Abstract
CONTEXT:
Mass gatherings (MGs) are established for different religious, social, political, cultural, and sport motivations. Many risks threaten the participants’ health in MGs for different reasons. One duty of health-care system is to identify the risks and manage them to reduce the participants’ injuries in MGs. This study aimed to identify and classify the risks threatening the health of participants in MGs and review related articles systematically.
SUBJECTS AND METHODS:
In this study, we investigated electronic databases including Science Direct, PubMed, Ovid, ProQuest, Web of Science, Scopus, and Google Scholar. This systematic review investigated those health articles which studied MGs published after 2000. Keywords that were searched included (Mass gathering OR Crowd) AND (Assessment OR Evaluation) AND (Disaster OR Emergencies) AND (Injuries OR Stamped). The final full text articles were assessed qualitatively by STROBE article assessment checklist, and then the data extracted from the results of the articles were analyzed and reported.
RESULTS:
Initially, a total of 1874 articles were found, qualitative exclusion and inclusion criteria were applied, and finally 29 full-text articles were selected for the analysis. More than forty health-related risks were recognized. In order to better understand the risks and use of the results more efficiently, the risks were classified and reported into the following five domains: environmental risks, individual risks, psychological risks, public health risks, and management risks.
CONCLUSION:
Many risks threaten the health of participants in MGs. Recognizing and managing the risks are considered the primary and basic essentials of health sector for the better management of MGs.
Keywords: Health, mass gatherings, risk assessment, risk evaluation
Introduction
Mass gatherings (MGs) are held for religious, social, cultural, political, and sport reasons, and they harbor health risks and events. Over the past decade, concerns have increased about health-related risks.[1] According to the World Health Organization (WHO), a MG is a planned or unplanned event in which planning and responsible resources are under pressure at local, state, or national level due to the large number of people.[2]
The main concerns of health-care system in MGs include infectious diseases such as diseases transmitted through the respiratory system, foodborne diseases, waterborne diseases, injuries, car crashes, heat exhaustion, insect bites, noncommunicable diseases, and terrorism.[3]
Most gatherings reported communicable diseases, noncommunicable diseases, injuries due to stampede, and terrorist attacks to cause high death rates.
In addition to the endemic and seasonal diseases (due to water, food, and respiratory diseases), the health system is faced with muscle strain, dizziness, headaches, asthma and respiratory problems, limb amputation, heat stroke, and abdominal pain, all of which demand special care.
Indeed, these events are considered complicated health challenges locally, nationally, and internationally.[4] Studies on health system response in Hajj MGs, a great MG, reported influential factors of health system's response such as gathering size, population density, weather, and amount of health facilities available to participants.
Hajj clinical issues are classified into communicable and noncommunicable diseases. Concerning communicable diseases, concerns include communicable respiratory and digestive diseases. However, in noncommunicable diseases, the health system encounters health problems such as accidents arising due to population pressure, fire events, terrorism, and heat exhaustion in Hajj customs.[5]
In addition to the abovementioned issues, the participants in MGs will face some psychological changes, and these changes may have a negative impact and consequently cause some risks to people's health.[6] The statistics throughout the world report various risks of MGs. Considering Hajj customs, 1426 individuals died in 1990, 270 in 1994, 118 in 1998, 35 in 2001, 14 in 2003, 251 in 2004, and 3 in 2000 from thirty countries.[7] Meanwhile, other statistics reported that 249 people were injured at a stadium in Britain in 1989, 249 in a religious ceremony in India in 2008, 450 in a bridge accident in Cambodia's capital in 2010, and 89 in a temple in India were injured due to pressure from the population mass.[8]
In this regard, the goal of the health-care system is to provide services to population in MGs, prevent and reduce injuries, prevent and reduce disease infection risks, and increase the safety level of the participants. The health system is faced with immense and complicated challenges to reach their objective.[9,10]
When numerous people gather in a defined place, they are threatened by different health problems. The risks of gatherings are related both to the participants’ number and different factors.[11] Disaster risks associated with MGs are directly related to the existing hazards, exposure level, and vulnerability of the population and environment.[1]
In order to provide efficient health resources and equipment, managers of MG administrators should have reliable data about the different aspects of gathering establishment.[12] Most injuries of individuals in MGs originate from lack of risk management strategies.[8,10]
For proper management of MGs and to fulfill preventive thoughts and risk reduction, risk factors and health risk potentials in MGs should be recognized in the first step so that a comprehensive risk assessment is performed. In other words, one can analyze and evaluate risks after recognizing them and study the occurrence of events and the effects on the participants.[8,10,13,14]
Accordingly, this present study was designed to identifying the risks that threaten the health of people participating in MGs. Moreover, we aimed to classify these risks in a clear domain for better perception.
Subjects and Methods
In this study, we investigated electronic databases including Science Direct, PubMed, Ovid, ProQuest, Web of Science, Scopus, and Google Scholar. Keywords including MG, disaster risks, disaster, stampede, and assessment were searched. In order to conduct a comprehensive search, (Mass gathering OR Crowd) AND Risks (Assessment OR Evaluation) AND (Disaster OR Emergencies) AND (Injuries OR Stampede) were used in all database searches. Inclusion criteria of the study included articles in English, published after 2000 with full text. On the other hand, exclusion criteria involved non-English published articles and those published before 2000, articles with lack of full text, review articles, and books.
Data extraction
In order to prevent any bias in the study, data extraction and qualitative evaluation of the articles were accomplished by two independent researchers. Thus, two separate forms were designed. The first one included general information of the articles including publishing year, study year, type of MGs, type of participants in gatherings, methodology of the article, and finally health risk factors reported in the study. The second form evaluated the articles qualitatively; for this reason, STROBE 22-item standard checklist was used.
Results
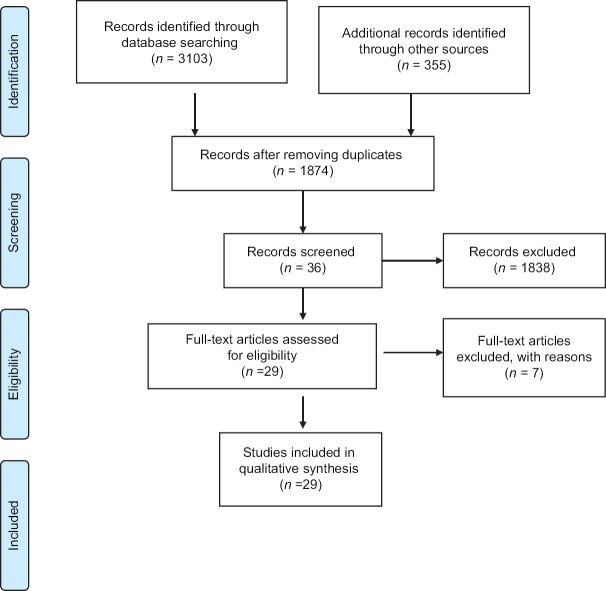
A total of 3103 articles were identified in the first survey by keywords in international resources. Furthermore, 355 more articles were added in manual Google Scholar research. As a result, the first survey included 3458 related articles, of which 1584 articles were removed due to being duplicated. After reading the abstract of 1874 articles, 1838 articles were excluded. Most studies excluded were review articles, editorial letter, and those with no available full text.
Consequently, 36 related articles entered the study for full-text evaluation based on the inclusion criteria. In this step, 7 articles were excluded after reviewing the full text as the results reported in them were irrelevant. Finally, 29 articles were included in the present study for data extraction.
Figure 1 depicts the flow diagram representing the way in which the articles were identified in this study based on the PRISMA flow diagram.
Figure 1.
PRISMA flow diagram
After qualitative evaluation of the final articles and studying their full text, the information and results extracted are presented in Table 1. In this table, in addition to the general information in the article, the health risks in MGs are presented for each study.
Table 1.
Health-related risks in mass gatherings based on the articles included in the study
| Authors and references | Publication date | Methodology | Mass gathering type | Health risks | Study conclusion |
|---|---|---|---|---|---|
| Hutton et al.[15] | 2012 | Pilot study to assess the tool (cross-sectional) | Music festival | Crowd behavior (“jumping up and down”). Crowd mood (energetic). Crowd type (participatory and cohesive). Presence of alcohol and drugs. Crowd density. Temperature and humidity | We need to explore the interaction of MG domains by further research |
| Perron et al.[16] | 2005 | Retrospective study | Games | Heat index (high) | Cold-related correlation will be researched |
| Alqahtani et al.[17] | 2017 | Cross-sectional surveys | Hajj, religious | Lack of some pilgrims’ awareness about the risk of accidents such as stampedes | In the pretravel briefing, injuries and personal safety must be mentioned |
| Bledsoe et al.[18] | 2012 | Retrospective, observational | Art festival | Lack of paramedic or physician. Attendance size. Significant distance. Austere environment | Our experience is useful for similar event |
| Sokhna et al.[19] | 2017 | Cross-sectional | Socio-religious | Road traffic accidents, heatstroke, terrorist attacks, cholera outbreak, infectious diseases | In the context that available medical resource is limited, international collaboration is needed |
| Selig et al.[12] | 2013 | Observational, retrospective | Race weekend | Weather factors such as temperature, precipitation, and humidity | Weather data influence the use of medical services |
| Dong et al.[20] | 2017 | Cross-sectional report | New year | Density of crowd, lack of flow direction, lack of self-protection awareness, environmental factors, lack of risk assessment, and lack of surveillance system and communications | Government must improve the fast emergency reaction in MG events |
| Feldman et al.[21] | 2016 | Retrospective, cross-sectional | Games | High temperatures | Individual education has an important role in prevention and improvement behaviors |
| Ma et al.[22] | 2002 | Cross-sectional | Games | Alcohol consumption | Alcohol drinking was responsible for most events |
| Alqahtani et al.[23] | 2016 | Cross-sectional | Hajj, religious | Lack of pre-event advice | We have to progress the participants’ awareness and have better communication with them |
| Gocotano et al.[24] | 2015 | Lessons from the field | Religious visit | Cold weather | Information accumulation from the venue is important to event assessment |
| Blumberg et al.[25] | 2016 | Cross-sectional | Sport event | Lack of pretravel vaccination. Lack of surveillance system | To encounter communicable disease, enhanced surveillance system is needed |
| Joseph et al.[26] | 2016 | Cross-sectional | Religious | Human stampedes, person-to-person communicable disease, lack of coordination, shortage of paramedical staff, difficulty in access to medical facilities | The findings are useful for any health sector for risk factor assessment in MGs |
| Cariappa et al.[27] | 2015 | Lessons from the field. Cross-sectional | Religious | Quality assurance of food and water, disease monitoring and surveillance, water sanitation, disposal of solid and liquid waste, allocation of medical resources | MG management requires modern medical services, sufficient funding, planning, and preparation |
| Hutton et al.[28] | 2010 | Cross-sectional | Mobile MG | Access to food and water, overcrowding | Health is an important issue in young minds who participate in MGs |
| Memish et al.[29] | 2015 | Cross-sectional | Religious (Hajj) | Crowded conditions | International MGs can provide a ground for globalization of a pathogen |
| Shirah et al.[30] | 2016 | Retrospective cohort analysis | Religious (Hajj) | Participants aged >50 years and participants with chronic diseases | Health workers’ and participants’ adherence to preventive measures is very effective in preventing the spread of diseases |
| Arbon et al.[31] | 2001 | Cross-sectional. Model creation | All types | Crowd size, weather, mobility of the crowd, availability of alcohol, number of patient care personnel on duty | For better health-care planning in MGs and predicting the rate of patients, we need to model making research |
| Locoh-Donou et al.[32] | 2016 | Retrospective | Mix (outdoor and indoor) | Outside and unbounded venues, absence of free water, no climate control, percentage of (occupied) seating, increase in heat index | The findings are useful for EMS resource providing before MGs |
| Kemp[33] | 2016 | Prospective, observational | Not mentioned | Lack of trained and experienced advanced nurse practitioners | Presence of professional nurses to reduce patient referral rates is very helpful |
| Grant et al.[34] | 2010 | Case study | Multi-day | Gender (female), age (increase) | Must notice at-risk participants |
| Khan et al.[35] | 2017 | Cross-sectional | Hajj, religious | Old age | Health-care system must improve the knowledge of participants about their health status and preventive measures |
| Grange et al.[36] | 2016 | Prospective, observational | Motor sports | Lack of on-site physicians | Presence of physician on the venue reduces the patient transportation and EMS workload |
| Hutton et al.[37] | 2010 | Framework evaluation | Scholes event | Alcohol consumption | Further evaluation is needed to judge this model |
| Polkinghorne et al.[38] | 2013 | Cross-sectional. Mix method | Music festival | Duration of MG, heat-related ailments | MGs in rural areas are facing more challenges due to limited resource and infrastructure and hence require more comprehensive planning |
| Balsari et al.[39] | 2016 | Cross-sectional, case study | Religious festival | Density of people, waterborne infection, and disease | To better communicate between the organizations in disasters, we need a incidence command system |
| Eberhardt et al.[40] | 2016 | Case-control | Sport | Insect bites, sunburns | The risks of participants in sport MGs are different from those of other travelers |
| Vortmann et al.[41] | 2015 | Mix method | Religious festival | Waterborne disease | As the number of people will increase in the coming years, the likelihood of disaster will increase |
| Zeitz et al.[42] | 2003 | Retrospective analysis | All types | Crowd size, daily temperature, humidity, day of the week | Historical experiences analysis is very useful to design a management framework |
MGs=Mass gatherings, EMS=Emergency medical service
According to the results, more than forty risks were recognized to be threatening the participants’ health in MGs.
Table 2 summarizes the extracted risks of articles according to individual domains. To better recognize the risks and for better analysis and understanding, the risks were classified into the following five domains: environmental risks such as heat, cold, humidity of environment; individual risks such as age and sex; risks related to public health such as water and food health; psychological risks such as participants’ behavior and risks associated to MGs; and management risks such as risk assessment and availability of caregiver personnel. Note that some of the risks overlapped in two or three domains, and thus were included in the dominant domain.
Table 2.
Risks threatening the health participants in mass gatherings based on domains
| Domain | Risks |
|---|---|
| Environmental domain | Crowd density and attendance size,[15,18,20,28,29,31,39,42] mobility of population,[31,42] high temperature[12,15,16,19,20,21,31,38,42] and humidity,[12,15,20,31,38,42] significant distance,[18] austere environment,[18] traffic accidents,[19] precipitation,[12] cold weather,[24] outside (external) and unbounded venues,[32] insect bites,[40] sunburns[40] |
| Psychological domain | Crowd behavior (jumping up and down), crowd mood (energetic), and crowd type (participatory and cohesive).[15] Presence of alcohol and drugs[15,22,37] |
| Individual domain | Lack of awareness about the risk of accidents,[17] lack of self-protection awareness,[20] participants with chronic disease,[30] gender (female),[34] age (increase) or old age[30,34.35] |
| Public health domain | Probability of outbreak and pretense of infectious disease,[19,26,41] quality assurance of food and water,[27] water sanitation and hygiene,[27,41] disposal of solid and liquid waste,[27] lack of disease monitoring and surveillance system[20,25,27] |
| Management domain | Lack or shortage of paramedic or physician or patient care personnel on duty,[18,26,31,33,36] terrorist attack,[19] lack of flow direction,[20] lack of risk assessment,[20] lack of disease monitoring and surveillance system,[20,25,27] lack of communications,[20] lack of pre-event advice,[23] lack of pre-event vaccination,[25,26] lack of coordination,[26] difficulty in access to medical facilities,[26] allocation of medical resources,[27] access to food and water,[28] availability of alcohol,[15,31] absence of free water (i.e., without cost),[32] duration of MG[38] |
MG=Mass gathering
Discussion
Many studies have been conducted on the health of participants in MGs. Most studies attempted to report health risks in a particular gathering or were based on prior models and were studied in one domain. Because our study objective was achieving maximum risk numbers in MGs, using a systematic review of the studies, different risks were recognized which were finally classified into five domains based on risks’ type. The following classification will be useful for better understanding and application of the results in MG management.
Environmental risk domain
In the present study, environmental risks threatening the health of participants in MGs included weather risks such as cold, environmental heat,[12,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42] precipitation,[12] higher humidity,[12,15,20,31,38,42] long distance of gatherings and austere environment,[18] mobility of population,[31,42] gatherings in outside (external) and unbounded venues,[32] MGs exposed to traffic accidents,[19] the participants’ number and crowd density,[15,18,20,28,29,31,39] insect bites, and sunburns.[40]
An important risk that threatens the health participants in MGs seems to be weather and climate conditions. Specifically, heat exhaustion and humidity as a morbid factor and even death have been reported in MGs.
Heat-related diseases that occur due to long exposure to heat, especially in outdoor gatherings, can be reduced.[43] Administrative managers should provide facilities such as adequate shade structures, chiller, cooling station, and sprinkler as well as methods to control the population to prevent such risks.[5,43,44,45] Furthermore, insect and arthropod bites were reported as health-threatening risks in the World Cup 2014 in Brazil. The participants are told to wear suitable clothes and cover exposed areas, while the health-care system had to prepare itself to recognize and treat the affected people.[46]
Population density is considered the main threat to health risks of the participants in MGs, which causes death and various injuries due to population pressure, trampling, and being strangled.[5,8,45,47,48] Only in the Hajj ceremony, hundreds of people lose their lives or are injured due to population density and pressure.[5,7]
In addition, significant statistics of injuries due to population pressure in MGs have been reported in other areas of the world.[8] Evidence also indicates that increasing population density increases the risk of communicable infectious diseases.[5,46,48,49] Further, increase in the extension and number of participants will amplify the health risks,[14] and it has been demonstrated that mobile populations generated more workload for emergency services than seated populations.[50] The epidemiological process of spreading diseases depends on factors such as pedestrian population, transportation type, and the duration and spatial extension of MGs.[51]
It is possible to manage this important risk through pre-event assessment, early warning systems, as well as population management and control methods including population simulating models, participants’ grouping, and using novel technologies.[8,47,51,52]
Risk of sunburn is higher in open-area gatherings. In addition to the short-term effects such as skin reaction, heat exhaustion, and dehydration, the light radiated from the sun causes other consequences such as cataracts and skin cancer. The participants should be trained about wearing suitable clothing, using sunscreens, and, as far as possible, moving and remaining in shady spaces.[53,54] In unbounded MGs, controlling the venue capacity is very difficult. Instead, in bounded venue like a stadium with fixed seats, planners have some control over the number of participants.[55] Traffic accidents and being drawn were reported as fatal causes and injuries of participants in the summer Olympics in Greece. Furthermore, a portion of injuries of Hajj participants were due to traffic accidents.[45,54]
It is suggested that participants in gatherings pay more attention to warnings in the field and be trained about safety measures.[54]
Public health risk domain
In public health domain, risks that threaten the participants’ health in MGs extracted from the study included probability of outbreak and spread of infectious diseases,[19,26,41] unsuitable sanitation and hygiene of water and improper food quality,[27,41] improper disposal of wet and dry waste,[27] and finally lack of disease monitoring and surveillance systems.[19,25,27]
The risk of spreading infectious diseases including respiratory tract infections, gastrointestinal infections, and skin infections is increasing in MGs.[5,45,56] Control of communicable diseases in the mass rallies is a very critical challenge because the outbreak of a disease in MGs can be a precursor to its spread to the entire community.[57]
In international MGs, a disease outbreak such as flu and measles is rarely seen due to vaccination protocol for diseases, while the outbreaks have mainly focused on gastrointestinal diseases. This fact further illustrates the importance of efforts on water and food health of the participants.[58] In addition, it was observed that the outbreak of waterborne disease with various pathogens (parasites, bacteria, and viruses) occurred due to the lack of personal and public hygiene and insufficient vaccination coverage.[58] Further, in addition to water sanitation, similar supervision should be considered for ice sources as well.[56] Due to the provision of safe drinking water during the Hajj, the risk of waterborne diseases is low. However, the use of ice cubes from unknown source for cool water and beverages has increased the risk of contamination.[59]
A vaccination program can reduce the incidence of infectious diseases, especially in international gatherings. In gatherings such as Hajj and Olympic games, a suggestive vaccination protocol should be designed, based on endemic disease, the participants’ conditions, and other specific factors.[13,49,56]
The country which hosts MGs should consider necessary planning based on its endemic communicable disease to reduce epidemic risk. Participants who travel to areas with higher prevalence of malaria should be assessed and if necessary, prophylactic treatment should be done according to the protocol. In addition to designing instructions for endemic and seasonal diseases, it is useful to have a preventive plan and disease monitoring system.[46]
Other studies suggested that recognizing the disease, reporting it, and monitoring system are necessary for disease diagnosis and preventing breakout.[5,48,54,56,60,61] Furthermore, disease surveillance systems can be useful and effective in the recognition of bioterrorism attacks.[54,60]
Inappropriate management of public and environmental health in MGs threatens the health and welfare of the participants and staff. Health managers have to notice the essential needs of individuals such as adequate public toilettes, sufficient cooling devices for frozen food, health food supplies, facilities for dry and wet waste disposal, and insect and rodent control.[51]
Individual risk domain
In the present study, individual risks threatening the participants health in MGs included lack of awareness about the risk of accidents,[17] lack of self-protection awareness,[20] participants with chronic disease,[30] as well as women's and elderly's presence.[30,34,35] Handwashing, using mask, and maintaining distance from others were considered as preventive factors; although for participants, especially the elderly, the use of masks was considered difficult in hot weather.[62] However, it is difficult to maintain social space and avoid contact with other participants in MGs, in this reason. Personal preventive activities such as mask utilization and handwashing may be suggested.[63]
The risk of presence of elders in MGs seems to be related to both chronic disease and inability for self-protection, which is a threat to their health.
According to suggestions of the WHO in Hajj, people aged above 65, those who are affected by a chronic disease, pregnant women, and children aged below 12 should receive vaccine injection according to the protocol and engage in more protective measures such as using a mask, washing hands, and keeping a distance from others.[64] Meanwhile, many articles reported deaths due to heat loss of the elderly and those due to the underlying disease.[5]
In walking gatherings, the groups with men and women in comparison to groups with only men had a lower moving speed, more population distance, and more population gap.[65] Risks related to individual risks indicated that authorities of MGs should cover information of participants such as age, sex, existing disease, awareness, and education level before gatherings so that necessary predictions can be provided accordingly.
Psychological risk domain
In this systematic review, the psychological risks threatening participants’ health in MGs included crowd behavior (jumping up and down), crowd mood (energetic), and crowd type (participatory and cohesive),[15] as well as alcohol or drug consumption.[15,22,37] On this basis, in the psychological domain, MGs with alcohol presence, jumping up and down (crowd behavior), energetic (crowd mood), and participatory and cohesive (crowd type) characteristics had the most risks.
The types of MGs influence the behavioral risks of people. For example, risks of a rock music concert are different from those of the Hajj. Meanwhile, failure in the successful implementation of other dimensions of health in MGs will cause stress in participating individuals and change their psychological status, thereby creating further risks.[6] Population behavior is affected by excitement such as fear, anger, and passion. Such excitement may reach an extreme level under particular conditions and be inducted to the whole population contagiously. Therefore, psychological conditions of the participants may result in intensified effects on the safety of population.[52] Knowing factors that result in behavioral change of people and consequently behavioral changes in the population is crucial. One of them is alcohol consumption by individuals.[53,66] In a review by Steffen et al. entitled “noncommunicable health in mass gatherings” in 2012, alcohol and drug consumptions were reported as noncommunicable risk factors in MGs, resulting in trauma and poisoning.[4] Crimes are reported less in Hajj gatherings due to lack of alcohol and drug consumption.[67] In music festivals involving alcohol consumption, there is an increased risk of sexually transmitted disease risks.[58]
Considering the psychological condition of the participants, identifying risks and recognizing psychological changes of the participants and the population in MGs play a key role in the domain management. Behavioral change in a part of the population may be considered as a spark to changes in the behavior across the entire population. The population behavior and resulted changes should be studied to prevent the associated risks.
Through risk assessment before gatherings, health-care systems recognize the risks and prepare for the required provisions to confront probable events.[53,66] Furthermore, risks associated with alcohol consumption can be minimized in MGs by forbidding alcohol and drug use.[4,44]
Management risk domain
In this study, the risks due to lack of support on resources and inefficiency of gatherings’ safety recognized in this domain were reported as Lack or shortage of patient care workers such as Physicians or Paramedics;[18,19,26,31,33,36] flow directions;[20] risk assessment;[20] communication;[20] pre-event advice;[23] a plan for vaccination before gatherings;[25,26] coordination;[26] free water as well as terrorist attacks; difficult access to water and food;[28] difficult access to medical facilities;[26,27,32] and duration of MG.[38]
One of the factors reducing the health risks in MGs is the presence of expert medical care staff in MGs including physicians, nurses, and emergency technicians. Presence of medical care staff not only speeds up medical handling but also prevents unnecessary dispatch of ambulance to health-care centers.[68]
Inability to manage the population leads to inadequate access of emergency personnel to the required areas.[51] Therefore, presence of emergency and medical care staff is not sufficient to reduce health-related risks; it is necessary to have separate safe entrance and exit gates for participants in addition to recognized ways for emergency and medical care staff to access all areas in the gatherings.
There are different reports concerning deaths and injuries caused by this problem.[68] Basic provisions such as plans and practices before gatherings, providing security of place of gatherings, providing radio communication and integrated command and control, being connected to urban and national services, and resource management should be accomplished for emergency staff to access all gathering areas.[10,69] On the other hand, in gatherings with ticket-selling services, extra ticket sales should be prohibited and population saturation should be prevented through proper notification.[68] Because of different reasons such as population density and releasing the news out, the gatherings are regarded as suitable targets for terrorist attacks.[5,54]
Authorities and security forces should consider and practice security arrangements before gatherings as much as possible; the reason is that security measures during gatherings may result in population stimulation and injuries due to population pressure and stampedes. Meanwhile, proper routes of entrance and exit gates should be considered with a particular guidance. This can allow one-way flow of the population at the necessary time.[68]
In order to prepare for successful implementation of MGs, the health department should practice necessary coordination in all parts. Note that it is impossible to implement health plans without cooperating with other sectors in the country. Therefore, the coordination and cooperation should be provided in a complete particular plan between the health ministry and other ministries. Necessary coordination, cooperation, and communications with other organizations such as the WHO should be provided in international gatherings.
Efficient methods should be considered to provide coordination to share data and information at all levels.[13,70] For example, more than 130 health-care centers and 17,000 health-care personnel engage in the Hajj ceremony. It is impossible to manage health-care centers and personnel without planning and a cooperation system. In addition, the health-care system should engage and cooperate with other organizations who are involved in MG management, which requires an effective communication mechanism.[67,70]
Meanwhile, engaging the participants before gatherings is considered a necessary action which plays a key role in health risk reduction in MGs. The provisions include recommendations and different standard plans for participants[45,46,48,57,71,72] and vaccination according to approved protocols.[5,45,46,48,56,58,67,71,72,73]
The duration of the gathering is another issue that should be considered in MGs. It is reported that increasing the duration of MGs has increased the health risks[14] and the workload of emergency services.[50]
Risk assessment is considered a basic pillar of MG management, which plays a significant role in recognizing health risks. Indeed, without recognizing probable risks threatening participants and their extent, it is not possible to accomplish appropriate interventions. Different articles have also acknowledged the importance of risk assessment in identifying and managing health hazards in MGs.[1,4,10,13,14,44,52,58,66,68,70,72,73]
In this study, we identified the health risks of participants in MGs. In addition, for better understanding and functional use, they are reported in five separate domains and discussed each of them individually. Limitation of this research is that included articles are only in English language.
Conclusion
The risks threatening the health of participants in MGs were extracted in this systematic review from 29 final articles. Due to the considerable number and breadth of the results, the recognized risks were classified into the following five domains: risks related to environment, public health, individual features, psychological conditions, and management. Some risks overlapped in one or two domains which were discussed in the dominant domain.
A successful implementation of MGs and reducing risks related to people's health requires attention to all recognized risks and integrated management, as neglecting a risk may threaten the health of all participants.
While different risks threaten the health of people in MGs, operating a MG may result in recognizing the problems and shortages of health-care system, leading to creativity and passion of staff, thereby providing a chance to develop health plans, personnel training, evaluation of the health-care system, as well as testing communication systems along with inter- and intra-coordination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This article was extracted from PhD thesis in Shahid Sadoughi University of Medical Sciences titled “Explanation of health risks associated with MGs and design appropriate risk assessment tool (a mix method study).”
References
- 1.Aitsi-Selmi A, Murray V, Heymann D, McCloskey B, Azhar EI, Petersen E, et al. Reducing risks to health and wellbeing at mass gatherings: The role of the Sendai Framework for Disaster Risk Reduction. Int J Infect Dis. 2016;47:101–4. doi: 10.1016/j.ijid.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Public Health for Mass Gatherings: Key Considerations. WHO, Geneva, Switzerland: 2015. [Google Scholar]
- 3.AlNsour M, Fleischauer A. Public health considerations for mass gatherings in the middle East and North Africa (MENA) region. East Mediterr Health J. 2013;19(Suppl 2):S42–7. [PubMed] [Google Scholar]
- 4.Steffen R, Bouchama A, Johansson A, Dvorak J, Isla N, Smallwood C, et al. Non-communicable health risks during mass gatherings. Lancet Infect Dis. 2012;12:142–9. doi: 10.1016/S1473-3099(11)70293-6. [DOI] [PubMed] [Google Scholar]
- 5.Shujaa A, Alhamid S. Health response to Hajj mass gathering from emergency perspective, narrative review. Turk J Emerg Med. 2015;15:172–6. doi: 10.1016/j.tjem.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hopkins N, Reicher S. The psychology of health and well-being in mass gatherings: A review and a research agenda. J Epidemiol Glob Health. 2016;6:49–57. doi: 10.1016/j.jegh.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salamati P, Rahimi-Movaghar V. Hajj stampede in Mina, 2015: Need for intervention. Arch Trauma Res. 2016;5:e36308. doi: 10.5812/atr.36308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bolia N. B. Risk management strategies to avoid stampede at Mass gatherings. Paper presented at the 2nd World Conference on Disaster Management: Visakhapatnam, Andhra Pradesh, India. 2015 [Google Scholar]
- 9.Alzahrani F, Kyratsis Y. Investigating the role of emergency nurses and disaster preparedness during mass gathering in Saudi Arabia. World Acad Sci Eng Technol Int J Soc Behav Educ Econ Bus Ind Eng. 2016;10:752–7. [Google Scholar]
- 10.Schwartz B, Nafziger S, Milsten A, Luk J, Yancey A., 2nd Mass gathering medical care: Resource document for the national association of EMS physicians position statement. Prehosp Emerg Care. 2015;19:559–68. [PubMed] [Google Scholar]
- 11.Smith WP, Wessels V, Naicker D, Leuenberger E, Fuhri P, Wallis LA, et al. Development of a mass-gathering medical resource matrix for a developing world scenario. Prehosp Disaster Med. 2010;25:547–52. doi: 10.1017/s1049023x00008748. [DOI] [PubMed] [Google Scholar]
- 12.Selig B, Hastings M, Cannon C, Allin D, Klaus S, Diaz FJ. Effect of weather on medical patient volume at Kansas speedway mass gatherings. J Emerg Nurs. 2013;39:e39–44. doi: 10.1016/j.jen.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Al-Tawfiq JA, Memish ZA. Mass gathering medicine: 2014 Hajj and Umra preparation as a leading example. Int J Infect Dis. 2014;27:26–31. doi: 10.1016/j.ijid.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thackway S, Churches T, Fizzell J, Muscatello D, Armstrong P. Should cities hosting mass gatherings invest in public health surveillance and planning? Reflections from a decade of mass gatherings in Sydney, Australia. BMC Public Health. 2009;9:324. doi: 10.1186/1471-2458-9-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hutton A, Zeitz K, Brown S, Arbon P. Assessing the psychosocial elements of crowds at mass gatherings. Prehosp Disaster Med. 2011;26:414–21. doi: 10.1017/S1049023X12000155. [DOI] [PubMed] [Google Scholar]
- 16.Perron AD, Brady WJ, Custalow CB, Johnson DM. Association of heat index and patient volume at a mass gathering event. Prehosp Emerg Care. 2005;9:49–52. doi: 10.1080/10903120590891976. [DOI] [PubMed] [Google Scholar]
- 17.Alqahtani AS, Yamazaki K, Alqahtani WH, Tashani M, Heywood AE, Booy R, et al. Australian Hajj pilgrims’ perception about mass casualty incidents versus emerging infections at Hajj. Travel Med Infect Dis. 2017;15:81–3. doi: 10.1016/j.tmaid.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bledsoe B, Songer P, Buchanan K, Westin J, Hodnick R, Gorosh L, et al. Burning man 2011: Mass gathering medical care in an austere environment. Prehosp Emerg Care. 2012;16:469–76. doi: 10.3109/10903127.2012.695432. [DOI] [PubMed] [Google Scholar]
- 19.Sokhna C, Mboup BM, Sow PG, Camara G, Dieng M, Sylla M, et al. Communicable and non-communicable disease risks at the Grand Magal of Touba: The largest mass gathering in Senegal. Travel Med Infect Dis. 2017;19:56–60. doi: 10.1016/j.tmaid.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Dong YH, Liu F, Liu YM, Jiang XR, Zhao ZX. Emergency preparedness for mass gatherings: Lessons of “12.31” stampede in Shanghai Bund. Chin J Traumatol. 2017;20:240–2. doi: 10.1016/j.cjtee.2016.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feldman LY, Gao C, Zhu J, Simatovic J, Licskai C, To T. Estimating Toronto's health services use for the 2015 Pan American and Parapan American games. Perspect Public Health. 2016;136:93–8. doi: 10.1177/1757913915612820. [DOI] [PubMed] [Google Scholar]
- 22.Ma OJ, Millward L, Schwab RA. EMS medical coverage at PGA tour events. Prehosp Emerg Care. 2002;6:11–4. doi: 10.1080/10903120290938706. [DOI] [PubMed] [Google Scholar]
- 23.Alqahtani AS, Wiley KE, Tashani M, Willaby HW, Heywood AE, BinDhim NF, et al. Exploring barriers to and facilitators of preventive measures against infectious diseases among Australian Hajj pilgrims: Cross-sectional studies before and after Hajj. Int J Infect Dis. 2016;47:53–9. doi: 10.1016/j.ijid.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gocotano AE, Dico FD, Calungsod NR, Hall JL, Counahan ML. Exposure to cold weather during a mass gathering in the Philippines. Bull World Health Organ. 2015;93:810–4. doi: 10.2471/BLT.15.158089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blumberg L, Regmi J, Endricks T, McCloskey B, Petersen E, Zumla A, et al. Hosting of mass gathering sporting events during the 2013-2016 ebola virus outbreak in West Africa: Experience from three African countries. Int J Infect Dis. 2016;47:38–41. doi: 10.1016/j.ijid.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Joseph JK, Babu N, Dev KA, Pradeepkumar A. Identification of potential health risks in mass gatherings: A study from Sabarimala pilgrimage, Kerala, India. Int J Disaster Risk Reduct. 2016;17:95–9. [Google Scholar]
- 27.Cariappa MP, Singh BP, Mahen A, Bansal AS. Kumbh mela 2013: Healthcare for the millions. Med J Armed Forces India. 2015;71:278–81. doi: 10.1016/j.mjafi.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hutton A, Roderick A, Munt R. Lessons learned at world youth day: Collecting data and using postcards at mass gatherings. Prehosp Disaster Med. 2010;25:273–7. doi: 10.1017/s1049023x00008153. [DOI] [PubMed] [Google Scholar]
- 29.Memish ZA, Assiri A, Turkestani A, Yezli S, Al Masri M, Charrel R, et al. Mass gathering and globalization of respiratory pathogens during the 2013 Hajj. Clin Microbiol Infect. 2015;21:571.e1–8. doi: 10.1016/j.cmi.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shirah BH, Zafar SH, Alferaidi OA, Sabir AM. Mass gathering medicine (Hajj pilgrimage in Saudi Arabia): The clinical pattern of pneumonia among pilgrims during Hajj. J Infect Public Health. 2017;10:277–86. doi: 10.1016/j.jiph.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arbon P, Bridgewater FH, Smith C. Mass gathering medicine: A predictive model for patient presentation and transport rates. Prehosp Disaster Med. 2001;16:150–8. doi: 10.1017/s1049023x00025905. [DOI] [PubMed] [Google Scholar]
- 32.Locoh-Donou S, Yan G, Berry T, O’Connor R, Sochor M, Charlton N, et al. Mass gathering medicine: Event factors predicting patient presentation rates. Intern Emerg Med. 2016;11:745–52. doi: 10.1007/s11739-015-1387-1. [DOI] [PubMed] [Google Scholar]
- 33.Kemp AE. Mass-gathering events: The role of advanced nurse practitioners in reducing referrals to local health care agencies. Prehosp Disaster Med. 2016;31:58–63. doi: 10.1017/S1049023X15005543. [DOI] [PubMed] [Google Scholar]
- 34.Grant WD, Nacca NE, Prince LA, Scott JM. Mass-gathering medical care: Retrospective analysis of patient presentations over five years at a multi-day mass gathering. Prehosp Disaster Med. 2010;25:183–7. doi: 10.1017/s1049023x00007950. [DOI] [PubMed] [Google Scholar]
- 35.Khan ID, Khan SA, Asima B, Hussaini SB, Zakiuddin M, Faisal FA, et al. Morbidity and mortality amongst Indian Hajj pilgrims: A 3-year experience of Indian Hajj medical mission in mass-gathering medicine. J Infect Public Health. 2018;11:165–70. doi: 10.1016/j.jiph.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grange JT, Baumann GW, Vaezazizi R. On-site physicians reduce ambulance transports at mass gatherings. Prehosp Emerg Care. 2003;7:322–6. doi: 10.1080/10903120390936518. [DOI] [PubMed] [Google Scholar]
- 37.Hutton A, Munt R, Zeitz K, Cusack L, Kako M, Arbon P. Piloting a mass gathering conceptual framework at an Adelaide Schoolies Festival. Collegian. 2010;17:183–91. doi: 10.1016/j.colegn.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 38.Polkinghorne BG, Massey PD, Durrheim DN, Byrnes T, MacIntyre CR. Prevention and surveillance of public health risks during extended mass gatherings in rural areas: The experience of the Tamworth country music festival, Australia. Public Health. 2013;127:32–8. doi: 10.1016/j.puhe.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 39.Balsari S, Greenough PG, Kazi D, Heerboth A, Dwivedi S, Leaning J, et al. Public health aspects of the world's largest mass gathering: The 2013 Kumbh mela in Allahabad, India. J Public Health Policy. 2016;37:411–27. doi: 10.1057/s41271-016-0034-z. [DOI] [PubMed] [Google Scholar]
- 40.Eberhardt KA, Vinnemeier CD, Dehnerdt J, Rolling T, Steffen R, Cramer JP. Travelers to the FIFA world cup 2014 in Brazil: Health risks related to mass gatherings/sports events and implications for the summer Olympic games in Rio De Janeiro in 2016. Travel Med Infect Dis. 2016;14:212–20. doi: 10.1016/j.tmaid.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 41.Vortmann M, Balsari S, Holman SR, Greenough PG. Water, sanitation, and hygiene at the world's largest mass gathering. Curr Infect Dis Rep. 2015;17:461. doi: 10.1007/s11908-015-0461-1. [DOI] [PubMed] [Google Scholar]
- 42.Zeitz KM, Schneider DP, Jarrett D, Zeitz CJ. Mass gathering events: Retrospective analysis of patient presentations over seven years. Prehosp Disaster Med. 2002;17:147–50. doi: 10.1017/s1049023x00000376. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention (CDC) Surveillance for early detection of disease outbreaks at an outdoor mass gathering – Virginia, 2005. MMWR Morb Mortal Wkly Rep. 2006;55:71–4. [PubMed] [Google Scholar]
- 44.Tam JS, Barbeschi M, Shapovalova N, Briand S, Memish ZA, Kieny MP. Research agenda for mass gatherings: A call to action. Lancet Infect Dis. 2012;12:231–9. doi: 10.1016/S1473-3099(11)70353-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ahmed QA, Arabi YM, Memish ZA. Health risks at the Hajj. Lancet. 2006;367:1008–15. doi: 10.1016/S0140-6736(06)68429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gallego V, Berberian G, Lloveras S, Verbanaz S, Chaves TS, Orduna T, et al. The 2014 FIFA world cup: Communicable disease risks and advice for visitors to Brazil – A review from the Latin American Society for Travel Medicine (SLAMVI) Travel Med Infect Dis. 2014;12:208–18. doi: 10.1016/j.tmaid.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 47.Alaska YA, Aldawas AD, Aljerian NA, Memish ZA, Suner S. The impact of crowd control measures on the occurrence of stampedes during mass gatherings: The Hajj experience. Travel Med Infect Dis. 2017;15:67–70. doi: 10.1016/j.tmaid.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 48.Shafi S, Dar O, Khan M, Khan M, Azhar EI, McCloskey B, et al. The annual Hajj pilgrimage-minimizing the risk of ill health in pilgrims from Europe and opportunity for driving the best prevention and health promotion guidelines. Int J Infect Dis. 2016;47:79–82. doi: 10.1016/j.ijid.2016.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rashid H, Abdul Muttalif AR, Mohamed Dahlan ZB, Djauzi S, Iqbal Z, Karim HM, et al. The potential for pneumococcal vaccination in Hajj pilgrims: Expert opinion. Travel Med Infect Dis. 2013;11:288–94. doi: 10.1016/j.tmaid.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 50.Zeitz K, Bolton S, Dippy R, Dowling Y, Francis L, Thorne J, et al. Measuring emergency services workloads at mass gathering events. Aust J Emerg Manag. 2007;22:23. [Google Scholar]
- 51.Johansson A, Batty M, Hayashi K, Al Bar O, Marcozzi D, Memish ZA, et al. Crowd and environmental management during mass gatherings. Lancet Infect Dis. 2012;12:150–6. doi: 10.1016/S1473-3099(11)70287-0. [DOI] [PubMed] [Google Scholar]
- 52.Gayathri H, Aparna P, Verma A. A review of studies on understanding crowd dynamics in the context of crowd safety in mass religious gatherings. Int J Disaster Risk Reduction. 2017;25:82–91. [Google Scholar]
- 53.Arbon P. Mass-gathering medicine: A review of the evidence and future directions for research. Prehosp Disaster Med. 2007;22:131–5. doi: 10.1017/s1049023x00004507. [DOI] [PubMed] [Google Scholar]
- 54.Pavli A, Maltezou HC. Travelling to Greece for the summer 2011 special Olympics. Travel Med Infect Dis. 2011;9:135–41. doi: 10.1016/j.tmaid.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 55.Turris SA, Lund A, Hutton A, Bowles R, Ellerson E, Steenkamp M, et al. Mass-gathering health research foundational theory: Part 2 – Event modeling for mass gatherings. Prehosp Disaster Med. 2014;29:655–63. doi: 10.1017/S1049023X14001228. [DOI] [PubMed] [Google Scholar]
- 56.Salmon-Rousseau A, Piednoir E, Cattoir V, de La Blanchardière A. Hajj-associated infections. Med Mal Infect. 2016;46:346–54. doi: 10.1016/j.medmal.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ishola DA, Phin N. Could influenza transmission be reduced by restricting mass gatherings? Towards an evidence-based policy framework. J Epidemiol Glob Health. 2011;1:33–60. doi: 10.1016/j.jegh.2011.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gautret P, Steffen R. Communicable diseases as health risks at mass gatherings other than Hajj: What is the evidence? Int J Infect Dis. 2016;47:46–52. doi: 10.1016/j.ijid.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 59.Rafiq SM, Rashid H, Haworth E, Booy R. Hazards of hepatitis at the Hajj. Travel Med Infect Dis. 2009;7:239–46. doi: 10.1016/j.tmaid.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 60.Paterson BJ, Durrheim DN. The remarkable adaptability of syndromic surveillance to meet public health needs. J Epidemiol Glob Health. 2013;3:41–7. doi: 10.1016/j.jegh.2012.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Parmar P, Thomas D. Public health and mass gathering events: Assessing need for surveillance in Wales, UK. Online J Public Health Inform. 2014;7(1) [Google Scholar]
- 62.Benkouiten S, Brouqui P, Gautret P. Non-pharmaceutical interventions for the prevention of respiratory tract infections during Hajj pilgrimage. Travel Med Infect Dis. 2014;12:429–42. doi: 10.1016/j.tmaid.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hoang VT, Gautret P. Infectious diseases and mass gatherings. Curr Infect Dis Rep. 2018;20:44. doi: 10.1007/s11908-018-0650-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.World Health Organization. Health conditions for travellers to Saudi Arabia for the pilgrimage to Mecca (Hajj) Wkly Epidemiol Rec. 2013;88:343–7. [PubMed] [Google Scholar]
- 65.Chattaraj U, Seyfried A, Chakroborty P. Comparison of pedestrian fundamental diagram across cultures. Adv Complex Syst. 2009;12:393–405. [Google Scholar]
- 66.Zeitz KM, Tan HM, Grief M, Couns PC, Zeitz CJ. Crowd behavior at mass gatherings: A literature review. Prehosp Disaster Med. 2009;24:32–8. doi: 10.1017/s1049023x00006518. [DOI] [PubMed] [Google Scholar]
- 67.Memish ZA, Stephens GM, Steffen R, Ahmed QA. Emergence of medicine for mass gatherings: Lessons from the Hajj. Lancet Infect Dis. 2012;12:56–65. doi: 10.1016/S1473-3099(11)70337-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Soomaroo L, Murray V. Disasters at mass gatherings: Lessons from history. PLoS Curr. 2012;4:RRN1301. doi: 10.1371/currents.RRN1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lund A, Gutman SJ, Turris SA. Mass gathering medicine: A practical means of enhancing disaster preparedness in Canada. CJEM. 2011;13:231–6. doi: 10.2310/8000.2011.110305. [DOI] [PubMed] [Google Scholar]
- 70.Illiyas FT, Mani SK, Pradeepkumar A, Mohan K. Human stampedes during religious festivals: A comparative review of mass gathering emergencies in India. Int J Disaster Risk Reduct. 2013;5:10–8. [Google Scholar]
- 71.Shibl A, Senok A, Memish Z. Infectious diseases in the Arabian Peninsula and Egypt. Clin Microbiol Infect. 2012;18:1068–80. doi: 10.1111/1469-0691.12010. [DOI] [PubMed] [Google Scholar]
- 72.McCloskey B, Endericks T, Catchpole M, Zambon M, McLauchlin J, Shetty N, et al. London 2012 Olympic and Paralympic games: Public health surveillance and epidemiology. Lancet. 2014;383:2083–9. doi: 10.1016/S0140-6736(13)62342-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Enock KE, Jacobs J. The Olympic and Paralympic games 2012: Literature review of the logistical planning and operational challenges for public health. Public Health. 2008;122:1229–38. doi: 10.1016/j.puhe.2008.04.016. [DOI] [PubMed] [Google Scholar]