Abstract
Background:
Polycystic ovary syndrome (PCOS) is a polygenic endocrine disorder in women of reproductive ages which will lead to infertility. This study is aimed to determine changes in levels of hyperandrogenism, hirsutism and menstrual regulation after a period of aquatic high intensity interval training (AHIIT) in women with PCOS.
Methods:
Thirty patients with PCOS having age between 20 and 35 and body mass index (BMI) ≥30 kg/m2 in obstetrics and gynaecology clinics in Isfahan were selected based on Rotterdam Diagnostic Criteria. They were randomly divided into experimental (AHIIT + metformin, N = 15) and control groups (metformin, N = 15). The exercises were done for 12 weeks, three sessions of 20 minutes. Metformin (1500 mg) was taken daily for 3 consecutive days for 12 weeks. Kolmogorov–Smirnov test, t-test, Covariance and Wilcoxon were applied (P value < 0.05).
Results:
After 12 weeks, no significant difference was observed in waist-to-hip ratio (WHR), but in AHIIT, the BMI and fat mass significantly decreased and levels of follicle-stimulating hormone (FSH), free testosterone (FT) and sex hormone binding globulin (SHBG) increased compared to control group (P < 0.05). While levels of improvement of total testosterone (TT), dehydroepiandrosterone sulphate (DHEAS), FT, luteinising hormone (LH) and free androgen index (FAI) were not significant between the two groups (P > 0.05). Furthermore, there was a significant decrease in homeostatic assessment of insulin resistance (HOMA-IR) and hirsutism severity in experimental group (P < 0.05). In both groups, the order of menstrual cycles improved significantly (P < 0.05).
Conclusions:
Doing AHIIT besides drug therapy can be effective for PCOS patients.
Keywords: AHIIT, hyperandrogenemia, hirsutism, menstrual, PCOS
Introduction
Polycystic ovary syndrome (PCOS) characterised by a chronic disorder in ovulation along with hyperandrogenism has become one of the most common endocrine disorders in women of productive age with an estimated 5%–15% prevalence. It is considered as the main reason for infertility due to lack of ovulation.[1,2,3] It has the symptoms such as menstrual disorders, infertility, hyperandrogenism, obesity, hirsutism and acne.[4] Furthermore, women with PCOS are at risk for other diseases such as insulin intolerance, diabetes type 2, metabolic syndrome, cardiovascular diseases, infertility and all kinds of reproductive system cancers.[5] Studies indicate that approximately 75% of people with PCOS are overweight or obese, and even in those with normal weight, PCOS has a fat accumulation in the central area of the body. On the other hand, regardless of the presence of obesity, fat gain is one of the most common characteristics in these women.[6] In addition, the findings of previous studies revealed that 70% of women with PCOS have insulin resistance (IR), and it is indicated that increase in body fat has a direct role in determining IR. Adipose tissue, and in particular visceral fat tissue, through IR can contribute to the pathophysiology of PCOS, metabolic complications as well as the increased fertility problems associated with it.[7,8] On the other hand, hyperandrogenism is the most common PCOS hormonal changes,[3] and insulin has a profound effect on both levels of ovarian stroma and follicles. Insulin secretes androgens in the ovary, and the increase in androgens causes the disappearance of growing follicles and may have a negative effect on follicular growth, ovarian obstruction and inhibition of mucosal maturation.[9] Therefore, IR and hyperandrogenism together create a defective cycle and affect each other.[10] Over the past decades, several therapies including metformin, clomiphene citrate and gonadotropins have been proposed for PCOS patients; but with regard to side effects such as nausea, vomiting, anorexia, headache and multiple cramps, the provision of therapies with supplements can be a good solution in order to cope with these complications and reduce the cost of medical treatments.[11] For this reason, in various studies, lifestyle interventions, especially physical activity, were regarded as the first line of treatment in women with PCOS which would result in improvement in metabolic symptoms and fertility syndrome as well.[12] In the meantime, high intensity interval training (HIIT) is a type of exercise with short training intervals at high intensity.[13] In these types of exercises, the existence of recovery cycles following an intense activity allows individuals to repeat the courses in intensity that cannot be sustained during continuous training.[14] There are the most popular forms of HIIT which consist of 4-minute periods (20 seconds of activity and 10 seconds of rest) with 75%–95% HRmax.[15] It is believed that within 20 seconds of activity (in comparison with low-intensity exercises), body masses such as legs, hips, trunk, abdomen and shoulder belt are more often used to increase calorie intake of fats. Even after intense short training, this process of fat burning continues.[16] Research shows that consumption of excessive calories and fat burning as a result of these exercises produce similar changes in cardiovascular fitness, improved body composition and even risk factors such as insulin activity in less time compared to traditional exercises, moderate intensity and sustained state with a 30- to 40-minute duration.[3,15,17] On the other hand, because of the unique hydrodynamic properties of water, performing HIIT in aquatic environment is more confident and leads to having less weight in exercises compared to HIIT on land.[18] In the review of the previous studies, there has been no study which investigated the effects of aquatic high intensity interval training (AHIIT) on the symptoms of PCOS. Therefore, the major objective of this study was to investigate the influence of a type of intense exercising in water on some types of PCOS symptoms and compare AHIIT by taking metformin alone.
Subjects and Methods
The current study was done through clinical trial. Thirty available patients with PCOS from AL Zahra and Beheshti hospitals were selected as the subjects. The participants of this study had the following characteristics: the ages ranged from 20 to 35 years, their body mass indexes (BMI) were ≥30 kg/m2, no use of hormonal drugs or contraceptives, no blood glucose lowering and physical inactivity during the past 3 months, suffering from IR which was defined by homeostatic assessment of insulin resistance (HOMA-IR) and diagnosis of PCOS by a gynaecologist based on the criteria suggested by the American Society for Reproductive Medicine (ASRM) at the Rotterdam Conference in 2003. The criteria were as follows:
Menstrual disorders (appeared as oligomenorrhea and amenorrhea)
Morphology of the ovary (increase in ovarian volume to more than 10 mm or the existence of 12 follicle or more with the thickness of 2–9 mm in at least one of the ovaries by the use of vaginal and abdominal sonography)
Biochemical or clinical symptoms of hyperandrogenism[19]
The selected participants were randomly divided into experimental (AHIIT and taking metformin, n = 15) and control groups (taking metformin, n = 15). Participants in both groups took 3 pills of metformin (1500 mg) from the beginning of intervention. At the beginning of the intervention (pre-test) and at the end of the third month (post-test), anthropometric measurements, blood samples and clinical symptoms (menstrual disorders and hirsutism) were measured.
Study design
In the current study, each of the indexes was measured as follows:
Participants’ fat mass and BMI using a body fat analyser (Olympia model 3/3, Guan Company and South Korea)
Waist-to-hip ratio (WHR): waist circumference (cm)/hip circumference (cm)
-
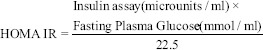
IR with HOMA index using the following formula:
Fasting blood samples were taken for measuring the levels of IR, sex hormone binding globulin (SHBG), free testosterone (FT), total testosterone (TT), luteinising hormone (LH), dehydroepiandrosterone sulphate (DHEAS) and follicle-stimulating hormone (FSH) in all subjects in 2 stages, 1 day before the initial training and 48 hours after the last exercise in the 12th week (after 36 sessions), and after 12 hours of fasting, 10 cc of blood were taken from the venous vein. Blood from the participants was taken during the first days of follicular phase (3 or 4 menstruation days) by electro chemi luminescence (ECL) method and using Roche Cobas device by Roche kit which was made in America. After completion of blood collection, samples were centrifuged and their serums, except for FAI hormone, were isolated and kept at 80°C in calf gel.
FAI was measured using the following formula: FAI = (TT × 100/SHBG)
Ferriman and Gallwey score (F-G score) was used as a visual method of evaluating and quantifying hirsutism in women. Nine androgenic sensitive areas (upper lip, chin, chest, upper back, lower back, upper abdomen, lower abdomen, upper arms and thigh) were taken into consideration. Scoring ranged from a minimum of 0 to a maximum of 36; 8–10 = mild, 11–14 = moderate and scores ≥15 were considered severe hirsutism.[20]
Abdominal or vaginal ultrasonography: At the early stages of the follicular phase (third to fourth menstrual periods), subjects were taken under ultrasonography of the uterus and appendices by the GE VOLUSAN 730 EXPERT device. In this way, the increase in ovarian volume by more than 10 cc, even in one ovary, was diagnosed as PCOS.
Registration menstrual cycle by self-report and filling up the checklist, in the way that, based on the calendar given to the participants, they were required to checkmark the time and duration of their bleeding (for 3 cycles) from the first cycle.
Peak oxygen uptake (VO2peak) assessment of all the participants by PACER Test: In an appropriate area of 20 m, it was identified by cone barriers. Subjects were deployed at the end of one of the 20-m marked lines and began testing. Participants quickly set their pace and increased their running speeds while increasing the number of turning rounds and reducing the time between two peaks until they were no longer able to continue the test. The last record reaching the 20-m line for a person (the number of complete round trips) was immediately recorded on the sheet. Then, for VO2peak evaluation, the number of rounds was calculated by the following formula as an index of aerobic capacity.[21,22]
In an appropriate place, an area of 20 m in length was identified by cone barriers. The participants were set at the end of one of the 20-m lines which was marked. They then started the test. The participants set their pace, and at the same time with increasing the number of round trips and decreasing the time between the two beeps, they increased their pace till they were unable to continue the test. The last record of reaching the 20-m line for the participants (total round trips) was registered immediately.
VO2peak = 28.1 + 0.274 TL
Total number of laps = TL.
Training protocol
Twelve-week protocol AHIIT, which was performed by the experimental group and consisted of 3 sessions in a week for 30 minutes (5 minutes for warm-up, 20 minutes TS and 5 minutes cooling-down). The AHIIT phase of the workout involved 4 times 4-minute bouts, each consisting of 8 rounds of 20-second all-out, maximal work intervals. Each 20-second work interval was followed by 10 seconds of rest in a ready stance with 80%–95% HRmax and 1 minute of rest (jugging) was provided between each 4-minute work bout with 75% HRmax.[15] This was done in a way that, first, 5 minutes jogging and stretching movements of the organs were performed for warm-up. Then, quick movements of the organs and body for 20 minutes and the last 5 minutes, and again, light stretching movements were done to return to the original state. The exercise intensity was measured based on maximum heart rate and based on the following Karvonen formula for each participant:
Maximum heart rate = age - 220
Maximum heart rate × 80%
Maximum heart rate × 95%
Furthermore, exercise intensity was controlled by rate monitor (polar beat, made in Finland) during the exercises in each session.[23] It is worth noting that during the 12-week intervention, participants in control group did not perform any regular exercises.
Statistical analysis
Statistical Package for Social Sciences (SPSS, version 23) was used to analyse the collected data. After confirming the normal distribution of theoretical data by using Kolmogorov–Smirnov test, t-test, Covariance and Wilcoxon were applied in dependent and independent groups to compare the groups’ means (P value < 0.05).
Results
Table 1 shows the participants’ characteristics in experimental and control groups. As indicated in Table 2, BMI and fat mass in training group decreased significantly (both P values < 0.05). The levels of hyperandrogenism (TT, DHEAS, FAI and LH) of women in experimental group decreased, but this reduction was not significant (all P values > 0.05). As can be seen from Table 2, there was a significant difference in experimental group between pre- and post-tests compared to control group in levels of FT, FSH and SHBG (all P values < 0.05). Furthermore, Table 2 shows that the levels of HOMA-IR and hirsutism severity in experimental group decreased compared to control group (both P values < 0.05). In both control and training groups, significant improvement was observed in setting menstrual cycles (both P values < 0.05).
Table 1.
Baseline characteristics of the participants
| (15 PCOS) Experimental |
(15 PCOS) Control |
Baseline characteristics |
|---|---|---|
| 80/2±25/29 | 83/4±00/26 | Age (Years) |
| 6/57±58/162 | 10/3±57/161 | Height (cm) |
| 33/18±72/98 | 62/12±14/97 | Weight (kg) |
| 3.14±1.42 | 3.38±1.20 | (>2.5) HOMA-IR |
| 14.06±5.18 | 15.53±3.77 | (F-G score) Hirsutism |
Table 2.
Clinical therapeutic effects, changes in hyperandrogenism, HOMA-IR, hirsutism and menstrual regulation after 12-week AHIIT
| Variable | Group | ||||
|---|---|---|---|---|---|
| Experimental | Control | ||||
| BMI (≥30 kg/m2) | Before treatment | 32.80±4.49 | 34.06±4.45 | ||
| After treatment | 30.68±2.28 | 33.99±4.41 | |||
| T Test | p* | 0.032 | 0.701 | ||
| Between subjects | T | 11.650 | |||
| p** | 0.002 | ||||
| Fat mass | Before treatment | 38.90±4.11 | 39.22±3.85 | ||
| After treatment | 37.25±3.13 | 39.18±4.14 | |||
| T Test | p* | 0.015 | 0.946 | ||
| Between subjects | T | 5.537 | |||
| p** | 0.026 | ||||
| WHR (cm) | Before treatment | 0.97±0.03 | 0.98±0.03 | ||
| After treatment | 0.95±0.03 | 0.97±0.03 | |||
| T Test | p* | 0.070 | 0.677 | ||
| Between subjects | T | 2.909 | |||
| p** | 0.100 | ||||
| VO2peak (mL/min) | Before treatment | 32.20±1.22 | 32.71±1.45 | ||
| After treatment | 35.20±1.54 | 32.78±1.47 | |||
| T Test | p* | 0.000 | 0.091 | ||
| Between subjects | T | 167.579 | |||
| p** | 0.000 | ||||
| LH (mIU/mL) | Before treatment | 20.91±14.87 | 17.26±12.18 | ||
| After treatment | 12.96±10.11 | 15.11±6.80 | |||
| T Test | p* | 0.028 | 0.267 | ||
| Between subjects | T | 2.267 | |||
| p** | 0.144 | ||||
| FSH (mIU/mL) | Before treatment | 5.06±1.59 | 5.25±2.11 | ||
| After treatment | 7.16±3.21 | 5.47±1.42 | |||
| T Test | p* | 0.012 | 0.512 | ||
| Between subjects | T | 5.334 | |||
| p** | 0.029 | ||||
| SHBG (nmol/L) | Before treatment | 36.40±21.00 | 49.07±28.80 | ||
| After treatment | 55.53±20.46 | 52.40±24.20 | |||
| T Test | p* | 0.000 | 0.148 | ||
| Between subjects | T | 9.551 | |||
| p** | 0.005 | ||||
| FT (pg/mL) | Before treatment | 2.13±0.60 | 2.27±0.64 | ||
| After treatment | 1.34±0.61 | 2.18±063 | |||
| T Test | p* | 0.001 | 0.099 | ||
| Between subjects | T | 17.601 | |||
| p** | 0.000 | ||||
| FAI (TT/SHBG) 100 | Before treatment | 1.73±0.80 | 1.78±1.10 | ||
| After treatment | 1.17±0.43 | 1.34±0.62 | |||
| T Test | p* | 0.001 | 0.019 | ||
| Between subjects | T | 1.821 | |||
| p** | 0.188 | ||||
| DHEAS (microg/mL) | Before treatment | 1.83±0.46 | 1.97±0.39 | ||
| After treatment | 1.72±0.42 | 1.90±0.32 | |||
| T Test | p* | 0.048 | 0.206 | ||
| Between subjects | T | 0.930 | |||
| p** | 0.344 | ||||
| TT (ng/mL) | Before treatment | 0.69±0.25 | 0.61±0.17 | ||
| After treatment | 0.57±0.14 | 0.58±0.11 | |||
| T Test | p* | 0.015 | 0.158 | ||
| Between subjects | T | 2.608 | |||
| p** | 0.118 | ||||
| HOMA-IR (>2.5) | Before treatment | 3.14±1.42 | 3.38±1.20 | ||
| After treatment | 2.69±0.78 | 3.23±0.98 | |||
| T Test | p* | 0.032 | 0.133 | ||
| Between subjects | T | 7.734 | |||
| p** | 0.010 | ||||
| Hirsutism (F-G score) | Before treatment | 14.06±5.18 | 15.53±3.77 | ||
| After treatment | 7.53±2.03 | 14.80±3.46 | |||
| T Test | p* | 0.000 | 0.003 | ||
| Between subjects | T | 73.809 | |||
| p** | 0.000 | ||||
| Premenstrual (between 38 and 28 days) | Before treatment | 69.33±20.24 | 66.73±19.72 | ||
| After treatment | 47.80±13.38 | 56.93±17.54 | |||
| Wilcoxon | Z | -3.296 | -3.175 | ||
| P | 0.001 | 0.001 | |||
p* for within-group comparisons (T test), p** for between-group comparisons (ANCOVA), BMI=body mass index, WHR=waist-to-hip ratio, VO2Peak=peak oxygen uptake, F-G score=Ferriman–Gallwey score, HOMA-IR=homeostatic assessment of insulin resistance, FSH=follicle-stimulating hormone, LH=luteinising hormone, TT=total testosterone, FT=free testosterone, FAI=free androgen index (TT×100/SHBG), SHBG=sex hormone binding globulin, DHEAS=dehydroepiandrosterone sulphate
Discussion
The findings revealed that 12-week AHIIT, along with taking metformin, compared with taking metformin only, both statistically and clinically lead to reduction in PCOS symptoms, including anthropometric indicators improvement (BMI and fat mass), HOMA-IR, some indexes of hyperandrogenism (FT, FSH and SHBG), reduction in severity of hirsutism and the number of days of menstrual cycle. Surprisingly, these exercises did not result in significant improvement in factors such as WHR, LH, FAI, DHEAS and TT, compared to control group. In the current study, BMI and fat mass decreased significantly, which was consistent with the findings of Marcondes et al. (2017) and Mario et al. (2017).[24,25] By examining the effect of daily walk on clinical parameters of 86 obese women with PCOS, Mario et al. (2017) showed significant changes in BMI and fat mass.[25] The results revealed that there were no changes in WHR, which match those of Zahang et al. (2017).[26] However, this finding does not support the previous research, such as Turan et al. (2015) and Miranda et al. (2016).[27,28] In the study conducted by Miranda et al. (2016), reduction of WHR during 4 months of strength training on women with healthy overweight and PCOS was reported.[28] A possible explanation of this contradiction is related to the difference in type, duration of each session and the duration of training in the current study. Furthermore, improvement was observed in HOMA-IR after 12 weeks of AHIIT. In previous studies, the effect of training with moderate intensity on IR in women with PCOS was reported.[29,30] Research showed that HIIT creates similar changes in body composition and even risk factors such as insulin activity compared to traditional, moderate and sustained exercise with a minimum of 30–40 minutes.[15,17] In a study by Babraj et al. (2009), it was shown that HIIT short training sessions influence insulin effects for 3 minutes per week, and when insulin is more effective, the muscles are able to use more amounts of fat as fuel. And, in turn, the risk of developing metabolic diseases such as T2D is reduced.[31] On the other hand, in the current study, 12 weeks of AHIIT exercise in infertile women with PCOS resulted in significant increase in VO2peak, which indicated the correct performance of exercises by participants. Doing physical exercises results in an increase in muscle blood flow and causes an increase in oxygen intake after the exercise. Therefore, regular physical exercises, particularly AHIIT, can reduce fats and enhance the efficiency of cardiovascular system. Because of increase in energy consumption, enzymes of aerobic and anaerobic energy supply system will increase and oxidation of fat will rise.[32] On the other hand, hyperandrogenism is the most common hormonal changes of PCOS, and women with PCOS often have high serum concentration of these androgens.[3] In the study done by Chen et al. (2015), it was found that women with PCOS have higher level of LH and lower level of FSH compared to healthy women. The high levels of LH/FSH cause to create hyperandrogenism which would lead to appearance of PCOS symptoms.[33] In the current study, it was revealed that 12 weeks of exercises along with taking metformin resulted in significant increase in FSH and SHBG and significant decrease in FT. These results match those observed in earlier studies.[2,25,34] Generally, gonadotropins are glycoprotein which release GnHR from pituitary in response to releasing hormones. Releasing GnHR produces FSH and LH concentrations.[35] In previous studies, it was found that physical activities in people lead to an increase in beta endorphin hormone and reduction of GnHR, and consequently decrease the level of LH.[34] The results of this study will now be compared to the findings of previous work in which physical exercising in women with PCOS results in an increase in SHBG.[28] In this study, reduction in FT can be considered as one reason for increase in FSH and SHBG and the effects of extreme exercising. In a physiological justification, increase in the amount of SHBG after 12 weeks of extreme exercising, as in the current study, seems to be the reason for decrease in the insulin levels, because insulin restrains the production of SHBG from human hepatoma cells, in addition to having direct effect on increase in androgen production. On the other hand, controlling insulin production by blood glucose lowering drugs and diet therapy cause tangible increase of serum levels but might not have any changes in the androgen levels. This issue indicates the direct effect of insulin on the production of SHBG.[36] There was reduction in other levels of hyperandrogenism (TT, DHEAS, FAI and LH), but this reduction was not significant enough. Another finding of this study is that significant decrease in the status of menstrual periods and hirsutism in both groups, and particularly in AHIIT group, matches with the study of Zahang (2017) who found that taking metformin along with daily physical activities resulted in dramatic changes in the weight, BMI, the size of the ovaries, the amount of menstruation, ovulation, pregnancy, sexual hormones and fasting insulin.[26] IR and hyperinsulinemia related to it in women with PCOS cause a decrease in the level of SHBG and increase in the level of FT hormone, which consequently lead to menstrual disorder, development of ovarian cyst, lack of ovulation and infertility. On the other hand, having direct effect on theca cells lead to enhancement of androgen secretion in ovaries and appearance of symptoms such as hirsutism and acne.[3] Cheema et al. (2014) believe that in the case of performing sport intervention (either in the form of resistance or aerobic exercises), provided that the sport programme is regular and has appropriate intensity, insulin sensitivity, and following that hirsutism and menstrual cycles will improve and possibility of reproduction will increase.[37] In fact, decrease in BMI, and especially abdominal fat, has a major role in reduction of risk factors for infertility and lead to improvement in hormonal and clinical disorders.[38] On the one hand, only enhancement of these symptoms is reported in studies such as Williams et al. (2015) and Visa et al. (2016).[39,40] In their study, Visa et al. (2016) investigated the effect of progressive strength training at home on a number of 15 women with PCOS. After 12 weeks, no significant changes on the order of menstrual periods between the two groups were reported.[40] In the current study, however, the significant change is probably because of type and intensity of exercises. There are three mechanisms for losing fat caused by HIIT exercises: (1) increase in mitochondrial density and capacity during HIIT leads to increase in fat oxidation; (2) increase in the amount of catecholamines results in fat breakdown, especially in abdominal region which has more β-adrenergic receptors compared to subcutaneous fat; (3) suppressing appetite: consuming energy the day after HIIT (300 kilo calories) is lower than aerobic exercises and (600 kilo calories) after a rest.[14]
Therefore, doing only 20 minutes AHIIT exercises by increase in VO2peak, weight loss and reduction in insulin level, improvement in insulin sensitivity and hormonal levels cause improvement in endocrine condition, hirsutism severity and menstrual order in obese women with PCOS.
The main limitation of the present study can be that the information about daily energy intake, psychological and mental conditions and motivation participant as two main interventions in women with PCOS was not collected before and after intervention. However, patients in the present study were asked to maintain their usual dietary intakes and psychological and mental conditions during study period and report any change.
Conclusions
The findings of this study revealed that performing 12-week AHIIT, 3 sessions in a week and each session for 20 minutes accompanied by taking metformin resulted in improvement in the levels of hyperandrogenism, hirsutism and menstrual regulation in women with PCOS. Therefore, performing AHIIT accompanied by taking metformin can be effective in curing and improvement of the symptoms of this disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank the personnel of the Isfahan University of Medical Sciences and PCOS participants.
References
- 1.Qi X, Pang Y, Qiao J. The role of anti-Müllerian hormone in the pathogenesis and pathophysiological characteristics of polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol. 2016;199:82–7. doi: 10.1016/j.ejogrb.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 2.Almenning I, Rieber-Mohn A, Lundgren KM, Shetelig Løvvik T, Garnæs K, Moholdt T. Effects of high intensity interval training and strength training on metabolic, cardiovascular and hormonal outcomes in women with polycystic ovary syndrome: A pilot study. PLoS One. 2015;10:e0138793. doi: 10.1371/journal.pone.0138793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Leo V, Musacchio MC, Cappelli V, Massaro MG, Morgante G, Petraglia F. Genetic, hormonal and metabolic aspects of PCOS: An update. Reprod Biol Endocrinol. 2016;14:38. doi: 10.1186/s12958-016-0173-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trikudanathan S. Polycystic ovarian syndrome. Med Clin. 2015;99:221–35. doi: 10.1016/j.mcna.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Sylwia B, Agnieszka S. The pathogenesis and treatment of polycystic ovary yndrome: What's new? Adv Clin Exp Med. 2017;26:359–67. doi: 10.17219/acem/59380. [DOI] [PubMed] [Google Scholar]
- 6.Zhang CM, Zhao Y, Li R, Yu Y, Yan LY, Li L, et al. Metabolic heterogeneity of follicular amino acids in polycystic ovary syndrome is affected by obesity and related to pregnancy outcome. BMC Pregnancy Childbirth. 2014;14:11. doi: 10.1186/1471-2393-14-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blüher M. Adipose tissue dysfunction contributes to obesity related metabolic diseases. Best Pract Res Clin Endocrinol Metab. 2013;27:163–77. doi: 10.1016/j.beem.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 8.Tosi F, Di Sara D, Kaufman JM, Bonin C, Moretta R, Bonora E, et al. Total body fat and central fat mass independently predict insulin resistance but not hyperandrogenemia in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2015;100:661–9. doi: 10.1210/jc.2014-2786. [DOI] [PubMed] [Google Scholar]
- 9.Suresh S, Vijayakumar T. Correlations of insulin resistance and serum testosterone levels with LH: FSH ratio and oxidative stress in women with functional ovarian hyperandrogenism. Indian J Clin Biochem. 2015;30:345–50. doi: 10.1007/s12291-014-0447-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rojas J, Chávez M, Olivar L, Rojas M, Morillo J, Mejías J, et al. Polycystic ovary syndrome, insulin resistance, and obesity: Bavigating the pathophysiologic labyrinth. Int J Reprod Med. 2014;2014:719050. doi: 10.1155/2014/719050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moran LJ, Ko H, Misso M, Marsh K, Noakes M, Talbot M, et al. Dietary composition in the treatment of polycystic ovary syndrome: A systematic review to inform evidence-based guidelines. J Acad Nutr Diet. 2013;113:520–45. doi: 10.1016/j.jand.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 12.Pinola P. Oulu: University of Oulu; 2016. Hyperandrogenism, Menstrual Irregularities and Polycystic Ovary Syndrome. Acta Universitatis Ouluensis. Disseration. [Google Scholar]
- 13.Lunt H, Draper N, Marshall HC, Logan FJ, Hamlin MJ, Shearman JP, et al. High intensity interval training in a real world setting: A randomized controlled feasibility study in overweight inactive adults, measuring change in maximal oxygen uptake. PLoS One. 2014;9:e83256. doi: 10.1371/journal.pone.0083256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cassidy S, Thoma C, Houghton D, Trenell MI. High-intensity interval training: A review of its impact on glucose control and cardiometabolic health. Diabetologia. 2017;60:7–23. doi: 10.1007/s00125-016-4106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller LJ, D’Acquisto LJ, D’Acquisto DM, Roemer K, Fisher MG. Cardiorespiratory responses to a 20-minutes shallow water tabata. Int J Aquat Res Educ. 2015;9:292–307. [Google Scholar]
- 16.The Tabata workout programme: Harder, faster, fitter, quicker? The Guardian [Internet] 2013. [Last cited 2014 Mar 24]. Available from: http://www.theguardian.com/lifeandstyle/2013/mar/25/tabata-harderfasterfitter-quicker .
- 17.Kester KN. A Comparison of Changes in Women's Cardiovascular Fitness and Body Composition After Performance in Zumba, Tabata, and Cycling. Honors Research Projects. 2017;562:13–33. [Google Scholar]
- 18.Batterham SI, Heywood S, Keating JL. Systematic review and meta-analysis comparing land and aquatic exercise for people with hip or knee arthritis on function, mobility and other health outcomes. BMC Musculoskelet Disord. 2011;12:123–35. doi: 10.1186/1471-2474-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Rahnama Z, Sohbati S, Safizadeh H. Effect of hirsutism on quality of life: A study in Iranian women. J Pakistan Assoc Dermatol. 2013;23:28–33. [Google Scholar]
- 21.Mahar MT, Welk GJ, Rowe DA. Estimation of aerobic fitness from PACER performance with and without body mass index. Meas Phys Educ Exerc Sci. 2018;22:239–49. [Google Scholar]
- 22.Akira M, Takahashi Y, Yamazoe M, Kumakura N, Ikeda A, Wilk B, et al. Validity of the multistage 20-M shuttle-run test for Japanese children, adolescents, and adults. Pediatr Exerc Sci. 2004;16:113–25. [Google Scholar]
- 23.Heath EH. ACSM's guidelines for exercise testing and prescription. Med Sci Sports Exerc. 2005;37:2018. [Google Scholar]
- 24.Marcondes RR, Maliqueo M, Fornes R, Benrick A, Hu M, Ivarsson N, et al. Exercise differentially affects metabolic functions and white adipose tissue in female letrozole- and dihydrotestosterone-induced mouse models of polycystic ovary syndrome. Mol Cell Endocrinol. 2017;448:66–76. doi: 10.1016/j.mce.2017.03.025. [DOI] [PubMed] [Google Scholar]
- 25.Mario FM, Graff SK, Spritzer PM. Habitual physical activity is associated with improved anthropometric and androgenic profile in PCOS: A cross-sectional study. J Endocrinol Invest. 2017;40:377–84. doi: 10.1007/s40618-016-0570-1. [DOI] [PubMed] [Google Scholar]
- 26.Zhang J, Si Q, Li J. Therapeutic effects of metformin and clomiphene in combination with lifestyle intervention on infertility in women with obese polycystic ovary syndrome. Pak J Med Sci. 2017;33:8–12. doi: 10.12669/pjms.331.11764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Turan V, Mutlu EK, Solmaz U, Ekin A, Tosun O, Tosun G, et al. Benefits of short-term structured exercise in non-overweight women with polycystic ovary syndrome: A prospective randomized controlled study. J Phys Ther Sci. 2015;27:2293–7. doi: 10.1589/jpts.27.2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miranda-Furtado CL, Picchi Ramos FK, Kogure GS, Santana-Lemos BA, Ferriani RA, Calado RT, et al. A nonrandomized trial of progressive resistance training intervention in women with polycystic ovary syndrome and its implications in telomere content. J Reprod Sci. 2016;23:644–54. doi: 10.1177/1933719115611753. [DOI] [PubMed] [Google Scholar]
- 29.Al-Eisa E, Gabr SA, Alghadir A. Effects of supervised aerobic training on the levels of anti-Mullerian hormone and adiposity measures in women with normo-ovulatory and polycystic ovary syndrome. J Pak Med Assoc. 2017;67:499–507. [PubMed] [Google Scholar]
- 30.Nybacka Š, Carlström K, Ståhle A, Nyrén S, Hellström PM, Hirschberg AL. Randomized comparison of the influence of dietary management and/or physical exercise on ovarian function and metabolic parameters in overweight women with polycystic ovary syndrome. Fertil Steril. 2011;96:1508–13. doi: 10.1016/j.fertnstert.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 31.Babraj JA, Vollaard NB, Keast C, Guppy FM, Cottrell G, Timmons JA. Extremely short duration high intensity interval training substantially improves insulin action in young healthy males. BMC Endocr Disord. 2009;9:3. doi: 10.1186/1472-6823-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Elizabeth N, Sanders ME, Franklin BA. Aquatic high intensity interval training for cardiometabolic health: Benefits and training design. Am J Lifestyle Med. 2016;11:64–76. doi: 10.1177/1559827615583640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen J, Shen S, Tan Y, Xia D, Xia Y, Cao Y, et al. The correlation of aromatase activity and obesity in women with or without polycystic ovary syndrome. J Ovarian Res. 2015;8:11. doi: 10.1186/s13048-015-0139-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miri M, Karimi Jashni H, Alipour F. Effect of exercise intensity on weight changes and sexual hormones (androstenedione and free testosterone) in female rats with estradiol valerate-induced PCOS. J Ovarian Res. 2014;7:37. doi: 10.1186/1757-2215-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Devlin TM. Tehran: Aeeig; 2011. Textbook of Biochemistry: With Clinical Correlations; pp. 1195–201. [Google Scholar]
- 36.Orsatti FL, Nahas EA, Maesta N, Nahas-Neto J, Burini RC. Plasma hormones, muscle mass and strength in resistance-trained postmenopausal women. Maturitas. 2008;59:394–404. doi: 10.1016/j.maturitas.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 37.Cheema BS, Vizza L, Swaraj S. Progressive resistance training in polycystic ovary syndrome: Can pumping iron improve clinical outcomes? Sports Med. 2014;44:1197–207. doi: 10.1007/s40279-014-0206-6. [DOI] [PubMed] [Google Scholar]
- 38.Kaiyun X, Meiyan Z, Xiaolan M. Clinical efficacy of metformin combined with clomiphene in patients with polycystic ovary syndrome and their effect on serum sex hormones. Int J Clin Exp Med. 2018;11:12467–73. [Google Scholar]
- 39.Williams NI, Leidy HJ, Hill BR, Lieberman JL, Legro RS, Jane De Souza M. Magnitude of daily energy deficit predicts frequency but not severity of menstrual disturbances associated with exercise and caloric restriction. Am J Physiol Endocrinol Metab. 2015;308:29–39. doi: 10.1152/ajpendo.00386.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vizza L, Smith CA, Swaraj S, Agho K, Cheema BS. The feasibility of progressive resistance training in women with polycystic ovary syndrome: A pilot randomized controlled trial. BMC Sports Sci Med Rehabil. 2016;8:14. doi: 10.1186/s13102-016-0039-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


