Abstract
Nonspecific, functional, and somatoform (NFS) syndromes is an umbrella term for various diagnoses with medically unexplained symptoms. These syndromes are more prevalent among women than among men, and associated with negative preconceptions that can impede rehabilitation. In two studies, we quantitatively assess how patients’ gender affects the diagnostic assessment of NFS syndromes, as well as the healthcare experiences of individuals diagnosed with NFS syndromes. In the first study, our vignette‐based experiment showed that Swedish general practitioners (N = 90) were gender biased in their diagnostic assessment of NFS syndromes, such that a female patient with back pain was more likely to be assigned a NFS syndrome compared to an otherwise identical male patient. In the second study, a large community sample of Swedish individuals with medically explained (n = 432) and unexplained pain (n = 521) evaluated their treating physician's relational conduct. Even after accounting for a variety of sociodemographic variables and other pain characteristics, women with at least one NFS syndrome percieved their physician's relational conduct as significantly poorer than other women as well as men with and without NFS syndromes. When women's pain is more likely than men's to be assessed as NFS, their rehabilitation could be prolonged as pertient alternative diagnoses and treatments are omittied and their negative healthcare experiences lower their volition to partake and persevere in treatment.
Keywords: Functional disorder, gender bias, MUS, primary care, relational conduct, somatoform disorder
Introduction
Prevalence studies have estimated that between 16%–30% of the Scandinavian population suffer from various chronic pain conditions (Breivik, Collett, Ventafridda, Cohen & Gallacher, 2006; Harker, Reid, Bekkering et al., 2012; Rustøen, Wahl, Hanestad et al., 2004), the majority of whom are women (Gerdle, Björk, Henriksson & Bengtsson, 2004). More women than men also suffer from pain symptomology not attributable to any organic cause (Schaefert, Hausteiner‐Wiehle, Häuser et al., 2012), also known as medically unexplained or nonspecific, functional, and somatoform (NFS) symptoms. As what symptoms are considered medically unexplained or NFS changes with advances in medical science, their operationalization differs between diagnostic manuals and their editions. Within Swedish primary care, diagnostic assessment is made according to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems ([ICD‐10], Socialstyrelsen, 2016), and therein NFS symptoms are classified under different diagnoses such as irritable bowel syndrome (IBS), fibromyalgia, chronic fatigue syndrome (ME/CFS), and tension headache (Wessely, Nimnuan & Sharpe, 1999). The purpose of the present article is to explore two aspects of how gender influence the assessment as well as the management of patients with NFS syndromes within primary care. The aim of the first study was to explore if general practitioners are gender biased in their diagnostic assessment of back pain, such that women's pain is more often assessed as NFS compared to men's. In the second study, we utilized a community sample to investigate if gender interacts with NFS syndromes to explain patients’ healthcare experiences. By studying these associations between gender and NFS syndromes, we aim to expand our current understanding of how assessment and ongoing management of medically unexplained pain within primary care is associated to the increased prevalence among women as compared to men.
Study 1
Women are clinically diagnosed with NFS syndromes up to three times as often as men (Schaefert et al., 2012), which could be due to a combination of sex‐ and gender‐related biological and psychosocial factors. For example, these could include differing hormonal levels that in turn affect pain modulation, and that women and men cope differently with stress (Fillingim, King, Ribeiro‐Dasilva, Rahim‐Williams & Riley, 2009). However, there is also the possibility of gender bias in the diagnostic process, such that similar symptoms are assessed as medically explained or unexplained depending on the patient's gender (Risberg, Johansson & Hamberg, 2009). This bias may ensue due to gender stereotypes, which are cognitive representations of what is considered typical for women and men (Ridgeway, 2009; Wood & Eagly, 2010). For example, as somatization is generally considered part of the clinical picture in NFS syndromes (Schaefert et al., 2012), and Tait, Chibnall and Kalauokalani (2009) found that women are believed to somatize their symptoms to a larger extent than men, physicians might be more likely to assess the pain of a female patient as NFS when compared to a male patient. This was the case in an experimental study by Hamberg, Risberg, Johansson and Westman (2002). By utilizing vignettes, they found that Swedish junior physicians (corresponding to UK preregistration house officers and US interns) were more likely to classify neck pain in a female patient as NFS when compared to an otherwise identical male patient. It is, however, still unknown if this bias is prevalent in certified medical professionals such as general practitioners. This is highly relevant, as patients with pain often are initially assessed within primary care and this early assessment might affect the remaining course of management (Fink & Rosendal, 2008; Reid, Whooley, Crayford & Hotopf, 2001).
Therefore, in our first study, we used an experimental design with vignettes to study if patients’ gender influenced whether general practitioners classified the pain as NFS or not. As Swedish junior physicians display gender bias when diagnosing NFS syndromes (Hamberg et al., 2002), we likewise hypothesized that certified general practitioners would assign the female patient an NFS diagnosis significantly more often than the male patient, even after accounting for the practitioner's experience, age, and own gender.
Method
Participants
The sample comprised 90 general practitioners (M age = 49.40, SD = 11.28), including 59% men, 40% women, and 1% who did not disclose their gender. On average, the participants had 20.30 years (SD = 11.15) of working experience.
Design
The study was a two‐factor between‐subjects design, where patient gender was manipulated between conditions. Patient gender was indicated by the first name and pronouns used in the patient description. We used three traditional Swedish names for each gender (female names: Anna, Linda, Maria; male names: Fredrik, Johan, Mikael), and these were randomized between participants. This was to ascertain that the name itself would not affect the diagnostic assessment of NFS syndromes, which was confirmed (female names: χ2(2) = 2.75, p = 0.25, male names: χ2(2) = 4.10, p = 0.13).
Materials: Patient description
The description detailed a 40‐year‐old patient with symptoms of low back pain. From an acute onset due to heavy carrying, the pain was described as gradually worsening over the past 6 months in terms of intensity and proliferation to other areas of the back and the legs. The current pain had a significant negative impact on the patient's day‐to‐day life; such as their ability to perform household work, ability to care for their family (spouse, and two children below 10 years of age), and their overall mood and quality of sleep. The patient had previously consulted a chiropractor and a physiotherapist, and been on full‐time sick‐leave for a month from their work as a bank official, but perceived that neither had alleviated their pain.
Materials: Most probable diagnosis/es
Participants were asked to indicate which diagnosis or diagnoses they considered as the most probable prior to further investigations. Answers were given in free text format, and coded according to ICD‐10 (World Health Organization, [WHO], 2016) by two independent coders. Any discrepancies between the coders were discussed until resolved. Based on a comprehensive list of NFS syndromes provided in Schaefert et al. (2012), answers were subsequently coded as NFS if the participant had provided at least one of the following diagnoses: unspecified back pain, myalgia, fibromyalgia, or unspecified pain.
Procedure
The majority of the participants in the current study were recruited from two health corporations, which distributed the online survey among its currently employed members. Sixty‐eight participants were recruited by this method. Additional participants (n = 22) were recruited through dedicated social media forums. Participants were initially briefed that the survey would entail making a medical assessment, but not about the characteristics of the symptoms or that the patient might be either a woman or a man. They were also informed about the estimated duration of the task, and their right to discontinue at any given moment. After providing written informed consent, participants were randomized by a computer algorithm to read the description of either a female or a male patient, whereupon they answered the questionnaire. Completion of the survey was reimbursed with a lottery ticket.
Statistical analyses
Initial analyses were conducted to check attrition and equivalence between participants depending on recruitment strategy. We observed two cases of missing data; one participant who did not disclose their working experience, and another who did not disclose their gender. These were removed case‐by‐case in the descriptive analyses. However, to maximize the available amount of cases prior to regression modeling, we imputed the missing value in participant working experience by expectation‐maximization but removed the participant whose gender was undisclosed.
Recruitment strategy was not significantly associated with participant gender (χ2(2) = 1.44, p = 0.49), but general practitioners recruited by social media were significantly younger (t(88) = 4.87, p < 0.001; M difference = 12.02 years) and had significantly less working experience (t(87) = 5.28, p < 0.001; M difference = 12.66 years) than those recruited from the healthcare corporations. However, as the participants were equally distributed across conditions (χ2(1) = 0.00, p = 1.00), both groups were included in the analysis.
Prior to hypothesis testing, a χ2‐test for independence and t‐tests were used to check for equivalence across conditions regarding participant gender, age, and working experience. Our hypothesis that patient gender (i.e., the experimental condition) would influence the assignment of an NFS‐syndrome was subsequently tested with a χ2‐test for independence, and logistic regression was used to check if this association changed when controlling for participant demographics. As adding participant age and working experience into the same model would result in considerable multicollinearity (r = 0.94, p < 0.001), only participant working experience was included as a predictor. Including participant age instead of working experience did not appreciably change any estimates (OR ± 0.01). Assumption testing confirmed linearity of the independent variables to the log odds, and sufficient sample size at minimum 10 observations per independent variable for the least frequent outcome (i.e., assigning an NFS syndrome; 32.22% likelihood). Model fit was evaluated with the receiver operating characteristic (ROC), and the contribution of individual variables with the z‐statistic and OR with 95% CIs.
Results and discussion
There was no significant difference between participants depending on which condition they were assigned to, with regard to either age (t(88) = 1.01, p = 0.32), gender (χ2(2) = 1.20, p = 0.55) or years of working experience, t(87) = −1.27, p = 0.21. As participant composition was equal, we tested if the experimental condition had a significant impact on whether participants assigned an NFS syndrome or not. We found such to be the case, as NFS syndromes were assigned significantly more often to the female patient (42.2% of cases) than the male patient (22.2% of cases), χ2(1) = 4.12, p = 0.04. Logistic regression (Table 1) confirmed that this association retained significance when participant gender and working experience were controlled for, and the logistic model performed better than chance (Fig. 1).
Table 1.
Results from logistic regression on predicting whether general practitioners (N = 89) assigned the patient an NFS syndrome or not in Study 1
| Independent variable | OR | 95% CI | z | p |
|---|---|---|---|---|
| Patient gender | 2.70 | 1.06–7.26 | 2.04 | 0.04 |
| Participant gender | 0.92 | 0.34–2.40 | −0.16 | 0.87 |
| Participant working experience | 0.98 | 0.94–1.03 | −0.73 | 0.47 |
Patient and participant gender was dummy coded as 0 = men, 1 = women. NFS = Non‐specific, somatoform, functional.
Figure 1.
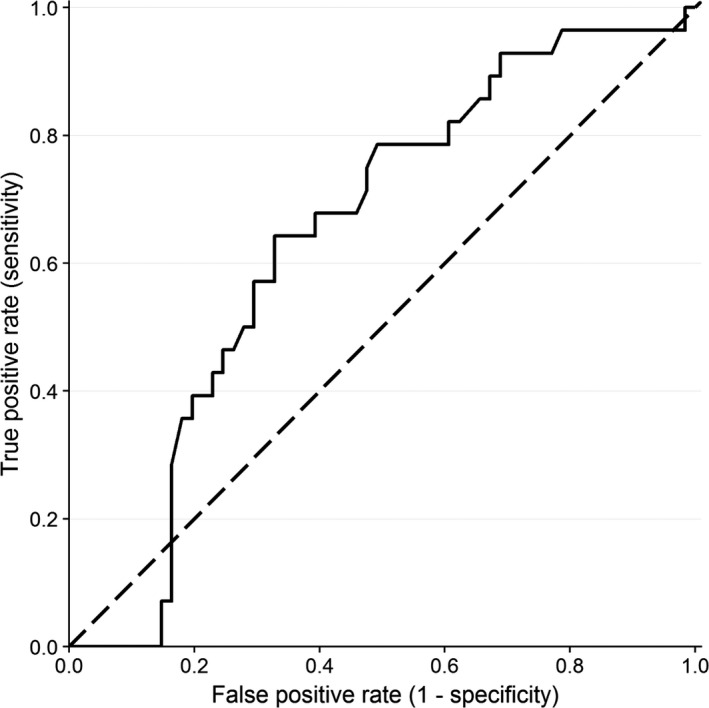
Receiver operating characteristic curves as a success rate < 0.50 for the logistic regression (solid) compared to the random curve (dashed) in Study 1.
The results thus supported our hypothesis that the female patient would be more likely than the male patient to be assigned an NFS syndrome, even when controlling for other relevant factors. As the case descriptions were identical with the exception of patient gender, we conclude that the general practitioners’ diagnostic assessment was gender biased such that a difference between the female and male patient was assumed when there was none (Risberg et al., 2009). According to ICD‐10 criteria, pain should be assessed as medically unexplained only when alternative options have been depleted (Fink, Rosendal & Olesen, 2005; Wessely et al., 1999); however, approximately 42% of general practitioners assigned an NFS syndrome to the female patients, and 22% to the male patient. Therefore, a considerable percentage of patients and especially female patients with back pain are at risk of being mismanaged within primary care, as provisional diagnostic assessments can prompt investigations and treatments which are not suitable for either refuting the initial hypothesis or providing adequate treatment (Croskerry, 2003; Elstein & Schwarz, 2002). Such has also been suggested for patients with low back pain (Taylor, Casas‐Ganem, Vaccaro et al., 2005), but also in studies on other conditions such as neck pain (Hamberg et al., 2002), chest pain (Chiaramonte & Friend, 2006; Martin, Gordon & Lounsbury, 1998), and postoperative pain (Calderone, 1990). In our study, the diagnostic assessment of NFS syndromes was not significantly affected by the general practitioner's gender or working experience, despite previous research discussing possible differences in diagnostic bias between female and male physicians (Hamberg, Risberg & Johansson, 2004), and between experienced and inexperienced physicians (Croskerry, 2003; Elstein & Schwarz, 2002).
Study 2
Not only are patients with pain initially assessed within primary care, but they are commonly managed therein as well (Fink & Rosendal, 2008; Reid et al., 2001). In primary care, patients diagnosed with NFS syndromes are often subject to treatments that require active patient participation, since such treatments has been shown to be more effective than passive measures including pharmacological interventions, operations, and injections (Henningsen, Zipfel & Herzog, 2007). Compliance with active treatment regimens has, however, been strongly associated with patients’ satisfaction with their treating physician (Barbosa, Balp, Kulich, Germain & Rofail, 2012; Berry, Parish, Janakiraman et al., 2008). Boquiren, Hack, Beaver and Williamson (2015) describe this relationship as that the aggregated positive experiences regarding, for example, physicians’ relational conduct (e.g., feeling understood, trusted, and respected) benefit treatment adherence by reducing anxiety, and increasing optimism for treatment success and recovery. Indeed, overall satisfaction with the patient–doctor relationship has been significantly associated to more favorable treatment outcomes, such as lower pain levels, better physical functioning, and higher quality of life (Farin, Gramm & Schmidt, 2013).
However, for patients with NFS syndromes, there are several threats to experiences of positive relational conduct. For example, managing patients with medically unexplained symptoms are by general practitioners often seen as frustrating, stressful, and difficult (Hahn, 2001; May, Allison, Chapple et al., 2004; Reid et al., 2001; Shattock, Williamson, Caldwell, Anderson & Peters, 2013; Woivalin, Krantz, Mäntyranta & Ringsberg, 2004). General practitioners may also doubt that patients’ symptoms are genuine (Murray, Toussaint, Althaus & Löwe, 2016), and aim their focus to providing symptom alleviation instead of emotional support (Nordin, Hartz, Noyes et al., 2006). On the other hand, patients with NFS syndromes emphasize a need for feeling understood by and receiving encouragement from their physician (Peters, Rogers, Salmon et al., 2009; Salmon, Ring, Dowrick & Humphris, 2005). They also report to a larger extent than patients without NFS syndromes that their treating physician does not adhere to their needs, and disbelieve their self‐reported pain intensity and disability (Dickson, Knussen & Flowers, 2007; Dwamena, Lyles, Frankel & Smith, 2009; McGowan, Luker, Creed & Chew‐Graham, 2007). Little is yet known about whether the healthcare experiences of patients with NFS syndromes differ depending on their gender, and studies which compare women's and men's healthcare perceptions without accounting for diagnosis show disparate results. Some studies report that men experience more negative encounters (Müssener, Festin, Upmark & Alexanderson, 2008; Wessel, Helgesson, Olsson, Juth, Alexanderson & Lynöe, 2012) whereas others suggest that women do (Upmark, Borg & Alexanderson, 2007). Nevertheless, women with NFS syndromes could be especially vulnerable due to the accession of several negative stereotypes general practitioners may have about their diagnosis and gender. For example, these could include that women's pain is often considered as exaggerated and is therefore underestimated and undertreated (Calderone, 1990; Hamberg et al., 2002; Tait et al., 2009), and similar associations have been made for patients with NFS syndromes (Murray et al., 2016; Tait et al., 2009).
The purpose of our second study was therefore to compare how patients with contra without NFS syndromes perceive the relational conduct of their treating physician, and if patient gender interacts with this effect. Based on previous research, we expected that patients with an NFS syndrome would perceive the relational conduct of their treating physician as more negative than would those without (Dickson et al., 2007; Dirkzwager & Verhaak, 2007). However, because earlier work comparing women's and men's perceptions of relational conduct has shown mixed results (Müssener et al., 2008; Upmark et al., 2007; Wessel et al., 2012), we chose not to specify a hypothesis for a main effect of gender. Nevertheless, we hypothesized that an interaction effect of gender and NFS syndromes, such that women with NFS syndromes would perceive their physician's relational conduct as more negative than would women with other pain conditions, and men both with and without NFS syndromes. This interaction was postulated as general practitioners underestimate and undertreat the pain of both women and patients with NFS syndromes (Calderone, 1990; Hamberg et al., 2002; Murray et al., 2016; Tait et al., 2009), which could amount to that women diagnosed with NFS syndromes perceive their healthcare encounters as more negative than others. In addition to testing our specified hypotheses, we conducted descriptive analyses to compare the demographics of our community‐recruited sample with regard to whether they had an NFS syndrome or not, for the purpose of assessing the comparability between our sample and those utilized in previous research.
Methods
Participants
Participants in the current study were selected from a larger sample of 1,184 individuals who partook in a cross‐sectional project on pain in the Swedish community during 2017 (cf. Claréus & Bäck, 2018). As our hypotheses concerned comparing women and men diagnosed with an NFS syndrome to those with other diagnoses, 231 of these participants were excluded in the current study: 188 for reporting that their current pain condition was not clinically diagnosed, 28 whose pain condition was undisclosed, 10 who did not disclose their gender, three who identified as neither a woman nor a man, and two participants with 30% and 60% of values missing, respectively.
The final sample comprised 953 participants, including 773 women and 180 men, and their mean age was 48.25 years (SD = 11.59). A detailed breakdown of the sample demographics can be found in Table 2.
Table 2.
Total and within‐group demographics, including between‐group difference tests in the online survey (N = 953) in Study 2
| Variable | n (%)/M (SD, range) | Difference test | ||
|---|---|---|---|---|
| Total (N = 953) | Non‐NFS syndrome (N = 432) | At least 1 NFS syndrome (N = 521) | ||
| Gender |
χ2(1) = 78.83, p < 0.001, Cramer's V = 0.29 |
|||
| Men | 180 (18.89) | 135 (31.25) | 45 (8.64) | |
| Women | 773 (81.11) | 297 (68.75) | 476 (91.36) | |
| Age | 48.25 (11.59, 18–83)a | 48.99 (12.63, 18–83)b | 47.63 (10.62, 18–78)c |
t(947) = 1.81, p = 0.07, Cohen's d = 0.12 |
| Shares household with a partner |
χ2(1) = 2.09, p = 0.15, Cramer's V = 0.05 |
|||
| Yes | 673 (70.62) | 315 (72.92) | 358 (68.71) | |
| No | 276 (28.96) | 115 (26.62) | 161 (30.90) | |
| N/A | 4 (0.42) | 2 (0.46) | 2 (0.38) | |
| Shares household with children younger than 18 years |
χ2(1) = 2.65, p = 0.10, Cramer's V = 0.05 |
|||
| Yes | 333 (34.94) | 139 (32.18) | 194 (37.24) | |
| No | 618 (64.85) | 292 (67.59) | 326 (62.57) | |
| N/A | 2 (0.21) | 1 (0.23) | 1 (0.19) | |
| Educational level |
χ2(2) = 17.36, p < 0.001, Cramer's V = 0.14 |
|||
| Elementary | 78 (8.18) | 30 (6.94) | 48 (9.21) | |
| Upper secondary | 472 (49.53) | 188 (43.52) | 284 (54.51) | |
| University | 398 (41.76) | 212 (49.07) | 186 (35.70) | |
| N/A | 5 (0.52) | 2 (0.46) | 3 (0.58) | |
| Employment status |
χ2(4) = 15.65, p = 0.004, Cramer's V = 0.13 |
|||
| Employed | 742 (77.86) | 341 (78.94) | 401 (76.97) | |
| Unemployed | 67 (7.03) | 19 (4.40) | 48 (9.21) | |
| Studying | 11 (1.15) | 5 (1.16) | 6 (1.15) | |
| Retried | 67 (7.03) | 41 (9.49) | 26 (4.99) | |
| N/A | 66 (6.93) | 26 (6.02) | 40 (7.68) | |
| Extent of current sick leave |
χ2(2) = 30.49, p < 0.001, Cramer's V = 0.18 |
|||
| Not on sick leave | 450 (47.22) | 242 (56.02) | 208 (39.92) | |
| Part‐time | 228 (23.92) | 101 (23.38) | 127 (24.38) | |
| Full‐time | 272 (28.54) | 89 (20.60) | 183 (35.12) | |
| N/A | 3 (0.31) | 3 (0.58) | ||
| Disclosed diagnoses |
χ2(1) = 58.83, p < 0.001, Cramer's V = 0.25 |
|||
| One | 605 (63.48) | 331 (76.62) | 274 (52.59) | |
| Two or more | 348 (36.52) | 101 (23.38) | 247 (47.41) | |
| Regular healthcare contacts |
χ2(1) = 0.50, p = 0.48, Cramer's V = 0.02 |
|||
| Yes | 662 (69.46) | 305 (70.60) | 357 (68.52) | |
| No | 289 (30.33) | 126 (29.17) | 163 (31.29) | |
| N/A | 2 (0.21) | 1 (0.23) | 1 (0.19) | |
| Pain disability | 42.07 (10.51, 8–60)d | 39.69 (11.00, 8–60)e | 44.04 (9.66, 10–60)f |
t(926) = ‐6.41, p < 0.001, Cohen's d = 0.42 |
N/A specifies those participants with missing values within the current variable. Missing cases were excluded in the between‐group comparisons, with the exception of employment status where missing cases were analyzed as a separate level. Pain disability was computed as the summed score of participants’ perceived disability to partake in six different activities (engaging in family/home responsibilities, recreational activities, sports, and social activities, and performing paid and unpaid work). NFS = Non‐specific, somatoform, functional.
a N = 949, b n = 431, c n = 518, d N = 928, e n = 421, f n = 507
Materials: Pain diagnosis/es
Participants were asked to indicate if their pain was clinically diagnosed or not, and if so, which diagnosis/diagnoses they had been diagnosed with. The coding procedure in which diagnoses were classified according to ICD‐10 is described elsewhere (Claréus & Bäck, 2018). Utilizing an operationalization of NFS syndromes provided by Schaefert et al. (2012), diagnoses subsequently coded as NFS included: fibromyalgia (n = 411), tension‐type headache (n = 35), myalgia (n = 25), unspecified chronic pain (n = 25), ME/CFS (n = 21), IBS (n = 11), unspecified pain (n = 11), trigeminal neuralgia (n = 11), repetitive strain injury (n = 10), tinnitus (n = 3), unspecified dosalgia (n = 3), unspecified headache (n = 3), postviral fatigue syndrome (n = 2), somatoform disorder (n = 2), and bruxism (n = 1). The number of disclosed diagnoses was computed as a separate variable, indicating either 1 disclosed diagnosis or ≥2 disclosed diagnoses.
Materials: Pain disability
Participants’ perceived disability was measured by an adapted version of the Pain Disability Index (Tait, Chibnall & Krause, 1990), not including sexual behavior, self‐care, and life‐support activities. Therefore, pain disability was in the current study, operationalized as the summed score of participants’ estimated disability to engage in family/home responsibilities, recreational activities, sports, and social activities, and perform paid and unpaid work. Participants were asked to estimate their overall disability to partake in these six activities on a 1 (No disability) to 10 (Full disability) scale, without accounting for when their pain is at its worst. In the current study, the Cronbach's alpha was 0.90 and the McDonald's omega (Dunn, Baguley & Brunsden, 2014) was 0.89, which indicate good internal reliability.
Materials: Regular contact with healthcare services
Participants were asked if they had regular contacts with healthcare services due to their pain, with the possibility of answering Yes or No.
Materials: Relational conduct
We designed four items with the purpose of assessing participants’ view on the relational conduct of their physician, including goal sharing (“Do you think that you and your physician share the same goals?”), understanding (“Do you think that your physician understands you?”), trust (“Do you think that your physician trusts your own pain assessment?”), and overall relationship quality (“Do you think that you and your physician have a good relationship with each other?”). Participants scored their agreement to these four statements on a 1 (No, not at all) to 7 (Yes, absolutely) Likert scale. As a Principal Components Analysis with Varimax rotation confirmed a single factor explaining 81.49% of the variance to which all items had loadings between 0.87–0.94, the items were averaged into a single scale with good internal consistency (Cronbach's alpha = 0.92, McDonald's omega = 0.92).
Procedure
The study was advertised through social media, patient societies, and health‐care clinics under the time period April–October 2017 (n = 825), and in November 2017 distributed through similar venues with an identical design but specifically directed toward male participants (n = 128). The advertisement invited individuals who currently experienced pain with a significant impact on their quality of life to partake in an online survey in exchange for a lottery ticket. Participants were initially briefed about the study's purpose and informed about their right to discontinue their participation at any given moment by terminating the webpage. After providing informed consent, they provided demographic data and answered a battery of questions including those of the current study.
Statistical analyses
Preliminary data checks were conducted to examine internal attrition, and to ensure that the assumptions of linear regression were not violated. With the exception of employment status (6.9% of values missing), no item exceeded 1.4% missingness. Further inspection with pattern analysis revealed that missingness in employment status was the only discernable pattern. Missing data in the employment variable could therefore be attributed to external factors, and were analyzed as a separate level. On the other hand, missing at random (MAR) could be assumed for the remaining variables. Therefore, to maximize the amount of available cases in hypothesis‐testing, missing values were imputed from the available data with either predictive mean matching (continuous variables) or logistic regression (dummy‐coded categorical variables). All imputations were carried out utilizing version 2.46.0 of the mice package (Buuren & Groothuis‐Oudshoorn, 2010) in R, with 50 imputed datasets over 20 iterations.
As results from the descriptive analyses did not differ appreciably between the pre‐ and post‐imputation data, Student's t‐tests and χ2‐tests of independence were performed on the pre‐imputation dataset as their main purpose was to compare the demographics of our sample with those utilized in previous research. Cohen's d and Cramer's V were used as estimates of effect size, interpreted according to Cohen's conventions (Cohen, 1988, 1992). Inspection of the histograms revealed no prominent deviations of normality for the continuous variables, and skewness values within the commonly used cutoff of ±1 (Hair, Tatham, Anderson & Black, 1998).
Linear regression was used to test our hypotheses regarding the effect of NFS syndromes and their interaction with gender on patients’ perceptions of their physician's relational conduct. In the first model, whether the participant had reported an NFS diagnosis or not (0 = No, 1 = Yes, at least one) and their gender (0 = man, 1 = woman) were entered as main effects. In the second, effects coding was utilized to successively compare women with at least one NFS syndrome (0) with other women, and with men both with and without at least one NFS syndrome. In each model, we utilized the following levels within parentheses as the reference category for the nominal variables with >2 levels: educational level (elementary education), employment status (missing value), and sick‐leave extent (currently not on sick‐leave). Model fit was evaluated with pooled F‐statistic and adjusted R 2, and the contribution of independent variables with the pooled t‐statistic, and the unstandardized (b) and standardized (β) regression coefficients. Regression diagnostics confirmed that both models met the assumptions of residual normality, homoskedasticity, and independence of the errors, and there was no considerable multicollinearity between any of the independent variables.
Results and discussion
The demographics of our sample (Table 2) were on several aspects similar to earlier research on cohorts, even if our study relied on self‐report and non‐probability sampling. For example, mean sample age fell between a span of 47–49 years and the majority were women, which correspond with that the prevalence of pain is the highest in Swedish individuals around 50 years of age and in Swedish women (Gerdle et al., 2004; Harker et al., 2012). Women were also significantly overrepresented among the 55% who reported at least one NFS syndrome, and prevalence estimates of NFS syndromes in primary care show similarly that a disproportionate number of women present with these syndromes as compared to men (Barsky, Orav & Bates, 2005; Dirkzwager & Verhaak, 2007; Verhaak, Meijer, Visser & Wolters, 2006). Moreover, participants with NFS syndromes reported higher comorbidity (47% vs. 23%) and pain disability (M difference = 4.35), which converge with earlier studies on functional impairment and comorbidity in patients with NFS syndromes (Carson, Stone, Hibberd et al., 2011; Dirkzwager & Verhaak, 2007; Fink et al., 2005; Wessely et al., 1999). Other significant demographic differences have been reported earlier as well, including that NFS syndromes were significantly associated with lower educational level (Dirkzwager & Verhaak, 2007), unemployment (Verhaak et al., 2006), and current full‐time sick‐leave (Rask et al., 2015). While we did not measure actual frequency of healthcare visits as did Barsky et al. (2005), we similarly found that participants with NFS syndromes were more likely to report that they were in regular contact with healthcare services.
Results from predicting participants’ perception of their treating physician's relational conduct by linear modeling on the imputed dataset are available in Table 3. Other researchers have described disparities between the goals of physicians and patients with NFS syndromes (Nordin et al., 2006; Salmon et al., 2005), and that patients with these conditions recall experiences of disrespectful and distrustful healthcare encounters (Dickson et al., 2007; Dirkzwager & Verhaak, 2007; Dwamena et al., 2009; McGowan et al., 2007). In correspondence with this work, the first model supported our hypothesis that individuals with at least one NFS diagnosis would report a significantly lower level of relational conduct, as compared to those with another diagnosis/other diagnoses (b = −0.26, β = −0.07, p = 0.04). However, we did not find a significant main effect of participant gender in Model 1 (b = −0.15, β = −0.03, p = 0.34), suggesting that neither women nor men perceived their relationship as more negative than did the other. While other Swedish studies which has shown significant yet directionally different results between men and women's perceptions of their healthcare experiences (Müssener et al., 2008; Upmark et al., 2007; Wessel et al., 2012), these studies focused on currently part‐ or full‐time sick‐listed individuals with a variety of diagnoses. The results of our study are, due to our inclusion criteria, instead more generalizable toward individuals with pain, regardless of the extent of their current sick‐leave.
Table 3.
Pooled regression coefficients from predicting patients’ (N = 953) perception of physician's relational conduct by linear regression in Study 2
| Variable | Model 1: F pooled(16, 936) = 12.64, p < 0.001, adjusted R 2 pooled = 0.16 | Model 2: F pooled(17, 935) = 12.08, p < 0.001, adjusted R 2 pooled = 0.17 | ||||||
|---|---|---|---|---|---|---|---|---|
| B (SE) | β | t | p | B (SE) | β | t | p | |
| Age | 0.02 (0.01) | 0.14 | 3.88 | <0.001 | 0.02 (0.01) | 0.14 | 3.95 | <0.001 |
| Shares household with a partner (0 = no, 1 = yes) | 0.12 (0.13) | 0.03 | 0.90 | 0.37 | 0.11 (0.13) | 0.03 | 0.84 | 0.40 |
| Shares household with children younger than 18 years (0 = no, 1 = yes) | 0.02 (0.13) | 0.005 | 0.15 | 0.88 | 0.02 (0.13) | 0.01 | 0.19 | 0.85 |
| Educational level (reference = elementary school) | ||||||||
| Upper secondary | 0.32 (0.21) | 0.09 | 1.51 | 0.13 | 0.33 (0.21) | 0.09 | 1.54 | 0.12 |
| University | 0.39 (0.22) | 0.11 | 1.81 | 0.07 | 0.38 (0.22) | 0.10 | 1.76 | 0.08 |
| Employment status (reference = missing values) | ||||||||
| Employed | 0.77 (0.23) | 0.17 | 3.38 | 0.001 | 0.75 (0.23) | 0.17 | 3.31 | 0.001 |
| Unemployed | 0.44 (0.56) | 0.03 | 0.79 | 0.43 | 0.43 (0.56) | 0.02 | 0.76 | 0.45 |
| Studying | 0.37 (0.30) | 0.05 | 1.25 | 0.21 | 0.38 (0.30) | 0.05 | 1.28 | 0.20 |
| Retired | 1.23 (0.34) | 0.17 | 3.67 | <0.001 | 1.22 (0.34) | 0.17 | 3.65 | <0.001 |
| Extent of current sick‐leave (reference = not on sick‐leave) | ||||||||
| Part‐time | 0.60 (0.15) | 0.14 | 4.09 | <0.001 | 0.61 (0.15) | 0.14 | 4.15 | <0.001 |
| Full‐time | 0.62 (0.15) | 0.15 | 4.11 | <0.001 | 0.63 (0.15) | 0.15 | 4.15 | <0.001 |
| Disclosed diagnoses (0 = one, 1 = two or more) | −0.25 (0.12) | −0.07 | −2.04 | 0.04 | −0.26 (0.12) | −0.07 | −2.07 | 0.04 |
| Regular healthcare contacts (0 = no, 1 = yes) | 1.05 (0.13) | 0.26 | 8.25 | <0.001 | 1.04 (0.13) | 0.26 | 8.17 | <0.001 |
| Pain disability | −0.02 (0.01) | −0.12 | −3.68 | <0.001 | −0.02 (0.01) | −0.12 | −3.68 | <0.001 |
| Gender (0 = men, 1 = women) | −0.15 (0.16) | −0.03 | −0.96 | 0.34 | ||||
| NFS syndrome (0 = no, 1 = yes, at least one) | −0.26 (0.12) | −0.07 | −2.11 | 0.04 | ||||
| Gender and NFS syndrome (reference = women with at least one NFS syndrome) | ||||||||
| Women without NFS syndrome | 0.35 (0.13) | 0.09 | 2.58 | 0.01 | ||||
| Men with at least one NFS syndrome | 0.51 (0.27) | 0.06 | 1.88 | 0.06 | ||||
| Men without NFS syndrome | 0.33 (0.18) | 0.06 | 1.83 | 0.07 | ||||
Both models were computed on data with missing values imputed by predictive mean matching with 50 datasets over 20 iterations. NFS = Non‐specific, somatoform, functional.
However, although we did not find a significant main effect of gender in our first model, an interesting pattern emerged when women with NFS syndromes were compared to other groups in the second model. These women perceived significantly poorer conduct than did women with other diagnoses (b = 0.35, β = 0.09, p = 0.01), and results approached significance when women with NFS syndromes were compared to men with similar conditions (b = 0.51, β = 0.06, p = 0.06) and those men with other diagnoses (b = 0.33, β = 0.06, p = 0.07).
Our results thus suggest that when demographics, comorbidity, pain disability, and regularity of healthcare contacts are accounted for, women and men without NFS syndromes have similar perceptions of their physician's relational conduct. Men with NFS syndromes had slightly more positive evaluations than individuals without NFS syndromes, but with considerable variation (Model 2: SE = 0.27) which can be attributed to small subsample size (n = 45). The perceptions of relational conduct among these three groups are in turn more positive than the perceptions of women with NFS syndromes, which is in line with what was hypothesized. These results could be explained by that being the subject of physician's stereotypes about the immateriality of pain due to both womanhood and having medically unexplained symptoms (Calderone, 1990; Hamberg et al., 2002; Murray et al., 2016; Tait et al., 2009) can amount to more negative perceptions of physician's relational conduct. This can have detrimental effects on these women's rehabilitation, as the management of NFS syndromes in primary care is often dependent on the interpersonal attributes of the patient–physician interaction (Fink & Rosendal, 2008; Woivalin et al., 2004).
With regard to the covariates included in this study, those who predicted more positive perceptions of physician's relational conduct in both models were having regular as compared to irregular health care visits, or being currently employed or in retirement. That retirement predicted more positive perceptions converge with our finding that age was a significant positive predictor as well, such that older people perceived better relational conduct than younger people did. Having finished a university education as compared to either elementary or upper secondary was borderline significant of more positive evaluations as well (p = 0.07–0.08). Finally, not currently being on sick‐leave, comorbidity, and experiencing high pain disability was predictive of worse perceptions of relational conduct. These findings replicate earlier research, which has demonstrated significant positive associations between healthcare satisfaction with healthcare utilization (Fan, Burman, McDonell & Fihn, 2005), employment (Fan et al., 2005), older age (Jackson, Chamberlin & Kroenke, 2001; Young, Meterko & Desai, 2000), and better functional status and overall health (Jackson et al., 2001; Young et al., 2000).
General Discussion
The purpose of the present article was to study two aspects of nonspecific, functional, and somatoform (NFS) syndromes in a Swedish context, which together could highlight different aspects gender bias in the primary care system. First, we intended to establish whether general practitioners display gender bias in the assessment of NFS syndromes. Even though NFS syndromes should only be considered when investigations are inconclusive (Fink et al., 2005; Wessely et al., 1999), our vignette‐based experiment showed that back pain in a female patient was more often assessed as NFS when compared to an otherwise identical male patient. A similar impact of gender bias on diagnostic assessment of NFS syndromes has been demonstrated for junior physicians as well (Hamberg et al., 2002). Whether the assessment was intended as provisional while continuing the investigation into potential organic causes or as warranting specific interventions is unknown. Nevertheless, as these syndromes should only be considered when alterative explanations have been refuted (Fink et al., 2005; Wessely et al., 1999), our results indicate a prevalence of a stereotype such that women's pain is likely to be medically unexplained. This stereotype could impact diagnostic reassessment in women with pain, as general practitioners are more likely to look for evidence which is congruent with rather than disparate to their initial hypothesis (Croskerry, 2003; Elstein & Schwarz, 2002), or can begin to doubt the authenticity of the reported symptoms (Murray et al., 2016).
Meanwhile, these women express that they are reliant on their treating physician's psychosocial support and communicative attributes in order to manage their symptoms and remain in treatment (Fink & Rosendal, 2008; Woivalin et al., 2004). Therefore, we examined patients’ perceptions of the relational conduct of their treating physician in the second study. Patients whom had been clinically diagnosed with at least one NFS syndrome perceived poorer relational conduct than those patients with other conditions did, even when a wide range of other pain characteristics and sociodemographic factors were controlled for. These findings are congruent with earlier work (e.g., Dickson et al., 2007; Dirkzwager & Verhaak, 2007), delineating that NFS syndromes are associated to more negative healthcare experiences among patients with pain. However, while we did not find a main effect of gender, we found that women with NFS syndromes evaluated their treating physician's conduct as poorer than did other women, as well as men with and without medically unexplained pain.
Taken together, our two studies combined describe how gender is an influencing factor in both the diagnostic assessment and ongoing management of patients with medically unexplained symptoms. When women's pain is assessed as medically unexplained due to stereotypes about its causes (or lack thereof), pertinent somatic interventions may not be considered for female patients whereas those are attempted for male patients (Calderone, 1990; Chiaramonte & Friend, 2006; Hamberg et al., 2002; Martin et al., 1998; Taylor et al., 2005). This gender bias could persist even if the current definition of NFS is revised; from several diagnoses based on the exclusion of an organic cause in ICD‐10, to one Bodily Distress Disorder (BDD) focusing on the inclusion of psychological symptoms as proposed in ICD‐11 (Gureje & Reed, 2016; Löwe, Mundt, Herzog et al., 2008). While the revision makes it possible to develop checklists that aid diagnostic assessment by increasing physician's symptom certainty and thus reducing their reliance on stereotypes (Fiske, Lin & Neuberg, 1999; Tait et al., 2009), research has shown that physicians are more likely to misattribute women's pain when psychological stressors are coexistent (Chiaramonte & Friend, 2006; Martin et al., 1998). Physicians may therefore retain their stereotypes about the role of socio‐cognitive and psychological factors are more salient than organic causes in explaining women's pain, even when the diagnostic criteria are revised. The negative attitudes and poor outcome expectations that physicians currently associate with NFS syndromes could be transferred to BDD (Gureje & Reed, 2016), which could adversley impact pain rehabilitation for women whose symptoms are biomedically unexplained. These women still require medical attention, as continued investigations might reveal an organic cause and special care is required to manage or treat their symptoms. However, as women with medically unexplained pain become subject of physician's negative preconceptions and subsequently experience more negative healthcare encounters, their volition to partake in futher investigations and either to begin or persevere in treatment is lowered (Barbosa et al., 2012; Berry et al., 2008).
In conclusion, due to stereotypes about medically unexplained pain and pain in women, those women whose pain is initially assessed as either NFS or BDD are at risk of being mismanaged within primary care, and of experiences that negatively influence their treatment compliance. Both are factors that would impede and prolong pain rehabilitation in women as compared to men, which therefore could contribute to the higher prevalence of chronic (e.g., Gerdle et al., 2004) and medically unexplained pain (e.g., Schaefert et al., 2012) in women. Most models which explain the higher prevalence of medically unexplained pain in women focus on the interaction between biological, socio‐cognitive, and psychological factors, as the evidence of a biomedical model is only preliminary at best (Fillingim et al., 2009; Yunus, 2001). We suggest expanding these models to include external factors, such as gender bias and gender‐associated stereotypes among medical professionals, which may be valuable for a more comprehensive picture of the higher prevalence of pain in women compared to men.
Limitations and future research
Some limitations of the present research are worth noting. First, regarding samples, it was difficult to reach general practitioners and our final sample was relatively small. Such problems limit the possibility to add other independent variables and covariates to the design, which could be desired. In addition, the patient sample was problematic in the considerable overrepresentation of women albeit special efforts were directed toward recruiting men. This is probably due to that women in general tend to participate more in surveys (Gosling, Vazire, Srivastava & John, 2004), but also that they are more often diagnosed with pain conditions and prescribed sick‐leave for such conditions (Bergman et al., 2001; Stålnacke, Haukenes, Lehti et al., 2015; Wijnhoven, De Vet & Picavet, 2006). Due to the recruitment issues, we suggest that future qualitative research about the healthcare experiences of men with medically unexplained pain could be utilized to better understand how this group perceives their physician's relational conduct.
Secondly, while the second study focused on participants’ aggravated interpretations of physician's relational conduct over many consultations, the first study focused on the initial visit and asked the physicians to make an assessment without access to any clinical evidence. Although it has been suggested that patients are more influenced by their aggravated impression of several healthcare consultations rather than singular consultations (Darlow, Dowell, Baxter et al., 2013; Street, Makoul, Arora & Epstein, 2009), replicating our studies longitudinally might provide important insights into how patients’ perceptions change over time and if interpersonal dynamics and clinical investigations moderate gender bias in diagnostic assessment.
Finally, while the first study focused on low back pain symptoms in particular, there was higher symptom variability both within the NFS group and among those participants with other conditions in Study 2. Therefore, research on more homogenous samples is necessary (e.g., comparing patients with spinal disc herniation and patients with medically unexplained back pain) to provide valid support for the association between NFS syndromes and poorer healthcare experiences among specific subpopulations. With the implementation of ICD‐11, there is also need to study the biases and patient experiences that are associated with BDD or a similar condition as changes in operationalization could change how these conditions are assessed and managed within primary care.
The current study was approved by the Regional Ethics Board at the University of Gothenburg (no. 1120‐16).
The present research was funded by AFA Försäkring, grant number 140379. AFA Försäkring had no role in study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. The authors have no other competing interests to report.
The authors wish to thank Amanda Klysing for the assistance with coding.
Claréus, B. & Renström, E. A. (2019). Physicians’ gender bias in the diagnostic assessment of medically unexplained symptoms and its effect on patient–physician relations. Scandinavian Journal of Psychology, 60, 338–347.
The copyright line for this article was changed on 28 May 2019 after original online publication.
References
- Barbosa, C. D. , Balp, M.‐M. , Kulich, K. , Germain, N. & Rofail, D. (2012). A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Preference and Adherence, 6, 39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barsky, A. J. , Orav, E. J. & Bates, D. W. (2005). Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Archives of General Psychiatry, 62, 903–910. [DOI] [PubMed] [Google Scholar]
- Bergman, S. , Herrström, P. , Högström, K. , Petersson, I. F. , Svensson, B. & Jacobsson, L. T. (2001). Chronic musculoskeletal pain, prevalence rates, and sociodemographic associations in a Swedish population study. The Journal of Rheumatology, 28, 1369–1377. [PubMed] [Google Scholar]
- Berry, L. L. , Parish, J. T. , Janakiraman, R. , Ogburn‐Russell, L. , Couchman, G. R. , Rayburn, W. L. & Grisel, J. (2008). Patients’ commitment to their primary physician and why it matters. The Annals of Family Medicine, 6, 6–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boquiren, V. M. , Hack, T. F. , Beaver, K. & Williamson, S. (2015). What do measures of patient satisfaction with the doctor tell us? Patient Education and Counseling, 98, 1465–1473. [DOI] [PubMed] [Google Scholar]
- Breivik, H. , Collett, B. , Ventafridda, V. , Cohen, R. & Gallacher, D. (2006). Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. European Journal of Pain, 10, 287–333. [DOI] [PubMed] [Google Scholar]
- Buuren, S. V. & Groothuis‐Oudshoorn, K. (2010). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45, 1–68. [Google Scholar]
- Calderone, K. L. (1990). The influence of gender on the frequency of pain and sedative medication administered to postoperative patients. Sex Roles, 23, 713–725. [Google Scholar]
- Carson, A. , Stone, J. , Hibberd, C. , Murray, G. , Duncan, R. , Coleman, R. et al (2011). Disability, distress and unemployment in neurology outpatients with symptoms ‘unexplained by organic disease’. Journal of Neurology, Neurosurgery & Psychiatry, 82, 810–813. [DOI] [PubMed] [Google Scholar]
- Chiaramonte, G. R. & Friend, R. J. H. P. (2006). Medical students’ and residents’ gender bias in the diagnosis, treatment, and interpretation of coronary heart disease symptoms. Health Psychology, 25, 255–266. [DOI] [PubMed] [Google Scholar]
- Claréus, B. & Bäck, E. A. (2018). An investigation of physical pain among Swedish community adults: Sample demographics and pain characteristics. Lund Psychological Reports, 18, 1–15. [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: L. Erlbaum Associates. [Google Scholar]
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112, 155–159. [DOI] [PubMed] [Google Scholar]
- Croskerry, P. (2003). The importance of cognitive errors in diagnosis and strategies to minimize them. Academic Medicine, 78, 775–780. [DOI] [PubMed] [Google Scholar]
- Darlow, B. , Dowell, A. , Baxter, G. D. , Mathieson, F. , Perry, M. & Dean, S. (2013). The enduring impact of what clinicians say to people with low back pain. Annals of Family Medicine, 11, 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson, A. , Knussen, C. & Flowers, P. (2007). Stigma and the delegitimation experience: An interpretative phenomenological analysis of people living with chronic fatigue syndrome. Psychology and Health, 22, 851–867. [Google Scholar]
- Dirkzwager, A. J. & Verhaak, P. F. (2007). Patients with persistent medically unexplained symptoms in general practice: Characteristics and quality of care. BMC Family Practice, 8, 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn, T. J. , Baguley, T. & Brunsden, V. (2014). From alpha to omega: A practical solution to the pervasive problem of internal consistency estimation. British Journal of Psychology, 105, 399–412. [DOI] [PubMed] [Google Scholar]
- Dwamena, F. C. , Lyles, J. S. , Frankel, R. M. & Smith, R. C. (2009). In their own words: Qualitative study of high‐utilising primary care patients with medically unexplained symptoms. BMC Family Practice, 10, 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elstein, A. S. & Schwarz, A. (2002). Clinical problem solving and diagnostic decision making: Selective review of the cognitive literature. BMJ, 324, 729–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan, V. S. , Burman, M. , McDonell, M. B. & Fihn, S. D. (2005). Continuity of care and other determinants of patient satisfaction with primary care. Journal of General Internal Medicine, 20, 226–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farin, E. , Gramm, L. & Schmidt, E. (2013). The patient‐physician relationship in patients with chronic low back pain as a predictor of outcomes after rehabilitation. Journal of Behavioral Medicine, 36, 246–258. [DOI] [PubMed] [Google Scholar]
- Fillingim, R. B. , King, C. D. , Ribeiro‐Dasilva, M. C. , Rahim‐Williams, B. & Riley, J. L. (2009). Sex, gender, and pain: A review of recent clinical and experimental findings. The Journal of Pain, 10, 447–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink, P. & Rosendal, M. (2008). Recent developments in the understanding and management of functional somatic symptoms in primary care. Current Opinion in Psychiatry, 21, 182–188. [DOI] [PubMed] [Google Scholar]
- Fink, P. , Rosendal, M. & Olesen, F. (2005). Classification of somatization and functional somatic symptoms in primary care. Australian and New Zealand Journal of Psychiatry, 39, 772–781. [DOI] [PubMed] [Google Scholar]
- Fiske, S. T. , Lin, M. & Neuberg, S. L. (1999). The continuum model: Ten years later In Chaiken S., & Trope Y. (Eds.), Dual‐process theories in social psychology (pp. 231–254). New York: Guilford Press. [Google Scholar]
- Gerdle, B. , Björk, J. , Henriksson, C. & Bengtsson, A. (2004). Prevalence of current and chronic pain and their influences upon work and healthcare‐seeking: A population study. The Journal of Rheumatology, 31, 1399–1406. [PubMed] [Google Scholar]
- Gosling, S. D. , Vazire, S. , Srivastava, S. & John, O. P. (2004). Should we trust web‐based studies? A comparative analysis of six preconceptions about internet questionnaires. American Psychologist, 59, 93–104. [DOI] [PubMed] [Google Scholar]
- Gureje, O. & Reed, G. M. (2016). Bodily Distress Disorder in ICD‐11: Problems and prospects. World Psychiatry, 15, 291–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn, S. R. (2001). Physical symptoms and physician‐experienced difficulty in the physician‐patient relationship. Annals of Internal Medicine, 134, 897–904. [DOI] [PubMed] [Google Scholar]
- Hair, J. F. , Tatham, R. L. , Anderson, R. E. & Black, W. C. (1998). Multivariate data analysis. London: Prentice Hall. [Google Scholar]
- Hamberg, K. , Risberg, G. & Johansson, E. E. (2004). Male and female physicians show different patterns of gender bias: A paper‐case study of management of irritable bowel syndrome. Scandinavian Journal of Public Health, 32, 144–152. [DOI] [PubMed] [Google Scholar]
- Hamberg, K. , Risberg, G. , Johansson, E. E. & Westman, G. (2002). Gender bias in physicians’ management of neck pain: A study of the answers in a Swedish national examination. Journal of Women's Health & Gender‐Based Medicine, 11, 653–666. [DOI] [PubMed] [Google Scholar]
- Harker, J. , Reid, K. J. , Bekkering, G. E. , Kellen, E. , Bala, M. M. , Riemsma, R. et al (2012). Epidemiology of chronic pain in Denmark and Sweden. Pain Research and Treatment, 2012, 371248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henningsen, P. , Zipfel, S. & Herzog, W. (2007). Management of functional somatic syndromes. The Lancet, 369, 946–955. [DOI] [PubMed] [Google Scholar]
- Jackson, J. L. , Chamberlin, J. & Kroenke, K. (2001). Predictors of patient satisfaction. Social Science & Medicine, 52, 609–620. [DOI] [PubMed] [Google Scholar]
- Löwe, B. , Mundt, C. , Herzog, W. , Brunner, R. , Backenstrass, M. , Kronmüller, K. & Henningsen, P. (2008). Validity of current somatoform disorder diagnoses: Perspectives for classification in DSM‐V and ICD‐11. Psychopathology, 41, 4–9. [DOI] [PubMed] [Google Scholar]
- Martin, R. , Gordon, E. E. & Lounsbury, P. (1998).Gender disparities in the attribution of cardiac‐related symptoms: Contribution of common sense models of illness. Health Psychology, 17, 346–357. [DOI] [PubMed] [Google Scholar]
- May, C. , Allison, G. , Chapple, A. , Chew‐Graham, C. , Dixon, C. , Gask, L. , et al(2004). Framing the doctor‐patient relationship in chronic illness: A comparative study of general practitioners’ accounts. Sociology of Health & Illness, 26, 135–158. [DOI] [PubMed] [Google Scholar]
- McGowan, L. , Luker, K. , Creed, F. & Chew‐Graham, C. A. (2007). ‘How do you explain a pain that can't be seen?’: The narratives of women with chronic pelvic pain and their disengagement with the diagnostic cycle. British Journal of Health Psychology, 12, 261–274. [DOI] [PubMed] [Google Scholar]
- Murray, A. M. , Toussaint, A. , Althaus, A. & Löwe, B. (2016). The challenge of diagnosing non‐specific, functional, and somatoform disorders: A systematic review of barriers to diagnosis in primary care. Journal of Psychosomatic Research, 80, 1–10. [DOI] [PubMed] [Google Scholar]
- Müssener, U. , Festin, K. , Upmark, M. & Alexanderson, K. (2008). Positive experiences of encounters with healthcare and social insurance professionals among people on long‐term sick leave. Journal of Rehabilitation Medicine, 40, 805–811. [DOI] [PubMed] [Google Scholar]
- Nordin, T. A. , Hartz, A. J. , Noyes, R. , Anderson, M. C. , Rosenbaum, M. E. , James, P. A. et al (2006). Empirically identified goals for the management of unexplained symptoms. Family Medicine, 38, 476–482. [PubMed] [Google Scholar]
- Peters, S. , Rogers, A. , Salmon, P. , Gask, L. , Dowrick, C. , Towey, M. et al (2009). What do patients choose to tell their doctors? Qualitative analysis of potential barriers to reattributing medically unexplained symptoms. Journal of General Internal Medicine, 24, 443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rask, M. T. , Rosendal, M. , Fenger‐Grøn, M. , Bro, F. , Ørnbøl, E. & Fink, P. (2015). Sick leave and work disability in primary care patients with recent‐onset multiple medically unexplained symptoms and persistent somatoform disorders: A 10‐year follow‐up of the FIP study. General Hospital Psychiatry, 37, 53–59. [DOI] [PubMed] [Google Scholar]
- Reid, S. , Whooley, D. , Crayford, T. & Hotopf, M. (2001). Medically unexplained symptoms‐GPs’ attitudes towards their cause and management. Family Practice, 18, 519–523. [DOI] [PubMed] [Google Scholar]
- Ridgeway, C. L. (2009). Framed before we know it: How gender shapes social relations. Gender & Society, 23, 145–160. [Google Scholar]
- Risberg, G. , Johansson, E. E. & Hamberg, K. (2009).A theoretical model for analysing gender bias in medicine. International Journal for Equity in Health, 8, 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rustøen, T. , Wahl, A. K. , Hanestad, B. R. , Lerdal, A. , Paul, S. & Miaskowski, C. (2004). Prevalence and characteristics of chronic pain in the general Norwegian population. European Journal of Pain, 8, 555–565. [DOI] [PubMed] [Google Scholar]
- Salmon, P. , Ring, A. , Dowrick, C. F. & Humphris, G. M. (2005). What do general practice patients want when they present medically unexplained symptoms, and why do their doctors feel pressurized? Journal of Psychosomatic Research, 59, 255–260. [DOI] [PubMed] [Google Scholar]
- Schaefert, R. , Hausteiner‐Wiehle, C. , Häuser, W. , Ronel, J. , Herrmann, M. & Henningsen, P. (2012). Non‐specific, functional, and somatoform bodily complaints. Deutsches Ärzteblatt International, 109, 803–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattock, L. , Williamson, H. , Caldwell, K. , Anderson, K. & Peters, S. (2013). ‘They've just got symptoms without science’: Medical trainees’ acquisition of negative attitudes towards patients with medically unexplained symptoms. Patient Education and Counseling, 91, 249–254. [DOI] [PubMed] [Google Scholar]
- Socialstyrelsen . (2016). Anvisningar för diagnosklassificering i öppenvård[Diagnostic classification directives for primary care] (Report no. 2016‐5‐22). Retrieved 29 April 2019 from http://www.socialstyrelsen.se/publikationer2016/2016-5-22
- Stålnacke, B.‐M. , Haukenes, I. , Lehti, A. , Wiklund, A. F. , Wiklund, M. & Hammarström, A. (2015). Is there a gender bias in recommendations for further rehabilitation in primary care of patients with chronic pain after an interdisciplinary team assessment? Journal of Rehabilitation Medicine, 47, 365–371. [DOI] [PubMed] [Google Scholar]
- Street, R. L. Jr , Makoul, G. , Arora, N. K. & Epstein, R. M. (2009). How does communication heal? Pathways linking clinician‐patient communication to health outcomes. Patient Education and Counseling, 74, 295–301. [DOI] [PubMed] [Google Scholar]
- Tait, R. C. , Chibnall, J. T. & Kalauokalani, D. (2009). Provider judgments of patients in pain: Seeking symptom certainty. Pain Medicine, 10, 11–34. [DOI] [PubMed] [Google Scholar]
- Tait, R. C. , Chibnall, J. T. & Krause, S. (1990). The Pain Disability Index: Psychometric properties. Pain, 40, 171–182. [DOI] [PubMed] [Google Scholar]
- Taylor, B. A. , Casas‐Ganem, J. , Vaccaro, A. R. , Hilibrand, A. S. , Hanscom, B. S. & Albert, T. J. (2005). Differences in the work‐up and treatment of conditions associated with low back pain by patient gender and ethnic background. Spine, 30, 359–364. [DOI] [PubMed] [Google Scholar]
- Upmark, M. , Borg, K. & Alexanderson, K. (2007). Gender differences in experiencing negative encounters with healthcare: A study of long‐term sickness absentees. Scandinavian Journal of Public Health, 35, 577–584. [DOI] [PubMed] [Google Scholar]
- Verhaak, P. F. , Meijer, S. A. , Visser, A. P. & Wolters, G. (2006). Persistent presentation of medically unexplained symptoms in general practice. Family Practice, 23, 414–420. [DOI] [PubMed] [Google Scholar]
- Wessel, M. , Helgesson, G. , Olsson, D. , Juth, N. , Alexanderson, K. & Lynöe, N. (2012). When do patients feel wronged? Empirical study of sick‐listed patients’ experiences with healthcare encounters. The European Journal of Public Health, 23, 230–235. [DOI] [PubMed] [Google Scholar]
- Wessely, S. , Nimnuan, C. & Sharpe, M. (1999). Functional somatic syndromes: One or many? The Lancet, 354, 936–939. [DOI] [PubMed] [Google Scholar]
- Wijnhoven, H. A. , De Vet, H. C. & Picavet, H. S. J. (2006). Prevalence of musculoskeletal disorders is systematically higher in women than in men. The Clinical Journal of Pain, 22, 717–724. [DOI] [PubMed] [Google Scholar]
- Woivalin, T. , Krantz, G. , Mäntyranta, T. & Ringsberg, K. C. (2004). Medically unexplained symptoms: Perceptions of physicians in primary health care. Family Practice, 21, 199–203. [DOI] [PubMed] [Google Scholar]
- Wood, W. & Eagly, A. H. (2010). Gender In Fiske S. T., Gilbert D. T., & Lindzey G. (Eds.), Handbook of social psychology (pp. 629–667). Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- World Health Organization . (2016).International Statistical Classification of Diseases and Related Health Problems (10th rev.). Retrieved 14 May 2018 from http://www.who.int/classifications/icd/en/
- Young, G. J. , Meterko, M. & Desai, K. R. (2000). Patient satisfaction with hospital care: Effects of demographic and institutional characteristics. Medical Care, 38(5), 325–334. [DOI] [PubMed] [Google Scholar]
- Yunus, M. B. (2001). The role of gender in fibromyalgia syndrome. Current Rheumatology Reports, 3, 128–134. [DOI] [PubMed] [Google Scholar]


