Abstract
Background/aims
Contingency management (CM) interventions have gained considerable interest due to their success in the treatment of addiction. However, their implementation can be resource‐intensive for clinical staff. Mobile telephone‐based systems might offer a low‐cost alternative. This approach could facilitate remote monitoring of behaviour and delivery of the reinforcer and minimize issues of staffing and resources. This systematic review and meta‐analysis assessed the evidence for the effectiveness of mobile telephone‐delivered CM interventions to promote abstinence (from drugs, alcohol and tobacco), medication adherence and treatment engagement among individuals with substance use disorders.
Design
A systematic search of databases (PsychINFO, CINAHL, MEDLINE PubMed, CENTRAL, Embase) for randomized controlled trials and within‐subject design studies (1995–2019). The review was conducted in accordance with the PRISMA statement. The protocol was registered on PROSPERO.
Setting
All included studies originated in the United states.
Participants
Seven studies were found, including 222 participants; two targeted alcohol abstinence among frequent drinkers and four targeted smoking cessation (in homeless veterans and those with post‐traumatic stress disorder). One targeted medication adherence.
Measures
The efficacy of CM to increase alcohol and nicotine abstinence was compared with control using several outcomes; percentage of negative samples (PNS), quit rate (QR) and longest duration abstinent (LDA) at the end of the intervention.
Findings
The random‐effects meta‐analyses produced pooled effect sizes of; PNS [d = 0.94, 95% confidence interval (CI) = 0.63–1.25], LDA (d = 1.08, 95% CI = 0.69–1.46) and QR (d = 0.46, 95% CI = 0.27–0.66), demonstrating better outcomes across the CM conditions. Most of the studies were rated as of moderate quality. ‘Fail‐safe N' computations for PNS indicated that 50 studies would be needed to produce a non‐significant overall effect size. None could be calculated for QR and LDA due to insufficient number of studies.
Conclusion
Mobile telephone‐delivered contingency management performs significantly better than control conditions in reducing tobacco and alcohol use among adults not in treatment for substance use disorders.
Keywords: Contingency management, drug use, financial incentives, mobile telephone, remote monitoring, substance use
Introduction
Contingency management (CM) interventions, based on the scientific principles of operant conditioning, involve the application of positive reinforcement (e.g. monetary incentives) contingent upon behaviour change. CM is among the most efficacious psychosocial interventions for substance use disorders and has gained considerable interest due to its success in encouraging health‐related behaviour change, including treatment engagement and attendance, medication adherence and abstinence from substance use, as evidenced in several recent meta‐analyses 1, 2, 3, 4, 5.
Despite the evidence for CM interventions in the treatment of substance use, there are challenges and barriers impeding their implementation. To ensure maximum effectiveness, there are several key principles of operant conditioning that contingency management interventions must satisfy: objective verification that the treatment goal has been achieved, minimal delay in delivering the reinforcement and sufficient magnitude of the reinforcer to make it effective 3. Therefore, CM requires frequent monitoring of behaviour change and differential delivery of reinforcement, making their implementation resource‐intensive and burdensome 6, 7, and creates challenges and barriers to their delivery. Given the widespread availability and use of mobile telephones among the general public (94% of adults in the United States and 95% in the United Kingdom 8), the use of mobile technologies is an expanding approach to enhance the reach of health‐care interventions. Mobile telephone ownership among those affected by substance use disorders is lower, but comparable to the national average. With 83% of patients receiving drug treatment in the United Kingdom reporting to own a mobile telephone 9, this might be a feasible platform upon which healthcare could be delivered in the treatment of substance use disorders 10. The remote delivery of CM interventions has been developed to enable greater accessibility to these interventions, allowing them to be delivered without the need for recurrent attendance at clinical services 11. Remote CM has been used to target substance use and other health‐related behaviours in individuals who might not normally access treatment services 12. This approach also enables services to maintain contact with patients over a longer period to support recovery and provide an early warning of relapse 13.
Development of these interventions can be guided by the basic scientific principles on which CM interventions are based, to ensure that they remain effective while being feasible and acceptable to all. Mobile technology has been used to accomplish one or both of the following key principles of contingency management: (a) monitor the target behaviour or (b) deliver incentives for satisfying the target behaviour contingency 14. Using mobile technology to monitor the target behaviour remotely is typically achieved by wireless submission of data. For example, a number of studies targeting alcohol intake require participants to continuously wear a secure remote alcohol monitoring (SCRAM) bracelet, which works by detecting metabolites of alcohol excreted through sweat 15, 16, 17. Data are available to researchers and provide a continuous overview of alcohol consumption. Studies promoting smoking cessation typically require participants to submit videos via a web camera of themselves taking a breath carbon monoxide test with the results 18, 19, 20. Medication adherence is typically monitored using electronic or medication event monitoring systems (MEMS) caps: micro‐circuitry fitted to pill bottles or containers that issue a time stamp upon opening and closing 21, 22, 23, 24.
Technology has been incorporated into CM interventions to deliver incentives remotely 15, 18, 19, 20, 25, 26, 27, 28, 29, 30, 31, 32, 33. Typically, participants receive messages about their ‘earnings' (monetary value accrued of reinforcer), which are generated automatically and sent shortly after the participant engages in the target behaviour 22. The emergence of study prepaid debit cards (an automated reward payment platform) allows financial incentives to be electronically loaded onto the participant's card once satisfaction of the target behaviour has been verified. Although these cards are linked to the study, they mimic that of a debit/credit card, allowing for the withdrawal of cash as automated teller machines (ATMs) and electronic purchases. Immediate delivery of the reinforcement is key to the principles of CM and has been consistently shown to be a significant moderator of effect size, responsible for generating an effect size almost twice that of studies using more delayed delivery 3. Additionally, inconsistent delivery of the reinforcement may result in insufficient exposure to the incentives and hinder the development of a clear contingent relationship between behaviour and the incentive 34. Technology makes it easier to deliver the reinforcer consistently and on every presentation of the target behaviour.
Given these advantages and the increasing use of mobile technologies, there is growing interest in utilizing mobile telephones to deliver CM. This is the first systematic review and meta‐analysis assessing the evidence specially for the effectiveness of mobile telephone‐delivered contingency management interventions to promote behaviours to encourage abstinence (from drugs, alcohol and tobacco), medication adherence and treatment engagement among individuals with substance use disorders.
Methods
We conducted a systematic review and meta‐analysis of randomized controlled trials and within‐subject designs to examine the effectiveness of mobile telephone‐based contingency management interventions for the treatment of substance use disorders. A protocol for the current review is available on PROSPERO (Registration number: CRD42018093598; please see Supporting information, Appendix A for a copy of the published protocol).
Search strategy
The review was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement 35. Studies were identified using a keyword search of the following on‐line databases: PsychINFO, CINAHL, MEDLINE PubMed and CENTRAL in the Cochrane Library and Embase using the following search terms: ‘contingency management' OR contingen* reinforcement OR voucher OR reinforcement OR reward OR incentive OR economics OR payment OR prize OR monetary OR money OR financial OR gift card OR lottery OR loyalty card AND substance‐related disorder OR drug dependence OR drug misuse OR drug abuse OR alcoholism OR alcohol abuse OR drug dependence OR addiction OR substance abuse OR substance misuse OR smoking OR nicotine OR opioid OR narcotic AND treatment outcome OR drug dependence treatment OR adher* OR compliance OR rehabilitation OR engage OR abstinen* OR cessation OR behaviour change OR therapy OR effective OR reduction OR attend AND text messaging OR telephone OR mobile OR telephone OR remote monitoring. All databases were searched for studies published between 1995 and December 2018.
Studies
Randomized controlled trials (RCTs) that compared telephone‐delivered CM interventions with other treatment interventions, such as motivational enhancement therapy, cognitive behaviour therapy or treatment as usual, were included. Within‐subject designs comparing no intervention/baseline with an intervention phase were also included, as these designs are relatively common in the field of behaviour analysis.
Intervention(s)/exposure(s)
We only included studies that used mobile telephones to monitor behaviour and/or deliver incentives remotely and targeted behaviours to encourage abstinence (from drugs, alcohol and tobacco), medication adherence and treatment engagement. Typically, reinforcement interventions include a number of components (e.g. financial incentives plus praise or feedback about progress), with the independent influence on treatment efficacy not always measured. Therefore, we did not require that studies isolated the effects of incentives from those common elements for inclusion. For studies that employed a between‐subject design, the comparator was the control group who received: no contingency management; treatment‐as‐usual; alternative comparable interventions; or face‐to‐face contingency management. For those studies that employed a within‐subjects design, the comparison could be a no‐intervention baseline phase that preceded and followed the intervention, or a multiple‐baseline design wherein the timing of the incentive intervention was staggered in time across different targets or different participants.
Primary outcomes
The efficacy of telephone‐delivered contingency management was assessed using the following outcomes:
Abstinence, as measured by: proportion of individuals who are continuously abstinent; length of abstinence period; PDA;
Medication adherence, as measured by: proportion of individuals who are taking their medication as prescribed; and
Treatment engagement, as measured by; percentage of days in attendance or engagement in therapeutic activities.
Data extraction and synthesis
Endnote X8 was used to manage records throughout this review, and Microsoft Excel was used for data extraction. All records were extracted, and duplicates removed by a single reviewer (C.G.) using an extraction table created specifically for the review. Two review authors (C.G., A.M.) independently scanned the title and abstract of every record retrieved to determine which studies should be further evaluated for inclusion. Three response options (‘yes', ‘no' and ‘maybe') were used for excluding records or promoting them to the next stage of the winnowing process. All potentially relevant articles were investigated as full text and any uncertainties were discussed between the review authors. This process is detailed in a PRISMA flowchart (Fig. 1). Authors of three studies 31, 36, 37 were contacted to obtain additional study data. Where not explicit in manuscripts, authors were also asked to clarify how missing samples were handled in the analyses (analysed as positive or omitted).
Figure 1.
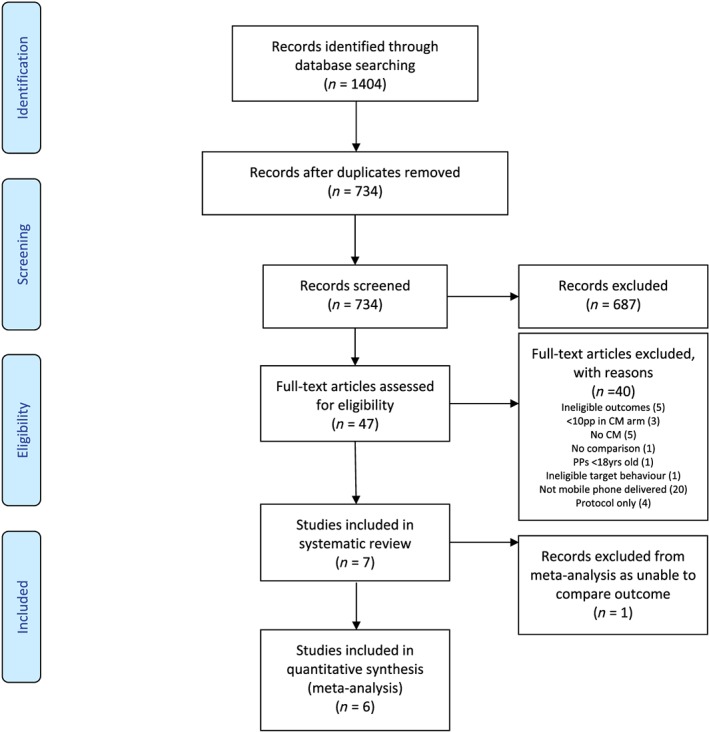
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram [Colour figure can be viewed at http://wileyonlinelibrary.com]
Outcome measures
Standardized mean differences were calculated for each individual study using percentage of negative samples (PNS) or longest duration abstinent (LDA). Odds ratios were calculated for quit rates (QR).
Quality assessment
The Quality Assessment Tool for Quantitative Studies 38 was used to assess the quality of included studies at outcome level. This tool assesses the internal and external validity of each study and rates the quality across six dimensions (selection bias, study design, confounds, blinding, data collection and withdrawals/dropouts). Studies are rated as being of a strong, moderate or weak quality based on these individual domains.
Risk of bias assessment
Due to studies reporting positive results being more likely to be published in the literature, resulting in an over‐representation of positive effects 39, publication bias was assessed using the ‘fail‐safe N' technique 40. Comprehensive Meta‐Analysis software version 3 41 was used to calculate the number of studies averaging a Z‐value of zero that would be needed to result in a non‐significant overall pooled effect size.
Data analysis
Meta‐analyses were carried out using Cochrane Collaboration Review Manager software 42. To calculate effect size for treatment evaluation studies, standardized mean difference is the most common method. Risk difference odds ratio was used for QR. All meta‐analyses were conducted as random‐effects analyses due to the variety of target behaviours, populations and CM interventions used. The efficacy of CM was compared with control using a number of outcomes: PNS, QR and LDA. Despite studies reporting data on other types of outcomes (e.g. money spent on alcohol/drugs), we only included those of greatest relevance to assessing the effectiveness of CM.
Results
Included studies
A total of 1404 records were identified. Following removal of duplicates, 734 records remained and were screened at title and abstract level. Following the removal of 687 ineligible records, 47 records were screened at full‐text level. A total of seven studies met the inclusion criteria (see PRISMA flow diagram, Fig. 1) and were included in the review 22, 31, 34, 36, 37, 43, 44.
Study targets and population
Intervention target behaviours varied across the seven studies. Six studies used mobile telephone‐delivered CM to target abstinence. More specifically, two targeted alcohol abstinence among frequent drinkers 34, 36 and four targeted smoking cessation in smokers [including homeless veterans and those with post‐traumatic stress disorder (PTSD)] 31, 37, 43, 44. One study targeted medication adherence among individuals with HIV and substance misuse 22. No studies targeted treatment engagement (attendance or engagement in therapeutic activities). The populations targeted were adults not in treatment for substance use disorder. See Table 1 for a full description of included studies.
Table 1.
Description of each included study and intervention.
| Study author (year) | Design | Sample size (baseline) | Retention (end of intervention) | Number of Conditions | Longest follow‐up (months) | Treatment duration | Target behaviour | Intervention procedure | Type of reinforcement | Reinforcement schedule | Reward delivery | Type of mobile used | Use of telephone | Primary outcomes | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CM condition Mean (SD) | Control condition Mean (SD) | ||||||||||||||
| Alessi et al. (2013) | RCT | 30 | 100% | 2 (BrAC monitoring only or BrAC monitoring plus CM) | None | 4 weeks | Alcohol abstinence | 1–3 daily prompts for BrAC readings Incentives earned for alcohol‐negative tests (< 0.02 g/dl % BrAC) | Monetary | Escalating with reset | Gift card or cheque | Study cellphone with video camera and breathalyser | Monitor behaviour and deliver reinforcer | PNS 87.1% (11.4). LDA 16.8 (10.1) | PNS 66.9% (19.1). LDA 5.9 (3.4) |
| Alessi et al. (2017) | RCT | 90 | 100% | 2 (mHealth monitoring only or mHealth monitoring + reinforcement) | 6 | 4 weeks | Smoking cessation | 1–3 daily prompts for CO tests. Prize draws for smoking‐negative on‐time CO tests (CO ≤ 6 p.p.m.) | Prize draw | Escalating draws with reset | Prize draws redeemable weekly | Study cellphone with video camera and CO monitor | Monitor behaviour and deliver reinforcer | PNS 89.1% (19.5%) LDA 27.0 (12.0) | PNS 65.9% (38.0%) LDA 15.2 (11.9) |
| Carpenter et al. (2015) | WS | 20 | 100% | NA | 6 | 4 weeks | Smoking cessation | 2 daily prompts for CO tests. Incentives earned for smoking‐negative CO tests (CO ≤ 6 p.p.m.) | Monetary | Escalating with reset | Mailed cheque | Study cellphone with video camera and CO monitor | Monitor behaviour and deliver reinforcer | Quit rate at 4 weeks 50% (n = 20) | |
| Hertzberg et al. (2013) | RCT | 22 | 91% | 2 (mCM or yoked mCM/non‐contingent) | 3 | 4 weeks | Smoking cessation | 2 daily prompts for CO tests Incentives earned or smoking‐negative CO tests (CO ≤ 8 p.p.m.) | Monetary | Escalating with reset | Mailed cheque | Study cellphone with video camera and CO monitor | Monitor behaviour | QR at 4 weeks 82% (n = 9 of 11) PNS 75.8% (42.9%) | QR at 4 weeks 45% (n = 5 of 11) PNS 55.8% (49.7%) |
| Moore et al. (2015) | WS | 10 | 100% | NA | None | 12 weeks | Medication adherence | Centralized Off‐site AdheRence Enhancement (CARE) programme Adherence was measured by electronic pill dispenser | Monetary | Escalating for weeks 1–6 of treatment, followed by tapering, variable interval reinforcement for weeks 7–12 | Debit card | Participant's own cellphone | Deliver reinforcer | PDA Medication adherence improved from 80.7% at the start of treatment to 93.2% at the end of treatment | |
| Raiff et al. (2017) | WS (non‐concurrent multiple‐baseline design) | 10 | 100% | NA | 1 | 14 days | Smoking cessation | Group CM procedure. 2 daily CO tests. Incentives earned for smoking negative CO tests (CO ≤ 4 p.p.m.) plus bonus when both members of the pair met their target | Monetary | Escalating with reset | Mailed gift card | Participant's own smartphone | Monitor behaviour | PNS at baseline (mean = 1.25%, SD = 4.0) and treatment (mean = 35.5%, SD = 35.7) | |
| Koffarnus et al. (2018) | RCT | 40 | 100% | 2 (mCM or yoked mCM/non‐contingent) | 1 | 21 days | Alcohol abstinence | Thrice daily prompts for BrAC readings Incentives earned for alcohol‐negative tests (<0.02 g/dl % BrAC) | Monetary | Escalating with reset | Debit card | Participant's own cellphone | Monitor behaviour and deliver reinforcer | PDA 85% PNS 91.5% (10.2%). | PDA 38%PNS 66.9% (23.9%) |
RCT = randomized clinical trial; WS = within‐subjects; BrAC = breath alcohol concentration; CM = contingency management; PNS: percentage of negative samples; LDA = longest duration abstinent; PDA = percentage of days abstinent; QR = quit rate; CO = carbon monoxide; SD = standard deviation; NA = not applicable; p.p.m. = parts per million.
Technologies used in monitoring and delivering reinforcement
Included in this review are studies that used mobile telephones to monitor behaviour and/or deliver the reinforcement remotely and targeted behaviours to encourage abstinence (from drugs, alcohol and tobacco), medication adherence and treatment engagement. Six studies used mobile telephones to monitor behaviour. The most common method involved participants taking videos of themselves completing a breath carbon monoxide (CO) test and presenting the results as proof of achieving the target behaviour. These videos were remotely submitted to the researchers before reinforcers were delivered. One study, targeting adherence to antiretroviral medications in individuals living with HIV and substance misuse problems, used electronic pill dispensers to transmit a message to a software program for analysis and interpretation each time the device was opened 22.
In five of the included studies mobile telephones were also used to deliver the reinforcement. More specifically, messages of verbal praise were commonly used to confirm achievement of the target behaviour and to indicate earnings 22, 31, 34, 36, 44. Remote monitoring of behaviour allows for prompt verification of goal satisfaction. While the majority of the studies mailed earnings to participants in cheque form, two studies employed the use of reloadable credit cards to deliver the reinforcer immediately following verification of the target behaviour 22, 36.
Reinforcement type and schedules
The type of reinforcement used varied across studies. Six studies used monetary incentives 22, 31, 34, 36, 37, 43: gift cards, cheques or cash loaded onto a debit card, while one used prize‐based reinforcement 44. Consistent with traditional face‐to‐face CM interventions, most of the studies included in this review employed differential reinforcement of other behaviour (DRO) to reinforce abstinence, whereby the reinforcement was delivered contingent on negative urine and breath CO samples. An escalating schedule of reinforcement whereby the amount of reinforcement increased progressively following consecutive achievement of the target behaviour was employed by all studies.
Quality assessment
To ascertain the internal and external validity as well as any biases and confounds of the included studies, two reviewers (C.G. and A.M.) worked independently to rate the quality of each study across six domains. Using the Quality Assessment Tool for Quantitative Studies 38, each study was rated as being of strong, moderate or weak across six dimensions (selection bias, study design, confounds, blinding, data collection and withdrawals/dropouts). Ratings for all included studies are summarized in Table 2. Overall, most of the retrieved studies had a high quality of data collection and reporting withdrawals/dropouts. None of the studies were double‐blinded, as blinding both participants and providers to contingency management interventions is not possible due to the nature of the intervention. All studies employing a randomized controlled trial design included details regarding the method used to randomize participants. Studies employing a within‐subjects design were rated as being of moderate quality as per guidelines from the Effective Public Health Practice Project (EPHPP) quality assessment tool 38.
Table 2.
EPHPP ratings for all included studies.
| Study | Selection bias | Study design | Confounds | Blinding | Data collection | Withdrawals/dropouts | Overall |
|---|---|---|---|---|---|---|---|
| Aharonovich (2017) | 2 | 1 | 1 | 2 | 1 | 1 | Strong |
| Alessi (2013) | 2 | 1 | 2 | 3 | 1 | 1 | Moderate |
| Alessi (2013) | 2 | 1 | 1 | 3 | 1 | 1 | Moderate |
| Carpenter (2015) | 3 | 2 | 1 | 3 | 1 | 1 | Weak |
| Hertzberg (2015) | 3 | 1 | 1 | 3 | 1 | 1 | Weak |
| Moore (2015) | 2 | 2 | 1 | 3 | 1 | 1 | Moderate |
| Raiff (2017) | 2 | 2 | 1 | 3 | 1 | 1 | Moderate |
| Koffarnus (2018) | 2 | 1 | 1 | 3 | 1 | 1 | Moderate |
1 = strong; 2 = moderate; 3 = weak; EPHPP = Effective Public Health Practice Project.
Publication bias
Publication bias was assessed using the ‘fail‐safe N' technique 40. For PNS, 50 studies would be needed to result in a non‐significant overall pooled effect size. For QR and LDA, ‘fail‐safe N' could not be calculated due to an insufficient number of studies.
Meta‐analyses
The efficacy of CM to encourage abstinence was compared with control using a number of outcomes: PNS, QR and LDA. Due to only one study targeting medication adherence, data for this outcome could not be collated. Therefore, data across six studies were used for the meta‐analyses.
The meta‐analysis for PNS combined results across five studies (191 participants) assigned to five CM conditions and five non‐CM conditions (non‐CM condition details are provided in Table 1). The random‐effects meta‐analysis produced a pooled effect size of d = 0.94 [95% confidence interval (CI) = 0.63–1.25], with CM performing better than the non‐CM condition (Fig. 2). Variability of effects between studies was not due to between‐study heterogeneity (I 2 = 6%).
Figure 2.
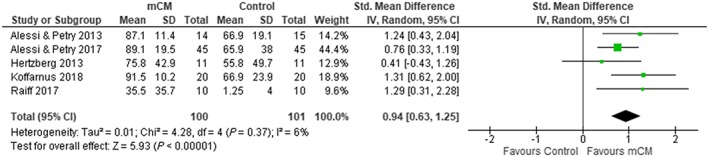
Forest plot for percentage negative samples by end of treatment for all substances [Colour figure can be viewed at http://wileyonlinelibrary.com]
For QR, two studies (62 participants) assigned to two CM conditions and two non‐CM conditions were included. The random‐effects meta‐analysis produced a pooled effect size of d = 0.46 (95% CI = 0.27–0.66), with CM performing better than the non‐CM condition (Fig. 3). Variability of effects between studies was not due to between‐study heterogeneity (I 2 = 0%).
Figure 3.
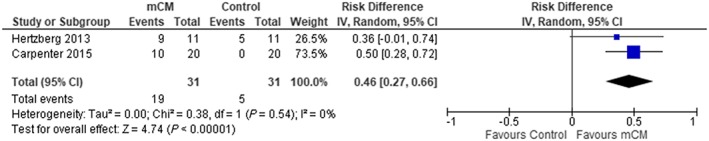
Forest plot for quit rate by end of treatment for nicotine [Colour figure can be viewed at http://wileyonlinelibrary.com]
The meta‐analysis for LDA combined results across two studies (119 participants) assigned to two CM conditions and two non‐CM conditions. The random‐effects meta‐analysis produced a pooled effect size of d = 1.08 (95% CI = 0.69–1.46), with CM performing better than the non‐CM condition (Fig. 4). Variability of effects between studies was not due to between‐study heterogeneity (I 2 = 0%).
Figure 4.
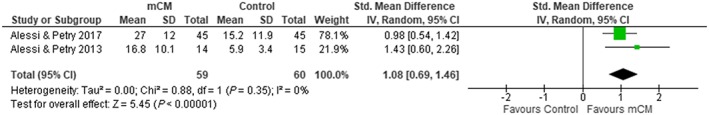
Forest plot for longest duration abstinent for all substances [Colour figure can be viewed at http://wileyonlinelibrary.com]
Discussion
In this systematic review and meta‐analysis, we examined the efficacy of mobile telephone‐delivered contingency management for enhancing treatment of substance use disorders. The random‐effects analyses showed that mobile telephone‐delivered CM performed significantly better than control conditions (involving no reinforcement contingent on behaviour change) in reducing tobacco and alcohol use among adults not in treatment for substance use disorders across the three outcomes of interest, PNS, QR and LDA, with pooled effect sizes of d = 0.94 (95% CI = 0.63–1.25); d = 0.46 (95% CI = 0.27–0.66) and d = 1.08 (95% CI = 0.69–1.46), respectively. Only one study has targeted medication adherence among individuals with HIV and substance misuse 22, and no studies have targeted treatment engagement (attendance or engagement in therapeutic activities). This review is the first to directly assess the evidence for the effectiveness of CM delivered using mobile telephones. The results across the three outcomes assessed in this review are of major clinical importance; however, they must be treated with caution due to the small number of studies with multiple outcomes.
The use of technology to monitor behaviour and deliver reinforcement has been well developed during the last decade and continues to offer an effective and practical means to target treatment‐related behaviours over longer periods of time and enable comprehensive outcome data to be collected on a continuous and ongoing basis. An existing systematic review 14 of controlled studies published between 2004 and 2015 provides support for the efficacy of technology‐based (e.g. internet, computer, mobile telephone) reinforcement interventions remotely implemented to target health behaviours, including substance use. However, the review was inclusive of all technology‐based CM, including less remote applications using computers and landline telephones. Also, a meta‐analysis was not undertaken by these authors and therefore no statistical comparisons and conclusions were provided. Nonetheless, considering the growing contribution of technology‐based interventions in the treatment of addiction, providing an up‐to‐date review of the literature is important. This is emphasized in this review, as almost 50% of included studies in the meta‐analysis have been published since the last review in 2015.
This review only included interventions delivered by mobile telephones, a strategy which led to almost 50% of articles screened for eligibility excluded, as they employed remote delivery by another means, most commonly by computer. Therefore, a small number of studies were included. Although our results should be interpreted with caution due to this, the effect across all studies is consistent and substantial, and allows us to draw preliminary conclusions regarding the potential effectiveness of mobile CM interventions. Furthermore, one might also argue that combining studies of different designs is a study limitation. However, all studies in each comparison employed the use of mobile telephones to address the same clinical outcome among a substance‐use population group. In addition to this, all studies had relatively consistent parameters of the contingency management interventions (i.e. escalating reinforcement schedules) to strengthen behaviour change, making it appropriate to combine them. A key distinction was not the design of the studies, but rather the extent to which they were able to yield an unbiased estimate of the effect size in question 45.
Overall, most of the identified studies demonstrated a high quality of data collection methods by employing standard assessment tools of known reliability and validity and explicitly reported numbers and reasons for withdrawals and dropouts. Nonetheless, none of the studies were double‐blinded, as blinding both participants and providers to contingency management interventions is not possible due to the nature of the treatment. Regarding informativeness of included studies, all employing a randomized controlled trial design included details regarding the method used to randomize participants. Studies employing a within‐subjects design were rated as moderate quality, as per guidelines from the EPHPP quality assessment tool 38. In addition, analyses of missed samples at an outcome level varied across studies. Although not always explicitly stated in study reports, missed samples could be treated as positive or simply omitted from analyses. Adherence to study procedures (i.e. providing daily CO and BrAC samples) was lower in control conditions across two studies 34, 43, resulting in fewer samples being obtained in these group. Therefore, coding missed tests as positive might have differentially deflated abstinence rates in the monitoring condition and inflated differences between conditions in these studies. In such cases, analysing the proportion of negative CO and BrAC tests outcome with the number of tests submitted in the denominator and missed tests omitted might have yielded more accurate results.
Despite these limitations, several study level strengths are also worth noting, such as retention rate across studies. In addition to this, comparison group conditions differed among studies, with some control participants being yoked to a participant in the contingency management condition and receiving a payment equal to their paired participant 38, 39. This strategy ensures that participants across both conditions receive the same payment schedule with the same likelihood of escalations, resets and bonuses. This isolates the effects of the contingency for comparison across groups. Another strength of the studies included in this review was the inclusion of biological indicators (objective measures) to verify substance use rather than relying on self‐report. This is key in ensuring that the reinforcer is only delivered upon the participant satisfying the target behaviour and outcome data are reflective of goal‐directed behaviour. Regarding the review, there are also several notable strengths. This is the first systematic review and meta‐analysis assessing the evidence especially for the effectiveness of mobile telephone‐delivered contingency management interventions to promote treatment in individuals with substance use disorders. Synthesizing data across the existing studies allows us to identify which outcome measures and population groups are most likely to benefit from the intervention. The last decade has seen an emergence in studies assessing the initial efficacy and feasibility of mobile telephone‐delivered CM interventions to promote smoking cessation and alcohol abstinence. In the near future, we suspect that the body of literature demonstrating the effectiveness of these interventions will flourish.
Furthermore, the studies in this review included relatively short interventions (on average 4–5 weeks) and small sample sizes (as illustrated in Table 1). Future research should assess the long‐term benefits of providing extended mobile telephone‐delivered CM interventions and use larger sample sizes to enable definitive conclusions to be made about clinical outcomes. Long‐term incentive programmes, as developed by Silverman and colleagues in the Therapeutic Workplace 46, have been shown to demonstrate sustained treatment effects among those with substance use disorders and may offer a cost‐effective means to encourage drug abstinence and treatment adherence over a much longer period.
It is also worth noting that no studies compared differences in treatment effects between in‐person‐delivered CM and mobile telephone‐delivered CM interventions. Our findings are broadly consistent with those found for face‐to‐face delivered CM targeted at smoking and alcohol cessation, as evidenced in previous meta‐analyses [smoking cessation (d = 0.31) 2 and alcohol cessation (d = 0.32) 3]. The limitations discussed and the lack of evidence available does, however, present avenues for future research. Although mobile telephone‐delivered CM might appear to be an efficacious treatment for alcohol abstinence and smoking cessation, there are no current studies evaluating its impact in reducing drug use behaviours. Technological developments will ultimately enable advances to be made in generating effective and accurate monitoring equipment to enable us to target substance misuse behaviours successfully. This is important, as the remote delivery of these interventions has the potential to expand the reach and landscape of treatment delivery among individuals not in contact or receiving treatment within drug services. Mobile telephones might offer a more accessible and convenient means of delivering CM interventions to those less accessible individuals at a potentially critical time in their treatment journey 12.
Declaration of interests
None.
Supporting information
Appendix A. A systematic review and meta‐analysis of the effectiveness of mobile telephone‐delivered contingency management interventions promoting behaviour change in individuals with substance use disorders.
Acknowledgements
The research reported in this publication was supported by the Society for the Study of Addiction as part of C.G.'s PhD Studentship. The authors would like to extend a thank‐you to all who took the time and effort to share data to aid in the analyses.
Getty, C.‐A. , Morande, A. , Lynskey, M. , Weaver, T. , and Metrebian, N. (2019) Mobile telephone‐delivered contingency management interventions promoting behaviour change in individuals with substance use disorders: a meta‐analysis. Addiction, 114: 1915–1925. 10.1111/add.14725.
[Correction added on 29 August 2019 after first online publication: Table 1 has been corrected in this version]
References
- 1. Ainscough T. S., McNeill A., Strang J., Calder R., Brose L. S. Contingency management interventions for non‐prescribed drug use during treatment for opiate addiction: a systematic review and meta‐analysis. Drug Alcohol Depend 2017; 178: 318–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Prendergast M., Podus D., Finney J., Greenwell L., Roll J. Contingency management for treatment of substance use disorders: a meta‐analysis. Addiction 2006; 101: 1546–1560. [DOI] [PubMed] [Google Scholar]
- 3. Lussier J. P., Heil S. H., Mongeon J. A., Badger G. J., Higgins S. T. A meta‐analysis of voucher‐based reinforcement therapy for substance use disorders. Addiction 2006; 101: 192–203. [DOI] [PubMed] [Google Scholar]
- 4. Griffith J. D., Rowan‐Szal G. A., Roark R. R., Simpson D. D. Contingency management in outpatient methadone treatment: a meta‐analysis. Drug Alcohol Depend 2000; 58: 55–66. [DOI] [PubMed] [Google Scholar]
- 5. Higgins S. T., Silverman K. Contingency Management in Substance Abuse Treatment. New York, NY: Guilford Press; 2008. [Google Scholar]
- 6. Rash C. J., Stitzer M., Weinstock J. Contingency management: new directions and remaining challenges for an evidence‐based intervention. J Subst Abuse Treat 2017; 72: 10–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Petry N. M. Contingency management treatments: controversies and challenges. Addiction 2010; 105: 1507–1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pew Research Center . Smartphone Ownership is Growing Rapidly Around the World, but Not Always Equally. Washington, DC: Pew Research Center; 2019.
- 9. Milward J., Day E., Wadsworth E., Strang J., Lynskey M. Mobile phone ownership, usage and readiness to use by patients in drug treatment. Drug Alcohol Depend 2015; 146: 111–115. [DOI] [PubMed] [Google Scholar]
- 10. Free C., Phillips G., Galli L., Watson L., Felix L., Edwards P. et al The effectiveness of mobile‐health technology‐based health behaviour change or disease management interventions for health care consumers: a systematic review. PLOS Med 2013; 10: e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Budman S. H. Behavioral health care dot‐com and beyond: computer‐mediated communications in mental health and substance abuse treatment. Am Psychol 2000; 55: 1290–1300. [PubMed] [Google Scholar]
- 12. Dallery J., Raiff B. R. Contingency management in the 21st century: technological innovations to promote smoking cessation. Subst Use Misuse 2011; 46: 10–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hämäläinen M. D., Zetterström A., Winkvist M., Söderquist M., Karlberg E., Öhagen P. et al Real‐time monitoring using a breathalyzer‐based eHealth system can identify lapse/relapse patterns in alcohol use disorder patients. Alcohol Alcohol 2018; 53: 368–375. [DOI] [PubMed] [Google Scholar]
- 14. Kurti A. N., Davis D., Redner R., Jarvis B., Zvorsky I., Keith D. R. et al A review of the literature on remote monitoring technology in incentive‐based interventions for health‐related behavior change. Transl Issues Psychol Sci 2016; 2: 128–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barnett N. P., Tidey J., Murphy J. G., Swift R., Colby S. M. Contingency management for alcohol use reduction: a pilot study using a transdermal alcohol sensor. Drug Alcohol Depend 2011; 118: 391–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dougherty D., Hill‐Kapturczak N., Liang Y., Karns T., Cates S., Lake S., et al Use of continuous transdermal alcohol monitoring during a contingency management procedure to reduce excessive alcohol use. Drug Alcohol Depend 2014; 142: 301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dougherty D. M. L. S., Hill‐Kapturczak N., Liang Y., Karns T. E., Mullen J., Roache J. D. Using contingency management procedures to reduce at‐risk drinking in heavy drinkers. Alcohol Clin Exp Res 2015; 39: 743–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dallery J. G. I. Effects of an internet‐based voucher reinforcement program for smoking abstinence: a feasibility study. J Appl Behav Anal 2005; 38: 349–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dallery J. M. S., Glenn I. M. A deposit contract method to deliver abstinence reinforcement for cigarette smoking. J Appl Behav Anal 2008; 41: 609–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stoops W. W., Dallery J., Fields N. M., Nuzzo P. A., Schoenberg N. E., Martin C. A. et al An internet‐based abstinence reinforcement smoking cessation intervention in rural smokers. Drug Alcohol Depend 2009; 105: 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Barnett P. G. S. J., Wong W., Haug N. A., Hall S. M. Effect of incentives for medication adherence on health care use and costs in methadone patients with HIV. Drug Alcohol Depend 2009; 100: 115–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moore B. A., Rosen M. I., Wang Y., Shen J., Ablondi K., Sullivan A. et al A remotely‐delivered CBT and contingency management therapy for substance using people with HIV. AIDS Behav 2015; 19: 156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rosen M. I. D. K., McMahon T. J., Valdes B., Petry N. M., Cramer J., Rounsaville B. Improved adherence with contingency management. AIDS Patient Care STDS 2007; 21: 30–40. [DOI] [PubMed] [Google Scholar]
- 24. Sorensen J. L. H. N., Delucchi K. L., Gruber V., Kletter E., Batki S. L. et al Voucher reinforcement improves medication adherence in HIV‐positive methadone patients: a randomized trial. Drug Alcohol Depend 2007; 88: 54–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Glenn I. M. D. J. Effects of internet‐based voucher reinforcement and transdermal nicotine patch on cigarette smoking. J Appl Behav Anal 2007; 40: 1–13; 40–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dallery J. G. I., Raiff B. R. An internet‐based abstinence reinforcement treatment for cigarette smoking. Drug Alcohol Depend 2007; 86: 230–238. [DOI] [PubMed] [Google Scholar]
- 27. Reynolds B. D. J., Shroff P., Patak M., Leraas K. A web‐based contingency management program with adolescent smokers. J Appl Behav Anal 2008; 41: 597–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Meredith S. E., Dallery J. Investigating group contingencies to promote brief abstinence from cigarette smoking. Exp Clin Psychopharmacol 2013; 21: 144–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ondersma S. J. S. D., Lam P. K., Connors‐Burge V. S., Ledgerwood D. M., Hopper J. A. A randomized trial of computer‐delivered brief intervention and low‐intensity contingency management for smoking during pregnancy. Nicotine Tob Res 2012; 14: 351–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Alessi S. M., Petry N. M. A randomized study of cellphone technology to reinforce alcohol abstinence in the natural environment. Addiction 2013; 108: 900–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Carpenter V. L., Hertzberg J. S., Kirby A. C., Calhoun P. S., Moore S. D., Dennis M. F. et al Multicomponent smoking cessation treatment including mobile contingency management in homeless veterans. J Clin Psychiatry 2015; 76: 959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dallery J., Meredith S., Jarvis B., Nuzzo P. A. Internet‐based group contingency management to promote smoking abstinence. Exp Clin Psychopharmacol 2015; 23: 176–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dallery J., Raiff B. R., Kim S. J., Marsch L. A., Stitzer M., Grabinski M. J. Nationwide access to an internet‐based contingency management intervention to promote smoking cessation: a randomized controlled trial. Addiction 2017; 112: 875–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Alessi S., Petry N. A randomized study of cellphone technology to reinforce alcohol abstinence in the natural environment. Addiction 2013; 108: 900–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Moher D. L. A., Tetzlaff J., Altman D. G., The PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: the PRISMA Statement. Ann Intern Med 2009; 151: 264–269. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 36. Koffarnus M. N., Bickel W. K., Kablinger A. S. Remote alcohol monitoring to facilitate incentive‐based treatment for alcohol use disorder: a randomized trial. Alcohol Clin Exp Res 2018; 42: 2423–2431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hertzberg J., Carpenter V., Kirby A., Calhoun P., Moore S., Dennis M. et al Mobile contingency management as an adjunctive smoking cessation treatment for smokers with posttraumatic stress disorder. Nicotine Tob Res 2013; 15: 1934–1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Effective Public Health Practice Project . Quality Assessment Tool For Quantitative Studies. Hamilton, ON: The Effective Public Health Practice Project (EPHPP); 1998. [Google Scholar]
- 39. Schmid C. H. Outcome Reporting Bias: A Pervasive Problem in Published Meta analyses. American Journal of Kidney Diseases 2017; 69: 172–174. [DOI] [PubMed] [Google Scholar]
- 40. Rosenthal R. The file drawer problem and tolerance for null results. Psychol Bull 1979; 86: 638–641. [Google Scholar]
- 41. Borenstein M., Hedges L., Higgins J., Rothstein H. Comprehensive Meta‐Analysis V3. Englewood, NJ: Biostat; 2013. [Google Scholar]
- 42. Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. [Google Scholar]
- 43. Raiff B. R., Arena A., Meredith S. E., Grabinksi M. J. Feasibility of a mobile group financial‐incentives intervention among pairs of smokers with a prior social relationship. Psychol Rec 2017; 67: 231–239. [Google Scholar]
- 44. Alessi S., Rash C., Petry N. A. Randomized trial of adjunct mHealth abstinence reinforcement with transdermal nicotine and counseling for smoking cessation. Nicotine Tob Res 2017; 19: 290–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Borenstein M., Hedges L. V., Higgins J. P., Rothstein H. R. Introduction to meta‐analysis. Chichester: John Wiley & Sons, Ltd; 2009. [Google Scholar]
- 46. Silverman K. W. C., Grabinski M. J., Hampton J., Sylvest C. E., Dillon E. M., Wentland R. D. A web‐based therapeutic workplace for the treatment of drug addiction and chronic unemployment. Behav Modif 2005; 29: 417–463. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix A. A systematic review and meta‐analysis of the effectiveness of mobile telephone‐delivered contingency management interventions promoting behaviour change in individuals with substance use disorders.


