Abstract
Background
Hidradenitis suppurativa (HS) is a chronic debilitating skin disease, frequently located in the groin and anogenital area, leading to a substantial impact on quality of life and sexual health in patients with HS. Skin‐tissue‐sparing excision with electrosurgical peeling (STEEP) is a procedure with known low recurrence rates and high patient satisfaction in retrospective series. However, a prospective study to investigate the impact of any major surgery on specific aspects of the quality of life has not yet been performed.
Objective
To assess surgical outcomes and the effect of major surgery on the general quality of life, sexual health and activity impairment in patients with HS.
Materials and methods
A single centre prospective survey study was conducted among 40 patients undergoing major surgery. Surveys were completed prior to the surgery and 2, 6, 12 and 26 weeks after surgery. Besides the objective parameters (time to wound closure and surface of the wound), patient‐reported outcomes were reported.
Results
Thirty‐nine patients with a total of 171 survey responses were included for analysis. Patients with Hurley stage I or II had a shorter time to wound closure (TTWC) compared to patients with Hurley stage III (P = 0.005). TTWC was significantly prolonged in patients treated with biologics (P < 0.001). Smoking did not significantly influence TTWC. For patient‐reported outcomes, DLQI and ASEX scores did not significantly improve during the study period of 6 months. However, activity and overall work impairment showed considerable improvement after surgery.
Conclusion
Time to wound closure is significantly prolonged by higher Hurley stage and treatment with biologics, contrastingly not by smoking. Major surgery improved the overall work and daily activity impairment.
Introduction
Hidradenitis suppurativa (HS) is a chronic debilitating skin disease with an estimated prevalence of 1% in the general population.1, 2 Recurrent painful nodules and abscesses, subsequently leading to formation of sinus tracts and scarring, are the main features.1 Since the disease is frequently located in the groin and anogenital area, patients suffering from HS experience an substantial impact on quality of life and sexual health.3, 4 Surgical interventions play a key role in the treatment of chronic HS.5, 6, 7 By excising the affected, painful skin, local disease control can be achieved. As described by Blok et al.,8 skin‐tissue‐sparing excision with electrosurgical peeling (STEEP) is a procedure with low recurrence rates and high patient satisfaction. This procedure is comparable to a wide excision, with the primary aim to maximally spare healthy tissue. This is achieved by performing successive tangential excisions of affected tissue until an epithelialized bottom of a sinus tract is reached. Any fibrotic tissue will be removed in the same manner.8 So far, prospective studies to investigate the effect of major surgery on aspects of the quality of life have not been done in patients with HS. Therefore, we sought to assess the impact of surgery on the general quality of life of patients with HS and, more specific, on sexual health and activity impairment. Additionally, surgical outcomes, such as time to wound closure, were also assessed.
Material and methods
Study design and subjects
A prospective, survey‐based study was conducted at the University Medical Center Groningen from January 2016 through December 2017. Consecutive patients with a diagnosis of HS, who underwent major surgery under general anaesthesia, were included. Informed consent was obtained from each patient. Adequate knowledge of the Dutch language was mandatory, since the survey was only available in Dutch. The survey consisted of thirty‐five questions and was completed online by the patients using a web‐based survey tool (Qualtrics 2018, Provo, Utah), prior to the surgery and 2, 6, 12 and 26 weeks after surgery. If extra visits outside scheduled timeframes occurred, the number of postoperative days was registered instead. At the last study visit, the patients’ electronic file was analysed for objective surgical outcome measures. One year after the last patient’s study visit, all records were screened for disease relapses in the operated area.
The local medical ethical committee from UMCG granted exemption from reviewing our protocol as the treatment was considered standard of care.
Outcome measures
Patients’ characteristics
From all patients, gender, age, body mass index, smoking status and the refined Hurley classification were registered.
Surgical outcomes
For all participants, the following surgery‐related objective outcomes were assessed: time to wound closure (TTWC) in days, size of the wound in cm2, location of the surgical site, relapse rate, complications and the use of a biological around the time of surgery. A relapse was defined as recurrence of an inflammatory lesion within 5 mm of the operated area.
Patient‐reported outcome measures (PROMs)
The DLQI is a widely used tool to assess quality of life consisting of ten questions with a minimum score of 0, no impact on quality of life and maximum score of 30, meaning a maximum impact on quality of life.9 The WPAI questionnaire was adjusted for HS (WPAI‐HS). Outcomes are expressed as impairment percentages for the following categories: per cent work time missed due to HS; per cent impairment while working due to HS; per cent overall work impairment due to health; and per cent activity impairment due to HS. Higher percentages indicate a greater impairment.10, 11
The ASEX assesses sexual dysfunction through five questions, specified per sex. A total score of 19 or higher, or any single item with a score of 5 or higher or any three items with a score of 4 or higher indicates sexual dysfunction for both men and women.12 For the pain assessment, the numeric rating scale (NRS) for pain was used. Patients were asked to score their pain at that moment from 0 to 10, with 0 indicating no pain and 10 the worst possible pain.
Statistics
All continuous outcomes were described as mean ± SD. The WPAI outcomes are presented as percentages. In case of missing values in the DLQI, WPAI or ASEX, the total scores were not calculated. The patient‐reported outcomes with repeated measures and with a normal distribution analyses were performed using linear mixed models. The surgical outcomes were analysed with descriptive statistics, linear regressions and independent t‐tests, depending on the variables. A P < 0.05 was considered significant. Statistical analysis was performed using IBM SPSS Statistics version 23.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Patients’ characteristics
A total of 40 patients were included; from them, 175 survey responses were received. One participant withdrew from the study before undergoing surgery. Three responses were excluded from analysis because a correct study identification number was missing from the survey. For analysis, 171 responses from 39 participants were included.
Participants had a mean age of 39.5 ± 11.1 years, and the majority of respondents was female (87.2%). Almost 75% of the participants had a refined Hurley stage of IIB or higher.13 The mean body mass index for both genders was 29.0 ± 5.5 kg/m2. An overview of the baseline characteristics is shown in Table 1.
Table 1.
Patient characteristics
| N = 39 | |
|---|---|
| Age (years ± SD) | 39.5 ± 11.1 |
| Gender | |
| Male (%) | 5 (13%) |
| Female (%) | 34 (87%) |
| Body mass index (kg/m2) | 29.0 ± 5.5 |
| Smoking status | |
| Current or ex‐smoker | 30 (76.9%) |
| Hurley stage distribution | |
| IA | 2 (10.3%) |
| IB | 2 (10.3%) |
| IIA | 6 (15.4%) |
| IIB | 21 (53.8%) |
| IIC | 4 (10.3%) |
| III | 4 (10.3%) |
| Biologics use | 5 (13%) |
Surgical outcomes
An overview of the surgical outcomes is shown in Tables 2 and 3. The majority of subjects (69.2%) underwent surgery of the groin or anogenital area. The approximated surface of the wound directly postsurgery varied from 6 to 450 cm2 with a mean of 74.0 ± 86.8 cm2. TTWC was on average 81.3 ± 48.9 days for all subjects. In our study, the variables age, gender, BMI and smoking status were not related to TTWC. We additionally compared patients with a healthy BMI (≤25) to patients with a BMI >25 and found no difference in TTWC (P = 0.230) with a comparable mean wound surface between these groups.
Table 2.
Frequencies surgical sites
| Surgical site | N (%) |
|---|---|
| Armpit | 12 (30.8) |
| Groin | 22 (56.4) |
| Labia/scrotum | 2 (5.2) |
| Other | 3 (7.7) |
| Total | 39 (100) |
Table 3.
Surgical outcomes
| N * | Mean wound surface (cm2) ± SD | P | Mean TTWC (days) ± SD | P | |
|---|---|---|---|---|---|
| TTWC | 35 | 81.3 ± 48.9 | |||
| Wound surface | 38 | 74.0 ± 86.8 | 0.002† | ||
| Biologics | |||||
| Yes | 4 | 118.8 ± 86.8 | 0.282‡ | 185 ± 25.4 | <0.0001‡ |
| No | 34 | 68.8 ± 86.4 | 67.9 ± 32.1 | ||
| Smoking | |||||
| Yes | 26/24 | 67.9 ± 65.9 | 0.531‡ | 68.5 ± 34.4 | 0.070‡ |
| No | 12 | 87.3 ± 123.2 | 109.4 ± 64.5 | ||
| Hurley stage | |||||
| I | 4/3 | 18.8 ± 14.4 | 0.046§ | 34.7 ± 6.4 | 0.031§ |
| II | 30/28 | 58.6 ± 53.9 | 0.072§ | 75.8 ± 37.6 | 0.001§ |
| III | 4 | 245 ± 138.2 | 155 ± 68.2 | ||
| BMI | 39 | 0.102† | |||
| ≤25 | 9/10 | 42.4 ± 62.1 | 0.216‡ | 68.6 ± 30.4 | 0.230‡ |
| >25 | 29/25 | 83.8 ± 91.8 | 86.4 ± 54.3 | ||
Number of patients with data available per outcome.
Regression analysis with outcome variable TTWC.
Independent samples t‐test.
Independent samples t‐test with Hurley I and Hurley II being compared with the Hurley III group.
The Hurley stage of the patient was of significant influence on the TTWC (P = 0.005). Subjects with Hurley stage I or II had a significant shorter TTWC (34.7 ± 6.4; P = 0.031 and 75.8 ± 37.6 days; P = 0.001 respectively), compared to subjects with Hurley stage III with an average TTWC of 155 ± 68.2 days. However, the average surface of the wound in subjects with Hurley III was significantly greater than subjects with Hurley I (P = 0.046), but comparable between Hurley II and Hurley III (P = 0.072). There was a significant relationship found between the surface of the wound and TTWC (P = 0.002), a larger the wound surface corresponded with a longer TTWC.
In our study, five patients were treated with biologics. An overview of their characteristics can be found in Table 4. Patients were started on biologics due to severe HS or presence of another inflammatory disease, i.e., psoriasis (patient 9) and Crohn’s disease (patient 28). Four patients started biologic treatment at least 3 months prior to the surgery, and the other patient started within 2 months after surgery. Four patients received adalimumab 40 mg weekly and one infliximab 500 mg every 6 weeks. Administration of adalimumab was withheld in all patients in the week of their surgery, and infliximab was administered 2 weeks after surgery. Data on wound closure were available from four patients. They showed a prolonged TTWC with a mean of 185 ± 25.4 days, compared with 68 ± 32.1 days for participants without biologic treatment (P < 0.001). Wound surface was comparable for the biologic and non‐biologic treated participants (P = 0.282). Using the chi‐square test (Fisher’s exact test), no differences were found in smoking status for the biologic and non‐biologic group (P = 0.082). No relapses were reported for these five patients, with a mean follow‐up period of 17 months. At this point, two patients discontinued their treatment and three had no change of treatment.
Table 4.
Characteristics of patients with biologic treatment
| Patient ID | Gender | Age (years) | Body mass index kg/m2 | Current smoker (Yes/No) | Refined Hurley stage | Biologic regimen | Started before/after surgery | Number of treatment weeks before surgery | Treatment ongoing at end of study? (week 26) | Relapse (Yes/No) |
|---|---|---|---|---|---|---|---|---|---|---|
| 6 | F | 51 | 36.7 | No* | III | Adalimumab 40 mg QW | Before | 14 | Yes | No |
| 9 | F | 34 | 28.7 | No* | IIB | Adalimumab 40 mg QW | Before | 13 | Yes | No |
| 24 | M | 26 | 33.0 | Yes† | III | Infliximab 500mg E6W | Before | 184§ | Yes | No |
| 28 | F | 44 | 25.7 | Yes | IIB | Adalimumab 40 mg QW | Before | 221 | Yes | No |
| 39 | F | 50 | 32.2 | No‡ | III | Adalimumab 40 mg QW | After | −7¶ | Yes | No |
Former smoker.
Smokes fruit tobacco.
Never smoked.
Estimation: no exact start date was reported.
Biologic treatment started 7 weeks after surgery.
The overall relapse rate was 23.7% with a mean follow‐up period of 12 months. Pain after surgery was reported in 38.5% of the participants. Complications occurred in 25.6% of all subjects. These included bleeding or hypergranulation of the wound, which accounted for 90% of all complications. No postoperative infections were reported.
Patient‐reported outcomes
In all patient‐reported outcomes, a higher score was related to more burden or impact. A decrease in the score is therefore a positive outcome. Overviews of the mean scores of the DLQI, WPAI‐HS and ASEX during the study are shown in Fig. 1a–c.
Figure 1.
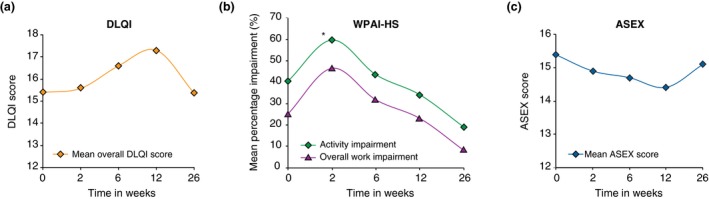
(a) Mean overall DLQI score. (b) Mean overall WPAI‐HS‐scores. *Significant increase in activity impairment at week 2 (P = 0.039). (c) Mean ASEX score.
Dermatology life quality index (DLQI)
The mean DLQI score at baseline was 15.3 ± 6.7 points, equal for men and women (P = 0.909). When comparing the DLQI scores for each time point to baseline, no significant differences were found. Instead of comparing the scores for each individual time point, we also analysed the trend over time. This showed slightly increasing DLQI scores in the first 3 months after surgery to 17.3, which then decreased steadily to 15.4 at 6 months. There was a significant difference in mean DLQI scores between time points (P = 0.047). The nature of this mixed model trend analysis does not specify between which exact time points, this significant difference is present. Both age and gender did not influence the mean DLQI score (P = 0.117 and P = 0.882, respectively). A similar trend for DLQI scores was found when patients with a relapse were excluded.
Work productivity and activity impairment questionnaire: WPAI‐HS
Activity impairment
At baseline, subjects reported an average impairment on daily activities of 40.4%, with no differences between men and women. Two weeks postsurgery, this increased significantly to 59.7% (P = 0.039) but decreased steadily to 18.8% at 6 months (P = 0.104), when comparing each time point individually to baseline. Analysis for trend showed no influence from age or gender on activity impairment.
Overall work impairment
On average, the overall work impairment at baseline was 25.0%, equal for both genders. Similar to the activity impairment, in the first 2 weeks after surgery there was an increase in overall work impairment to 46.4%. In the next 4 weeks, that score decreased to 31.6% and this continued to ultimately 7.9% at 6 months, however not significant. Analysis for trend showed no influence from age or gender on overall work impairment.
The other domains (percentage work missed due to HS and impairment while working) showed similar trends, a slight increase followed by a steady decrease. Both were not significant.
Arizona sexual experiences scale: ASEX
At baseline, the mean ASEX score was 15.4 ± 4.5 points and did not differ between both genders (P = 0.77). Nine respondents (22.5%) met the criteria for sexual dysfunction at one or more time points. Three months postsurgery, the mean overall score showed a small improvement to 14.4 points, however not significant (P = 0.443). At 6 months, the average ASEX scores were comparable again to baseline. The trend analysis showed a significant influence from age on the average ASEX score (P = 0.008). We further analysed this through independent sample t‐tests, comparing the scores for participants ≤35 years and ≥36 years at baseline (n = 27), 3 (n = 16) and 6 months (n = 9) postsurgery. There was a difference in ASEX scores for all time points between the groups, with a significant difference at 6 months (18.0 vs 13.5 points for the ≥36 years group; P = 0.02).
Pain level
Mean pain intensity at baseline was 2.8 ± 2.4 points out of 10. After 2 weeks, patients reported an average pain level of 3.3 points, which decreased to 1.6 points at 6 months, both not significant. However, the effect of time on the level of pain was significant (P = 0.029). Trend analysis showed no additional influence from age or gender.
Discussion
In this prospective single centre study, we assessed the influence of major surgery on the general quality of life, work and activity impairment and sexual health in patients with HS. We found that patients with Hurley stage I or II had a shorter TTWC compared to patients with Hurley stage III and TTWC was significantly prolonged in patients treated with biologics. Furthermore, a larger wound surface area was significantly related to prolonged TTWC.
For the Hurley stage, this can partially be explained by a substantial difference in wound surface between Hurley I and Hurley III. Notably, body mass index and smoking were not significantly related to time to wound closure in our study. Dixon et al.14 described no increased risk of wound complications for smokers in a cohort of 4197 patients who underwent excisions for skin malignancies. Most reported wound complications due to smoking are wound dehiscence, necrosis of a flap or graft, prolonged healing time and infections. However, studies assessing wound healing mainly focus on healing of acute wounds, rather than secondary wound healing, which could explain our somewhat contrasting findings.15, 16 Further studies on the effect of smoking on secondary wound healing are necessary.
All procedures in this study were done under general anaesthesia. Another convenient option for patients with smaller lesions is using local tumescent anaesthesia. By diluting lidocaine and epinephrine with normal saline, a larger area can be numbed and radical surgery can be achieved. The addition of epinephrine limits blood loss via vasoconstriction.
We found an overall relapse rate of 23.7%, which is slightly lower compared with previous studies.17, 18 Interestingly, none of the patients treated with biologics experienced a relapse. All surgical procedures were performed by the same dermatologist, with years of experience in performing this technique. One could therefore expect a slightly lower recurrence rate. However, the mean follow‐up was relatively short. Longer follow‐up time could have resulted in similar relapse rate compared with other studies. More importantly, surgical skills need to be practiced continuously; therefore, education and training is mandatory in HS surgery.
All patient‐reported outcomes demonstrated similar trends: a modest increase in scores at first, which translates to worsening of, e.g., quality of life, followed by a steady decrease, thus improvement. The high DLQI score at baseline confirms the enormous impact of HS on quality of life once again. For the DLQI, the increase lasted until the third month, before declining to baseline value at 6 months. Notably, the average amount of days before wound closure was 81 days (2.7 months), which is accompanied by daily wound care, pain and reduced mobility. This might explain the trend of DLQI scores and why we did not find a significant decrease in DLQI score compared with baseline. A significant decrease in DLQI scores was found in the retrospective study of Posch et al.6 where patients with Hurley stage III had wide local excision (n = 74) and a minimum follow‐up period of 6 months.
Kofler et al. carried out a retrospective survey study of 255 HS patients with Hurley stage III, who underwent wide local excision between 2006 and 2015. The majority of patients experienced impairment of their everyday life (97%) and of their professional life (60%) before surgery. These findings are comparable for our study, where almost 90% of patients experienced impairment of everyday life at baseline. In both studies, these percentages decreased after surgery.5 For the WPAI‐HS, the activity impairment showed a significant increase at week 2; however, this rapidly improved to only a third of the value at week 2 after 6 months. For overall work impairment, the impairment nearly doubled after 2 weeks. Again, this also substantially improved at 6 month to less than a fifth of the impairment at week two. Even though this was not significant after 6 months, a positive trend is clear. Indicating that major surgery improved work productivity and daily activity of these patients, this has not been previously published.
Overall, 9 out of 39 subjects met the criteria for sexual dysfunction at one or more time points. Besides a modest improvement in sexual health after 3 months, this effect did not seem to sustain through the end of the study. In our study, the vast majority of patients had moderate to severe HS, which likely indicates several preceding years with active disease. This observation is in agreement with that of Janse et al.,3 who showed, that the majority of patients with HS have the experience, that sexual problems are not given enough attention by their physicians.
Summarizing, we found a significant influence of Hurley stage and biologic treatment on TTWC, contrastingly not of smoking and some improvement in work and activity impairment after major surgery, which were not previously published. However, not every aspect of the patients’ quality of life showed significant changes after 6 months. It may be that a single procedure with only 6 months of follow‐up might not suffice for either improving or detecting a considerable change in sexual health or other aspects of quality of life. Our results indicate the need for a more comprehensive approach, if the goal is to improve the patients’ quality of life.
This study had some limitations, because of its small sample size and relatively short follow‐up period. The number of participants might be too small to draw hard conclusions concerning the TTWC and influencing parameters. A larger prospective study with longer follow‐up period is needed to confirm our findings. Another limitation of this study is that TTWC was not evaluated using matched pairs. The 6‐month follow‐up period evidently was too short to adequately assess change in general quality of life and sexual health in a skin disease with a long history. Unfortunately, only a quarter of the respondents completed the entire survey for all time points, which could influence our current findings.
Conclusion
Our results show a considerable negative influence of Hurley stage III, treatment with biologics and wound surface on time to wound closure after major surgery. The time of wound closure was surprisingly not influenced by smoking. Furthermore, we found acceptable recurrence rates and an improvement in overall work activity and improvement in activity impairment after surgery. Future long‐term studies on the effect of major surgery on the quality of life in HS are needed.
Author contribution
All authors involved in study design. Prens, Horvath and Huizinga analysed and collected the data. All authors drafted and/or revised the manuscript and approved the manuscript for submission.
Acknowledgements
The authors thank all the patients who participated.
Conflicts of interest
Prens reports no conflicts of interest. Huizinga reports fees from AbbVie for consultation/advisory, scientific research, congress, and fees from Novartis for scientific research and fees from MediReva for consultation/advisory and congress. Janse reports a research grant from Abbvie. Horváth reports fees from AbbVie, Novartis, UCB Pharma, Solenne BV, Celgene, Akari therapeutics, Leo Pharma and Janssen‐Cilag for consultation/advisory, scientific research, congress and courses, and fees from Novartis for consultation/advisory, scientific research and congress outside the submitted work. Consultation fees from Philips and Roche.
Funding source
None declared.
References
- 1. Revuz J. Hidradenitis suppurativa. J Eur Acad Dermatology Venereol 2009; 23: 985–998. [DOI] [PubMed] [Google Scholar]
- 2. Jemec GBE, Kimball AB. Hidradenitis suppurativa: Epidemiology and scope of the problem. J Am Acad Dermatol 2015; 73: S4–S7. [DOI] [PubMed] [Google Scholar]
- 3. Janse IC, Deckers IE, van der Maten AD et al Sexual health and quality of life are impaired in hidradenitis suppurativa: a multicentre cross‐sectional study. Br J Dermatol 2017; 176: 1042–1047. [DOI] [PubMed] [Google Scholar]
- 4. Alavi A, Farzanfar D, Rogalska T, Lowes MA, Chavoshi S. Quality of life and sexual health in patients with hidradenitis suppurativa. Int J Womens Dermatol 2018; 4: 74–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kofler L, Schweinzer K, Heister M, Kohler M, Breuninger H, Häfner HM. Surgical treatment of hidradenitis suppurativa: an analysis of postoperative outcome, cosmetic results and quality of life in 255 patients. J Eur Acad Dermatol Venereol 2018; 32: 1570–1574. [DOI] [PubMed] [Google Scholar]
- 6. Posch C, Monshi B, Quint T, Vujic I, Lilgenau N, Rappersberger K. The role of wide local excision for the treatment of severe hidradenitis suppurativa (Hurley grade III): retrospective analysis of 74 patients. J Am Acad Dermatol 2017; 77: 123–129.e5. [DOI] [PubMed] [Google Scholar]
- 7. Yazdanyar S, Jemec GB. Current and future treatments of hidradenitis suppurativa. Expert Rev Dermatol 2010; 5: 335–343. [Google Scholar]
- 8. Blok JL, Spoo JR, Leeman FWJ, Jonkman MF, Horváth B. Skin‐tissue‐sparing excision with electrosurgical peeling (STEEP): a surgical treatment option for severe hidradenitis suppurativa Hurley stage II/III. J Eur Acad Dermatology Venereol 2015; 29: 379–382. [DOI] [PubMed] [Google Scholar]
- 9. Finlay AY, Khan GK. Dermatology life quality index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol 1994; 19: 210–216. [DOI] [PubMed] [Google Scholar]
- 10. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 1993; 4: 353–365. [DOI] [PubMed] [Google Scholar]
- 11. Reilly M. Reilly Associates Health Outcomes Research [Internet]; 2002.
- 12. McGahuey CA, Gelenberg AJ, Laukes CA et al The arizona sexual experience scale (Asex): reliability and validity. J Sex Marital Ther 2000; 26: 25–38. [DOI] [PubMed] [Google Scholar]
- 13. Horváth B, Janse IC, Blok JL et al Hurley staging refined: a proposal by the dutch hidradenitis suppurativa expert group. Acta Derm Venereol 2017; 97: 412–413. [DOI] [PubMed] [Google Scholar]
- 14. Dixon AJ, Dixon MP, Dixon JB, Del Mar CB. Prospective study of skin surgery in smokers vs. nonsmokers. Br J Dermatol 2009; 160: 365–367. [DOI] [PubMed] [Google Scholar]
- 15. Gill JF, Yu SS, Neuhaus IM. Tobacco smoking and dermatologic surgery. J Am Acad Dermatol 2013; 68: 167–172. [DOI] [PubMed] [Google Scholar]
- 16. McDaniel JC, Browning KK. Smoking, chronic wound healing, and implications for evidence‐based practice. J Wound Ostomy Continence Nurs 2014; 41: 415–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Saunte DML, Jemec GBE. Hidradenitis suppurativa: advances in diagnosis and treatment. JAMA 2017; 318: 2019–2032. [DOI] [PubMed] [Google Scholar]
- 18. Blok JL, Boersma M, Terra JB et al Surgery under general anaesthesia in severe hidradenitis suppurativa: a study of 363 primary operations in 113 patients. J Eur Acad Dermatol Venereol 2015; 29: 1590–1597. [DOI] [PubMed] [Google Scholar]


