Introduction
Unequivocally, vaccinations can be considered one of the greatest global achievements for public health. Since the introduction of the first vaccines, vaccination programs have contributed to a substantial decline in both mortality and morbidity of many previously lethal infectious diseases around the globe.1 However, high and sustained vaccine uptake is necessary for these efforts to remain successful. Beyond the direct protection provided for vaccinated individuals, high vaccine coverage also induces indirect protection against vaccine-preventable diseases (VPD) at a population level through herd immunity.2 Yet despite consensus on the public health benefits of vaccination, recent reports of clustered outbreaks and the resurgence of VPDs in under- or nonimmunized groups3 highlight the ongoing challenges.
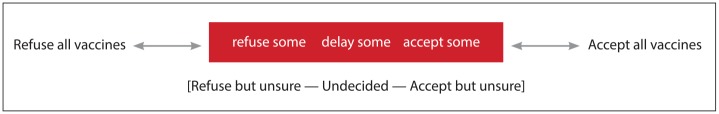
The concept of vaccine hesitancy represents a significant conceptual shift away from the traditional dichotomy of accept or reject, of pro- or antivaccine. Defined by the World Health Organization’s (WHO) SAGE Working Group as “the delay in acceptance or refusal of vaccination despite availability of vaccination services,” vaccine hesitancy is “complex and context specific, varying across time, place and vaccines. It is influenced by factors such as complacency, convenience and confidence.”4 Vaccine hesitancy highlights the wide spectrum of vaccination beliefs, attitudes and behaviours of a large heterogeneous group of individuals situated between the 2 end points of the continuum (see Figure 1). For example, vaccine-hesitant individuals may refuse some vaccines but accept or delay others; some may accept a vaccine but remain concerned with their decision; and others may even personally refuse all vaccines but remain supportive of vaccinations more broadly. While vaccine hesitancy is not always the root cause of under- or nonimmunization, it is listed in the top 10 threats to global health for 2019 by the WHO5 and remains an important contributor to suboptimal vaccine coverage across many jurisdictions.6-8
Figure 1.
Spectrum of vaccine hesitancy
A large body of interdisciplinary research has explored the factors and determinants that shape vaccine-hesitant beliefs, attitudes and behaviours.2,9-12 From a practice perspective, 3 observations are particularly important:
Individual determinants of vaccine hesitancy never act in isolation.
The same determinant cannot be assumed to influence in the same direction across different contexts or vaccines.
These factors and determinants are never static.
Thus, vaccine-hesitant individuals are not static on the continuum but move dynamically across the spectrum over time, context and across different vaccines. For pharmacists, this complex and context-specific interplay of determinants and factors can pose a real challenge when engaging with hesitant individuals about vaccination; however, the potential for influencing movement across the spectrum also presents a great opportunity, particularly for adult vaccination.
Assumption of binary vaccination outcomes continues to impact pharmacy practice
Beyond identifying the determinants and factors contributing to vaccine hesitancy, considerably less attention has been paid to exploring how pharmacists and other health care providers understand the concept of vaccine hesitancy and address it in practice. For example, the current WHO definition recognizes the complexity of factors influencing vaccination beliefs but still retains a focus on the binary behavioural outcome of vaccination or nonvaccination.13 Ongoing research at the University of Waterloo’s School of Pharmacy suggests that many pharmacists also continue to perceive vaccination as binary (limited to only 2 potential outcomes) and static, which can have a number of important, albeit unintended consequences for practice:
Engagement with vaccine-hesitant individuals in the community pharmacy is frequently framed directly within the context of binary behavioural outcomes (e.g., will you be getting your vaccine today?). This may limit patients’ options to either receiving or not receiving a vaccine, thereby narrowing the space for effective conversations.
The binary outlook also often leads to assumptions that all vaccine-hesitant individuals are “anti-vaxxers.” This may limit engagement with patients who can be positively influenced by having their concerns or questions addressed. This also minimizes pharmacists’ self-perceived abilities to influence vaccination decisions.
Fear that all vaccine-hesitant individuals are “anti-vaxxers” and/or that discussions with them may quickly escalate into arguments may prevent proactive initiation of engagement by the pharmacist. Accordingly, pharmacists may wait until patients voluntarily express their interest in vaccination, rather than inquiring about vaccination status among all patients who could benefit from vaccination.
While administration of the vaccine might be the optimal outcome, it is not the only positive outcome. Nudging vaccine-hesitant individuals across the spectrum of hesitancy is arguably just as valuable. Recognizing positive progress towards a goal is well established across other clinical areas such as smoking cessation, weight loss and other lifestyle modifications; however, the same perspective has not yet been widely adopted for vaccine hesitancy. This may stem from the fact that publicly funded remuneration to pharmacies related to vaccinations is currently provided only upon administration of the vaccine, not for a consultation that does not result in vaccination.14,15
Patient engagement and addressing vaccine hesitancy in practice
Research consistently shows that health care provider recommendations are one of the strongest predictors of vaccination.16,17 This is particularly important in community pharmacy, as patients increasingly consider their pharmacist not only a trusted immunizer but also a trusted source of health and vaccination information.18 By framing conversations with patients beyond the binary yes/no decision to vaccinate (e.g., “Do you have any questions about the vaccine?” instead of “Will you be getting your vaccine?”), community pharmacists can focus on proactively engaging with patients to discuss their concerns, address relevant knowledge gaps and provide high-quality evidence-based information outside of the context of a completed vaccination. This effectively opens up the space for productive vaccine conversations with patients at every interaction. To be sure, initiating patient engagement with a focus on nudging patients towards making positive vaccine decisions (rather than simply aiming for a completed vaccination) truly capitalizes on the pharmacists’ dual role as both an educator and an immunizer (see Table 1).
Table 1.
Addressing vaccine hesitancy: Tips for communication
| Engage | Frame the conversation beyond a binary yes/no vaccination decision. |
| Listen | Listen to and acknowledge patient concerns without judgement. |
| Correct | Correct misinformation, accept questions and explain the relevant scientific findings. |
| Avoid | Avoid debating back and forth. |
| Remind | Remind of the benefits of vaccinations and point out the risk of not immunizing. |
| Provide | Provide fact sheets and other resources about vaccination (e.g., websites). |
| Accommodate | Accommodate patient requests (e.g., alternative schedule) as clinically appropriate within scope of practice. |
| Examples | Provide personal examples (own vaccination/examples of vaccine-preventable diseases in practice). |
| Nudge | Positively nudge patient further along the vaccine hesitancy continuum and recognize that a completed immunization is not the only acceptable outcome. |
| Refer | Refer patient to other providers or schedule another appointment to discuss remaining vaccination concerns. |
If engagement is restricted only to patient-initiated interactions, there are countless missed opportunities. However, we recognize that the ability for pharmacists to offer such interactions is often constrained by limited pharmacy resources such as staffing, time and remuneration for services. According to results of a recent survey with health care providers, 87% of front-line vaccine providers reported that vaccine hesitancy resulted in increased time spent discussing vaccination issues with concerned patients.13 However, a number of resources are available to help structure these conversations in an efficient and effective manner and to minimize potential drain on pharmacy resources (Box 1). Interactions can also be tailored more effectively by first identifying the individual’s specific questions and concerns, thereby reducing the time spent discussing other vaccination details that are not of greatest relevance to the individual’s decision.
Box 1 Communication resources to support productive vaccine conversations.
OHRI—Patient decision aids www.decisionaid.ohri.ca
PHAC—Communicating effectively about immunization www.phac-aspc.gc.ca
CDC—Provider resources for vaccine conversations www.cdc.gov
ECDC—Let’s talk about protection www.ecdc.europa.eu
WHO—Vaccination and trust www.euro.who.int
Recognizing individuals’ potential to move both backwards and forwards along the vaccine hesitancy continuum over time, context and across different vaccines, the nature of interactions can also be tailored to a patient’s current state. While this article has generally focused on interactions with vaccine-hesitant individuals, consideration of the vaccine-hesitancy spectrum and its fluidity can also be applied to those who have made the decision to be vaccinated. For example, individuals requesting or strongly considering vaccination will benefit from interactions that utilize positive reinforcement to improve patient satisfaction, trust and sustain motivation across time and other vaccines. This is an important yet often-overlooked goal, particularly since positive prior vaccine experience (including effective management of any adverse events) is an important determinant of future vaccine acceptance.10
Conclusion
A key challenge of vaccination lies not with the small vocal minority of outright vaccine refusers, but rather with those who are hesitant to vaccinate. When engaging with the latter group, it is important for community pharmacists to move beyond the usual assumptions of binary vaccination outcomes and instead focus on positively moving individuals further along the vaccine-hesitancy continuum and to support them in making informed vaccine decisions in their own time. Pharmacists should continue to capitalize on their role as educators and public health advocates. While reaching a vaccine decision may not happen during a single interaction, it should be acknowledged that this is perfectly acceptable. Even if no remuneration is obtained for administering a vaccination during a specific encounter, continued positive interactions with pharmacists can foster patient trust and loyalty for future health care needs and may ultimately increase the chances of future vaccination.
This series of articles has been accredited for 1.75 CEUs under CCCEP file #: 8002-2019-2888-I-P. To earn your CEUs, please review each article, then click on www.pharmacists.ca/immunizers to complete a series of short assessments.
Footnotes
ORCID iD:Richard Violette  https://orcid.org/0000-0002-7773-1202
https://orcid.org/0000-0002-7773-1202
References
- 1. World Health Organization. Global vaccine action plan 2011-2020. 2013:1-77. Available: https://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/ (accessed Dec. 15, 2018). [Google Scholar]
- 2. Dube E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother 2013;9(8):1763-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Public Health Agency of Canada. Vaccine preventable disease. Surveillance report to December 31, 2015. 2017;2561-312X:1-60. Available: https://www.canada.ca/en/public-health/services/publications/healthy-living/vaccine-preventable-disease-surveillance-report-december-31-2015.html (accessed Dec. 15, 2018).
- 4. SAGE Working Group on Vaccine Hesitancy. Report of the SAGE working group on vaccine hesitancy. 2014:1-63. Available: https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf (accessed Dec. 15, 2018).
- 5. World Health Organization. Ten threats to global health in 2019. Available: https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 (accessed Mar. 25, 2019).
- 6. Thomson A, Robinson K, Vallee-Tourangeau G. The 5As: a practical taxonomy for the determinants of vaccine uptake. Vaccine 2016;34(8): 1018-24. [DOI] [PubMed] [Google Scholar]
- 7. Thomson A, Watson M. Vaccine hesitancy: a vade mecum v1.0. Vaccine 2016;34(17):1989-92. [DOI] [PubMed] [Google Scholar]
- 8. Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Bohm R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One 2018;13(12):e0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Butler R, MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Diagnosing the determinants of vaccine hesitancy in specific subgroups: the guide to tailoring immunization programmes (TIP). Vaccine 2015;33(34):4176-9. [DOI] [PubMed] [Google Scholar]
- 10. MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine 2015;33(34): 4161-4. [DOI] [PubMed] [Google Scholar]
- 11. Dube E, Gagnon D, MacDonald N, Bocquier A, Peretti-Watel P, Verger P. Underlying factors impacting vaccine hesitancy in high-income countries: a review of qualitative studies. Expert Rev Vaccines 2018;17(11):989-1004. [DOI] [PubMed] [Google Scholar]
- 12. Taddio A, Ipp M, Thivakaran S, et al. Survey of the prevalence of immunization non-compliance due to needle fears in children and adults. Vaccine 2012;30(32):4807-12. [DOI] [PubMed] [Google Scholar]
- 13. Dube E, Gagnon D, Ouakki M, et al. Understanding vaccine hesitancy in Canada: results of a consultation study by the Canadian Immunization Research Network. PLoS One 2016;11(6):e0156118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Houle SK, Grindrod KA, Chatterley T, Tsuyuki RT. Publicly funded remuneration for the administration of injections by pharmacists: an international review. Can Pharm J (Ott) 2013;146(6):353-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Houle SKD, Carter CA, Tsuyuki RT, Grindrod KA. Remunerated patient care services and injections by pharmacists: an international update. J Am Pharm Assoc (2003) 2019;59(1):89-107. [DOI] [PubMed] [Google Scholar]
- 16. Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ; SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy: a systematic review. Vaccine 2015;33(34):4180-90. [DOI] [PubMed] [Google Scholar]
- 17. Dube E, Gagnon D, MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: review of published reviews. Vaccine 2015;33(34):4191-203. [DOI] [PubMed] [Google Scholar]
- 18. Alsabbagh MW, Church D, Wenger L, et al. Pharmacy patron perspectives of community pharmacist administered influenza vaccinations. Res Social Adm Pharm. 2019;15(2):202-6. [DOI] [PubMed] [Google Scholar]