Abstract
Anxiety is the most prevalent childhood psychopathology. Cognitive behavioural therapy is considered the most effective treatment, but outcomes remain variable. This study investigated children's communication patterns in child–therapist conversations and whether changes in these patterns, from rigid to more flexible, were associated with better treatment outcomes. Fifty‐three children (31% boys), with a mean age in years of M = 9.68 (SD = 1.85), completed a 12‐week cognitive behavioural therapy program. Maternal as well as children's reports of children's anxiety were assessed pretreatment and posttreatment. Additionally, 15‐min segments of two therapy sessions were audiotaped and children's conversational turns were coded for properties of response and initiative. The structure of children's communication patterns was further quantified using recurrence quantification analysis. As expected children entering treatment were characterised by rigid and inhibited conversational behaviour. Children who became less repetitive and deterministic over time had better maternal‐rated treatment outcomes. These findings did not generalize to child reports. Last, the hypothesis that the positive relation between the breaking of rigid communication patterns and treatment outcome would be mediated by increases in proactive conversational behaviours of the child was only partly supported. These study findings contribute to the emergent literature on processes of change in childhood anxiety treatment by providing initial support for the hypothesis that breaking rigid (communication) patterns may be a prerequisite of clinical change.
Keywords: childhood anxiety, clinical change, cognitive behavioural treatment, communication patterns, therapist‐client conversations
Key Practitioner Message.
Children with anxiety show rigid and withdrawn communication patterns at the beginning of treatment. Breaking rigid conversational behaviours may be a prerequisite of clinical change.
Taking into consideration a client's processes of change, including the process of breaking down rigid patterns, may ultimately allow us to personalize treatment, that is, tailor specific treatment elements to the current state that the client is in.
Cognitive behavioural therapy (CBT) is recognized as one of the most effective treatment strategies for children with anxiety (Cartwright‐Hatton, Roberts, Chitsabesan, Fothergill, & Harrington, 2004; Compton et al., 2004; Higa‐McMillan, Francis, Rith‐Najarian, & Chorpita, 2016; James, James, Cowdrey, Soler, & Choke, 2015). Unfortunately, effect sizes are moderate at best (Fisak, Richard, & Mann, 2011; Mychailyszyn, Brodman, Read, & Kendall, 2012) and a substantial group of children (around 40%) does not profit from CBT at all (James et al., 2015; Silverman, Pina, & Viswesvaran, 2008). Remarkably, decades of research on CBT have not resulted in higher average effect sizes nor has the rate of nonresponders improved over time (Johnsen & Friborg, 2015; Öst, 2008; Weisz et al., 2017).
One important reason for this lack of progress may be that CBT, all too often, is understood as a uniform process, that is, analogous to one type of prescribed pill that works the same for everyone (see Sparks, Duncan, & Miller, 2007, for a similar argument). Research shows that this is not the case, and we need to wonder what the underlying processes of change are that can help explain the variability in outcomes (Kazdin, 2007; Kazdin, 2009; Kazdin & Nock, 2003; Moses & Barlow, 2006; Pachankis & Goldfried, 2007; Rosen & Davison, 2003). Defining clients' processes of change that are associated with successful treatment outcomes may help us to inform clinicians how to personalize treatment (e.g., by adapting interventions to different clients or tailoring specific treatment elements to the current state of the client; Norcross & Wampold, 2011). This may be the only way to reduce the 40% “failures” and to significantly boost the effectiveness of CBT treatments. In this study, we attempted to pave the way towards a better understanding of intra‐individual processes of change. We hypothesised that a more general shift from rigidity towards flexibility is a prerequisite for clinical change. Specifically, we investigated whether changes in rigidity of microlevel in‐session communication patterns of children with anxiety were associated with treatment outcomes.
PROCESSES OF CHANGE
Although still in its infancy, there is accumulating research within the field of youth psychotherapy that focuses on processes of change and how they impact on treatment outcomes (see for meta‐analyses: Karver, De Nadai, Monahan, & Shirk, 2018; Karver, Handelsman, Fields, & Bickman, 2006; McLeod, 2011; Shirk, Karver, & Brown, 2011; and for a meta‐analytic review: Shirk & Karver, 2003). To our knowledge, there is only one systematic review that focuses specifically on CBT and children with anxiety (see Fjermestad, Mowatt Haugland, Heiervang, & Öst, 2009). An initial study by Chu and Kendall (2004) showed that observer‐based ratings of child involvement were associated with treatment outcomes. More specifically, they found that child involvement at midtreatment was positively related to treatment gains, whereas child involvement early in treatment was unrelated to treatment outcomes. In 2009, Chu and Kendall investigated child involvement in combination with therapist flexibility as an engagement strategy to increase child involvement. Again, results showed that late but not early child involvement was associated with better treatment outcomes. Further, therapist flexibility was unrelated to early child involvement but significantly predicted late child involvement, which predicted better treatment outcomes. These two studies together seem to suggest that positive involvement shifts, rather than initial levels, are predictive of better treatment outcomes.
These results are somewhat in contrast with the findings of a study by Hudson et al. (2014). In this study mean trajectories of process variables (i.e., alliance, child involvement, and therapist flexibility) across the course of treatment were examined. Child and therapist alliance showed a linear decreasing pattern over time, whereas child involvement and therapist flexibility showed a concave quadratic pattern over time, with peaks around midtreatment. Generally, initial values of process variables early in therapy were related as well as changes in these process variables over time. These findings are in line with a study by McLeod et al. (2014) that found a bidirectional relation between alliance and child engagement. The results by Hudson et al. showed that although the process variables were predictive of outcomes, it was mostly the initial values and not the changes over time that were related to treatment outcome, which is in contrast to the studies by Chu and Kendall (2004, 2009). There was some support that progressively increasing alliance and involvement positively impacts on treatment outcomes, but these findings were not consistent across reporters or time points.
Similar to the results of Chu and Kendall (2004, 2009) on involvement shifts, a study by Chiu, McLeod, Har, and Wood (2009) found that alliance shifts, that is, improvements in alliance from early to late treatment, were associated with better posttreatment outcomes. In contrast, a study by Liber et al. (2010) found mixed results concerning the outcome–alliance associations. No associations were found when using traditional measurements but a small association was found when using the reliable change index based on child‐reported anxiety symptoms. Interestingly, treatment adherence appeared to be unrelated to treatment outcome.
Together these studies provide initial albeit somewhat inconsistent evidence that the process factor child engagement and alliance are predictive of treatment outcome. The goal of the present study was to add to this growing body of research by investigating (changes in) moment‐to‐moment therapist–child interactions. More specifically we were interested in structural changes (i.e., relative rigidity versus flexibility) in children's communication patterns and whether these were associated with treatment outcomes. This process of changing rigid (communication) patterns towards more healthy and flexible patterns (of communication) has not been investigated in the field of CBT, nor in children with anxiety but has been put forward by psychotherapy researchers as a general process of change (Hayes & Strauss, 1998; Mahoney, 1991).
COMMUNICATION PATTERNS
Communication is central to psychological treatments. In fact, words are the primary medium of psychotherapy across orientations (Wachtel, 2011). They are however seldom the focus of research in this field (see for exceptions Moyers & Martin, 2006; Moyers, Martin, Houck, Christopher, & Tonigan, 2009; Ruiz‐Sancho, Frojan‐Parga, & Calero‐Elvira, 2013; Tomicic, Martinez, & Krause, 2015). From a constructivist communication science perspective, conversations provide a window into the inner lives of individuals (see Shotter, 1997, based on the work of language philosophers Bakhtin, 1984; Volosinov, 1973) and their characteristic ways of “being with others” (Lyons‐Ruth, 1999). Hence, studying clients' communication patterns and changes therein over the course of treatment may be an important indicator of the client's therapeutic change process.
To our knowledge, no research has investigated children's communication patterns and how those relate to treatment outcomes. From the literature, we do know that children with anxiety are generally characterised by withdrawn, inhibited and restricted ways of being with others (Rapee, Schniering, & Hudson, 2009). Moreover, they tend to behave anxiously during challenging (social) situations (Lau, Eley, & Stevenson, 2006) and display their distress with avoidant behaviours and/or withdrawal (Barlow, 2002). Also, peers view children with anxiety as shy and socially withdrawn (Strauss, Frame, & Forehand, 1987), and indeed, these children tend to be more passive, less actively engaged, and display more neutral affect in interactions with their friends compared to control children (Schneider, 2009). Thus, one might expect that children with anxiety generally enter treatment in a withdrawn, inhibited, and restricted way of being with others, being with their therapist (responding only minimally, for example, “yes,” “no” to the therapist's requests). A state of being that has evolved over the course of their lives and that can be defined as rigid, like a jailhouse with only very little movement (Bonanno & Burton, 2013; Hayes, Yasinski, Barnes, & Bockting, 2015; Kashdan, 2010; Mahoney, 1991; Schiepek, 2009).
BREAKING UP RIGID PATTERNS
A first step in the therapeutic process might then be to break this rigid state of being and shake loose old patterns to trigger a qualitative shift towards more healthy and flexible patterns of functioning (Hayes & Strauss, 1998; Mahoney, 1991). Something that we can observe particularly well in the treatment of anxiety disorders, in which exposure is one of the key evidence‐based ingredients (Higa‐McMillan et al., 2016). During exposure, a child's fear network becomes activated and then destabilized by disconfirmatory experiences, which is assumed to invoke a process of reorganization (Carey, 2011).
Several adult treatment studies have found that breaking down rigid patterns is a relevant process of change that is predictive of treatment outcomes (i.e., Gumz, Bauer, & Brähler, 2012; Hayes et al., 2015; Hayes & Strauss, 1998; Hayes & Yasinski, 2015; Heinzel, Tominschek, & Schiepek, 2014; Schiepek, Tominschek, & Heinzel, 2014). To our knowledge, only one study so far focused on this particular process of change in children. Lichtwarck‐Aschoff, Hasselman, Cox, Pepler, and Granic (2012) examined profiles of change in repeated mother–child interactions over the course of a 12‐week treatment period for childhood aggression. They found that children who showed a breaking down of rigid interaction patterns (i.e., a temporary increase in variability in mother‐child interactions) had better treatment outcomes. Taken together, these studies demonstrate that long‐term changes (i.e., improvement in therapeutic outcomes) are associated with intraindividual changes in variability at a week‐to‐week, day‐to‐day, or even moment‐to‐moment level. Building from these results, we expected that breaking down the rigid anxious state that children are in when entering treatment should manifest in the child's in‐session communication patterns. Further, we expected that shifts from being withdrawn and inhibited to being more engaged and proactive in their conversations with the therapist, would be a sign of positive therapeutic change and should thus relate to better treatment outcomes.
CURRENT STUDY
The general aim of this study was to investigate changes in children's communication patterns and whether these changes were associated with successful treatment outcomes in children with anxiety following a protocolized CBT program. Data were taken from a randomized controlled trial in which the effectiveness of the manualized CBT program developed by Bögels (2008) was evaluated against treatment as usual (see Jansen et al., 2012, for study protocol and Van Doorn, Jansen, Bodden, Lichtwarck‐Aschoff, & Granic, 2017, for outcomes). The data were collected at Dutch mental health care agencies between January 2012 and January 2014, and results showed that the CBT program was generally effective although outcomes did not differ between conditions (Van Doorn et al., 2017). The most probable explanation for the reason why the CBT condition did not outperform the treatment‐as‐usual condition is that the vast majority of treatment‐as‐usual included elements of CBT.
In the current study, only data of the experimental group were considered to ensure consistency in treatment specific factors (e.g., frequency of sessions, goals and tasks, content, and order of treatment sessions). From January 2015 until November 2015, 10 additional children who were screened for clinical levels of anxiety were included through a follow‐up grant. All these children received the Bögels CBT protocol at one of the three participating mental health care agencies, without random allocation. Children's communication patterns of two sessions were analysed; the first one in which the child was alone (i.e., without parents) with the therapist and a second session in which the exposure phase started. Child reports as well as maternal reports of children's anxiety levels were used to assess treatment outcome.
In order to analyse children's communication patterns, we used the initiative‐response analysis developed by Linell, Gustavsson, and Juvonen (1988). This approach starts with breaking down the dialogue into its most basic units: the interactional turns. Each turn is then qualified as having properties of response, how it is linked to previous turns, and initiative, how it links to next turns. The dynamic and transactive flow of a conversation can then be studied in a chain‐like structure. The advantage of the initiative‐response analysis is that it provides information on the structure of conversational behaviours (e.g., does an individual show rigid and repetitive communication patterns?) as well as the functionality of certain conversational behaviours (e.g., do turns include properties of response and/or initiative?). It hereby allowed us to investigate the (breaking of) rigid and withdrawn communication patterns and the opening up towards more flexible and proactive conversational behaviour that is assumed to be crucial in the treatment process of children with anxiety. Specifically, the following research questions were examined:
-
1
How do communication patterns of children with anxiety look like at the beginning of treatment?
Based on the (observational) literature on interactions of children with anxiety (Barlow, 2002; Lau et al., 2006; Rapee et al., 2009; Strauss et al., 1987), we expected that communication patterns of children would be characterised by high rigidity in terms of withdrawn and inhibited behaviours.
-
2
Are changes in communication patterns associated with treatment outcome?
Based on the adult literature investigating breaking down rigid patterns as a process of therapeutic change (Gumz et al., 2012; Hayes & Strauss, 1998; Hayes & Yasinski, 2015; Hayes et al., 2015; Heinzel et al., 2014; Schiepek et al., 2014;) and the general characterization of children with anxiety by withdrawn, inhibited and restricted ways of being with others, we hypothesised that better treatment outcomes would be associated with the breaking down of rigid communication patterns.
-
3
Is the relation between changes in rigidity of communication patterns and treatment outcome (partially) mediated by increases in more proactive conversational behaviour of the child?
On the basis of studies demonstrating the importance of active child engagement for treatment outcomes (Chu & Kendall, 2004, 2009; Hudson et al., 2014) we predicted that higher levels of response and initiative of the child would partially mediate the relation between changes in rigidity and treatment outcome.
METHOD
Participants
Children
Children for this study were selected by one of two procedures described in more detail in van Doorn et al. (2017). The Screen for Child Anxiety Related Emotional Disorders (SCARED‐NL; Muris, Bodden, Hale, Birmaher, & Mayer, 2007) was used to screen children (either at the participating mental health agencies or schools) for eligibility to participate in the study. Both child self‐reports and maternal reports of children's anxiety levels were used. If the child's or the mother's total SCARED‐NL score or one of the following subscales' scores: generalized anxiety, social anxiety, separation anxiety, or panic disorder, fell in the “high” or “at risk” category, eligibility for participation was further examined by a clinician. Inclusion criteria were an anxiety disorder as defined by the Diagnostic and Statistical Manual of Mental Disorders IV (DSM‐IV; American Psychiatric Association, 2000), and exclusion criteria were a primary diagnosis of posttraumatic stress disorder, autism spectrum disorder, specific phobia, obsessive‐compulsive disorder, an IQ below 80, and the need for immediate intervention to prevent the child or the family from harm (e.g., suicidal intentions). These exclusion criteria were chosen because children meeting these criteria require a different approach than the manualized treatment that was provided in the study.
The pooled sample used in this study included 53 children. The mean age in years was M = 9.68 (SD = 1.85) and 31% were boys. The majority (85%) was of Dutch origin. Most of the children (88%) attended primary school, three children were in secondary school, and three children attended special education (i.e., for children with behavioural and psychiatric problems). Mean age in years of the mothers was M = 43.79 (SD = 5.05). Due to low‐quality audiotapes (n = 7) and drop‐out (n = 13), sample sizes differed per research question. The description of the communication patterns at the beginning of treatment (research question 1) were based on n = 50, and the sample for analyzing the relation between changes in communication patterns and posttreatment anxiety levels (research question 2 and 3) included n = 39 children.
Therapists
Ten therapists, all working at one of three participating mental health care agencies and randomly assigned to the treatment condition, participated in this study. Eight of them were licensed psychologists, and two were mental health workers. The majority of the therapists was female (70%) with a mean age of 51.63 years (SD = 9.38). On average, they had 19.75 years (SD = 7.59) of experience.
Procedure
Written informed consent was obtained from the participating families before random allocation to treatment conditions. At intake and after concluding the treatment, families were asked to fill out the SCARED‐NL. Children were given small gifts for participating in the study, and families received €15 after completing the postassessment. Ethical approval has been granted for the original study of Jansen et al. (2012) by the ethical committee of the Faculty of Social Sciences, Radboud University (ECG16122010).
Children included in the current study all received the manualized CBT Thinking + Doing = Daring developed for children in the age of eight to 18 years (Bögels, 2008). The program has previously shown to be effective in treating anxiety disorders (Bodden et al., 2008) and consists of 12 weekly 1‐hr sessions with the child of which three (at least partly) together with the parents.
Measures
Treatment outcome
To assess treatment outcome, both child and maternal reports of children's anxiety symptoms were used. The child and parent versions of the SCARED‐NL were administered pretreatment and posttreatment. Both versions of SCARED‐NL measure seven anxiety disorders (69 items in total) on a 3‐point scale with response options ranging from 1 (never or almost never) to 3 (often), but from either the child or parent perspective, respectively. The psychometric properties of the SCARED‐NL are good (Hale, Raaijmakers, Muris, & Meeus, 2005; Jansen, Bodden, Muris, Van Doorn, & Granic, 2015; Muris, Dreessen, Bögels, Weckx, & van Melick, 2004). In this study, high internal consistency was confirmed for both the parent (pre: α = .87; post: α = .93) and child (pre: α = .89; post: α = .94) versions. Total scores were calculated by taking the mean of all 69 item scores.
Coding
The first 15 min of the second and fifth therapy sessions were coded starting from when therapist and client were alone in the therapy room and settled to start with the session. Prior to coding, audiotapes were transcribed by master's level social science students. In the coding process verbatims and audiotapes were used in conjunction. To code communication patterns, turns were coded with the response‐initiative system developed by Linell et al. (1988). This system comprises 18 different categories (plus three noncategories: turn miscarriages, back‐channel items, and inaudible turns), each category highlighting a turn's response properties and the (non)presence of initiative. The basic building blocks of the coding system are four symbols that represent initiative and response features of conversational turns. The symbol “<” comprises turns that contain an adequate response to an interlocutor's preceding turn (e.g., the therapist asks a question and the child gives an answer). Symbol “=” also represents responses, but in this case self‐linked responses, so the person is linking up with his/her own preceding turn (e.g., the child continues on a topic). Symbol “>” indicates turns that involve strong initiatives, that is someone is (explicitly) soliciting or demanding a response from the other partner (e.g., asking a question). Last, the symbol “^” represents weak initiatives (e.g., submissively asking). The four symbols and combinations thereof (see Linell et al., 1988, for a complete overview) make‐up the categorical coding system.
Master's level social science students, blind to children's anxiety levels, naïve to study hypotheses, and having received approximately 10 hr of training to attain acceptable inter‐rater agreement, coded the data. During coding, weekly checks were performed to keep agreement high and avoid coder drift. For the second session 20% and for the fifth session 22% were double coded, demonstrating respectively 85% and 90% perfect inter‐rater agreement.
Data analysis
Constructing measures
Coding of each 15‐min segment of the therapist–child conversations resulted in data series of alternating conversational turns by therapist and child. Each data point represents a category that is assigned to a specific turn (e.g., “<>” by the therapist, followed by “<” by the child, etc.). From these interactional data series, child data series were extracted in which only the consecutive turns of the child were preserved.
Next, the distribution of categories (i.e., the Linell codes) per data series was computed, providing information on the functionality of the conversational behaviours that children display. For example, a high density of “<” (i.e., a response from the child to the therapist's preceding turn) may indicate less proactive involvement in the conversation than a high density of “>” (i.e., strong initiative). For each 15‐min segment, percentages of the child's Linell codes were calculated by dividing the frequency of each particular code by the total amount of turns. Simple change scores (e.g., subtracting the value for the later session from that of the earlier session; Rogosa, 1988) were computed in order to allow evaluation of whether intraindividual changes in the functionality of conversational turn‐taking were significant mediators of treatment outcome.
Next, the structure of the child's turn‐taking was analysed using recurrence quantification analysis (RQA). RQA quantifies the complexity of time series and can be used to reveal qualitative changes in the organization of the underlying system (Webber & Zbilut, 1994; applied to categorical data by Dale & Spivey, 2005). Here, we used RQA to quantify the structural rigidity of the child's contribution to the therapist–child conversations.
A key component of RQA is a two‐dimensional graphic visualization of the number and duration of repetitions in the data, a so‐called recurrence plot (RP). Figure 1 displays the recurrence plots of the same child's conversational turns during two sessions, and an additional close‐up that illustrates how the RP is constructed for a short snippet of Linell codes.
Figure 1.
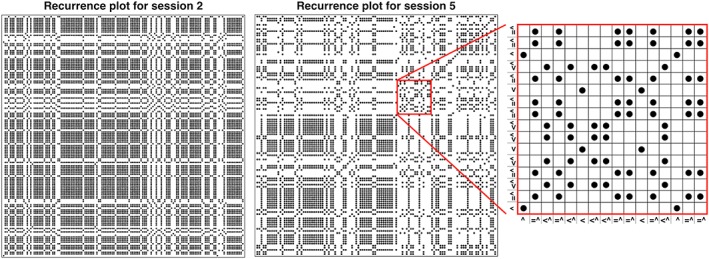
Autorecurrence plots for the same child for sessions two and five (left, middle) and a close‐up from session five (right). [Colour figure can be viewed at http://wileyonlinelibrary.com]
From the RP, several measures can be extracted that quantify the recurrence in the underlying data. The central measure to RQA is the recurrence rate (RR), which is simply the number of points in the RP divided by the squared length of the data series. Here, RR equals the probability that turn taking categories recur over time. In other words, conversational segments characterised by a high RR are highly repetitive in terms of turn‐taking. For example, the RP for session two displayed in Figure 1 has a high RR (RR = .54), which is corroborated by the fact that this particular child used the “<” turn more than 70% of the time. In session five, the child's turn‐taking became much less repetitive, which is indicated by a lower RR (RR = .35).
In addition to the general recurrence of categories, an RP can also contain consecutive repetitions of categories. Looking at the close‐up in Figure 1, it can be seen, for example, that “=^” immediately repeats itself (and again later in time), creating vertical and horizontal lines (because the RP is symmetric around the diagonal, these can be used interchangeably and we refer to both when discussing vertical lines). The percentage of points that form vertical lines is called laminarity (LAM). Here, LAM reflects rigidity of the child's turn‐taking, with high LAM values corresponding to high amounts of consecutive repetitions of the same type of turn‐taking.
The close‐up in Figure 1 shows another type of recurrence. Looking at the sequence “=^, <^,” it can be seen that the entire sequence repeats, creating a diagonal line. The percentage of points in the RP that fall on a diagonal line is called determinism (DET). Here, DET reflects the predictability of the child's turn‐taking behaviour in the conversational segments. High DET values correspond to high amounts of repeating characteristic sequences of turn‐taking.
Together, the three RQA measures described above can be used as a quantification of the amount of rigidity and repetition in the child's communication patterns; high RR, DET, and LAM mean little variation in general and highly repetitive and predictable turn‐taking behaviour in particular. For each child and for each session, RR, DET, and LAM were computed. Next, for each measure and in line with the Linell codes, simple change scores were computed by subtracting the value for the later session from that of the earlier session, to assess whether intraindividual changes in communication patterns were predictive of treatment outcome.
Data inspection
First, all study variables were examined for normality and outliers. No multivariate outliers were detected. Because our sample size is relatively small, using z‐scores for skewness and kurtosis is recommended (Kim, 2013). Following this, preanxiety and postanxiety scores were normally distributed. Most of the RQA measures were within acceptable bounds of normality with the exception of RR being positively skewed at both sessions. For the Linell measures, the relative occurrence (in %) of the codes “<,”“<^,”and “=^” were normally distributed, but relative occurrence of the “<>” code was highly positively skewed. Because of the nonnormal distribution of some of our measures we reran our analyses using a nonparametric approach, that is, bootstrapping (Fox, 2016), to see whether results converged. Results were highly similar, and therefore, only results without bootstrapping are presented.
Second, because children were nested within therapists we tested for mean‐level differences among therapists in all study variables using analyses of variance (ANOVAs) and examined the effects of nesting by looking at the intraclass correlations (ICC's computed using the formula by DeCoster, 2002; Cohen, Cohen, West, & Aiken, 2003). Results of the ANOVAs showed no therapist effects. The mean ICC was .00 with a range of ICCs across study variables between .00 and .11. Again, we reran our analyses including the nesting within therapists to see whether results were similar. Nesting within therapists appeared to not influence the results and results including the nesting are therefore not reported here.
Main analyses
First, descriptive analyses were conducted for all study variables and correlations between study variables were computed. Descriptives were used to answer our first research question concerning the characterization of children's conversational behaviour at the beginning of treatment. Second, to test the hypothesis that treatment outcome was associated with the breaking down of rigid communication patterns by the child, a series of regression analyses were performed with posttreatment anxiety scores as dependent variable, simple change scores of each RQA measure as independent variable, and pretreatment anxiety scores as covariate to control for initial anxiety levels. Two separate sets of analyses were conducted: one using maternal reports of children's anxiety levels and the other using children's own reports of their anxiety. Third, to test the hypothesis that the effect of a decrease in children's conversational rigidity on treatment outcome would be partially explained by increases in proactive engagement of the child in the conversation, mediation analyses were performed, using the PROCESS macro for SPSS (Hayes, 2013). Again, pretreatment anxiety scores were entered as a covariate. Change scores of each of the RQA measures were used as independent variables. The mediator was operationalized in terms of the changes in the “<>” coefficient. This coefficient refers to turns with clear properties of both response and initiative and therefore reflect more proactive engaged conversational behaviours.
RESULTS
Descriptive results
In Table 1 means and standard deviations of anxiety measures, the four most relevant Linell coefficients (e.g., “<” for an adequate response but without initiative, “<^” for linking up to the therapist's turn with weak initiative, “=^” for linking up to the child's own preceding turn with weak initiative, and “<>” for turns with clear properties of both response and initiative), and RQA measures and correlations between them can be found. Note that the n are different at different time points. As one can see in the Table 1, the “<” coefficient was negatively correlated with the other coefficients, except for the “<>” coefficients, at both time points. Over time, coefficients were strongly correlated, except for the “<>” coefficient, indicating relative stability over time. Mothers' reports of children's anxiety at pre were uncorrelated with children's anxiety reports at pre, but post anxiety measures were correlated. Children's anxiety reports did not correlate with any of the other study variables. Maternal reports of children's anxiety at post were correlated with the Linell coefficient “<>” and DET in the later session.
Table 1.
Descriptive statistics and bivariate correlations for all study variables
| Study variable | n | M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 AnxMpre | 53 | 0.61 (0.22) | |||||||||||||||||
| 2 AnxMpost | 40 | 0.44 (0.25) | .56** | ||||||||||||||||
| 3 AnxCpre | 49 | 0.79 (0.25) | .26 | .28 | |||||||||||||||
| 4 AnxCpost | 38 | 0.54 (0.30) | .59** | .46** | .47** | ||||||||||||||
| 5 <coef2 | 50 | .43 (.14) | .19 | ‐.08 | ‐.06 | ‐.10 | |||||||||||||
| 6 <ˆcoef2 | 50 | .35 (.10) | ‐.19 | ‐.05 | .14 | .04 | ‐.68** | ||||||||||||
| 7 =ˆcoef2 | 50 | .14 (.09) | .01 | .02 | .02 | .17 | ‐.43** | ‐.18 | |||||||||||
| 8 <>coef2 | 50 | .01 (.02) | .06 | .12 | .02 | .17 | ‐.22 | .05 | .03 | ||||||||||
| 9 RR2 | 50 | .37 (.08) | .05 | ‐.26 | .05 | ‐.05 | .66** | .09 | ‐.57** | ‐.39** | |||||||||
| 10 DET2 | 50 | .60 (.10) | .16 | ‐.11 | .13 | .12 | .65** | ‐.17 | ‐.32** | ‐.46** | .88** | ||||||||
| 11 LAM2 | 50 | .71 (.11) | .15 | ‐.13 | .02 | .18 | .49** | ‐.06 | ‐.35** | ‐.27 | .75** | .82** | |||||||
| 12 <coef5 | 46 | .39 (.13) | .13 | .12 | .11 | .11 | .70** | ‐.57** | ‐.25 | ‐.10 | .27 | .40** | .19 | ||||||
| 13 <ˆcoef5 | 46 | .37 (.10 | ‐.05 | ‐.21 | ‐.05 | ‐.22 | ‐.18 | .52** | ‐.38** | ‐.02 | .20 | ‐.03 | .09 | ‐.52** | |||||
| 14 =ˆcoef5 | 46 | .15 (.10) | .01 | .19 | ‐.04 | .12 | ‐.51** | .03 | .69** | .04 | ‐.44 | ‐.32** | ‐.27 | ‐.55** | ‐.31* | ||||
| 15 <>coef5 | 46 | .02 (.03) | ‐.11 | ‐.41* | ‐.13 | ‐.18 | ‐.08 | .15 | .03 | .19 | ‐.01 | ‐.11 | ‐.04 | .07 | .04 | ‐.22 | |||
| 16 RR5 | 46 | .35 (.06) | .28 | .31 | .17 | .18 | .47** | ‐.19 | ‐.35* | ‐.21 | .49** | .52** | .39** | .55** | .07 | ‐.43** | ‐.36* | ||
| 17 DET5 | 46 | .57 (.09) | .24 | .42** | .14 | .27 | .40** | ‐.31* | ‐.09 | ‐.26 | .36** | .49** | .32* | .52** | ‐.24 | ‐.11 | ‐.43** | .86** | |
| 18 LAM5 | 46 | .68 (.10) | .04 | .23 | ‐.01 | .19 | .12 | ‐.10 | ‐.06 | ‐.19 | .25 | .31* | .17 | .30* | ‐.17 | ‐.10 | ‐.22 | .62** | .78** |
Note. AnxM: maternal‐reported children's anxiety scores; AnxC: child‐reported anxiety scores; 2 represents second session measures; 5 are fifth session measures; and coef are the coefficients based on the Linell codes.
Correlation is significant at the .01 level.
Correlation is significant at the .05 level.
How do communication patterns of children with anxiety look like at the beginning of treatment?
Children in the second session 15‐min conversation segment had on average 88 turns (SD = 28.90). Children's turns were on average rather brief (M = 2.84 seconds, SD = 4.04), which is corroborated by the nature of their turns. As can be seen in Table 1 children's turns were most often categorized as “<” (e.g., linking to the therapist adjacent turn and involving no initiating properties such as “yes,” “no,” and “don't know”). The second most frequent category was “<^” (e.g., linking up to the therapist's turn with weak initiative such as providing more information). The initiative part of the turn however is weak in a sense that the child does not explicitly solicit or demand a response from the therapist (e.g., the turn does not end with a question). The third most prevalent category was “=^” (e.g., linking to the child's own preceding turn involving only weak initiative such as providing a clarification or expanding on own preceding turn). Only very few turns were coded as “<>,” which are turns with clear properties of both response and initiative (e.g., “yes this is a good idea, should we do it this way?”).
Mean values of children's RR, DET, and LAM further indicated that children were largely repetitive and predictable in their conversational behaviour. The mean values of all RQA measures were relatively high (see Table 1). In particular, LAM was high, which corresponds to high amounts of consecutive repetitions of the same type of turn‐taking. Looking at the means of the Linell coefficients shows that this high recurrence is mainly driven by high percentages of the “<” coefficient, which was significantly positively correlated with all RQA measures of the early session. Given that “<” turns are reactive and lack initiative, this indicates that as expected children's conversational behaviour when entering treatment was characterised by high rigidity in terms of withdrawn and inhibited behaviours.
Are changes in communication patterns associated with treatment outcome?
In Table 2 model results of the regression analyses separately for child and maternal reports of children's anxiety levels and controlling for initial levels of anxiety can be found.
Table 2.
Hierarchical regression analysis predicting postanxiety scores from the differences in RQA measures controlled for anxiety scores at pretest
| Model | Maternal reports | Child reports | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unstandardized estimate | Model statistics | Unstandardized estimate | Model statistics | |||||||||
| B | p value | Δ F | Error df | Δ R 2 | p value | B | p value | ΔF | Error df | ΔR 2 | p value | |
| Anxpre | .68 | <.001 | 17.29 | 38 | .31 | <.001 | .55 | .003 | 10.12 | 36 | .22 | .003 |
| Anxpre | .55 | .001 | 17.17 | 37 | .32 | <.001 | .51 | .005 | 9.09 | 35 | .21 | .005 |
| RR Δ | ‐1.36 | .005 | 8.88 | 36 | .14 | .005 | ‐.68 | .280 | 1.21 | 34 | .03 | .280 |
| Anxpre | .61 | .001 | 17.17 | 37 | .32 | <.001 | .53 | .004 | 9.09 | 35 | .21 | .005 |
| DET Δ | ‐.97 | .001 | 8.95 | 36 | .14 | .005 | ‐.46 | .319 | 1.02 | 34 | .02 | .319 |
| Anxpre | .69 | .001 | 17.17 | 37 | .32 | <.001 | .51 | .005 | 9.09 | 35 | .21 | .005 |
| LAM Δ | ‐.44 | .068 | 3.55 | 36 | .06 | .068 | ‐.09 | .788 | 0.074 | 34 | .00 | .788 |
Note. Anxpre = anxiety scores at pre test, Δ = simple difference score.
Abbreviation: RQA: recurrence quantification analysis.
With respect to maternal reports we found a significant effect of changes in RR, indicating that decreases in the repetitiveness of children's conversational behaviours were associated with better treatment outcomes. Similarly, decreases in DET predicted lower posttreatment anxiety scores, suggesting that reductions in the predictability of children's communication patterns were related to lower anxiety scores posttreatment. Both measures explained 14% of the variance in posttreatment anxiety scores above and beyond initial anxiety levels. Changes in LAM, however, were not significantly associated with lower posttreatment anxiety scores. When using children's reports of their anxiety levels, only the baseline model was significant. None of the RQA measures significantly predicted child‐rated treatment outcome, although estimates were in the same direction as for maternal reports.
Is the relation between changes in rigidity of communication patterns and treatment outcome (partially) mediated by changes towards more proactive conversational behaviour of the child?
After investigating the relation between changes in children's conversational structure and treatment outcomes, we examined whether this relation could be explained by increases in the “<>” coefficient. Because none of the models including child reports of anxiety were significant, mediational analyses were only performed for the maternal reports of children's anxiety. Changes in LAM were unrelated to maternal‐reported treatment outcome; hence, no meditational analyses were performed for changes in LAM.
With respect to changes in RR, results showed that the independent variable (i.e., changes in RR) was significantly related to the mediator (i.e., changes in “<>”; b a = ‐0.211, SE = 0.068, t(36) = ‐3.103, p = .004) such that greater reductions in RR were associated with increases in the “<>” coefficient. The mediator, however, was unrelated to posttreatment anxiety scores (b b = 1.712, SE =1.099, t(35) = 1.558, p = .128). Last, the direct path of changes in RR on posttreatment anxiety levels was significant (b c = ‐1.364, SE = 0.458, t(36) = ‐2.980, p = .005) and dropped in significance when the mediator was included (b c′ = ‐1.002, SE = 0.505, t(36) = ‐1.984, p = .055). This difference between the c and c′ path is reflected in the 95% confidence interval around the indirect effect (b = ‐0.362, SE = 0.321, 95% CI [‐1.2216, 0.0166]), but the indirect effect was not significant.
With respect to changes in DET, results showed a similar pattern. First, changes in DET were significantly related to changes in “<>” (b a = ‐0.128, SE = 0.050, t(36) = ‐2.549, p = .015) such that decreases in DET were associated with increases in the “<>” coefficient. The mediator, however, was not significantly related to posttreatment anxiety scores (b b = 1.829, SE =1.052, t(35) = 1.740, p = .091). Last, the direct path of changes in DET on post anxiety levels was significant (b c = ‐0.971, SE = 0.325, t(36) = ‐2.992, p = .005) and dropped in significance when the mediator was included (b c′ = ‐0.738, SE = 0.343, t(36) = ‐2.149, p = .039). The difference between the c and c′ path can also be seen in the 95% confidence interval around the indirect effect (b = ‐0.233, SE = 0.178, 95% CI [‐0.7080, 0.0170]), but again, the indirect effect was not significant.
DISCUSSION
The general aim of this study was to investigate children's in‐session communication patterns and intraindividual changes herein and examine whether these changes were associated with CBT treatment outcomes in children with anxiety. The finding that the conversational behaviour of these children at the beginning of treatment could be generally described as withdrawn, inhibited, and restricted is not surprising given how children with anxiety tend to behave in novel and challenging situations (Barlow, 2002; Lau et al., 2006; Rapee et al., 2009). Certainly, starting therapy with an unknown therapist is a challenging situation for most children with anxiety. The children who did break this rigid conversational style had better treatment outcomes, but only according to maternal reports of children's anxiety levels. Descriptive results show that maternal and child reports about children's anxiety levels were unrelated at pre and moderately associated at post. This clear discrepancy between informants about the severity of the child's symptoms likely explains the inconsistent findings across reporters around the association between changes in communication patterns and treatment outcome. Informant discrepancies are a robust finding in child treatment studies (Achenbach, 2006; De Los Reyes & Kazdin, 2005). Discrepancies are generally moderate to large and even more pronounced when it comes to internalizing problems like anxiety (Achenbach, 2006). We can only speculate about why changes in children's communication patterns were predictive of maternal but not child reports. It may be that changes in children's communication patterns generalize to the way the child communicates in other settings and with other people. Mothers may also use the child's communication as a window into the child's state of being and picking up changes therein may be reflected in their rating of the child's anxiety levels.
The finding that breaking of rigid communication patterns was associated with maternal rated treatment gains is in line with research that investigated destabilization processes in adult samples (Gumz et al., 2012; Hayes et al., 2015; Hayes & Strauss, 1998; Hayes & Yasinski, 2015; Heinzel et al., 2014; Schiepek et al., 2014). Importantly, our study results suggest that clients' destabilization processes can be detected in the conversations between therapist and client. Thus, given that therapists are aware and able to reflect on the communication structure, this provides them with important information on whether the child is “ready for change.” Such readiness for change is also emphasized in the transtheoretical model of change by Prochaska, DiClemente, and Norcross (1992), and it would be interesting to investigate whether changes in microlevel conversational behaviours signify progression in their stages of change.
Next, beyond examining the structural changes in conversational behaviours, we also looked at the functionality of those behaviours. Based on research about positive involvement shifts (Chu & Kendall, 2004, 2009; Hudson et al., 2014), we expected that increases in more proactive conversational behaviours of the child would explain the positive relation between the breaking of rigid communication patterns and treatment outcome. This hypothesis was only partially supported by our results; changes in conversational structure were related to increases in more proactive behaviour but increases in proactive behaviour were unrelated to treatment outcomes. One explanation may be the small sample size, precluding detection of significant effects. On the other hand, it is also possible that children did not yet fully shift into more active and engaged conversational behaviours. If breaking down rigid patterns is the first and necessary step to discover new ways of being, then the child might need more time (and guidance) to settle into and consolidate new conversational behaviours. A question that is worth investigating.
Strengths, Limitations, and Suggestions for Future Research
A strength of this study is the testing of general processes of change within an evidence‐based protocolized CBT treatment. This way, treatment‐specific factors (e.g., frequency of sessions, goals and tasks, content, and order of treatment sessions) were similar across children, allowing us to look at the unique effect of individual change processes. Further, child reports as well as maternal reports of children's anxiety symptoms were used to assess treatment gains. Additionally, we looked at changes in conversational behaviours over time rather than treating conversation style as a static property. This approach directly followed from our main hypothesis that the breaking of rigid communication patterns was associated with treatment outcome, which in itself is informed by the growing propensity to study therapeutic treatment as a change process (Barlow, Bullis, Comer, & Ametaj, 2013; Harvey, 2004; Hayes et al., 2015; Hershenberg & Goldfried, 2015). This is not simply an alternative viewpoint; there is convincing empirical support that suggests that therapeutic processes are highly dynamic and ignoring this characteristic property may lead to erroneous evaluation of treatment effects (Kowalik, Schiepek, Kumpf, Roberts, & Elbert, 1997; Schiepek et al., 1997; Van de Leemput et al., 2014; Wichers, Groot, Psychosystems, EWS Grp, & ESM Grp, 2016). In this study, changes in children's communication patterns were therefore assessed as change over two time points. Additional time points would have allowed the analysis of a so‐called phase transition profile (e.g., see Lichtwarck‐Aschoff et al., 2012), which follows a specific destabilization and restabilization pattern. Further, it is likely that the timing of destabilization is idiographic, in that it could occur at any time. Additional time points would have allowed us to conduct analyses on an individual level, taking into account the idiosynchratic nature of treatment processes, which eventually is crucial to inform clinical practice (e.g., for an application of client‐focused research see Lutz, 2002; Lutz et al., 2005).
Also, we should keep in mind that this study's results are based on coding the first 15 min of two therapy sessions, starting once therapist and child were settled and ready to start with the session. Coding only segments of a session is in line with observational work in this field (e.g., Chu & Kendall, 2004, 2009), a restriction that is mostly driven by the labour‐intensive nature of coding. Although we do believe that these 15 min gives us a good indication of the child's characteristic way of being with others, whether and how the conversational behaviours changed throughout a session remains unknown. For example, it is possible that children display particularly withdrawn and inhibited conversational behaviour at the beginning of each session and loosen up towards the end, thereby influencing the results. However, if this is indeed the case, then both sessions would be affected and not the change scores between them, which were related to treatment outcome. It would certainly be interesting for future research to investigate both within‐ and between‐session changes in communication patterns for time effects and test the relation with treatment outcome.
A related limitation of this study concerns the fact that only the child part of the children–therapist interactions was included in the analysis. The changes in rigidity predictive of better treatment outcomes may not only occur within the children's conversational behaviour; the way therapists organize their contribution to the conversation may be equally important, especially because they take the majority of initiative. In fact, rigid communication patterns by the child may be complemented by equal levels of rigidity of the therapist, albeit of a different nature. For example, therapists may find themselves caught in a repetitive pattern of initiative taking in an attempt to break through the withdrawn and inhibited conversational behaviour of the child. Creed and Kendall (2005) have identified “pushing the child to talk” as specific therapist behaviour that negatively impacts child‐rated alliance. We suspect that this particular strategy manifests itself in specific therapist turns, turns with strong initiative that demand a response of the child. Investigating communication patterns on a microlevel as has been done in the current study adds a more in‐depth layer to these more “global” measures of therapist behaviours. Moreover, identifying the transactional microdynamics between therapist and child may aid in creating awareness among therapists about their own contribution to conversational rigidity and the importance of breaking these patterns. Existing work on therapist behaviours such as alliance building (Creed & Kendall, 2005) and therapist flexibility (e.g., Chu & Kendall, 2009; Hudson et al., 2014) should be complemented by future investigations of whether an equal and more conscious breaking of rigidity of conversational behaviour by the therapist may elicit or speed up that of the child.
Another limitation of this study was our relative small sample, which did not permit more sophisticated analyses, nor to include more predictors and investigate their effect simultaneously. It would be interesting to include other process variables such as child engagement, therapist behaviours, or alliance. For example, a positive alliance is known to positively impact CBT outcomes for children (McLeod, 2011). In the context of breaking rigid (communication) patterns it may be that a positive alliance creates the necessary boundary conditions facilitating the reorganization into more flexible behaviour (Haken & Schiepek, 2006). Support for this has been found in a study by Schiepek et al. (2014) in which clients that experienced both a process of destabilization and a positive alliance had the best treatment outcomes.
In addition, diagnostic assessment of DSM‐IV diagnoses was conducted by agency clinicians who followed their agency's usual practice and not through standardized diagnostic interviews. As a result, the evaluation of treatment efficacy in the original study as well as the outcome variables used in the current study are based on the same instrument that was used for screening (i.e., SCARED‐NL; Muris et al., 2007). Hence, it was not possible to look at diagnostic outcomes and whether these were associated with changes in communication patterns. Relatedly, not having a standardized diagnostic procedure precluded us from looking at specific subtypes of anxiety disorders. It might be that conversational structures are different in for instance children with social anxiety compared with children with generalized anxiety. This should be part of a larger follow‐up study. Also, we do not know whether our findings would generalize across diagnostic categories (e.g., children with conduct problems) or different treatment orientations (e.g., psychodynamic therapies). Based on the fact that the process of breaking down rigid patterns has been found conducive for depressed individuals (Hayes et al., 2015; Hayes & Strauss, 1998), personality disorders (Hayes & Yasinski, 2015), and childhood aggression (Lichtwarck‐Aschoff et al., 2012), we are confident that the general process of breaking down rigid (communication) patterns would hold. Some of the specific patterns, however, such as the breaking of withdrawn and inhibited behaviours towards more active engagement, might very well be specific to children with anxiety.
GENERAL CONCLUSION
In sum, this study provides initial support for the hypothesis that the breaking of rigid and inhibited communication patterns may be a relevant change process in the field of CBT anxiety treatment for children, which warrants further investigation. The current study complements existing work on processes of change in the childhood treatment literature and contributes to the movement in the psychotherapy field to identify general—transtheoretical and transdiagnostic—processes underlying psychopathology and clinical change (e.g., see Barlow et al., 2013; Harvey, 2004; Hershenberg & Goldfried, 2015). Taking into consideration a client's process of change, including the process of breaking rigid patterns, may ultimately allow us to tailor specific treatment elements to the current state that the client is in, which should significantly push the effectiveness of existing (CBT) interventions.
CONFLICT OF INTEREST STATEMENT
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this manuscript.
Lichtwarck‐Aschoff A, van Rooij MMJW. Are changes in children's communication patterns predictive of treatment outcomes for children with anxiety?. Clin Psychol Psychother. 2019;26:572–585. 10.1002/cpp.2383
Author Note
This research was supported by a grant from the Netherlands Organisation for Health Research and Development (ZonMw 70‐72900‐98‐14015).
REFERENCES
- Achenbach, T. M. (2006). As others see us: Clinical and research implications of cross‐informant correlations for psychopathology. Current Directions in Psychological Science, 15, 94–98. 10.1111/j.0963-7214.2006.00414.x [DOI] [Google Scholar]
- American Psychiatric Association . (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: Author. [Google Scholar]
- Bakhtin, M. M. (1984). Problems of Dostoevsky's poetics. Minneapolis: University of Minnesota Press. [Google Scholar]
- Barlow, D. H. (2002). Anxiety and its disorders: The nature and treatment of anxiety and panic (2nd ed.). New York: The Guilford Press. [Google Scholar]
- Barlow, D. H. , Bullis, J. R. , Comer, J. S. , & Ametaj, A. A. (2013). Evidence‐based psychological treatments: An update and a way forward In Nolen‐Hoeksema S., Cannon T. D., & Widiger T. (Eds.), Annual Review of Clinical Psychology (Vol. 9) (pp. 1–27). Palo Alto, CA: Annual Reviews. [DOI] [PubMed] [Google Scholar]
- Bodden, D. H. , Bögels, S. M. , Nauta, M. H. , De Haan, E. , Ringrose, J. , Appelboom, C. , … Appelboom‐Geerts, K. C. M. M. J. (2008). Child versus family cognitive behavioral therapy in clinically anxious youth: An efficacy and partial effectiveness study. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 1384–1394. 10.1097/CHI.0b013e318189148e [DOI] [PubMed] [Google Scholar]
- Bögels, S. M. (2008). Behandeling van angststoornissen bij kinderen en adolescenten. Met het cognitief‐gederagstherapeutisch protocol Denken + Doen = Durven. Houten: Bohn Stafleu van Loghum. [Google Scholar]
- Bonanno, G. A. , & Burton, C. L. (2013). Regulatory flexibility. Perspectives on Psychological Science, 8, 591–612. 10.1177/1745691613504116 [DOI] [PubMed] [Google Scholar]
- Carey, T. A. (2011). Exposure and reorganization: The what and how of effective psychotherapy. Clinical Psychology Review, 31, 236–248. 10.1016/j.cpr.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Cartwright‐Hatton, S. , Roberts, C. , Chitsabesan, P. , Fothergill, C. , & Harrington, R. (2004). Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. British Journal of Clinical Psychology, 43, 421–436. 10.1348/0144665042388928 [DOI] [PubMed] [Google Scholar]
- Chiu, A. W. , McLeod, B. D. , Har, K. , & Wood, J. J. (2009). Child–therapist alliance and clinical outcomes in cognitive behavioral therapy for child anxiety disorders. Journal of Child Psychology and Psychiatry, 50, 751–758. 10.1111/j.1469-7610.2008.01996.x [DOI] [PubMed] [Google Scholar]
- Chu, B. C. , & Kendall, P. C. (2004). Positive association of child involvement and treatment outcome within a manual‐based cognitive‐behavioral treatment for children with anxiety. Journal of Consulting and Clinical Psychology, 72, 821–829. 10.1037/0022-006X.72.5.821 [DOI] [PubMed] [Google Scholar]
- Chu, B. C. , & Kendall, P. C. (2009). Therapist responsiveness to child engagement: Flexibility within manual‐based CBT for anxious youth. Journal of Clinical Psychology, 65, 736–754. 10.1002/jclp.20582 [DOI] [PubMed] [Google Scholar]
- Cohen, J. , Cohen, P. , West, S. G. , & Aiken, L. S. (2003). Applied multiple correlation/regression analysis for the behavioral sciences. UK: Taylor & Francis. [Google Scholar]
- Compton, S. N. , March, J. S. , Brent, D. , Albano, A. M. , Weersing, V. R. , & Curry, J. (2004). Cognitive‐behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence‐based medicine review. Journal of the American Academy of Child & Adolescent Psychiatry, 43, 930–959. 10.1097/01.chi.0000127589.57468.bf [DOI] [PubMed] [Google Scholar]
- Creed, T. A. , & Kendall, P. C. (2005). Therapist alliance‐building behavior within a cognitive‐behavioral treatment for anxiety in youth. Journal of Consulting and Clinical Psychology, 73, 498–505. 10.1037/0022-006X.73.3.498 [DOI] [PubMed] [Google Scholar]
- Dale, R. , & Spivey, M. J. (2005). Categorical recurrence analysis of child language In Proceedings of the 27th annual meeting of the cognitive science society (pp. 530–535). Mahwah, NJ: Lawrence Erlbaum. [Google Scholar]
- De Los Reyes, A. , & Kazdin, A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131, 483–509. 10.1037/0033-2909.131.4.483 [DOI] [PubMed] [Google Scholar]
- DeCoster, J. (2002). Using ANOVA to examine data from groups and dyads. Retrieved March, 28, 2011.
- Fisak, B. J. Jr. , Richard, D. , & Mann, A. (2011). The prevention of child and adolescent anxiety: A meta‐analytic review. Prevention Science, 12, 255–268. 10.1007/s11121-011-0210-0 [DOI] [PubMed] [Google Scholar]
- Fjermestad, K. W. , Mowatt Haugland, B. S. , Heiervang, E. , & Öst, L. G. (2009). Relationship factors and outcome in child anxiety treatment studies. Clinical Child Psychology and Psychiatry, 14, 195–214. 10.1177/1359104508100885 [DOI] [PubMed] [Google Scholar]
- Fox, J. (2016). Applied regression analysis and generalized linear models. Thousand Oaks, California: Sage Publications Inc. [Google Scholar]
- Gumz, A. , Bauer, K. , & Brähler, E. (2012). Corresponding instability of patient and therapist process ratings in psychodynamic psychotherapies. Psychotherapy Research, 22, 26–39. 10.1080/10503307.2011.622313 [DOI] [PubMed] [Google Scholar]
- Haken, H. , & Schiepek, G. (2006). Synergetik in der Psychologie: Selbstorganisation verstehen und gestalten. Göttingen: Hogrefe. [Google Scholar]
- Hale, W. W. , Raaijmakers, Q. , Muris, P. , & Meeus, W. (2005). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED) in the general adolescent population. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 283–290. 10.1097/00004583-200503000-00013 [DOI] [PubMed] [Google Scholar]
- Harvey, A. G. (2004). Cognitive behavioural processes across psychological disorders: A transdiagnostic approach to research and treatment. USA: Oxford University Press. [Google Scholar]
- Hayes, A. F. (2013). PROCESS SPSS Macro [Computer software and manual].
- Hayes, A. M. , & Strauss, J. L. (1998). Dynamic systems theory as a paradigm for the study of change in psychotherapy: An application to cognitive therapy for depression. Journal of Consulting and Clinical Psychology, 66, 939–947. 10.1037/0022-006X.66.6.939 [DOI] [PubMed] [Google Scholar]
- Hayes, A. M. , & Yasinski, C. (2015). Pattern destabilization and emotional processing in cognitive therapy for personality disorders. Frontiers in Psychology, 6, 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, A. M. , Yasinski, C. , Barnes, J. B. , & Bockting, C. L. (2015). Network destabilization and transition in depression: New methods for studying the dynamics of therapeutic change. Clinical Psychology Review, 41, 27–39. 10.1016/j.cpr.2015.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinzel, S. , Tominschek, I. , & Schiepek, G. (2014). Dynamic patterns in psychotherapy—Discontinuous changes and critical instabilities during the treatment of obsessive compulsive disorder. Nonlinear Dynamics, Psychology, and Life Sciences, 18, 155–176. [PubMed] [Google Scholar]
- Hershenberg, R. , & Goldfried, M. R. (2015). Implications of RDoC for the research and practice of psychotherapy. Behavior Therapy, 46, 156–165. 10.1016/j.beth.2014.09.014 [DOI] [PubMed] [Google Scholar]
- Higa‐McMillan, C. K. , Francis, S. E. , Rith‐Najarian, L. , & Chorpita, B. F. (2016). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child & Adolescent Psychology, 45, 91–113. 10.1080/15374416.2015.1046177 [DOI] [PubMed] [Google Scholar]
- Hudson, J. L. , Kendall, P. C. , Chu, B. C. , Gosch, E. , Martin, E. , Taylor, A. , & Knight, A. (2014). Child involvement, alliance, and therapist flexibility: Process variables in cognitive‐behavioural therapy for anxiety disorders in childhood. Behaviour Research and Therapy, 52, 1–8. 10.1016/j.brat.2013.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James, A. C. , James, G. , Cowdrey, F. A. , Soler, A. , & Choke, A. (2015). Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database of Systematic Reviews, (2), CD004690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen, M. , Bodden, D.H. , Muris, P. , Van Doorn, M.M. , & Granic, I. (2015). Reliability and validity of the Screen for Child Anxiety‐Related Emotional Disorders‐Parent version: The importance of separate mother and father reports. Manuscript submitted for publication.
- Jansen, M. , Van Doorn, M. M. , Lichtwarck‐Aschoff, A. , Kuijpers, R. C. , Theunissen, H. , Korte, M. , … Granic, I. (2012). Effectiveness of a cognitive‐behavioral therapy (CBT) manualized program for clinically anxious children: Study protocol of a randomized controlled trial. BMC Psychiatry, 12, 16 10.1186/1471-244X-12-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnsen, T. J. , & Friborg, O. (2015). The effects of cognitive behavioral therapy as an anti‐depressive treatment is falling: A meta‐analysis. Psychological Bulletin, 141, 747–768. 10.1037/bul0000015 [DOI] [PubMed] [Google Scholar]
- Karver, M. S. , De Nadai, A. S. , Monahan, M. , & Shirk, S. R. (2018). Meta‐analysis of the prospective relation between alliance and outcome in child and adolescent psychotherapy. Psychotherapy, 55, 341–355. 10.1037/pst0000176 [DOI] [PubMed] [Google Scholar]
- Karver, M. S. , Handelsman, J. B. , Fields, S. , & Bickman, L. (2006). Meta‐analysis of therapeutic relationship variables in youth and family therapy: The evidence for different relationship variables in the child and adolescent treatment outcome literature. Clinical Psychology Review, 26, 50–65. 10.1016/j.cpr.2005.09.001 [DOI] [PubMed] [Google Scholar]
- Kashdan, T. B. (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30, 865–878. 10.1016/j.cpr.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin, A. E. (2007). Mediators and mechanisms of change in psychotherapy research. The Annual Review of Clinical Psychology, 3, 1–27. 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- Kazdin, A. E. (2009). Understanding how and why psychotherapy leads to change. Psychotherapy Research, 19, 418–428. 10.1080/10503300802448899 [DOI] [PubMed] [Google Scholar]
- Kazdin, A. E. , & Nock, M. K. (2003). Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, 44, 1116–1129. 10.1111/1469-7610.00195 [DOI] [PubMed] [Google Scholar]
- Kim, H. Y. (2013). Statistical notes for clinical researchers: Assessing normal distribution using skewness and kurtosis. Restorative Dentistry & Endodontics, 38, 52–54. 10.5395/rde.2013.38.1.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalik, Z. , Schiepek, G. , Kumpf, K. , Roberts, L. , & Elbert, T. (1997). Psychotherapy as a chaotic process II. The application of nonlinear analysis methods on quasi time series of the client‐therapist interaction: A nonstationary approach. Psychotherapy Research, 7, 197–218. 10.1080/10503309712331331973 [DOI] [Google Scholar]
- Lau, J. Y. , Eley, T. C. , & Stevenson, J. (2006). Examining the state‐trait anxiety relationship: A behavioural genetic approach. Journal of Abnormal Child Psychology, 34, 19–27. 10.1007/s10802-005-9006-7 [DOI] [PubMed] [Google Scholar]
- Liber, J. M. , McLeod, B. D. , Van Widenfelt, B. M. , Goedhart, A. W. , van der Leeden, A. J. , Utens, E. M. , & Treffers, P. D. (2010). Examining the relation between the therapeutic alliance, treatment adherence, and outcome of cognitive behavioral therapy for children with anxiety disorders. Behavior Therapy, 41, 172–186. 10.1016/j.beth.2009.02.003 [DOI] [PubMed] [Google Scholar]
- Lichtwarck‐Aschoff, A. , Hasselman, F. , Cox, R. , Pepler, D. , & Granic, I. (2012). A characteristic destabilization profile in parent‐child interactions associated with treatment efficacy for aggressive children. Nonlinear Dynamics, Psychology, and Life Sciences, 16, 353–379. [PubMed] [Google Scholar]
- Linell, P. , Gustavsson, L. , & Juvonen, P. (1988). Interactional dominance in dyadic communication: A presentation of initiative‐response analysis. Linguistics, 26, 415–442. [Google Scholar]
- Lutz, W. (2002). Patient‐focused psychotherapy research and individual treatment progress as scientific groundwork for an empirically based clinical practice. Psychotherapy Research, 12, 251–272. 10.1080/713664389 [DOI] [Google Scholar]
- Lutz, W. , Leach, C. , Barkham, M. , Lucock, M. , Stiles, W. B. , Evans, C. , … Iveson, S. (2005). Predicting change for individual psychotherapy clients on the basis of their nearest neighbors. Journal of Consulting and Clinical Psychology, 73, 904–913. 10.1037/0022-006X.73.5.904 [DOI] [PubMed] [Google Scholar]
- Lyons‐Ruth, K. (1999). The two‐person unconscious: Intersubjective dialogue, enactive relational representation, and the emergence of new forms of relational organization. Psychoanalytic Inquiry, 19, 576–617. 10.1080/07351699909534267 [DOI] [Google Scholar]
- Mahoney, M. J. (1991). Human change processes: The scientific foundations of psychotherapy. New York: Basic Books. [Google Scholar]
- McLeod, B. D. (2011). Relation of the alliance with outcomes in youth psychotherapy: A meta‐analysis. Clinical Psychology Review, 31, 603–616. 10.1016/j.cpr.2011.02.001 [DOI] [PubMed] [Google Scholar]
- McLeod, B. D. , Islam, N. Y. , Chiu, A. W. , Smith, M. M. , Chu, B. C. , & Wood, J. J. (2014). The relationship between alliance and client involvement in CBT for child anxiety disorders. Journal of Clinical Child & Adolescent Psychology, 43, 735–741. 10.1080/15374416.2013.850699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moses, E. B. , & Barlow, D. H. (2006). A new unified treatment approach for emotional disorders based on emotion science. Current Directions in Psychological Science, 15, 146–150. 10.1111/j.0963-7214.2006.00425.x [DOI] [Google Scholar]
- Moyers, T. B. , & Martin, T. (2006). Therapist influence on client language during motivational interviewing sessions. Journal of Substance Abuse Treatment, 30, 245–251. 10.1016/j.jsat.2005.12.003 [DOI] [PubMed] [Google Scholar]
- Moyers, T. B. , Martin, T. , Houck, J. M. , Christopher, P. J. , & Tonigan, J. S. (2009). From in‐session behaviors to drinking outcomes: A causal chain for motivational interviewing. Journal of Consulting and Clinical Psychology, 77, 1113–1124. 10.1037/a0017189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris, P. , Bodden, D. , Hale, W. W. , Birmaher, B. , & Mayer, B. (2007). SCARED NL: Vragenlijst over angst en bang‐zijn bij kinderen en adolescenten. Amsterdam: Boom test uitgevers. [Google Scholar]
- Muris, P. , Dreessen, L. , Bögels, S. , Weckx, M. , & van Melick, M. (2004). A questionnaire for screening a broad range of DSM‐defined anxiety disorder symptoms in clinically referred children and adolescents. Journal of Child Psychology and Psychiatry, 45, 813–820. 10.1111/j.1469-7610.2004.00274.x [DOI] [PubMed] [Google Scholar]
- Mychailyszyn, M. P. , Brodman, D. M. , Read, K. L. , & Kendall, P. C. (2012). Cognitive‐behavioral school‐based interventions for anxious and depressed youth: a meta‐analysis of outcomes. Clinical Psychology: Science and Practice, 19, 129–153. [Google Scholar]
- Norcross, J. C. , & Wampold, B. E. (2011). What works for whom: Tailoring psychotherapy to the person. Journal of Clinical Psychology, 67, 127–132. 10.1002/jclp.20764 [DOI] [PubMed] [Google Scholar]
- Öst, L. G. (2008). Efficacy of the third wave of behavioral therapies: A systematic review and meta‐analysis. Behaviour Research and Therapy, 46, 296–321. 10.1016/j.brat.2007.12.005 [DOI] [PubMed] [Google Scholar]
- Pachankis, J. E. , & Goldfried, M. R. (2007). On the next generation of process research. Clinical Psychology Review, 27, 760–768. 10.1016/j.cpr.2007.01.009 [DOI] [PubMed] [Google Scholar]
- Prochaska, J. O. , DiClemente, C. C. , & Norcross, J. C. (1992). In search of the structure of change In Self change (pp. 87–114). New York: Springer; 10.1007/978-1-4612-2922-3_5 [DOI] [Google Scholar]
- Rapee, R. M. , Schniering, C. A. , & Hudson, J. L. (2009). Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology, 5, 311–341. 10.1146/annurev.clinpsy.032408.153628 [DOI] [PubMed] [Google Scholar]
- Rogosa, D. R. (1988). Myths about longitudinal research In Schaie K. W., Campbell R. T., Meredith W., & Rawlings S. C. (Eds.), Methodological issues in aging research (pp. 171–210). New York: Springer Publishing Company. [Google Scholar]
- Rosen, G. M. , & Davison, G. C. (2003). Psychology should list empirically supported principles of change (ESPs) and not credential trademarked therapies or other treatment packages. Behavior Modification, 27, 300–312. 10.1177/0145445503027003003 [DOI] [PubMed] [Google Scholar]
- Ruiz‐Sancho, E. M. , Frojan‐Parga, M. X. , & Calero‐Elvira, A. (2013). Functional analysis of the verbal interaction between psychologist and client during the therapeutic process. Behavior Modification, 37, 516–542. 10.1177/0145445513477127 [DOI] [PubMed] [Google Scholar]
- Schiepek, G. (2009). Complexity and nonlinear dynamics in psychotherapy. European Review, 17, 331–356. 10.1017/S1062798709000763 [DOI] [Google Scholar]
- Schiepek, G. , Kowalik, Z. , Schütz, A. , Köhler, M. , Richter, K. , Strunk, G. , … Elbert, T. (1997). Psychotherapy as a chaotic process I. Coding the client‐therapist interaction by means of Sequential Plan Analysis and the search for chaos: a stationary approach. Psychotherapy Research, 7, 173–194. 10.1080/10503309712331331953 [DOI] [Google Scholar]
- Schiepek, G. K. , Tominschek, I. , & Heinzel, S. (2014). Self‐organization in psychotherapy: testing the synergetic model of change processes. Frontiers in Psychology, 5, 1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider, B. H. (2009). An observational study of the interactions of socially withdrawn/anxious early adolescents and their friends. Journal of Child Psychology and Psychiatry, 50, 799–806. 10.1111/j.1469-7610.2008.02056.x [DOI] [PubMed] [Google Scholar]
- Shirk, S. R. , & Karver, M. (2003). Prediction of treatment outcome from relationship variables in child and adolescent therapy: A meta‐analytic review. Journal of Consulting and Clinical Psychology, 71, 452–464. 10.1037/0022-006X.71.3.452 [DOI] [PubMed] [Google Scholar]
- Shirk, S. R. , Karver, M. S. , & Brown, R. (2011). The alliance in child and adolescent psychotherapy. Psychotherapy, 48, 17–24. 10.1037/a0022181 [DOI] [PubMed] [Google Scholar]
- Shotter, J. (1997). The Social construction of our inner selves. Journal of Constructivist Psychology, 10, 7–24. 10.1080/10720539708404609 [DOI] [Google Scholar]
- Silverman, W. K. , Pina, A. A. , & Viswesvaran, C. (2008). Evidence‐based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology, 37, 105–130. 10.1080/15374410701817907 [DOI] [PubMed] [Google Scholar]
- Sparks, J. , Duncan, B. L. , & Miller, S. D. (2007). Common factors and the uncommon heroism of youth. Psychotherapy in Australia, 13, 34–43. [Google Scholar]
- Strauss, C. C. , Frame, C. L. , & Forehand, R. (1987). Psychosocial impairment associated with anxiety in children. Journal of Clinical Child Psychology, 16, 235–239. 10.1207/s15374424jccp1603_8 [DOI] [Google Scholar]
- Tomicic, A. , Martinez, C. , & Krause, M. (2015). The sound of change: A study of the psychotherapeutic process embodied in vocal expression. Laura Rice's ideas revisited. Psychotherapy Research, 25, 263–276. 10.1080/10503307.2014.892647 [DOI] [PubMed] [Google Scholar]
- Van de Leemput, I. A. , Wichers, M. , Cramer, A. O. , Borsboom, D. , Tuerlinckx, F. , Kuppens, P. , … Scheffer, M. (2014). Critical slowing down as early warning for the onset and termination of depression. Proceedings of the National Academy of Sciences, 111, 87–92. 10.1073/pnas.1312114110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doorn, M. E. M. , Jansen, M. , Bodden, D. H. M. , Lichtwarck‐Aschoff, A. , & Granic, I. (2017). A randomized controlled effectiveness study comparing manualized cognitive behavioral therapy (CBT) with treatment‐as‐usual for clinically anxious children. Journal of Clinical Trials, 7, 330. [Google Scholar]
- Volosinov, V. N. (1973). Marxism and the philosophy of language. Cambridge, Mass: Harvard University Press. [Google Scholar]
- Wachtel, P. L. (2011). Therapeutic communication: Knowing what to say when (2nd ed.). New York: Guilford. [Google Scholar]
- Webber, C. L. , & Zbilut, J. P. (1994). Dynamical assessment of physiological systems and states using recurrence plot strategies. Journal of Applied Physiology, 76, 965–973. 10.1152/jappl.1994.76.2.965 [DOI] [PubMed] [Google Scholar]
- Weisz, J. R. , Kuppens, S. , Ng, M. Y. , Eckshtain, D. , Ugueto, A. M. , Vaughn‐Coaxum, R. , … Weersing, V. R. (2017). What five decades of research tells us about the effects of youth psychological therapy: A multilevel meta‐analysis and implications for science and practice. American Psychologist, 72, 79–117. 10.1037/a0040360 [DOI] [PubMed] [Google Scholar]
- Wichers, M. , Groot, P. C. , Psychosystems, ESM Grp , & EWS Grp (2016). Critical slowing down as a personalized early warning signal for depression. Psychotherapy and Psychosomatics, 85, 114–116. 10.1159/000441458 [DOI] [PubMed] [Google Scholar]


