Abstract
BACKGROUND:
Although rabies is highly fatal, with timely and correct postexposure prophylaxis (PEP) of animal bite victims, it could be prevented. Medical school students should be trained about the appropriate rabies management during their formative years so that they put the right practice later on. The study was conducted to assess the knowledge about rabies epidemiology and prophylaxis among medical students and to find the effect of an educational intervention.
MATERIALS AND METHODS:
This was a quasi-experimental study conducted with 156 third academic year medical school students at a tertiary care teaching hospital. The study participants were given health education intervention. A study tool assessed the knowledge of study participants on domains such as epidemiology of rabies, pre-exposure prophylaxis (PrEP) and PEP, and national program guidelines of rabies prevention. The study tool was administered before and after the intervention. The impact of educational intervention was measured with scores. Wilcoxon signed-rank test was applied to test the difference.
RESULTS:
The overall total mean pretest total score was 14.9 (±3.7) and posttest score was 22.7 (±3.23) for a maximum score of 29. The mean pretest scores for epidemiology, PrEP and PEP and national program components were 6.09, 7.95, and 0.85 respectively. Likewise, the mean posttest scores were 8.09, 13.26, and 1.35 respectively. There were a statistically significant improvement in the scores after health education intervention.
CONCLUSIONS:
After educational intervention, there were statistically significant improvement in the scores of all the three domains. PrEP and PEP and national program domain of rabies need to be emphasized during formative years.
Keywords: Health education, intervention, medical students, rabies
Introduction
Rabies is 100% fatal but a vaccine-preventable disease. It is a neglected zoonotic disease which occurs in more than 150 countries of the world.[1] According to the World Health Organization (WHO), the number of human rabies deaths globally is estimated to be 61,000 (95% confidence interval 37.000–86.000) per annum based on probability decision tree approach with 84% deaths occurring in rural areas. These estimates also project about 1.9 million disability-adjusted life years.[2] Rabies is transmitted to other animals and humans through close contact with saliva from infected animals by bites, scratches, and licks on broken skin and mucous membranes. Although a number of carnivorous animals serve as natural reservoirs, dogs are the main source of human infections and pose a potential threat to billions of humans.[3] In India, an estimated 17.4 million animal bites occur annually which accounts for an incidence of 1.7%, and an estimated 20,000 human rabies death occurs per annum.[4,5]
Rabies though highly fatal is 100% preventable. With timely and correct postexposure prophylaxis (PEP) for these animal bite victims, rabies can be prevented. Therefore, primary care physicians should be aware about the appropriate PEP, which includes proper wound washing, a full course of anti-rabies vaccination (ARV), and local wound infiltration of rabies immunoglobulin (RIG) into and around the wounds to save lives, in addition to the epidemiology to control rabies in the community. They must also know certain do's and dont's with respect to the PEP such as no application of any irritants, no interchanging of the route of administration and regimen of ARV, no administering of RIG in the gluteal region, and no suturing/bandaging the animal bite wounds before adequate management. Hence, in this context, budding physicians should be educated and made aware about the appropriate rabies epidemiology and prophylaxis during their formative years in the medical school so that they follow correct practice later on in their life. Only few studies have been done with assessment of knowledge about rabies and its prophylaxis before and after educational intervention. This educational intervention is a unique method as it used two different modes as detailed below. In this background, the study was conducted to assess the knowledge about rabies epidemiology and prophylaxis among medical students and to find the effect of educational intervention on their knowledge.
Materials and Methods
Study design
This was a quasi-experimental (before and after type) study conducted among the study population with the assessment done before and after the educational intervention.
Study setting
The study was conducted at a tertiary care teaching hospital in Chennai, Tamil Nadu, India. The study duration was from September to December 2017.
Study population
The study population constitutes third academic year medical school students (pursuing MBBS course) at tertiary care hospital in Chennai. Medical school students who were more than 18 years of age and willing to participate in the study were included in the study.
Sample size determination and sampling
Sample size calculation for one group before and after the study design was obtained from the formula,[6] considering a minimal effect size (E), alpha error = 0.05, power = 80%, and standard deviation of change in outcome (S) (within subject correlation of outcome (r) = 0.85), (Zα = 1.96, Zβ = 0.842, E = 0.25, S = 1.1).
N = (Zα + Zβ) 2/(E/S) 2
Substituting the values, the sample size obtained was 152.
In this study, a total of 156 medical students were included. The students of third academic year were arranged as per their university enrollment number, and simple random sampling was done to enroll the medical students in the study till the sample size was achieved.
Study tool
All the study participants were administered a pretested, semi-structured questionnaire. In addition to certain baseline information, the questionnaire assesses the knowledge about rabies such as epidemiological aspects, mode of transmission, PrEP and PEP including vaccines and immunoglobulins, management of animal bite wound, vaccination regimen, WHO guidelines on prophylaxis, and national program guidelines. The assessment of correct response was done with scores for every question grouped into three domains, i.e., epidemiology of rabies, prophylaxis, and program guidelines with maximum scores of 10, 17, and 2, respectively.
Intervention
Pretesting information was collected using the study tool before educational intervention. The educational intervention was given for the duration of 1 h. The intervention was given in two phases: lecture with audiovisual aid for a period of 30 min on topics covering rabies epidemiology, clinical features, prophylaxis, management and program guidelines, followed by a 30 min short film with audio projected which re-emphasized on the same aspects. After 1-month period, the same study tool was administered to the study participants to collect the posttest data.
Outcomes of the study
The impact of educational intervention (lecture and video) was measured with scores. The difference in scores before and after educational intervention was measured. The study participants were included as per the inclusion criteria. The study participants underwent 1 h educational intervention, and the same study participants were included in postintervention assessment done after 1 month.
Data analysis
Data were entered into Microsoft Excel Spread Sheet and analyzed using Statistical Package for Social Sciences (SPSS-IBM) version 22.0, India. The descriptive statistics like percentage and inferential statistics like Wilcoxon signed-rank test were applied to test the difference between pre and posttest score.
Ethical considerations
Written informed consent was obtained from each study participants. The institutional ethical committee approval was obtained before the initiation of the study.
Results
A total of 156 participants were included. Of 156 participants, 91 (58.3%) were females and 65 (41.7%) were males. The mean age of the study participants was 20.28 (±1.6) years. Majority (66%) of the study participants were hostellers and 135 (86%) were Hindu by religion [Table 1].
Table 1.
Profile of the study participants (n=156)
| Variables | n (%) |
|---|---|
| Age (years) | |
| 19-20 | 88 (56.4) |
| 21-22 | 65 (41.7) |
| >22 | 3 (1.9) |
| Gender | |
| Male | 91 (58.3) |
| Female | 65 (41.7) |
| Residence | |
| Hosteller | 103 (66) |
| Day scholar | 54 (34) |
| Religion | |
| Hindu | 135 (86) |
| Muslim | 10 (6.4) |
| Christian | 10 (6.4) |
| Jain | 1 (0.3) |
Adequate knowledge was found on domains such as epidemiology of rabies, prophylaxis and program guidelines before educational intervention. The score obtained on these domains was 75.7%, 42.4%, and 70.8%, respectively. There has been considerable improvement in knowledge after intervention among the study participants in epidemiology (93.1%), prophylaxis (97%), and program guidelines (93.8%) domains. This was found to be statistically significant (P < 0.01) [Table 2].
Table 2.
Comparison of the proportion of study participants with adequate knowledge pre- and postintervention
| Domain | Knowledge | Pretest, n (%) | Posttest, n (%) | P* |
|---|---|---|---|---|
| Epidemiology | Adequate | 118 (75.7) | 145 (93.1) | <0.01 |
| Inadequate | 38 (24.3) | 11 (6.9) | ||
| PrEP and PEP |
Adequate | 66 (42.4) | 151 (97) | <0.01 |
| Inadequate | 90 (57.6) | 5 (3) | ||
| Program | Adequate | 110 (70.8) | 146 (93.8) | <0.01 |
| Inadequate | 46 (29.2) | 10 (6.2) |
*Mc Nemar’s test was used. PEP=Postexposure prophylaxis, PrEP=Preexposure prophylaxis
Scores
The maximum score of domains for both pre and post tests were 10, 17, and 2 for epidemiology of rabies, prophylaxis, and program guidelines respectively. The overall total maximum for pre and post test evaluation was 29.
The mean pretest and posttest scores scored by participants in epidemiology, prophylaxis, and program guidelines domains were (6.09 vs. 8.09); (7.95 vs. 13.26), and (0.85 vs. 1.35) respectively. There was a statistically significant improvement in the scores of all the three domains after educational intervention [Table 3]. The overall total mean pretest total score was 14.9 (±3.7), and posttest score was 22.7 (±3.23) out of 29. There was a statistically significant improvement in the total scores after health education [Table 3 and Figure 1].
Table 3.
Comparison of pre- and posttest scores of domains on rabies among medical students (n=156)
| Domains | Mean±SD |
Z score |
P* | |
|---|---|---|---|---|
| Pretest score | Posttest | |||
| Epidemiology | 6.09±3.74 | 8.09±3.22 | −6.79 | <0.01 |
| PrEP and PEP | 7.95±5.1 | 13.26±4.56 | −9.43 | <0.01 |
| Program guidelines | 0.85±1.3 | 1.35±1.18 | −5.07 | <0.01 |
| Total score | 14.90±3.70 | 22.70±3.23 | −9.37 | <0.01 |
*Wilcoxon signed-ranks test. SD=Standard deviation, PEP=Postexposure prophylaxis, PrEP=Preexposure prophylaxis
Figure 1.
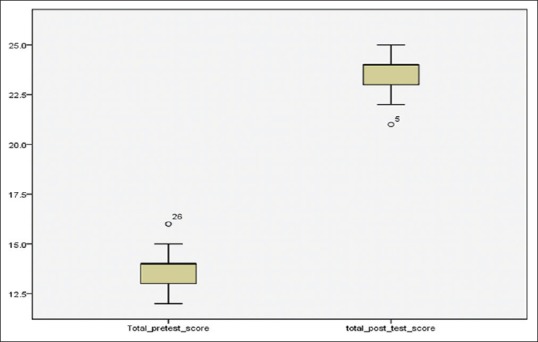
Comparison of pretest and posttest total scores of the study participants (n = 156)
Discussion
In the present study, it was found that there has been a statistically significant improvement in the total scores after health education. The mean pretest scores for epidemiology, prophylaxis, and national program guidelines domains were 6.09 (60.1%), 7.95 (46.8%), and (42.5%) respectively. The knowledge pertaining to epidemiology domain was much better compared to knowledge pertaining to PrEP and PEP and national program guidelines.
In our study, adequate knowledge on epidemiology of rabies, correct prophylaxis, and prescribed program guidelines was found in 75.7%, 42.4%, and 70.8% of study participants respectively. The present study results were found to be similar with previous study findings.
A study done by Praveen and Rajashekar reported that 42.2%–97.7% of the participants were aware of the various aspects of epidemiology and transmission and 2.2%–61.1% were aware of the various aspects of PEP.[7] Shashikantha et al. reported that 74% of the study participants were aware of dog bite as the mode of transmission, 68.8% about hydrophobia as a sign of rabies, 62%–72% about the different categories of wounds, and 10%–52% about the various aspects of PrEP and PEP.[8] Chowdhury et al. in their study conducted on medical interns have reported that 27.5%–95% were aware of the different categories of wounds, 10%–73.8% about the various aspects of vaccine administration, 10%–85% about the various aspects of immunoglobulin administration, and 60%–77% about the various aspects of wound management.[9] A study by Jana et al.[10] reported that awareness regarding prophylaxis in general population was comparatively less (43.5%), and in a study by Prakash et al.,[11] the authors reported that 55.5% of the participants are aware of prophylaxis of rabies after dog bite. A study by Sarkar et al.[12] found that only 50% of students were aware about ARV schedule.
After health education, it was observed that there has been significant improvement in adequate knowledge in epidemiology (93.1%), prophylaxis (97%), and program guidelines (93.8%) domains. There was increase in post test scores for the domains like epidemiology of rabies, PrEP and PEP and national program guidelines. The scores were 8.09 (80.1%), 13.26 (78%) and 1.09 (54.5%) respectively which was found to be statistically significant. Practical oriented teaching of management of animal bites as per health program guidelines and periodical, interactive, continued medical education would help in addressing knowledge gaps of students and practicing physicians.
The limitation of the study was that the findings could not generalized since it was single centered study. Multicentric study including both public and private medical schools could have been better in concluding on the strategy followed in this educational intervention.
Conclusions
The baseline knowledge of the study participants pertaining to epidemiology domain of rabies was reasonably good but that pertaining to PrEP and PEP and national program guidelines domains was below par. There has been significant improvement in the scores of all the three domains after educational intervention. PrEP and PEP, and national program domain of rabies need to be emphasized more during health education sessions. Animal bite cases are more common at all medical institutions (both public and private), and lack of adequate knowledge on rabies prophylaxis and health program guidelines would lead to loss of lives of patients which could have been otherwise saved.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank all the study participants who agreed to participate in pre- and postintervention session.
References
- 1.World Health Organization. Rabies. [Last accessed on 2017 Nov 09]. Available from: http://www.who.int/mediacentre/factsheets/fs099/en/
- 2.World Health Organization. WHO Expert Consultation on Rabies. Second Report. Technical Report Series No. 982. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 3.World Health Organization. Rabies Vaccines: WHO position paper. Wkly Epidemiol Record. 2010;85:309–20. [Google Scholar]
- 4.Sudarshan MK, Mahendra BJ, Madhusudana SN, Ashwoath Narayana DH, Rahman A, Rao NS, et al. An epidemiological study of animal bites in India: Results of a WHO sponsored national multi-centric rabies survey. J Commun Dis. 2006;38:32–9. [PubMed] [Google Scholar]
- 5.Sudarshan MK, Madhusudana SN, Mahendra BJ, Rao NS, Ashwath Narayana DH, Abdul Rahman S, et al. Assessing the burden of human rabies in India: Results of a national multi-center epidemiological survey. Int J Infect Dis. 2007;11:29–35. doi: 10.1016/j.ijid.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Rosner B. 4th ed. Boston, USA: Duxbury Press; 1995. Fundamentals of Biostatistics; p. 221. [Google Scholar]
- 7.Praveen G, Rajashekar HK. Knowledge, awareness and perception of medical college students on rabies and its prevention. Int J Med Sci Public Health. 2014;3:1484–6. [Google Scholar]
- 8.Shashikantha SK, Sheethal MP, Shashank KJ. Awareness among students of a medical college regarding management of animal bite in Bijapur, Karnataka. Natl J Community Med. 2017;8:421–4. [Google Scholar]
- 9.Chowdhury R, Mukherjee A, Naskar S, Lahiri SK. A study on knowledge of animal bite management and rabies immunization among interns of a government medical college in Kolkata. Int J Med Public Health. 2013;3:17–20. [Google Scholar]
- 10.Jana PK, Sarkar TK, Chellaiyan DV, Adhikary M, Jha SN. Rabies menace and control – Knowledge, awareness, and practices among patients in a tertiary care hospital in West Bengal. Int J Med Sci Public Health. 2017;6:1–4. [Google Scholar]
- 11.Prakash M, Bhatti VK, Venkatesh G. Rabies menace and control – An insight into knowledge, attitude and practices. Med J Armed Forces India. 2013;69:57–60. doi: 10.1016/j.mjafi.2012.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sarkar A, Bhavsar S, Bundela C, Gohel A, Makwana N, Parmar D. An assessment of knowledge of prevention and management of Rabies in interns and final year students of Shri M. P. Shah Government Medical College, Jamnagar, Gujarat. J Res Med Dent Sci. 2013;1:62–6. [Google Scholar]


