 0.00 | — |
| Proteus mirabilis | 20.00 ± 0.00 | 4.00 ± 0.00 | — |
Abbreviation: —, no bactericidal effect.
Discussion
Medicinal plants are increasingly targeted in the search for new antimicrobial agents.6,41–43 In the 20th century, the primary sources of the present-day antimicrobials were microorganisms such as fungi and bacteria.44 In the 21st century, however, there is alarmingly increasing antimicrobial resistance on the available agents with very slow development of new antimicrobials.45,46 Hence, we are facing a potential post-antibiotic era where the present-day agents are no longer effective.47,48 It is, therefore, mandatory to extensively search for new agents based on the traditional use of herbal medicines as potential sources.
The use of and search for drugs derived from medicinal plants have accelerated in recent years. Ethnopharmacologists, botanists, microbiologists, and natural products chemists are searching worldwide for phytochemicals and “leads” that could be developed for treatment of infectious diseases. While around 50% of current pharmaceuticals are derived from plants origin, none are used as antimicrobials.6 Traditional healers have long used plants to prevent or cure infectious conditions. However, there is no sufficient scientific evidence to integrate the traditional system with modern medicine. To this end, plants are rich in a wide variety of secondary metabolites, such as tannins, terpenoids, alkaloids, and flavonoids, which have been found in vitro to have antimicrobial properties. Our finding has tried to provide a sort of scientific evidence for antibacterial activities of crude extracts of 3 medicinal plants having folkloric repute.
Based on this, the hydromethanolic extract of the leaves of V officinalis has shown a relatively moderate level of antibacterial activity against S aureus. Likewise, this plant extract is also endowed with secondary metabolites having antibacterial activity against a wide range of gram-negative pathogens. To this end, comparable level of activity was observed against E coli and S typhi, whereas poor antibacterial activity was recorded in P aeruginosa with the lowest concentration being totally devoid of any activity. M elegans is devoid of any antibacterial activity against S aureus, P aeruginosa, and P mirabilis in all tested concentrations. Nevertheless, this hydromethanolic extract exhibited appreciable antibacterial activity against standard strains of E coli and with mild to moderate zone of inhibition against S typhi and S flexneri.
The third medicinal plant is M communis, which is one of the most important medicinal plants that are being used in the Unani system of phytomedicine since ancient Greece period. Much has been investigated in the ethnobotany, ethnopharmacology, and phytochemistry of this plant in different parts of the world with high priority in Arabian countries.49–53 Though not conclusive, published reports indicated that the antibacterial activity of this plant material is broader in coverage with a remarkable activity.23,28,53 Indeed, the hydromethanolic extract of the leaves of M communis showed potent and concentration-dependent antibacterial activity against all tested gram-positive and gram-negative isolates. The remarkable activity of this plant extract against S aureus and P aeruginosa in particular put this agent as an important target for further purification and identification of bioactive constituents for treatment of infectious diseases.
The difference in antibacterial activity of these medicinal plants against different strains of bacteria is possibly attributable to the variation in the quality and quantity of bioactive secondary metabolites in the extracts of targeted morphological part (leaf). In line with this preliminary phytochemical screening, which showed the presence of terpenoids and flavonoids, previous phytochemical studies had reported the presence of iridoids (type of monoterpenoids), phenyl-propanoids, flavonoids, and terpenoids as the main components of V officinalis. More specifically, the hydroalcoholic and aqueous extracts were found rich in glucuronide-based flavonoids.12,54 M communis, in particular, is very rich in secondary metabolites, notably supporting the high overall antibacterial activity from synergistic or additive interaction of these bioactive components. According to the preliminary phytochemical screening, M elegans is endowed with flavonoids and saponins as main secondary metabolites. Concordant with this, previously published reports revealed that flavonol glycosides, particularly kaempferol, were found as a major secondary metabolite.55 The reputed applications of M elegans leaves for the treatment of wounds, hemorrhoids, and other skin diseases in traditional medical practice seem to be well founded. As previous reports indicated, the activity of the plant is attributed to a combination of secondary metabolites, which belong to at least 3 classes of plant metabolites, namely, coumarins, flavonoids, and saponins. Based on this, the anti-inflammatory activity of this plant is well studied.12,55,56 However, the possible antibacterial activity was not evaluated before.
Being common secondary metabolites in 3 medicinal plants, efficacy and spectrum of antibacterial activity is probably due to, but not limited to, flavonoids. M communis is also rich in other secondary metabolites including terpenoids, tannins, saponins, and steroids, whereas M elegans contains saponins in addition to flavonoids. The antibacterial effects of V officinalis might be due to the combined effects of terpenoids and flavonoids detected in the leaf extract. Although it was found insufficient and unclear, a previous study conducted in 2 bacterial isolates (S aureus and E coli) indicated the high zone of inhibition and good MIC results of V officinalis against these pathogens without further analysis of MBC cutoff point.57 This study is expanded to address 1 gram-positive and 5 gram-negative bacteria with vivid MIC and MBC results for each. Apart from this, the poor antibacterial activity of M elegans might be due to the quality and quantity of its metabolites such as saponins and flavonoids in which the individual or combined antibacterial effect was found very modest. Several studies indicated that flavonoids, terpenoids, and tannins are secondary metabolites with high antibacterial potential, whereas saponins have little or no activity.58–62 This justification somehow supports the poor antibacterial activity of M elegans. Moreover, flavonoids and tannins have been shown to exhibit activity against Enterobacteriaceae including E coli, P aeruginosa, K pneumonia, and P mirabilis. 60–62 With regard to natural products, it is generally accepted that phytochemicals are less potent antibiotics than agents of microbial origin. However, new classes of antimicrobial drugs are urgently required and the flavonoids generally represent a novel set of leads for drug development. Future optimization of these compounds through structural modification (structure activity relationship) may allow the development of a pharmacologically acceptable antimicrobial agent or group of agents.63 Flavonoids have shown to inhibit a number of bacterial virulence factors, including quorum-sensing signal receptors, enzymes, and toxins. Evidence of these molecular effects at the cellular level includes in vitro inhibition of biofilm formation and inhibition of bacterial attachment to host ligands.61,62
With the exception of M communis L, the rest plant extracts have shown poor or no activity against the difficult to treat gram-negative bacteria P aeruginosa. This might be due to the fact that this bacterium has outer membrane (porine channel) permeability problems coupled with efflux pump mechanisms.64–66 Besides, it allows highly polar constituents to pass through. Fortunately, the bioactive secondary metabolites of M communis possibly with expanded polarity reach to this target.
In line with the zone of inhibition, M communis has relativity good MIC results in all isolates tested. The MIC cutoff points of V officinalis ranges from 0.16 to 4.00 mg/mL. The higher MBC values than MIC cutoff points, recorded in all extracts, indicated the possibility of concentration-dependent bactericidal effects as observed in certain antibiotics such as aminoglycosides. M elegans has poor bactericidal activity against E coli only with the MBC value being 20 mg/mL.
All in all, this study has provided a starting point for further purification and isolation of active constituents with promising antibacterial activity. The extracts should be standardized for use in traditional medicine. Substantial efforts are needed to integrate the traditional medical systems with conventional medicine, a process that is currently at its infancy.
Conclusion
The study attempted to validate the potential antibacterial activity of medicinal plants having folkloric repute in Ethiopian traditional medicine. Accordingly, the leaf extract of M communis showed remarkable zone of inhibitions in all tested bacterial isolates including P aeruginosa. Besides, V officinalis showed good antibacterial activity against S aureus, E coli, and S typhi, indicating the broader spectrum of activity. Nevertheless, M elegans has shown good activity against E coli with little or no activity to the rest of the isolates. Generally, M communis and V officinalis have good MIC and MBC results. The higher MBC value indicates the concentration-dependent bactericidal effect of extracts. The difference in the antibacterial activity of these medicinal plants is possibly due to the variation in the quality and quantity of bioactive phytoconstituents.
Strength and Limitations
Even though this study has evaluated the antibacterial activity of 3 medicinal plants against a wide range of microorganisms with vivid MIC and MBC cutoff points, it is limited to the standard isolates of ATCC because the ultimate purpose of this study was to confirm antibacterial activity but not to test susceptibility.
Acknowledgments
We acknowledge Haramaya University for granting financial assistance and materials to conduct this laboratory-based research work.
Footnotes
Author Contributions: MS and GM conceived and designed the study; all authors conducted the experiment and acquired the data. MS also analyzed and interpreted the data, drafted the manuscript, and prepared the final version for publication. All authors have read and approved the final version.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Haramaya University covered financial costs for research work.
ORCID iD: Mekonnen Sisay, MSc  https://orcid.org/0000-0001-6611-1174
https://orcid.org/0000-0001-6611-1174
Ethical Approval: Ethical approval of this research project was obtained from Institutional Health Research Ethics Review Committee (IHRERC) of College of Health and Medical Sciences, Haramaya University.
References
- 1. Tiwari S. Plants: a rich source of herbal medicine. J Nat Prod. 2008;1:27–35. [Google Scholar]
- 2. Pathak K, Das RJ. Herbal medicine—a rational approach in health care system. Int J Herbal Med. 2013;1:86–89. [Google Scholar]
- 3. Verma S, Singh S. Current and future status of herbal medicines. Veterinary World. 2008;1:347. [Google Scholar]
- 4. Joos S, Glassen K, Musselmann B. Herbal medicine in primary healthcare in Germany: the patient’s perspective. Evid Based Complement Altern Med. 2012;2012:294638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Njume C, Goduka N. Treatment of diarrhoea in rural African communities: an overview of measures to maximise the medicinal potentials of indigenous plants. Int J Environ Res Public Health. 2012;9:3911–3933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cowan MM. Plant products as antimicrobial agents. Clin Microbiol Rev. 1999;12:564–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Umer S, Tekewe A, Kebede N. Antidiarrhoeal and antimicrobial activity of Calpurnia aurea leaf extract. BMC Complement Altern Med. 2013;13:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Molla Y, Nedi T, Tadesse G, Alemayehu H, Shibeshi W. Evaluation of the in vitro antibacterial activity of the solvent fractions of the leaves of Rhamnus prinoides L’Herit (rhamnaceae) against pathogenic bacteria. BMC Complement Altern Med. 2016;16:287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Andualem G, Umar S, Getnet F, Tekewe A, Alemayehu H, Kebede N. Antimicrobial and phytochemical screening of methanol extracts of three medicinal plants in Ethiopia. Adv Biol Res. 2014;8:101–106. [Google Scholar]
- 10. Taye B, Giday M, Animut A, Seid J. Antibacterial activities of selected medicinal plants in traditional treatment of human wounds in Ethiopia. Asian Pac J Trop Biomed. 2011;1:370–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abebe A, Abebe M, Mekonnen A. Assessment of antioxidant and antibacterial activities of crude extracts of Verbena officinalis Linn root or atuch (Amharic). Chem Int. 2017;3:172–184. [Google Scholar]
- 12. Calvo M. Anti-inflammatory and analgesic activity of the topical preparation of Verbena officinalis L. J Ethnopharmacol. 2006;107:380–382. [DOI] [PubMed] [Google Scholar]
- 13. Ivanova D, Gerova D, Chervenkov T, Yankova T. Polyphenols and antioxidant capacity of Bulgarian medicinal plants. J Ethnopharmacol. 2005;96:145–150. [DOI] [PubMed] [Google Scholar]
- 14. Rigat M, Bonet MÀ, Garcia S, Garnatje T, Valles J. Studies on pharmaceutical ethnobotany in the high river Ter valley (Pyrenees, Catalonia, Iberian Peninsula). J Ethnopharmacol. 2007;113:267–277. [DOI] [PubMed] [Google Scholar]
- 15. Guarrera PM, Forti G, Marignoli S. Ethnobotanical and ethnomedicinal uses of plants in the district of Acquapendente (Latium, Central Italy). J Ethnopharmacol. 2005;96:429–444. [DOI] [PubMed] [Google Scholar]
- 16. Teklay A, Abera B, Giday M. An ethnobotanical study of medicinal plants used in Kilte Awulaelo district, Tigray region of Ethiopia. J Ethnobiol Ethnomed. 2013;9:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tolossa K, Debela E, Athanasiadou S, Tolera A, Ganga G, Houdijk JG. Ethno-medicinal study of plants used for treatment of human and livestock ailments by traditional healers in South Omo, Southern Ethiopia. J Ethnobiol Ethnomed. 2013;9:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Enyew A, Asfaw Z, Kelbessa E, Nagappan R. Ethnobotanical study of traditional medicinal plants in and around Fiche District, Central Ethiopia. Curr Res J Biol Sci. 2014;6:154–167. [Google Scholar]
- 19. Gebeyehu G, Asfaw Z, Enyew A, Raja N. Ethnobotanical study of traditional medicinal plants and their conservation status in Mecha Wereda West Gojjam Zone of Ethiopia. Int J Pharm Health Care Res. 2014;2:137–154. [Google Scholar]
- 20. Tadesse M, Mesfin B. A review of selected plants used in the maintenance of health and wellness in Ethiopia. Ethiopian e-J Res Innov Foresight. 2010;2:85–102. [Google Scholar]
- 21. Hedberg I, Kelbessa E, Edwards S, Demissew S, Person E. Flora of Ethiopia and Eritrea: Gentianaceae to cyclocheilaceae. Vol 5 Addis Ababa, Ethiopia: Addis Ababa University; 2006. [Google Scholar]
- 22. Sumbul S, Ahmad MA, Asif M, Akhtar M. Myrtus communis Linn: a review. Indian J Nat Prod Resour. 2011;2:395–402. [Google Scholar]
- 23. Alipour G, Dashti S, Hosseinzadeh H. Review of pharmacological effects of Myrtus communis L. and its active constituents. Phytother Res. 2014;28:1125–1136. [DOI] [PubMed] [Google Scholar]
- 24. Farzaei MH, Abbasabadi Z, Shams-Ardekani MR, Abdollahi M, Rahimi R. A comprehensive review of plants and their active constituents with wound healing activity in traditional Iranian medicine. Wounds. 2014;26:197–206. [PubMed] [Google Scholar]
- 25. Sarri M, Mouyet FZ, Benziane M, Cheriet A. Traditional use of medicinal plants in a city at steppic character (M’sila, Algeria). J Pharm Pharmcogn Res. 2014;2:31–35. [Google Scholar]
- 26. Haq F, Ahmad H, Alam M. Traditional uses of medicinal plants of Nandiar Khuwarr catchment (district Battagram), Pakistan. J Med Plants Res. 2011;5:39–48. [Google Scholar]
- 27. Dogan Y, Ugulu I. Medicinal plants used for gastrointestinal disorders in some districts of Izmir province, Turkey. Stud Ethnomed. 2013;7:149–161. [Google Scholar]
- 28. Teklehaymanot T, Giday M. Ethnobotanical study of medicinal plants used by people in Zegie Peninsula, Northwestern Ethiopia. J Ethnobiol Ethnomed. 2007;3:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Getaneh S, Girma Z. An ethnobotanical study of medicinal plants in Debre Libanos Wereda, Central Ethiopia. Afr J Plant Sci. 2014;8:366–379. [Google Scholar]
- 30. Gebre-Mariam T, Neubert R, Schmidt PC, Wutzler P, Schmidtke M. Antiviral activities of some Ethiopian medicinal plants used for the treatment of dermatological disorders. J Ethnopharmacol. 2006;104:182–187. [DOI] [PubMed] [Google Scholar]
- 31. Hedberg I, Edwards S. Flora of Ethiopia: Pittosporaceae to Araliaceae. Vol 3 Addis Ababa, Ethiopia: National Herbarium, Biology Department, Science Faculty, Addis Ababa University; 1989. [Google Scholar]
- 32. Asres A, Eder U, Bucar F. Studies on the anti-inflammatory activity of extracts and compounds from the leaves of Melilotus elegans . Ethiopian Pharm J. 2000;18:15–24. [Google Scholar]
- 33. Abate G. Etse debdabe In: Demissew S, ed. Ethiopian Traditional Medicine. Addis Ababa, Ethiopia: Addis Ababa University Press; 1989:99–183. [Google Scholar]
- 34. Zohra SF, Meriem B, Samira S, Muneer MA. Phytochemical screening and identification of some compounds from mallow. J Nat Prod Plant Resour. 2012;2:512–516. [Google Scholar]
- 35. Sisay M, Engidawork E, Shibeshi W. Evaluation of the antidiarrheal activity of the leaf extracts of Myrtus communis Linn (myrtaceae) in mice model. BMC Complement Altern Med. 2017;17:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bhandary SK, Kumari NS, Bhat VS, Sharmila KP, Bekal MP. Preliminary phytochemical screening of various extracts of Punica granatum peel, whole fruit and seeds. Nitte Univ J Health Sci. 2012;2:34–38. [Google Scholar]
- 37. Clinical and Laboratory Standards Institute. CLSI Document M07-A9. Wayne, PA: Clinical and Laboratory Standards Institute; 2012. [Google Scholar]
- 38. Mummed B, Abraha A, Feyera T, Nigusse A, Assefa S. In vitro antibacterial activity of selected medicinal plants in the traditional treatment of skin and wound infections in Eastern Ethiopia. Biomed Res Int. 2018;2018:1862401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wasihun Y, Adraro T, Ali S. Evaluation of antibacterial activity and phytochemical constituents of leaf extract of Lippia adoensis . Asia Pac J Energy Environ. 2014;1:45–53. [Google Scholar]
- 40. Rouis Z, Abid N, Koudja S, et al. Evaluation of the cytotoxic effect and antibacterial, antifungal, and antiviral activities of Hypericum triquetrifolium Turra essential oils from Tunisia. BMC Complement Altern Med. 2013;13:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Rios J, Recio M. Medicinal plants and antimicrobial activity. J Ethnopharmacol. 2005;100:80–84. [DOI] [PubMed] [Google Scholar]
- 42. Iwu MW, Duncan AR, Okunji CO. New antimicrobials of plant origin In: Janick J, ed. Perspectives on New Crops and New Uses. Alexandria, VA: ASHS Press; 1999:457–462. [Google Scholar]
- 43. Savoia D. Plant-derived antimicrobial compounds: alternatives to antibiotics. Future Microbiol. 2012;7:979–990. [DOI] [PubMed] [Google Scholar]
- 44. Dougherty TJ, Pucci MJ. Antibiotic Discovery and Development. New York, NY: Springer Science + Business Media; 2011. [Google Scholar]
- 45. Fauci AS. Infectious diseases: considerations for the 21st century. Clin Infect Dis. 2001;32:675–685. [DOI] [PubMed] [Google Scholar]
- 46. Saga T, Yamaguchi K. History of antimicrobial agents and resistant bacteria. JMAJ. 2009;52:103–108. [Google Scholar]
- 47. Alanis AJ. Resistance to antibiotics: are we in the post-antibiotic era? Arch Med Res. 2005;36:697–705. [DOI] [PubMed] [Google Scholar]
- 48. Kåhrström CT. Entering a post-antibiotic era? Nat Rev Microbiol. 2013;11:146. [Google Scholar]
- 49. Sisay M, Gashaw T. Ethnobotanical, ethnopharmacological, and phytochemical studies of Myrtus communis Linn: a popular herb in Unani system of medicine. J Evid Based Complementary Altern Med. 2017;22:1035–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Jamal A, Siddiqui A, Jafri M. A review on gastric ulcer remedies used in Unani system of medicine. Nat Prod Radiance. https://pdfs.semanticscholar.org/646e/e034dae1a79fe3cc6b5de4932205df230dc9.pdf?_ga=2.39053408.2103761218.1571289689-1720952739.1570613531. Accessed October 17, 2019.
- 51. Jamil S, Ahmad S, Akhtar J, Alam K. Antiamoebic plants used in Unani system of medicine. http://nopr.niscair.res.in/handle/123456789/12239. Published 2003. Accessed October 21, 2019.
- 52. Aliasl J, Khoshzaban F. Traditional herbal remedies for burn wound healing in canon of Avicenna. Jundishapur J Nat Pharm Prod. 2013;8:192–196. [Google Scholar]
- 53. Öztürk M, Altundağ E, Gücel S. Medicinal and aromatic plants (Turkey). Ethnopharmacology, Encyclopedia of Life Support Systems (EOLSS). http://apjee-my.weebly.com/uploads/1/3/4/5/13455174/4_apjee_1st_issue.pdf. Accessed October 21, 2019.
- 54. Rehecho S, Hidalgo O, de Cirano MGI, et al. Chemical composition, mineral content and antioxidant activity of Verbena officinalis L. LWT Food Sci Technol. 2011;44:875–882. [Google Scholar]
- 55. Gebre-Mariam T, Asres K, Getie M, Endale A, Neubert R, Schmidt PC. In vitro availability of kaempferol glycosides from cream formulations of methanolic extract of the leaves of Melilotus elegans . Eur J Pharm Biopharm. 2005;60:31–38. [DOI] [PubMed] [Google Scholar]
- 56. Asres K, Gibbons S, Hana E, Bucar F. Anti-inflammatory activity of extracts and a saponin isolated from Melilotus elegans . Pharmazie. 2005;60:310–312. [PubMed] [Google Scholar]
- 57. Mengiste B, Yesufn JM, Getachew B. In-vitro antibactserial activity and phytochemical analysis of leaf extract of Verbena officinalis . Int J Pharmacogn. 2014;1:744–779. [Google Scholar]
- 58. Akiyama H, Fujii K, Yamasaki O, Oono T, Iwatsuki K. Antibacterial action of several tannins against Staphylococcus aureus . J Antimicrob Chemother. 2001;48:487–491. [DOI] [PubMed] [Google Scholar]
- 59. Shu JC, Liu JQ, Chou GX. A new triterpenoid from Verbena officinalis L. Nat Prod Res. 2013;27:1293–1297. [DOI] [PubMed] [Google Scholar]
- 60. Buzzini P, Arapitsas P, Goretti M, et al. Antimicrobial and antiviral activity of hydrolysable tannins. Mini Rev Med Chem. 2008;8:1179–1187. [DOI] [PubMed] [Google Scholar]
- 61. Cushnie TT, Lamb AJ. Recent advances in understanding the antibacterial properties of flavonoids. Int J Antimicrob Agents. 2011;38:99–107. [DOI] [PubMed] [Google Scholar]
- 62. Bylka W, Matlawska I, Pilewski N. Natural flavonoids as antimicrobial agents. JANA. 2004;7:24–31. [Google Scholar]
- 63. Cushnie TT, Lamb AJ. Antimicrobial activity of flavonoids. Int J Antimicrob Agents. 2005;26:343–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Nikaido H. Molecular basis of bacterial outer membrane permeability revisited. Microbiol Mol Biol Rev. 2003;67:593–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Iyer R, Erwin AL. Direct measurement of efflux in Pseudomonas aeruginosa using an environment-sensitive fluorescent dye. Res Microbiol. 2015;166:516–524. [DOI] [PubMed] [Google Scholar]
- 66. Strateva T, Yordanov D. Pseudomonas aeruginosa—a phenomenon of bacterial resistance. J Med Microbiol. 2009;58:1133–1148. [DOI] [PubMed] [Google Scholar]