Abstract
Background:
There is a high incidence of a secondary anterior cruciate ligament (ACL) injury in unbraced adolescent athletes. Little is known about the effect of functional bracing with regard to the risk of secondary ACL injuries among adolescents.
Hypothesis:
Our primary hypothesis was that adolescents would have a high rate of secondary ACL injury even with brace use. A secondary hypothesis was that the reinjury rate with brace use would be lower than that of a historical control group of unbraced patients.
Study Design:
Case series; Level of evidence, 4.
Methods:
A group of 219 patients (age <20 years at surgery) who underwent ACL reconstruction and were prescribed postoperative functional bracing during cutting and pivoting sports for 2 years after surgery completed a survey regarding reinjury to either knee. Rates of knee injuries following ACL reconstruction were calculated and compared with those reported in a similar unbraced cohort. The effect of demographic and anatomic factors on risk of secondary ACL injuries was also investigated.
Results:
The overall follow-up rate was 65% (142/219) at a mean 5.6 years after surgery. In the braced cohort, the overall graft retear rate was 10%, with the highest retear rates observed in male patients 17 years of age and younger (18%). The overall contralateral ACL injury and combined (graft or contralateral ACL) secondary injury rates were 13% and 23%, respectively, with female patients younger than 18 years having the highest contralateral and combined injury rates (17% and 26%, respectively). Younger age (odds ratio [OR], 0.70; P = .021), family history of ACL injury (OR, 2.81; P = .015), and higher lateral tibial slope (OR, 1.25; P = .016) were associated with increased risk of secondary knee injury in the braced cohort. Compared with the unbraced cohort, the braced cohort had a lower overall graft retear rate (P = .028), a lower graft retear rate in patients younger than 18 years (P = .012), lower early graft retear rate (within the first year after surgery) (P = .011), and lower early graft retear rate in subjects younger than 18 years (P = .003).
Conclusion:
Postoperative use of functional bracing can result in reduced risk of graft retear and no change in contralateral injury rates. Clinicians may want to consider the use of postoperative functional bracing in adolescent patients.
Keywords: ACL reconstruction, graft injury, functional bracing
Adolescents are uniquely prone to a second anterior cruciate ligament (ACL) injury—either graft rupture or contralateral tear—after ACL reconstruction.19,26,28 In an Australian cohort study of patients treated with hamstring tendon autograft ACL reconstruction, the overall failure rate was only 4.5%.28 However, when the cohort was stratified by age, the risk of graft tear in patients younger than 20 years was 14% at a mean 3 years after surgery.28 In a more recent study of patients younger than 20 years,26 the same group reported a graft rupture rate of 18%, with half of ruptures occurring in the first postoperative year. The highest graft rupture rate was seen in male patients 17 years of age and younger (28%), and it was noted that retear rates were twice as high in patients 17 years of age and younger than in patients who were 18 and 19 years old. These findings support the assertion that adolescents appear to be at particular risk for ACL graft rupture after reconstruction.
Functional ACL bracing upon return to sport was not part of the rehabilitation protocol in these Australian studies. Bracing is not standard practice in Australia, and <8% of physicians there recommend a brace for return to sport.8 In a survey of the American Orthopaedic Society for Sports Medicine, Delay et al7 reported that functional ACL bracing is recommended 63% of the time in the United States, with another study reporting that surgeons recommend functional bracing for 9 to 12 months upon return to sport.6 A systematic review demonstrated that advantages of functional bracing following ACL reconstruction include normalizing joint mechanics, improving patient confidence, assisting with the transition back to sporting activities, and protecting healing tissue.16 Disadvantages include increased risk of injury when braces are worn improperly, muscle atrophy, reduced knee extension velocity, additional cost, increased exercise fatigability, and decreased patient perception of maximal performance.16 While functional ACL bracing has been studied with regard to in vivo knee kinematics, biomechanics, and early clinical outcomes, there is currently limited evidence and lack of validation on the use of functional bracing to decrease the rate of reinjury following ACL reconstruction.3,16
Given the sparsity of literature regarding bracing upon return to sport in relation to the risk of reinjury, the aim of this study was to determine the rate of reinjury in a cohort of young patients who were prescribed functional bracing following ACL reconstruction with hamstring autograft. As a secondary aim, we compared our findings with the age-matched unbraced cohort reported earlier.28 Our secondary hypothesis was that the reinjury rate with brace use would be lower than that of a historical unbraced control group.
Methods
Patient Selection
A retrospective review was performed of a consecutive US cohort of 219 patients younger than 20 years who had primary hamstring autograft ACL reconstruction surgery between January 2009 and December 2013 by a single experienced knee surgeon (M.M.M.). Patients were initially confirmed to have an ACL tear by physical examination with a positive Lachman test result and later confirmed with magnetic resonance imaging (MRI). Prior to ACL reconstruction, all patients had a positive pivot-shift examination result under anesthesia and visual confirmation of a complete tear of the ACL. All patients were prescribed postoperative functional ACL bracing to be used during participation in cutting and pivoting sports for a minimum of 2 years. After institutional ethics approval, all were invited to participate in the current study. Patients were at a minimum of 3 years following reconstructive surgery and were queried at a mean 5.6 years (range, 3-8 years) after surgery. Additionally, as a secondary aim, data from an Australian cohort of patients younger than 20 years26 were used as a historical control to compare the reinjury rates following primary hamstring autograft ACL reconstruction in patients who were prescribed postoperative functional ACL bracing upon return to sport (US cohort) and those who were not (Australian cohort).
Data Collection
Patient databases were searched for demographic information, injury, and surgical information. Demographics included age at the time of surgery, sex, and history of contralateral ACL injury. Surgical details and subsequent injuries were confirmed when available in the medical record. All patients were mailed or emailed a link to an online survey. Patients were excluded if they had a prior ACL injury or reconstruction to either knee. Patients were included in the study only if they completed the survey, given that questions regarding brace use could not be retrieved from the medical records. This survey was adapted from Webster et al28 and included structured questions regarding mechanism of injury, further injury to the ACL-reconstructed knee or injury to the contralateral knee, whether patients had returned to strenuous sport, and their Marx activity level in the year preceding the survey. In addition, questions were added regarding duration of postoperative bracing. Family history was considered positive if the patient had a first-degree relative with an ACL tear.
Surgical Procedure and Rehabilitation
All participants had a positive pivot-shift examination result under anesthesia and visual confirmation of a complete tear of the ACL, followed by a hamstring autograft reconstruction. The semitendinosus and gracilis tendons were harvested through a 3-cm incision over the proximal tibia and were doubled over a continuous-loop EndoButton (Smith & Nephew) to form a 4-stranded graft, which was placed under 15 lb of tension during tunnel preparation. A transtibial approach was used to drill the femoral tunnel, with the tibial tunnel entering the joint slightly posterior in the tibial footprint and the femoral tunnel aperture in the femoral ACL footprint. The graft was passed through the tunnels and the EndoButton engaged on the lateral femoral cortex. The graft was cycled under maximum manual tension and fixed to the tibia using a bioabsorbable interference screw (Smith & Nephew) with the knee in 5° of flexion.
Postoperatively, the patients in the current cohort were prescribed the same rehabilitation protocol, with an emphasis on regaining full extension and quadriceps function first. Partial weightbearing in a locking hinge brace set from 0° to 90° was used for the first 4 weeks, after which weightbearing was allowed as tolerated. A graded return to vigorous activities over the 6-month period was supervised by the physician and physical therapist, with a typical return to running at 3 months and evaluation for return to sport performed at 6 months after surgery. Functional bracing for cutting and pivoting sports was prescribed for 2 years after surgery. For the unbraced cohort, the postoperative rehabilitation was similar, with encouragement of immediate full knee extension and the restoration of quadriceps function as soon as possible. No braces or splints were used. For the current cohort as well as the prior (Australian) cohort, the decision about the timing of return to sport was made by the treating surgeon based on the following: no swelling, an essentially full range of motion, a stable knee on clinical examination, good quadriceps strength on clinical examination, control of a single-leg step-down or squat exercise, and the patient’s confidence in his or her knee. In both cohorts, from 4 to 6 months, patients were typically allowed return to sports-specific drills and activities, including controlled change of direction. From 6 months, patients were encouraged to increase training intensity and to pursue a gradual return to competitive sport as tolerated without pain or swelling. A minimum of 4 weeks of unrestricted training was required prior to return to competitive sports.
Anatomy Measurements
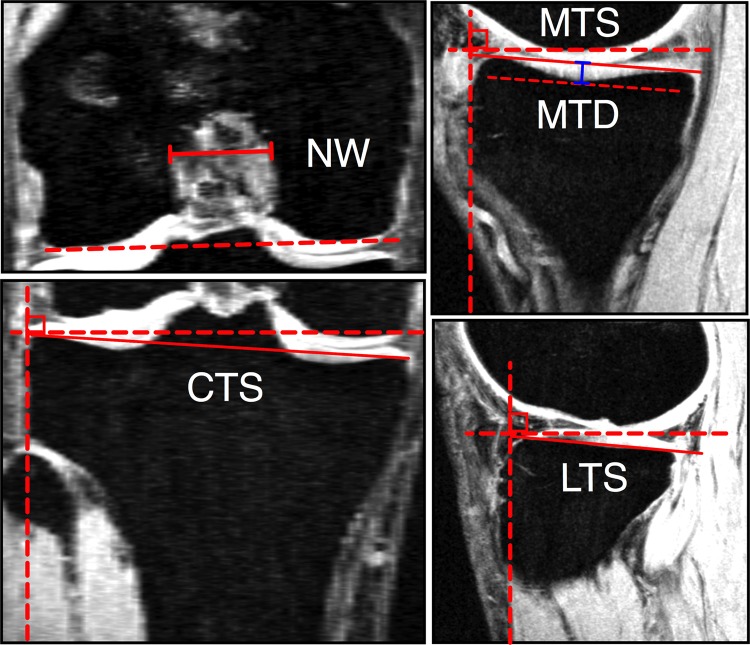
Posterior tibial slope, coronal tibial slope, medial tibial depth, and femoral notch width were measured for patients who had preoperative MRI available by 2 independent examiners (G.M.P. and A.V.), as shown in Appendix Figure A1. The posterior slopes of the medial and lateral tibial plateaus were measured with the techniques described by Hudek et al10 and Hashemi et al.9 The slope of the tibial plateau in the coronal plane and medial tibial depth were measured with the technique described by Hashemi et al.9 The width of the femoral notch was measured in the coronal plane, parallel to a line along the most inferior aspects of the femoral condyles.18 The measurement was taken at the middle of the ACL attachment.29
Statistical Analysis
Binomial logistic regression was used to determine the demographic and anatomic predictors of injury risk. The analysis was performed only on the braced cohort. Each demographic or anatomic factor was used as an independent variable, and the status of secondary injury was considered an independent variable. Given the retrospective nature of the analysis, no a priori sample size calculation was performed. Odds ratios (ORs) were calculated, and an alpha of 0.05 was used. The percentage of graft ruptures, contralateral ACL injuries, and overall secondary ACL injuries (ipsilateral or contralateral) were calculated. The Fisher exact test with a 2 × 2 contingency table was used to compare observed injury ratios with those of previously reported in a comparable cohort of 316 unbraced patients (mean age, 17.2 years [range, 11-19 years]; 36.7% female patients).26 To minimize the effect of nation-specific sports played on the rates of injury, the analysis was performed by excluding patients who played Australian Rules football and netball from the unbraced cohort, as these sports were not found in the US cohort. A secondary analysis was also performed where all athletes were included and is included as Appendix Table A1. The remaining patients in the unbraced cohort (n = 140) predominantly played soccer (38%) and basketball (34%). P values were 2-sided and considered statistically significant at P ≤ .05. Statistical analysis was performed using SPSS (v 23; IBM Corp).
Results
Of the 219 patients in the braced cohort, 142 (65%) could be contacted and followed up with at a mean ± SD of 5.6 ± 1.5 years postsurgically. Seven patients were excluded due to prior ipsilateral or contralateral ACL injuries or reconstructions, resulting in a total study population of 135 patients. Demographic information for the overall cohort population (n = 219) and included patients (n = 135) is presented in Table 1. Of 135 included patients, 131 indicated their mechanism of injury, of which 57 (44%) had a noncontact mechanism of injury, and 74 (56%) had a contact mechanism of injury. Of 135 patients in the braced cohort, 41 (30%) had a family history of ACL injury, and 86 had available preoperative MRI that was used to quantify knee anatomy (Table 2). Demographic information for the unbraced Australian cohort is presented in Table 3. Detailed characteristics of the study were previously published by Webster and Feller.26
Table 1.
Baseline Demographic Data for the Patients in the Braced Cohort
| Total | Male | Female | |
|---|---|---|---|
| Surveyed patients | |||
| n | 219 | 70 | 149 |
| Age at surgery,a y | 16.4 ± 1.5 | 16.3 ± 1.3 | 16.9 ± 1.7 |
| Final included patients | |||
| n | 135 | 31 | 104 |
| Age at surgery,a y | 15.8 ± 1.5 | 16.4 ± 1.7 | 15.7 ± 1.4 |
| Preinjury sports (rank order), % | |||
| First | Soccer: 50 | Soccer: 32 | Soccer: 55 |
| Second | Basketball: 22 | Lacrosse: 26 | Basketball: 24 |
| Third | Lacrosse: 15 | Football/basketball: 17 | Lacrosse: 12 |
aValues are presented as mean ± SD.
Table 2.
Anatomic Measurements for the Patients With Available MRI in the Braced Cohorta
| Total (n = 86) | Male (n = 20) | Female (n = 66) | |
|---|---|---|---|
| Tibial slope, deg | |||
| Lateral | 6.8 ± 3.3 | 6.2 ± 2.8 | 7.0 ± 3.5 |
| Medial | 6.0 ± 1.0 | 5.3 ± 3.1 | 6.2 ± 2.8 |
| Coronal | 4.9 ± 2.7 | 5.7 ± 3.1 | 4.6 ± 2.5 |
| Medial tibial depth, mm | 1.6 ± 1.0 | 1.4 ± 0.8 | 1.7 ± 1.1 |
| Notch width, mm | 17.1 ± 3.2 | 18.5 ± 3.0 | 16.7 ± 3.2 |
aValues are presented as mean ± SD. MRI, magnetic resonance imaging.
Table 3.
Baseline Demographic Data for the Patients in the Unbraced Cohort26
| Total (n = 140) | Male (n = 86) | Female (n = 54) | |
|---|---|---|---|
| Age at surgery,a y | 17.1 ± 1.8 | 17.4 ± 1.7 | 16.6 ± 1.8 |
| Preinjury sports (rank order), % | |||
| First | Soccer: 38 | Soccer: 45 | Basketball: 46 |
| Second | Basketball: 34 | Basketball: 26 | Soccer: 30 |
| Third | Rugby: 5 | Rugby: 8 | Gymnastics/dance: 7 |
aValues are presented as mean ± SD.
Compliance With Recommended Brace Use
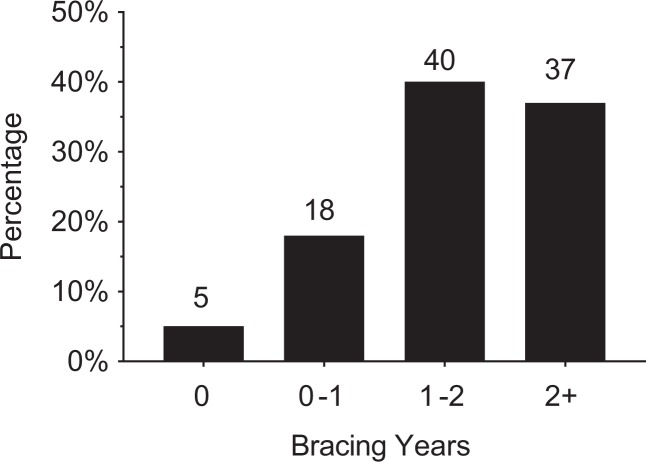
Of 135 patients, 128 (95%) reported wearing a brace following surgery, and 104 (77%) reported wearing a brace for more than 1 year following surgery (Figure 1).
Figure 1.
Frequency distribution of bracing years (n = 135).
Return to Sport
Of the respondents in the braced cohort, 63% reported having returned to very strenuous activity, including jumping and pivoting, as in football, basketball, or soccer, at follow-up. In the unbraced historic cohort, 88% of the patients reported a return to strenuous activity. The mean Marx score in the braced cohort at follow-up was 8, with 96 of 135 (71%) having a score ≥4 (which requires cutting, pivoting, or deceleration at least once a month) and 39 (29%) having a score ≥12 (a score that corresponds to performing cutting, pivoting, or deceleration activities 2 to 3 times per week).
Graft Injury Rate
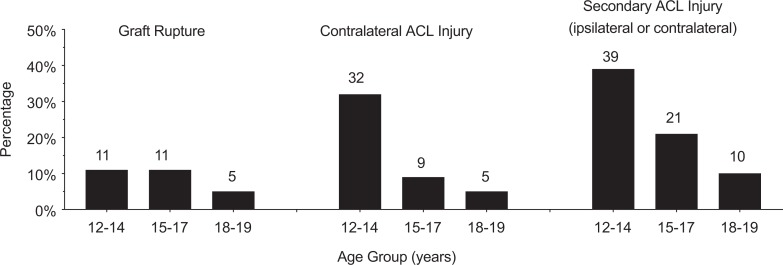
In the braced cohort, graft injury occurred in 14 patients (10%) at a mean 2.3 years, with the earliest occurring at 22 weeks and the latest occurring at 5.8 years after the initial ACL reconstruction. Out of the 14 graft injuries, 2 (14%) occurred within the first postoperative year and 5 (36%) occurred within the first 2 years following surgery. Graft rupture rates for different age groups are shown in Figure 2. Graft rupture rates categorized by sex and age stratification are displayed in Table 4. Of 115 patients 17 years of age and younger, 13 (11%) had a subsequent graft injury, as opposed to 1 of 20 (5%) patients 18 and 19 years of age. Of 13 patients, 7 (54%) were wearing a brace at the time of graft rupture. One of the patients with a torn graft did not answer the brace use question. Of those patients who had a graft rupture, 7 of 14 (50%) underwent revision ACL reconstruction.
Figure 2.
Percentage of patients who sustained a graft rupture, contralateral ACL injury, and overall secondary ACL injury (ipsilateral or contralateral) per age group: 12-14 years (n = 28), 15-17 years (n = 87), and 18-19 years (n = 20). ACL, anterior cruciate ligament.
TABLE 4.
Graft Rupture Rates Categorized by Age and Sex
| Patients, n (%) | ||
|---|---|---|
| Age at Surgery, y | Male | Female |
| <18 | 4 of 21 (18) | 9 of 96 (10) |
| 18 or 19 | 0 of 10 (0) | 1 of 10 (10) |
Contralateral ACL Injury Rate
In the braced cohort, contralateral injury occurred in 18 patients (13%) at a mean 2.4 years, with the earliest occurring at 41 weeks and the latest occurring at 5.7 years. Of the 18 contralateral injuries, 4 (22%) occurred within the first postoperative year and 8 (44%) occurred with the first 2 years following surgery. Contralateral injury rates for each age group are shown in Figure 2. Contralateral ACL injury rates categorized by sex and age are displayed in Table 5. Out of 115 patients 17 years of age and younger, 17 (15%) had a subsequent contralateral ACL injury, as opposed to 1 of 20 (5%) patients 18 and 19 years of age. Of 18 patients who had a contralateral tear, 10 (56%) were wearing a functional brace on the postoperative knee when they were injured. All patients who suffered a contralateral ACL injury underwent ACL reconstruction.
TABLE 5.
Contralateral ACL Injury Rates Categorized by Age and Sexa
| Patients, n (%) | ||
|---|---|---|
| Age at surgery, y | Male | Female |
| <18 | 1 of 21 (5) | 16 of 94 (17) |
| 18 or 19 | 0 of 10 (0) | 1 of 10 (10) |
aACL, anterior cruciate ligament.
Combined Graft and Contralateral ACL Injury Rates
One patient sustained both a graft rupture and a contralateral ACL injury on separate occasions. This patient was 12 years of age at the time of the first ACL surgery and was wearing a brace on the indexed knee when she sustained a graft rupture and contralateral ACL injury. The total number of patients who had at least 1 subsequent ACL injury to either knee following their primary surgery was 31 (23%). Combined secondary ACL or graft injury rates for each age group are shown in Figure 2. Secondary ACL or graft rupture rates categorized by sex and age stratification are displayed in Table 6. The highest reinjury rate was in the youngest-age female group (<18 years) at 26%. Of 115 patients younger than 18 years, 29 (25%) had a subsequent graft rupture or contralateral ACL injury, as opposed to 2 of 20 (10%) patients 18 and 19 years of age.
TABLE 6.
Combined Secondary (Graft Rupture or Contralateral) ACL Injury Rates Categorized by Age and Sexa
| Patients, n (%) | ||
|---|---|---|
| Age at Surgery, y | Male | Female |
| <18 | 5 of 21 (24) | 24 of 94 (26) |
| 18 or 19 | 0 of 10 (0) | 2 of 10 (20) |
aACL, anterior cruciate ligament.
Differences in Injury Rates Between the Braced and Unbraced Cohorts
The differences in graft, contralateral ACL, and combined injury rates between the braced cohort reported in this study and the unbraced cohort reported by Webster and Feller26 are presented in Table 7 with the netball and Australian football athletes excluded. For the same analysis with those athletes included, see Appendix Table A1.
TABLE 7.
Differences in Injury Rates Between the Braced and Unbraced Cohortsa
| Injury Rates, n (%) | |||
|---|---|---|---|
| Braced | Unbraced | P Value | |
| Graft injury | |||
| Overall | 14 of 135 (10) | 29 of 140 (21) | .028 |
| <18 y | 13 of 115 (11) | 22 of 89 (25) | .012 |
| 18 and 19 y | 1 of 20 (5) | 7 of 51 (14) | .427 |
| Male | 4 of 31 (13) | 20 of 86 (23) | .302 |
| Female | 10 of 104 (10) | 9 of 54 (17) | .207 |
| Early graft injuryb | |||
| Overall | 2 of 135 (1) | 12 of 140 (9) | .011 |
| <18 y | 2 of 115 (2) | 11 of 89 (12) | .003 |
| 18 and 19 y | 0 of 20 (0) | 1 of 51 (2) | .999 |
| Male | 1 of 31 (3) | 9 of 86 (11) | .287 |
| Female | 1 of 104 (1) | 3 of 54 (6) | .116 |
| Contralateral ACL injury | |||
| Overall | 18 of 135 (13) | 17 of 140 (12) | .857 |
| <18 y | 17 of 115 (15) | 11 of 89 (12) | .685 |
| 18 and 19 y | 1 of 20 (5) | 6 of 51 (12) | .664 |
| Male | 1 of 31 (3) | 11 of 86 (13) | .178 |
| Female | 17 of 104 (16) | 6 of 54 (11) | .479 |
| Combined secondary injury | |||
| Overall | 31 of 135 (23) | 45 of 140 (32) | .106 |
| <18 y | 29 of 115 (25) | 32 of 89 (36) | .123 |
| 18 and 19 y | 2 of 20 (10) | 13 of 51 (26) | .204 |
| Male | 5 of 31 (15) | 30 of 86 (35) | .067 |
| Female | 26 of 104 (25) | 15 of 54 (28) | .848 |
aSignificant differences are highlighted in bold. ACL, anterior cruciate ligament.
bWithin the first year after surgery.
Predictors of Injury
Details of all the associations between the demographic and anatomic predictors and risk of secondary ACL injuries are presented in Appendix Tables A2 through A4. None of the studied factors were associated with the risk of graft injury (P > .06) (Appendix Table A2). Younger age (β = –0.6; OR, 0.54; P = .005) was predictive of increased risk of contralateral ACL injury (Appendix Table A3). Younger age (β = –0.36; OR, 0.70; P = .021), family history of an ACL injury (β = 1.03; OR, 2.81; P = .015), and higher lateral tibial slope (β = 0.23; OR, 1.25; P = .016) were predictive of increased risk of secondary ACL injury to either knee (Appendix Table A4).
Discussion
Numerous studies have reported on the high rate of secondary ACL injuries to either knee (17%-37%) following initial injury in younger patients.12,20,22,24,28 This study confirms the high rate of secondary ACL injuries in younger patients and also examines the effect of functional bracing following ACL reconstruction. A recent systematic review regarding functional bracing following ACL reconstruction concluded that there was limited evidence to support the use of routine bracing to decrease the rate of reinjury after ACL reconstruction.17 Despite the high rate of second ACL injury found in this study, when compared with an unbraced cohort, a braced adolescent group had a significantly decreased risk of graft rupture, in particular patients 17 years of age and younger at the time of ACL reconstruction. Thus, clinicians treating adolescent patients may want to consider the use of functional bracing after ACL reconstruction in this patient population.
Risk of secondary ACL injury has also been linked to postoperative activity level.2,11 A 63% rate of return to cutting and pivoting sports was found for the patients in this study. This is similar to that reported in a systematic review and meta-analysis of 48 studies and 5770 participants after ACL reconstruction surgery,1 where 2 in 3 individuals returned to their previous level of sport. This is also consistent with more recent reports suggesting that approximately half of athletes aged 25 years and younger have returned to level 1 sports at 1 year after surgery.27 In addition, this cohort of patients had a median postoperative Marx score of 8 at the time of the survey (mean, 5.6 years). This is consistent with prior work that reported a median Marx activity level of 9 points at 2 years after surgery and 7 points at 6 years after surgery in a cohort of more than 1500 patients.17 The observed injury patterns showed that the rates of graft rupture were higher in patients younger than 18 years (11%) as compared with those 18 and 19 years of age (5%). This trend was similar to that observed in an unbraced cohort where patients younger than 18 years and male patients exhibited the highest rate of graft injury.26 The overall graft retear rate in the braced cohort was half of that seen in the unbraced cohort (10% vs 21%). Similar trends were observed by comparing the graft retear rates across each age and sex subgroup, with statistically significant findings for the group younger than 18 years showing decreased retear rates in the braced cohort.
Interestingly, the early graft tear rate (within 1 year of surgery) was lower in the braced group than in the unbraced group, in particular among those younger than 18 years (2% vs 12%). This is an important consideration, as previous investigators reported that the majority of graft ruptures and ACL revision procedures occur within the first 1 to 2 years after initial surgery.15,26 Also, histologic studies suggest that hamstring tendon autografts are in the “remodeling phase” within this time frame, potentially the phase where the graft is at greatest risk.21 This information suggests that younger patients who undergo primary ACL reconstruction with hamstring autograft should delay return to strenuous activity for at least 1 year, preferably 2 years. However, in this young population, it may be difficult to achieve compliance where athletes are focused on returning to sport as soon as possible. Our findings suggest that functional bracing may provide a benefit of decreased risk of graft tear during this early period of return. Furthermore, our study shows that functional bracing compliance is relatively high in this age group, with 77% of patients reporting wearing a brace for sports for at least 1 to 2 years following surgery.
One of the concerns about the use of functional bracing is the effect that the brace may have on contralateral injury rates.17 No statistically significant difference was observed in contralateral ACL injury rates after ACL reconstruction between the unbraced cohort and the patients with functional bracing. This lack of difference could have been due to our limited sample size. Further studies with a larger sample size are required to determine whether bracing can influence the contralateral ACL injury risk.
In addition, this study found that a high lateral tibial slope, younger age, and family history of ACL injury are risk factors for secondary ACL injury, even in patients who use postoperative functional bracing. Prior studies have shown increased risk of graft failure and contralateral ACL injury in patients with a steep lateral tibial slope.5,13,14,23,25 Similarly, younger age and family history of ACL injury have been linked to increased risk of secondary ACL injury.4,26,28 Our results confirm those earlier observations and further highlight the importance of these factors as they continue to influence the risk of injury. Additional injury prevention strategies (ie, neuromuscular training, physical activity modification) should be considered for patients with these risk factors in an effort to lower the risk of secondary ACL injuries.
This study has several limitations. There are several ways that the patients studied here differed from those of the previously reported unbraced cohort, including age, sex, sports participation, and rehabilitation. The rehabilitation protocol used in the unbraced group had weightbearing as tolerated starting on the first day, where the braced group had partial weightbearing for 4 weeks. Other rehabilitation factors were similar, including an early emphasis on the regaining of full extension and quadriceps strength. At a mean 4.8 years (unbraced) and 5.7 years (braced) after surgery, return to strenuous sport was 88% in the unbraced cohort and 63% in the braced cohort. As neither cohorts prospectively collected the return to sport data, we could not assess whether one group or another had an actual difference in the timing of return to sport and to what sport they returned in the early postoperative period, when most graft failures occurred. Moreover, when a historical cohort is being used for comparison, there may be other confounding factors not accounted for, and the effect of bracing cannot truly be known until participants are randomized. We attempted to minimize those effects by including patients with similar sports types, as well as stratifying the results by age and sex. Another major limitation of our study is the low follow-up rate (65%). Prior studies of adolescent patients have reported rates of follow-up of between 75% and 89%.22,24,26,28 Our lower follow-up rate can be explained by the lack of postoperative bracing compliance information in the medical record and the need for direct patient communication, which inherently yields a decreased follow-up rate. In addition, there is always the risk for recall bias in a retrospective study and especially in our cohort, where functional bracing use and compliance cannot be confirmed through the medical record. Finally, our small sample size and limited number of reinjuries may have influenced our ability to properly determine the effect of bracing on risk of secondary ACL injuries. While no definitive conclusions can be drawn from these findings, our results highlight the need for further studies with large sample sizes and a prospective design.
Of note, patients who had a contralateral ACL injury had subsequent ACL surgery in all cases, while approximately half of those who had a graft retear underwent additional ACL surgery on that knee. Thus, if we had only queried whether patients had revision ACL surgery, we may have missed a large percentage of patients who sustained a graft injury. This discrepancy between reinjury rate and revision rate may be the result of multiple factors. Patients may be more amenable to activity modification because of (1) a gradual lifestyle adoption that involves less cutting and pivoting sports activity or (2) a reluctance to undergo a surgical procedure that had already failed in their case. Future studies should specify whether graft failure rates are those due to reinjury versus revision surgery, as these rates may not be the same in all patient populations.
In summary, the results of this study confirm the high ACL reinjury rates in younger patients who undergo an ACL reconstruction, while adding to the evidence base regarding prescription and use of postoperative functional ACL bracing. The data suggest that functional bracing may help minimize the number of subsequent ACL injuries in young patients undergoing primary ACL reconstruction with hamstring autograft.
Acknowledgment
The authors acknowledge the contributions of Dr Julian Feller, particularly with regard to his work on the initial project with Dr Kate Webster.
Appendix
Figure A1.
Measurement techniques used to quantify notch width (NW), coronal tibial slope (CTS), medial tibial slope (MTS), medial tibial depth (MTD), and lateral tibial slope (LTS).
TABLE A1.
Differences in Injury Rates Between the Braced and Unbraced Cohorts Including Participants Playing Australian Rules Football and Netballa
| Injury Rates, n (%) | P | ||
|---|---|---|---|
| Braced | Unbraced | ||
| Graft injury | |||
| Overall | 14 of 135 (10) | 57 of 316 (18) | .048 |
| Age <18 y | 13 of 115 (11) | 39 of 168 (23) | .012 |
| Age 18 and 19 y | 1 of 20 (5) | 18 of 148 (12) | .476 |
| Male patients | 4 of 31 (13) | 44 of 200 (22) | .342 |
| Female patients | 10 of 104 (10) | 13 of 116 (11) | .826 |
| Early graft injuryb | |||
| Overall | 2 of 135 (1) | 27 of 316 (9) | .005 |
| Age <18 y | 2 of 115 (2) | 23 of 168 (14) | <.001 |
| Age 18 and 19 y | 0 of 20 (0) | 4 of 148 (3) | .999 |
| Male patients | 1 of 31 (3) | 22 of 200 (11) | .219 |
| Female patients | 1 of 104 (1) | 5 of 116 (4) | .216 |
| Contralateral ACL injury | |||
| Overall | 18 of 135 (13) | 56 of 316 (18) | .270 |
| Age <18 y | 17 of 115 (15) | 31 of 168 (19) | .427 |
| Age 18 and 19 y | 1 of 20 (5) | 23 of 148 (16) | .314 |
| Male patients | 1 of 31 (3) | 36 of 200 (18) | .061 |
| Female patients | 17 of 104 (16) | 20 of 116 (17) | .999 |
| Combined secondary injury | |||
| Overall | 31 of 135 (23) | 110 of 316 (35) | .015 |
| Age <18 y | 29 of 115 (25) | 74 of 168 (44) | .007 |
| Age 18 and 19 y | 2 of 20 (10) | 36 of 148 (24) | .171 |
| Male patients | 5 of 31 (15) | 76 of 200 (38) | .025 |
| Female patients | 26 of 104 (25) | 34 of 116 (29) | .545 |
a Significant differences are highlighted in bold (P ≤ .05). ACL, anterior cruciate ligament.
bWithin the first year of surgery.
TABLE A2.
Demographic and Anatomic Predictors of ACL Graft Injurya
| Predictor | Slope, β | P Value | Odds Ratio (95% CI) |
|---|---|---|---|
| Female sex | –0.33 | .599 | 0.72 (0.21-2.47) |
| Age | –0.14 | .484 | 0.87 (0.59-1.29) |
| Contact injury | 0.46 | .431 | 1.59 (0.50-5.01) |
| Family history of ACL injury | 0.94 | .100 | 2.56 (0.84-7.84) |
| Tibial slope | |||
| Lateral | 0.18 | .110 | 1.20 (0.95-1.50) |
| Medial | 0.04 | .735 | 1.04 (0.83-1.30) |
| Coronal | 0.25 | .065 | 1.28 (0.98-1.67) |
| Medial tibial depth | –0.21 | .553 | 0.81 (0.40-1.63) |
| Notch width | 0.10 | .325 | 1.11 (0.91-1.35) |
aACL, anterior cruciate ligament.
TABLE A3.
Demographic and Anatomic Predictors of Contralateral ACL Injurya
| Predictor | Slope, β | P Value | Odds Ratio (95% CI) |
|---|---|---|---|
| Female sex | 1.77 | .092 | 5.86 (0.75-45.95) |
| Age | –0.61 | .005 | 0.54 (0.36-0.83) |
| Contact injury | –0.70 | .215 | 0.50 (0.16-1.50) |
| Family history of ACL injury | 0.71 | .169 | 2.04 (0.74-5.61) |
| Tibial slope | |||
| Lateral | 0.14 | .180 | 1.15 (0.94-1.41) |
| Medial | –0.02 | .848 | 0.98 (0.79-1.21) |
| Coronal | 0.09 | .410 | 1.09 (0.87-1.38) |
| Medial tibial depth | 0.30 | .244 | 1.35 (0.82-2.22) |
| Notch width | 0.09 | .316 | 1.10 (0.91-1.32) |
aACL, anterior cruciate ligament.
TABLE A4.
Demographic and Anatomic Predictors of Secondary ACL Injury (Graft or Contralateral ACL)a
| Predictor | Slope, β | P Value | Odds Ratio (95% CI) |
|---|---|---|---|
| Age | –0.36 | .021 | 0.70 (0.52-0.95) |
| Contact injury | –0.19 | .659 | 0.83 (0.36-1.90) |
| Family history of ACL injury | 1.03 | .015 | 2.81 (1.22-6.47) |
| Tibial slope | |||
| Lateral | 0.23 | .016 | 1.25 (1.04-1.51) |
| Medial | 0.01 | .923 | 1.00 (0.85-1.20) |
| Coronal | 0.19 | .055 | 1.22 (0.99-1.48) |
| Medial tibial depth | 0.18 | .429 | 1.20 (0.77-1.87) |
| Notch width | 0.16 | .061 | 1.18 (1.00-1.38) |
aACL, anterior cruciate ligament.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Medical School, Harvard University or its affiliated academic health care centers, the National Football League Players Association, or Boston Children’s Hospital.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding for this study was provided from the Children’s Hospital Orthopaedic Surgery Foundation and the Children’s Hospital Sports Medicine Foundation. This research was also conducted with support from the Football Players Health Study at Harvard University. The Football Players Health Study is funded by a grant from the National Football League Players Association. M.M.M. and Boston Children’s Hospital have equity interests in MIACH Orthopaedics, a company that has licensed the BEAR scaffolding technology from Boston Children’s Hospital. M.M.M. has received royalties from Springer Publishing; research support from the National Institutes of Health, Department of Defense, and National Football League Players Association through the Harvard Football Players Health Study; and honoraria from the Musculoskeletal Transplant Foundation. A.M.K. receives research support from the National Institutes of Health and National Football League Players Association through the Harvard Football Players Health Study. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Boston’s Children Hospital Institutional Review Board (IRB-P00023197).
References
- 1. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. [DOI] [PubMed] [Google Scholar]
- 2. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37(12):2362–2367. [DOI] [PubMed] [Google Scholar]
- 3. Bordes P, Laboute E, Bertolotti A, et al. No beneficial effect of bracing after anterior cruciate ligament reconstruction in a cohort of 969 athletes followed in rehabilitation. Ann Phys Rehabil Med. 2017;60(4):230–236. [DOI] [PubMed] [Google Scholar]
- 4. Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985–1992. [DOI] [PubMed] [Google Scholar]
- 5. Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(10):2510–2514. [DOI] [PubMed] [Google Scholar]
- 6. Decoster LC, Vailas JC. Functional anterior cruciate ligament bracing: a survey of current brace prescription patterns. Orthopedics. 2003;26(7):701–706. [DOI] [PubMed] [Google Scholar]
- 7. Delay BS, Smolinski RJ, Wind WM, Bowman DS. Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. Am J Knee Surg. 2001;14(2):85–91. [PubMed] [Google Scholar]
- 8. Feller JA, Cooper R, Webster KE. Current Australian trends in rehabilitation following anterior cruciate ligament reconstruction. Knee. 2002;9(2):121–126. [DOI] [PubMed] [Google Scholar]
- 9. Hashemi J, Chandrashekar N, Gill B, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90(12):2724–2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Consortium M, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kamath GV, Murphy T, Creighton RA, Viradia N, Taft TN, Spang JT. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: analysis of an NCAA Division I cohort. Am J Sports Med. 2014;42(7):1638–1643. [DOI] [PubMed] [Google Scholar]
- 13. Levins JG, Argentieri EC, Sturnick DR, et al. Geometric characteristics of the knee are associated with a noncontact ACL injury to the contralateral knee after unilateral ACL injury in young female athletes. Am J Sports Med. 2017;45(14):3223–3232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Levins JG, Sturnick DR, Argentieri EC, et al. Geometric risk factors associated with noncontact anterior cruciate ligament graft rupture. Am J Sports Med. 2016;44(10):2537–2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551–1557. [DOI] [PubMed] [Google Scholar]
- 16. Lowe WR, Warth RJ, Davis EP, Bailey L. Functional bracing after anterior cruciate ligament reconstruction: a systematic review. J Am Acad Orthop Surg. 2017;25(3):239–249. [DOI] [PubMed] [Google Scholar]
- 17. Moon Knee Group, Spindler KP, Huston LJ, et al. Ten-year outcomes and risk factors after anterior cruciate ligament reconstruction: a MOON longitudinal prospective cohort study. Am J Sports Med. 2018;46(4):815–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Park JS, Nam DC, Kim DH, Kim HK, Hwang SC. Measurement of knee morphometrics using MRI: a comparative study between ACL-injured and non-injured knees. Knee Surg Relat Res. 2012;24(3):180–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pauzenberger L, Syré S, Schurz M. “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy. 2013;29(10):1712–1721. [DOI] [PubMed] [Google Scholar]
- 22. Pinczewski LA, Morgan M, Salmon LJ, Waller A, Thompson S, Roe JP. 15 year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and under. Orthop J Sports Med. 2015;3(3)(suppl):2325967115S2325900007. [DOI] [PubMed] [Google Scholar]
- 23. Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA. 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46(3):531–543. [DOI] [PubMed] [Google Scholar]
- 24. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. [DOI] [PubMed] [Google Scholar]
- 25. Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41(12):2800–2804. [DOI] [PubMed] [Google Scholar]
- 26. Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
- 27. Webster KE, Feller JA. Return to level I sports after anterior cruciate ligament reconstruction: evaluation of age, sex, and readiness to return criteria. Orthop J Sports Med. 2018;6(8):2325967118788045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–647. [DOI] [PubMed] [Google Scholar]
- 29. Whitney DC, Sturnick DR, Vacek PM, et al. Relationship between the risk of suffering a first-time noncontact ACL injury and geometry of the femoral notch and ACL: a prospective cohort study with a nested case-control analysis. Am J Sports Med. 2014;42(8):1796–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]