Abstract
Objectives:
Any potential harm-reduction benefit of electronic cigarettes (e-cigarettes) could be offset by nonsmokers who initiate e-cigarette use and then smoke combustible cigarettes. We examined correlates of e-cigarette use at baseline with combustible cigarette smoking at 1-year follow-up among adult distant former combustible cigarette smokers (ie, quit smoking ≥5 years ago) and never smokers.
Methods:
The Population Assessment of Tobacco and Health Study, a nationally representative, longitudinal study, surveyed 26 446 US adults during 2 waves: 2013-2014 (baseline) and 2014-2015 (1-year follow-up). Participants completed an audio computer-assisted interview in English or Spanish. We compared combustible cigarette smoking at 1-year follow-up by e-cigarette use at baseline among distant former combustible cigarette smokers and never smokers.
Results:
Distant former combustible cigarette smokers who reported e-cigarette past 30-day use (9.3%) and ever use (6.7%) were significantly more likely than those who had never used e-cigarettes (1.3%) to have relapsed to current combustible cigarette smoking at follow-up (P < .001). Never smokers who reported e-cigarette past 30-day use (25.6%) and ever use (13.9%) were significantly more likely than those who had never used e-cigarettes (2.1%) to have initiated combustible cigarette smoking (P < .001). Adults who reported past 30-day e-cigarette use (7.0%) and ever e-cigarette use (1.7%) were more likely than those who had never used e-cigarettes (0.3%) to have transitioned from never smokers to current combustible cigarette smokers (P < .001). E-cigarette use predicted combustible cigarette smoking in multivariable analyses controlling for covariates.
Conclusions:
Policies and counseling should consider the increased risk for nonsmokers of future combustible cigarette smoking use as a result of using e-cigarettes and any potential harm-reduction benefits e-cigarettes might bring to current combustible cigarette smokers.
Keywords: e-cigarettes, smoking, trajectories, adults, surveillance
Use of electronic cigarettes (e-cigarettes) among adults has increased since 2010.1–3 E-cigarette use among adults rose from 0.3% in 2010 to 6.8% in 2013.2 Although some research suggests that these products may be a useful strategy for combustible cigarette cessation,4–6 other research has found that e-cigarette use reduces the likelihood of successful cessation.7–9 Some health authorities have recommended their use in cessation and efforts to end tobacco use and nicotine addiction.10–12 Others have expressed concern about their effectiveness, and emerging data show substantial health harms.13,14 A 2018 consensus study review found limited evidence that e-cigarettes may be effective aids to promote cessation of combustible cigarette smoking.15 However, any potential harm-reduction benefit of e-cigarettes to adult combustible cigarette smokers could be offset by nonsmokers initiating e-cigarette use and then transitioning to combustible cigarette use. The population health effect of e-cigarettes should also consider whether they attract users who were otherwise unlikely to be smoking combustible cigarettes.16 The features and marketing designed to make e-cigarettes more attractive to smokers than other nicotine replacement therapies are also likely to broaden their appeal to nonsmokers. In one study, at least 20% of current e-cigarette users had either never smoked or were former combustible cigarette smokers who had quit before e-cigarettes were first marketed.2
Recent (2015-2019) prospective research among adolescents and young adults indicates that e-cigarette use among never smokers is a risk factor for future combustible cigarette smoking. Numerous studies have found that e-cigarette use is associated with subsequent initiation of combustible cigarette smoking17–24 and current combustible cigarette smoking23,24 among young never smokers, after controlling for psychosocial predictors of smoking. Moreover, 3 studies found this association to be the strongest among those who were least susceptible to smoking combustible cigarettes at baseline.20,22,25 Both a 2017 meta-analysis and 2018 consensus study review of these studies found that e-cigarette use at baseline was consistently associated with a higher risk of future combustible cigarette smoking, even after controlling for multiple potential confounding factors.15,18
Most research to date on the association between e-cigarette use and future combustible cigarette smoking has focused on adolescent and young adult never smokers. Less is known about the association between e-cigarette use and future combustible cigarette smoking among adults in general, particularly adults who quit smoking before ever using e-cigarettes. Our nationally representative, prospective study examined relapse to combustible cigarette smoking among adult distant former combustible cigarette smokers (ie, had quit smoking ≥5 years ago) and initiation of smoking and transitioning to current established smoking at 1-year follow-up among adults who had never smoked a combustible cigarette, based on e-cigarette use at baseline. We addressed 2 research questions: (1) Do former smokers who used e-cigarettes at baseline have higher rates of relapsing to combustible cigarette smoking than former combustible cigarette smokers who never used e-cigarettes? and (2) Do never smokers who used e-cigarettes at baseline have higher rates of combustible cigarette initiation and current combustible cigarette smoking than never smokers who never used e-cigarettes?
Methods
The Population Assessment of Tobacco and Health (PATH) Study, a nationally representative, longitudinal study, collected data from civilian, noninstitutionalized US adults aged ≥18 from September 12, 2013, through December 14, 2014 (wave 1, baseline), and from October 23, 2014, through October 30, 2015 (wave 2, 1-year follow-up). The PATH Study recruited households by using address-based, area-probability sampling, and an in-house screener selected up to 2 adults in each household to be interviewed. During wave 1, 32 320 of 44 303 adults in participating households (weighted household screener rate, 54.0%; weighted response rate, 74.0%) participated in an audio computer-assisted interview available in English and Spanish.26,27 Sampling rates provided sufficiently large sample sizes for young adults and tobacco users.28
All wave 1 respondents were eligible for the wave 2 interview if they resided in the United States and were not incarcerated. The target period for administering wave 2 interviews was within a 4-month range of 12 months after the earliest interview was completed by a member of the household, beginning with the month before this anniversary month and ending 2 months after this month. Retention efforts for nonresponsive wave 1 participants continued until the last day of the data collection period. The weighted retention rate of wave 1 respondents (n = 32 320) for wave 2 was 83.1% (n = 26 446). Details are available elsewhere.28
We examined 2 populations of adults: (1) distant former combustible cigarette smokers who quit smoking cigarettes ≥5 years before the baseline survey and (2) never combustible cigarette smokers. Distant former combustible cigarette smokers were unlikely to have tried e-cigarettes before quitting given the limited availability of these products in the United States before 2011.2
The Westat Institutional Review Board approved the PATH Study. The PATH Study also obtained a Certificate of Confidentiality from the US Public Health Service National Institutes of Health.28
Wave 1
In wave 1, respondents were asked, “Have you ever smoked a cigarette, even 1 or 2 puffs?” Respondents who replied yes were asked, “Do you now smoke cigarettes every day, some days, or not at all?” and “How many cigarettes have you smoked in your entire life?” Then all respondents who reported having ever smoked a combustible cigarette and who no longer smoked at all were asked, “About how long has it been since you completely quit smoking cigarettes?” We defined distant former combustible cigarette smokers as adults who reported having ever smoked a combustible cigarette, having smoked ≥100 combustible cigarettes in their lifetime, no longer smoking combustible cigarettes, and having quit smoking combustible cigarettes ≥5 years before completing the survey (n = 2322). We defined never combustible cigarette smokers as adults who had never smoked a combustible cigarette, even 1 or 2 puffs (n = 5776). The PATH Study oversamples tobacco users; thus, the sample size for distant former combustible cigarette smokers and never combustible cigarette smokers was smaller than would be expected in a random sample.
All respondents were asked, “Have you ever seen or heard of an electronic cigarette or e-cigarette before this study?” Respondents who replied yes were asked, “Have you ever used an e-cigarette, such as NJOY, Blu, or Smoking Everywhere, even 1 or 2 times?” Respondents who replied yes were asked, “Do you now use e-cigarettes every day, some days, or not at all?” We categorized baseline e-cigarette use at 3 levels: never e-cigarette user, ever e-cigarette user (but no past 30-day use), and past 30-day e-cigarette user.
We included several potential confounders as covariates. Demographic variables were race/ethnicity (non-Hispanic white, non-Hispanic black, and other [Hispanic, American Indian/Alaska Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian, Native Hawaiian, Guamanian or Chamorro, Samoan, other Pacific Islander, or multiple races]), sex, age (18-34, ≥35), and education (<high school, high school/general education diploma, some college, ≥college degree). Psychosocial predictors of combustible cigarette smoking risk were having household smoking rules29–31 and living with someone who smokes combustible cigarettes.32 All respondents were asked, “For tobacco products that are burned, such as cigarettes, cigars, pipes, or hookahs, which statement best describes the rules about smoking a tobacco product inside your home?” Response options were the following: it is not allowed anywhere or at any time inside my home, it is allowed in some places or at some times inside my home, and it is allowed anywhere and at any time inside my home. We categorized adults who reported that smoking was not allowed anywhere or at any time inside the home as living in a household inside of which smoking was not allowed. Respondents who did not live alone were asked, “Does anyone who lives with you now do any of the following? [Choose all that apply.]” Response options were smoke cigarettes; use smokeless tobacco, such as chewing tobacco, snuff, dip, or SNUs; smoke cigars, cigarillos, or filtered cigars; use any other form of tobacco; or no one who lives with me now uses any form of tobacco.
Wave 2
In wave 2, all respondents were asked, “In the past 30 days, have you smoked a cigarette, even 1 or 2 puffs?” Respondents who replied no were asked, “In the past 12 months, have you smoked a cigarette, even 1 or 2 puffs?” Respondents who replied yes were asked, “Do you now smoke cigarettes every day, some days, or not at all?” Never smokers from wave 1 who reported currently smoking combustible cigarettes every day or some days were asked, “How many cigarettes have you smoked in your entire life?”
We used 2 variables to assess combustible cigarette use during wave 2. Adult “never to ever smokers” in wave 2 were adults who had never smoked combustible cigarettes before wave 1 and who reported at wave 2 that they had smoked a combustible cigarette in the past 12 months. Wave 2 “current established smokers” also reported having smoked ≥100 cigarettes and currently smoked every day or some days. Baseline distant former combustible cigarette smokers responded to the question about lifetime combustible cigarette consumption in wave 1, whereas baseline never smokers responded to this question in wave 2.
Statistical Analyses
We used SPSS version 24.0 Complex Samples33 to calculate all variance estimates, adjusted for the 92 strata and 156 primary sampling units in the sample design, and we applied the sample weights provided with the public-use data sets.34,35 (The weight variable was R02_A_PWGT.) We used the CSTABULATE command to calculate the baseline distribution of sample characteristics among distant former combustible cigarette smokers and never smokers, the association of covariates with e-cigarette use at baseline among distant former combustible cigarette smokers and never smokers, and the association of baseline e-cigarette use with combustible cigarette smoking at 1-year follow-up. We tested significance using the Pearson χ2 statistic, with P < .05 considered significant. We used the CSLOGISTIC command to calculate logistic regression estimates (crude odds ratios [ORs] and adjusted ORs) predicting combustible cigarette smoking at 1-year follow-up by baseline e-cigarette use and covariates, using 95% confidence intervals (CIs).
Of the 5776 never combustible cigarette smokers and 2332 distant former combustible cigarette smokers in wave 1, respondents were missing data for the following variables: race/ethnicity (n = 745), sex (n = 27), age (n = 5), education (n = 133), lives with a combustible cigarette smoker (n = 88), household rules about smoking combustible cigarettes (n = 109), never combustible cigarette smoker at wave 1 (n = 13), distant former combustible cigarette smoker at wave 1 (n = 25), never to ever combustible cigarette smoker at wave 2 (n = 8), and current established combustible cigarette smoker (n = 39).
Results
Baseline
Among 8108 respondents, a higher percentage of distant former combustible cigarette smokers (weighted 95.0%) than never smokers (weighted 63.7%) were aged ≥35 (Table 1).
Table 1.
Characteristics of respondents to the PATH Studya at baselineb who completed a 1-year follow-up (n = 22 997),c by smoking status, United States, 2013-2015
| Characteristic | Distant Former Combustible Cigarette Smokerd | Never Combustible Cigarette Smokere | ||
|---|---|---|---|---|
| Unweighted Sample Size, No.f | Weighted,g % (95% CI) | Unweighted Sample Size, No. | Weighted,g % (95% CI) | |
| Sex | ||||
| Male | 1374 | 54.4 (51.8-57.0) | 2363 | 40.0 (38.0-42.0) |
| Female | 946 | 45.6 (43.0-48.2) | 3402 | 60.0 (58.0-62.0) |
| Age | ||||
| 18-34 | 209 | 5.0 (4.1-6.0) | 3425 | 36.3 (34.3-38.3) |
| ≥35 | 2112 | 95.0 (94.0-95.9) | 2349 | 63.7 (61.7-65.6) |
| Race/ethnicity | ||||
| Non-Hispanic white | 1964 | 88.4 (85.9-90.5) | 3706 | 71.2 (68.0-74.3) |
| Non-Hispanic black | 176 | 6.0 (4.8-7.4) | 1206 | 15.0 (12.8-17.6) |
| Otherh | 160 | 5.6 (4.0-7.8) | 675 | 13.8 (12.0-15.7) |
| Education | ||||
| <High school | 182 | 8.1 (6.7-9.9) | 678 | 11.8 (10.4-13.3) |
| High school/GED | 498 | 29.2 (27.0-31.5) | 1617 | 28.4 (36.6-30.3) |
| Some college | 799 | 31.2 (28.8-33.7) | 1999 | 29.3 (27.6-31.0) |
| ≥College degree | 835 | 31.5 (28.9-34.2) | 1438 | 30.5 (28.4-32.7) |
| Lives with someone who smokes cigarettes | ||||
| No | 1612 | 68.2 (63.3-68.8) | 4387 | 76.2 (74.3-78.0) |
| Yes | 705 | 31.8 (31.2-36.7) | 1367 | 23.8 (22.0-25.7) |
| Smoking in the home | ||||
| Allowed | 137 | 5.0 (4.1-6.1) | 275 | 3.9 (3.4-4.6) |
| Allowed with limits | 189 | 6.8 (5.5-8.4) | 442 | 5.7 (4.9-6.7) |
| Not allowed | 1993 | 88.2 (86.5-89.8) | 5029 | 90.3 (89.2-91.4) |
Abbreviations: GED, general education diploma; PATH, Population Assessment of Tobacco and Health.
a Data source: US Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse; US Food and Drug Administration, Center for Tobacco Products.34
b Baseline was from September 13, 2013, through December 14, 2014.
c Follow-up was from October 23, 2014, through October 30, 2015.
d Defined as adults who reported having ever smoked a combustible cigarette, having smoked ≥100 combustible cigarettes in their lifetime, no longer smoking combustible cigarettes, and having quit smoking combustible cigarettes ≥5 years before completing the survey.
e Defined as adults who had never smoked a combustible cigarette, even 1 or 2 puffs.
f Numbers may not sum to totals because of missing data.
g Weights compensated for variable probabilities of selection, differential nonresponse rates, and possible deficiencies in the sampling frame.
h Hispanic, American Indian/Alaska Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian, Native Hawaiian, Guamanian or Chamorro, Samoan, other Pacific Islander, or multiple races.
Most distant former combustible cigarette smokers (95.7%; 95% CI, 95.1%-96.2%) and never smokers (98.5%; 95% CI, 98.2%-98.7%) had never tried an e-cigarette at baseline (Tables 2 and 3). Among distant former combustible cigarette smokers, adults aged 18-34 were significantly less likely to report no e-cigarette use (79.0%; 95% CI, 72.2%-84.4%) than adults aged ≥35 (96.6%; 95% CI, 96.0%-97.0%; P < .001), and adults who lived in a house where smoking was allowed were significantly less likely to report no e-cigarette use (96.1%; 95% CI, 95.6%-96.6%) than adults who lived in a house where smoking was allowed with limits (92.2%; 95% CI, 88.8%-94.7%) or where smoking was not allowed (92.6%; 95% CI, 88.2%-95.5%; P < .001). Among never combustible cigarette smokers, adults aged 18-34 were significantly less likely to report no e-cigarette use (96.5%; 95% CI, 95.8%-97.1%) than adults aged ≥35 (99.6%; 95% CI, 99.4%-99.7%; P < .001), males were less likely to report no e-cigarette use (97.8%; 95% CI, 97.3%-98.3%) than females (98.9%; 95% CI, 98.6%-99.1%; P < .001), and adults who lived in a house where smoking was allowed were more likely to report no e-cigarette use (98.8%; 95% CI, 98.5%-99.0%) than adults who lived in a house where smoking was allowed with limits (94.9%; 95% CI, 92.5%-96.6%) or where smoking was not allowed (97.3%; 95% CI, 95.3%-98.4%; P < .001).
Table 2.
Characteristics of distant former combustible cigarette smokersa (n = 2318) at baselineb of the PATH Study, by e-cigarette use, United States, 2013-2014c,d
| Characteristic | Never Tried an E-Cigarette, % (95% CI) | Tried an E-Cigarette, No Past 30-Day Use, % (95% CI) | Past 30-Day E-Cigarette Use, % (95% CI) | P Valuee |
|---|---|---|---|---|
| Overall | 95.7 (95.1-96.2) | 3.3 (2.9-3.9) | 1.0 (0.8-1.2) | —f |
| Age | <.001 | |||
| 18-34 | 79.0 (72.2-84.4) | 16.9 (12.4-22.5) | 4.2 (2.3-7.3) | |
| ≥35 | 96.6 (96.0-97.0) | 2.6 (2.2-3.2) | 0.8 (0.6-1.1) | |
| Race/ethnicity | .67 | |||
| Non-Hispanic white | 95.7 (95.1-96.3) | 3.3 (2.9-3.9) | 0.9 (0.7-1.2) | |
| Non-Hispanic black | 94.9 (91.4-97.0) | 3.4 (1.8-6.4) | 1.7 (0.7-4.1) | |
| Otherg | 95.9 (92.8-97.7) | 3.3 (1.6-6.8) | 0.7 (0.3-1.7) | |
| Sex | .35 | |||
| Male | 95.3 (94.4-96.1) | 3.6 (3.0-4.4) | 1.1 (0.8-1.4) | |
| Female | 96.1 (95.4-96.8) | 3.0 (2.4-3.8) | 0.9 (0.6-1.3) | |
| Lives with a smoker | .03 | |||
| Yes | 94.7 (93.3-95.8) | 4.0 (3.0-5.2) | 1.3 (0.9-2.0) | |
| No | 96.2 (95.6-96.6) | 3.1 (2.6-3.6) | 0.8 (0.6-1.1) | |
| Smoking in the home | .001 | |||
| Allowed | 96.1 (95.6-96.6) | 3.0 (2.5-3.5) | 0.9 (0.7-1.2) | |
| Allowed with limits | 92.2 (88.8-94.7) | 6.5 (4.3-9.8) | 1.2 (0.5-2.8) | |
| Not allowed | 92.6 (88.2-95.5) | 6.0 (3.5-10.1) | 1.4 (0.6-3.4) | |
Abbreviations: e-cigarette, electronic cigarette; PATH, Population Assessment of Tobacco and Health.
a Defined as adults who reported having ever smoked a combustible cigarette, having smoked ≥100 combustible cigarettes in their lifetime, no longer smoking combustible cigarettes, and having quit smoking combustible cigarettes ≥5 years before completing the survey.
b Baseline was from September 13, 2013, through December 14, 2014.
c Data source: US Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse; US Food and Drug Administration, Center for Tobacco Products.34
d Any “don’t know” or “refused to answer” categories were excluded.
e P values derived by using the Pearson χ2 test of equal proportions. P < .05 was considered significant.
f No statistical test or P value for the overall percentages.
g Hispanic, American Indian/Alaska Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian, Native Hawaiian, Guamanian or Chamorro, Samoan, other Pacific Islander, or multiple races.
Table 3.
Characteristics of never smokersa at baseline,b by e-cigarette use, PATH Study (n = 5762), United States, 2013-2014c,d
| Characteristic | Never Tried an E-Cigarette, % (95% CI) | Has Tried an E-Cigarette, No Past 30-Day Use, % (95% CI) | Past 30-Day E-Cigarette Use, % (95% CI) | P Valuee |
|---|---|---|---|---|
| Overall | 98.5 (98.2-98.7) | 1.1 (0.9-1.3) | 0.4 (0.3-0.6) | —f |
| Age | <.001 | |||
| 18-34 | 96.5 (95.8-97.1) | 2.4 (1.9-2.9) | 1.1 (0.8-1.5) | |
| ≥35 | 99.6 (99.4-99.7) | 0.3 (0.2-0.5) | 0.1 (0.0-0.2) | |
| Race/ethnicity | .61 | |||
| Non-Hispanic white | 98.5 (98.2-98.8) | 1.0 (0.8-1.3) | 0.4 (0.3-0.6) | |
| Non-Hispanic black | 98.5 (97.9-98.9) | 1.2 (0.8-1.8) | 0.3 (0.2-0.5) | |
| Otherg | 98.3 (97.5-99.9) | 1.0 (0.6-1.8) | 0.6 (0.3-1.2) | |
| Sex | <.001 | |||
| Male | 97.8 (97.3-98.3) | 1.5 (1.1-1.9) | 0.7 (0.5-1.0) | |
| Female | 98.9 (98.6-99.1) | 0.8 (0.7-1.0) | 0.3 (0.2-0.4) | |
| Lives with a smoker | .001 | |||
| Yes | 97.9 (97.3-98.4) | 1.4 (1.0-1.8) | 0.7 (0.5-1.2) | |
| No | 98.7 (98.4-98.9) | 1.0 (0.8-1.2) | 0.3 (0.3-0.5) | |
| Smoking in home | <.001 | |||
| Allowed | 98.8 (98.5-99.0) | 0.9 (0.7-1.1) | 0.3 (0.2-0.4) | |
| Allowed with limits | 94.9 (92.5-96.6) | 3.0 (1.8-5.0) | 2.1 (1.2-3.7) | |
| Not allowed | 97.3 (95.3-98.4) | 1.8 (0.9-3.7) | 0.9 (0.4-2.0) | |
Abbreviation: PATH, Population Assessment of Tobacco and Health.
a Defined as adults who had never smoked a combustible cigarette, even 1 or 2 puffs.
b Baseline was from September 13, 2013, through December 14, 2014.
c Data source: US Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse; US Food and Drug Administration, Center for Tobacco Products.34
d Any “don’t know” or “refused to answer” categories were excluded.
e P values were from the Pearson χ2 test of equal proportions. P < .05 was considered significant.
f No statistical test or P value for the overall percentages.
g Hispanic, American Indian/Alaska Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian, Native Hawaiian, Guamanian or Chamorro, Samoan, other Pacific Islander, or multiple races.
One-Year Follow-Up
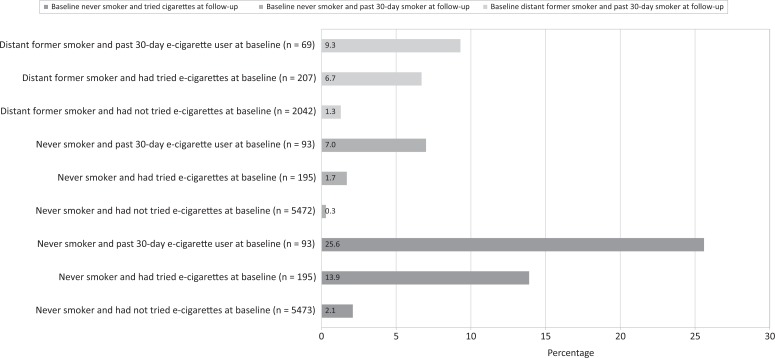
Ever and distant former combustible cigarette smokers who had tried e-cigarettes or reported past 30-day e-cigarette use were at significantly higher risk of combustible cigarette use at 1-year follow-up than at baseline (Figure). Among distant former combustible cigarette smokers, past 30-day e-cigarette users (9.3%; 95% CI, 4.0%-20.3%) and ever e-cigarette users (6.7%; 95% CI, 4.0%-11.1%) were significantly more likely than those who had never used e-cigarettes (1.3%; 95% CI, 1.0%-1.8%) to have relapsed to past 30-day smoking (P < .001). Among never smokers, past 30-day e-cigarette users (25.6%; 95% CI, 17.8%-35.2%) and ever e-cigarette users (13.9%; 95% CI, 10.5%-18.2%) were significantly more likely than those who had never used e-cigarettes (2.1%; 95% CI, 1.7%-2.5%) to have transitioned from never to ever combustible cigarette smokers (P < .001). E-cigarette use at baseline among never smokers also predicted an increased risk of becoming an established smoker (P < .001).
Figure.
Three cross-tabulations predicting cigarette smoking among adults aged ≥18 from wave 1 of the Population Assessment of Tobacco and Health (PATH) Study (2013-2014) who responded in wave 2 of the PATH Study (2014-2015), United States. Any “don’t know” or “refused to answer” categories were excluded. P values are from the Pearson χ2 test of equal proportions. Baseline e-cigarette use predicted combustible cigarette smoking at 1-year follow-up among distant former combustible cigarette smokers (who had quit ≥5 years before baseline), ever use of combustible cigarettes at 1-year follow-up among never smokers (adults who had never tried a combustible cigarette) at baseline, and past 30-day combustible cigarette smoking at 1-year follow-up among never smokers (adults who had never tried a combustible cigarette, not even 1 or 2 puffs; P < .001).
In adjusted multivariable models, distant former combustible cigarette smokers who had ever tried an e-cigarette (OR = 3.3; 95% CI, 1.6-6.7) and those who reported past 30-day e-cigarette use (OR = 5.2; 95% CI, 1.6-16.3) were significantly more likely than those who had never used e-cigarettes to have relapsed to past 30-day combustible cigarette smoking. Younger adults were more likely than older adults (OR = 4.0; 95% CI, 1.7-9.6), and adults who lived in homes with partial smoking bans were more likely than adults in smoke-free homes (OR = 4.0; 95% CI, 1.7-9.6), to relapse to smoking combustible cigarettes (Table 4).
Table 4.
Predicted odds of combustible cigarette smoking at 1-year follow-up,a by baselineb e-cigarette use, covariates, and smoker type, PATH Study, United States, 2013-2015c
| Cigarette Use | Distant Former Combustible Cigarette Smokerd at Baseline and Relapsed to Established Combustible Cigarette Smokere at Follow-up, OR (95% CI) (n = 2318) | Never Cigarette Smokerf at Baseline, OR (95% CI) (n = 5762) | |
|---|---|---|---|
| Initiated Combustible Cigarette Smokingg at Follow-up | Established Combustible Cigarette Smoker at Follow-up | ||
| Unadjusted model | |||
| E-cigarette use | |||
| Never tried an e-cigarette | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| Has tried an e-cigarette, no past 30-day use | 5.4 (2.9-10.2)h | 7.7 (5.4-11.0)h | 5.9 (1.7-20.7)h |
| Past 30-day e-cigarette use | 7.6 (3.0-19.4)h | 16.4 (9.8-27.5)h | 25.5 (10.6-61.4)h |
| Adjusted modeli | |||
| E-cigarette use | |||
| Never tried an e-cigarette | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| Has tried an e-cigarette, no past 30-day use | 3.3 (1.6-6.7)h | 4.0 (2.6-6.1)h | 2.5 (0.6-10.9) |
| Past 30-day e-cigarette use | 5.2 (1.6-16.3)h | 6.6 (3.7-11.8)h | 8.0 (2.8-22.7)h |
| Lives with someone who smokes cigarettes | |||
| No | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| Yes | 1.1 (0.6-2.0) | 1.5 (0.9-2.4) | 3.7 (1.6-9.0) |
| Smoking in the home | |||
| Not allowed | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| Allowed | 2.6 (0.8-8.7) | 2.0 (1.1-3.3)h | 1.8 (0.7-4.5) |
| Allowed with limits | 3.3 (1.4-7.3)h | 2.2 (1.2-4.1)h | 2.5 (0.7-9.5) |
| Age | |||
| ≥35 | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| 18-34 | 4.0 (1.7-9.6)h | 4.4 (2.8-6.9)h | 3.8 (1.1-13.2)h |
| Sex | |||
| Female | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| Male | 1.3 (0.6-2.7) | 2.1 (1.5-3.0)h | 1.8 (0.6-4.9) |
| Race/ethnicity | |||
| Non-Hispanic white | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| Non-Hispanic black | 3.1 (1.3-7.3)h | 1.2 (0.8-1.8) | 0.4 (0.1-1.3) |
| Otherj | 0.8 (0.2-3.2) | 0.9 (0.5-1.6) | 0.7 (0.3-1.8) |
Abbreviations: aOR, adjusted odds ratio; OR, odds ratio; PATH, Population Assessment of Tobacco and Health.
a Follow-up was from October 23, 2014, through October 30, 2015.
b Baseline was from September 13, 2013, through December 14, 2014.
c Data source: US Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse; US Food and Drug Administration, Center for Tobacco Products.34
d Defined as adults who reported having ever smoked a combustible cigarette, having smoked ≥100 combustible cigarettes in their lifetime, no longer smoking combustible cigarettes, and having quit smoking combustible cigarettes ≥5 years before completing the survey.
e Defined as adults who had never smoked a combustible cigarette, even 1 or 2 puffs.
f Defined as adults who reported having smoked ≥100 combustible cigarettes and currently smoked every day or some days.
g Adults who had never smoked combustible cigarettes before wave 1 and who reported that they had ever smoked at wave 2.
h Significant at P < .05.
i Adjusted for race/ethnicity, sex, age, education, household smoking rules, and living with someone who smokes cigarettes.
j Hispanic, American Indian/Alaska Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian, Native Hawaiian, Guamanian or Chamorro, Samoan, other Pacific Islander, or multiple races.
In multivariable analyses, never combustible cigarette smokers who reported ever trying e-cigarettes at baseline were 4 times as likely to have transitioned to ever combustible cigarette smokers than never smokers who had never used e-cigarettes (OR = 4.0; 95% CI, 2.6-6.1); however, these experimenters were no more likely than adults who had never tried e-cigarettes to become established smokers (OR = 2.5; 95% CI, 0.6-10.9; Table 4). Past 30-day e-cigarette users at baseline were more than 6 times as likely to have transitioned from never to ever combustible cigarette smokers (OR = 6.6; 95% CI, 3.7-11.8) and 8 times more likely to have become established combustible cigarette smokers (OR = 8.0; 95% CI, 2.8-22.7) than those who had never used e-cigarettes. Age and household smoking rules were also associated with increased risk for never smokers transitioning to combustible cigarette smoking.
Discussion
The higher risk of future combustible cigarette smoking among adolescent and young adult e-cigarette users compared with nonusers is well-established.15,18 Our study extends this finding to adult never smokers and distant former combustible cigarette smokers. As previous studies have suggested, several possible mechanisms relate ever-use and past 30-day use of e-cigarettes to subsequent combustible cigarette smoking. First, susceptible nonsmokers may simply use e-cigarettes before they try combustible cigarettes and, therefore, may try combustible cigarettes even if e-cigarettes did not exist.25 However, 3 studies found that these associations were higher among less susceptible nonsmokers than among more susceptible nonsmokers at baseline.20,22,25 Second, the use of e-cigarettes could facilitate the transition to smoking through the development of cognitive or behavioral processes for combustible cigarette smoking.18 Third, e-cigarette use could normalize nicotine use25,34,35 and initiate nicotine dependence.18,25,35,36 Fourth, e-cigarette use could potentially desensitize the lungs to harsh or adverse effects of nicotine inhalation.20
To our knowledge, our study is the first to examine the risk of e-cigarette use on relapse among distant former combustible cigarette smokers and initiation of combustible cigarette smoking among never smokers in a representative sample of US adults. Our findings from an adult population are consistent with previous studies demonstrating an increased risk of combustible cigarette smoking initiation among adolescents and young adults.17–24
Strengths and Limitations
This study had several strengths and limitations. One strength was that the data were prospective, which provided confidence that e-cigarette trial and past 30-day use occurred before the use of combustible cigarettes. A second strength was the short time interval between wave 1 and wave 2, which precluded the likelihood that external events confounded the association between e-cigarette use and future smoking.18 Finally, given that almost 90% of combustible cigarette smokers have tried smoking before their 18th birthday,37 it is unlikely that the adult e-cigarette users in the PATH study who became ever smokers and current smokers were simply susceptible never smokers and would have become smokers in the absence of e-cigarette use.
This study also had several limitations. First, the number of never smokers and distant former combustible cigarette smokers who reported past 30-day e-cigarette use at baseline was small. However, the ability to detect a significant association of baseline e-cigarette use and combustible cigarette smoking at follow-up with a small subsample suggests that the signal was strong. The small subsample also prevented us from appraising the incremental risk of various daily usage patterns of e-cigarettes at baseline on future combustible cigarette use. Second, self-report of e-cigarette use and combustible cigarette use was not biologically verified in the currently available public-use PATH Study sample; thus, we may have underrepresented or overrepresented the true rates of product use. Third, the timing of the baseline survey administration in 2013-2014 might have captured the effects of early types of e-cigarettes, and these products may differ from products that were developed later.18,25 Current e-cigarettes that more effectively deliver nicotine to the brain might lead to different trajectories of nicotine-product use than e-cigarettes that were on the market in 2013-2014. Fourth, the sample of baseline e-cigarette users across age groups was not sufficient to test for an interaction between age and e-cigarette and future combustible cigarette smoking. Finally, the PATH Study collected data on a broad range of demographic characteristics, but it did not collect data on all the psychosocial and behavioral covariates that have been associated with tobacco use in other studies. As such, this study was not able to address additional psychosocial confounders that may have existed.
Conclusions
This study provides longitudinal data from the first 2 waves of a nationally representative sample demonstrating that e-cigarette use precedes and predicts future combustible cigarette smoking and also demonstrates that distant former combustible cigarette smokers who use e-cigarettes, particularly young adults, are more likely to relapse than distant former combustible cigarette smokers who do not use e-cigarettes. Policies and clinical counseling must consider the public health harm that these products place on nonsmokers, in addition to any potential harm-reduction benefits that might accrue to current combustible cigarette smokers.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This article was made possible by the Flight Attendant Medical Research Institute under award No. 052302_CoE to the American Academy of Pediatrics. The information, views, and opinions contained herein are those of the authors and do not necessarily reflect the views and opinions of the funding organizations.
ORCID iD: Robert McMillen, PhD  https://orcid.org/0000-0001-8145-9275
https://orcid.org/0000-0001-8145-9275
References
- 1. King BA, Patel R, Nguyen KH, Dube SR. Trends in awareness and use of electronic cigarettes among U.S. adults, 2010-2013. Nicotine Tob Res. 2015;17(2):219–227. doi:10.1093/ntr/ntu191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McMillen RC, Gottlieb MA, Shaefer RM, Winickoff JP, Klein JD. Trends in electronic cigarette use among U.S. adults: use is increasing in both smokers and nonsmokers. Tob Control. 2015;17(10):1195–1202. doi:10.1093/ntr/ntu213 [DOI] [PubMed] [Google Scholar]
- 3. Filippidis FT, Laverty AA, Gerovasili V, Vardavas CI. Two-year trends and predictors of e-cigarette use in 27 European Union member states. Tob Control. 2017;26(1):98–104. doi:10.1136/tobaccocontrol-2015-052771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brown J, Beard E, Kotz D, Michie S, West R. Real-world effectiveness of e-cigarettes when used to aid smoking cessation: a cross-sectional population study. Addiction. 2014;109(9):1531–1540. doi:10.1111/add.12623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bullen C, Howe C, Laugesen M. et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–1637. doi:10.1016/S0140-6736(13)61842-5 [DOI] [PubMed] [Google Scholar]
- 6. Zhu SH, Zhuang YL, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US Current Population Surveys. BMJ. 2017;358:j3262 doi:10.1136/bmj.j3262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Intern Med. 2014;174(5):812–813. doi:10.1001/jamainternmed.2014.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Popova L, Ling PM. Alternative tobacco product use and smoking cessation: a national study. Am J Public Health. 2013;103(5):923–930. doi:10.2105/AJPH.2012.301070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vickerman KA, Carpenter KM, Altman T, Nash CM, Zbikowski SM. Use of electronic cigarettes among state tobacco cessation quitline callers. Nicotine Tob Res. 2013;15(10):1787–1791. doi:10.1093/ntr/ntt061 [DOI] [PubMed] [Google Scholar]
- 10. Sweanor D. Public health and electronic cigarettes. Can J Respir Ther. 2014;50(2):41–42. [PMC free article] [PubMed] [Google Scholar]
- 11. Levy DT, Borland R, Lindblom EN. et al. Potential deaths averted in USA by replacing cigarettes with e-cigarettes. Tob Control. 2018;27(1):18–25. doi:10.1136/tobaccocontrol-2017-053759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fairchild AL, Bayer R, Colgrove J. The renormalization of smoking? E-cigarettes and the tobacco “endgame” [published correction appears in N Engl J Med. 2014;370(24):2354]. N Engl J Med. 2014;370(4):293–295. doi:10.1056/NEJMp1313940 [DOI] [PubMed] [Google Scholar]
- 13. Behar RZ, Wang Y, Talbot P. Comparing the cytotoxicity of electronic cigarette fluids, aerosols and solvents. Tob Control. 2018;27(3):325–333. doi:10.1136/tobaccocontrol-2016-053472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zawertailo L, Pavlov D, Ivanova A, Ng G, Baliunas D, Selby P. Concurrent e-cigarette use during tobacco dependence treatment in primary care settings: association with smoking cessation at three and six months. Nicotine Tob Res. 2017;19(2):183–189. doi:10.1093/ntr/ntw218 [DOI] [PubMed] [Google Scholar]
- 15. National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes. Washington, DC: National Academies Press; 2018. [PubMed] [Google Scholar]
- 16. Kalkhoran A, Glantz SA. Modeling the health impact of expanding e-cigarettes sales in the United States and United Kingdom: a Monte Carlo analysis. JAMA Intern Med. 2015; 175(10):1671–1680. doi:10.1001/jamainternmed.2015.4209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Miech R, Patrick ME, O’Malley PM, Johnston LD. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob Control. 2017;26(e2):e106–e111. doi:10.1136/tobaccocontrol-2016-153291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Soneji S, Barrington-Trimis JL, Wills TA. et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–797. doi:10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Spindle TR, Hiler MM, Cooke ME, Eissenberg T, Kendler KS, Dick DM. Electronic cigarette use and uptake of cigarette smoking: a longitudinal examination of U.S. college students. Addict Behav. 2016;67:66–72. doi:10.1016/j.addbeh.2016.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barrington-Trimis JL, Urman R, Berhane K. et al. E-cigarettes and future cigarette use. Pediatrics. 2016;138(1):pii:e20160379 doi:10.1542/peds.2016-0379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatr. 2015;169(11):1018–1023. doi:10.1001/jamapediatrics.2015.1742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Leventhal AM, Strong DR, Kirkpatrick MG. et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700–707. doi:10.1001/jama.2015.8950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Unger JB, Soto DW, Leventhal A. E-cigarette use and subsequent cigarette and marijuana use among Hispanic young adults. Drug Alcohol Depend. 2016;163:261–264. doi:10.1016/j.drugalcdep.2016.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hornik R, Gibson L. Evidence for a plateau in the use of e-cigarettes since mid-2014: comparisons with combustible cigarette use: time series results from a nationally representative survey of 13-25 year olds. Poster presented at the Annual Meeting of the Society for Research on Nicotine & Tobacco, March 2016, Chicago, IL. [Google Scholar]
- 25. Conner M, Grogan S, Simms-Ellis R. et al. Do electronic cigarettes increase cigarette smoking in UK adolescents? Evidence from a 12-month prospective study [published online August 17, 2017]. Tob Control. doi:10.1136/tobaccocontrol-2016-053539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ambrose BK, Day HR, Rostron B. et al. Flavored tobacco product use among US youth aged 12-17 years, 2013-2014. JAMA. 2015;314(17):1871–1873. doi:10.1001/jama.2015.13802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kasza KA, Ambrose BK, Conway KP. et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N Engl J Med. 2017;376(4):342–353. doi:10.1056/NEJMsa1607538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. US Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse, US Food and Drug Administration, Center for Tobacco Products. Population Assessment of Tobacco and Health (PATH) Study [United States] public-use files (ICPSR 36498). September 28, 2018 https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/36498. Accessed April 23, 2019.
- 29. Conley Thomson C, Siegel M, Winickoff J, Biener L, Rigotti NA. Household smoking bans and adolescents’ perceived prevalence of smoking and social acceptability of smoking. Prev Med. 2005;41(2):349–356. doi:10.1016/j.ypmed.2004.12.003 [DOI] [PubMed] [Google Scholar]
- 30. Farkas AJ, Gilpin EA, Distefan JM, Pierce JP. The effects of household and workplace smoking restrictions on quitting behaviours. Tob Control. 1999;8(3):261–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pizacani BA, Martin DP, Stark MJ, Koepsell TD, Thompson B, Diehr P. A prospective study of household smoking bans and subsequent cessation related behaviour: the role of stage of change. Tob Control. 2004;13(1):23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tyas SL, Pedderson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control. 1998;7(4):409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. SPSS Statistics for Macintosh, Version 24.0. Armonk, NY: IBM Corp; 2016. [Google Scholar]
- 34. US Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse; US Food and Drug Administration, Center for Tobacco Products. Population Assessment of Tobacco and Health (PATH) Study [United States] Biomarker Restricted-Use Files. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2019. [Google Scholar]
- 35. Wills TA, Sargent JD, Knight R, Pagano I, Gibbons FX. E-cigarette use and willingness to smoke: a sample of adolescent non-smokers. Tob Control. 2016;25(e1):e52–e59. doi:10.1136/tobaccocontrol-2015-052349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wills TA. E-cigarettes and adolescents’ risk status. Pediatrics. 2017;139(2). doi:10.1542/peds.2016-3736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, US Public Health Service, Office of the Surgeon General; 2014. [Google Scholar]