Abstract
Objectives
Lack of access to safe surgery is seen as a major issue that needs to be addressed. The aim of this study was to understand which combinations of factors relate to high occurrences of unmet needs and disability in Nepal, and consequently, how to focus future work to maximise impact in this country.
Methods
A large population‐based survey was conducted in Nepal in 2014 to evaluate the unmet surgical needs that result in disability. Recorded factors included diseased anatomical areas, disease specifics, disease locations, injury types, reasons for having an unmet need and the types of disability.
Results
Included in the study were 2695 individuals. The anatomical areas facing the highest disabling unmet surgical need were Head (3.9% of population), Groin/Genitalia (2.2% of population) and Extremities (3.6% of population). Four focus areas could be defined. Increase affordability, availability and acceptability of surgical care to non‐traumatic disabling conditions of (i) the eye, and (ii) extremities, and (iii) to traumatic disabling conditions of extremities and finally (iv) increase acceptability of having surgical care for non‐traumatic conditions in the groin and genital area. For the latter, fear/no trust was the main reason for receiving no surgical care despite the resulting shame.
Conclusions
This study defined four focus areas that showed the largest unmet needs that resulted in a perceived disability. For those areas, affordability, availability and acceptability of surgical need to be addressed through technical developments, capacity building and raising awareness.
Keywords: low and middle income country, Nepal, global surgery, unmet need, disability
Abstract
Objectifs
L'absence d'accès à une chirurgie sûre est considérée comme un problème majeur à résoudre. Le but de cette étude était de comprendre quelles combinaisons de facteurs étaient liées aux besoins non satisfaits et aux incapacités au Népal, et par conséquent, comment cibler les travaux futurs pour maximiser l'impact dans ce pays.
Méthodes
Une vaste enquête de population a été menée au Népal en 2014 pour évaluer les besoins chirurgicaux non satisfaits qui entraînent une incapacité. Les facteurs enregistrés comprenaient les zones anatomiques, les spécificités, les localisations de la maladie, les types de blessures, les raisons pour lesquelles les besoins n’étaient pas satisfaits et les types d'incapacité.
Résultats
2695 personnes ont été incluses dans l’étude. Les zones anatomiques impliquées dans des besoins chirurgicaux les plus invalidants étaient les suivantes: tête (3,9% de la population), aine/organes génitaux (2,2% de la population) et extrémités (3,6% de la population). Quatre domaines cibles d'intervention pourraient être définis. Premièrement, augmenter l'accessibilité financière, la disponibilité et l'acceptabilité des soins chirurgicaux aux affections invalidantes non traumatiques de 1) l’œil, 2) des extrémités et 3) aux affections traumatisantes des extrémités, et enfin 4) augmenter l'acceptabilité des soins chirurgicaux pour les affections non traumatiques dans l'aine et les parties génitales. Pour ces derniers, la crainte/l'absence de confiance était la principale raison de ne pas recevoir de soins chirurgicaux malgré la honte qui en résultait.
Conclusions
Cette étude a défini quatre domaines cibles d'intervention qui ont montré les besoins non satisfaits les plus importants ayant entraîné une incapacité perçue. Pour ces domaines, il convient de prendre en compte le caractère abordable, la disponibilité et l'acceptabilité des interventions chirurgicales par le biais de développements techniques, d'un renforcement des capacités et la sensibilisation.
Keywords: PRFI, Népal, chirurgie générale, besoin non atteint, incapacité
Introduction
Nepal is a landlocked country, positioned between China and India, and currently ranking number 149 on the Human Development Index (HDI 0.547) 1. Nepal has a population of 29.3 million, a GDP of USD 2,443 and a Healthcare Expenditure of 6.1% of GDP 1. Vulnerability to multidimensional poverty is faced by 24.3% of the population, of which health is accounting for 32.3% 1. There is a huge disparity between rural and urban locations with poverty indexes of the mid‐ and far‐western regions comparable to sub‐Saharan values 2. 70% of trauma surgeons live in urban areas, whereas 80% of trauma and disability occur in the rural areas where trauma care services are unavailable 3. Only two rehabilitation centres exist in the country. Poverty compels the poor to undertake risky tasks without safety measures. Hence, there is a high prevalence of injury amongst the poor population. Former cultural practices, inability to afford treatment and poor access to health services result in disabilities 4, 5. Those affected are usually breadwinners with numerous dependent family members. This vicious cycle of poverty and disability has negatively affected the socio‐economical backbone of the country.
Access to surgical care has become a global health priority 6, 7. Multidisciplinary approaches should be taken to describe, isolate and address the structural, cultural and financial barriers 7 that limit universal access to safe, affordable and acceptable surgery. This includes, amongst others, local capacity building, developing new surgical procedures, improved training of medical, technical and support staff, medical innovations and local involvement 6, 7, 8, 9, 10, 11, 12. This is true on both the global and the national scale for individual countries like Nepal.
Various studies have described the healthcare situation in the country in different ways. Some studies used hospital data to describe both epidemiology and barriers for health care for specific conditions such as head injuries from traffic accidents in a tertiary centre or a children's hospital reporting mainly congenital problems such as clubfoot. 13, 14. However, this limits the data to patients who had access to hospitals and neglects patients who did not have access. Others used WHO guidelines for emergency care 15 to assess the availability of surgical technology in various governmental hospitals at primary, secondary or tertiary level 16. Deficiencies in equipment and problematic equipment unsuitable for the context were identified. This yields a good overview of the status of medical equipment in the hospitals and of their readiness for essential trauma care, but does not depict the need of the population.
Therefore, an assessment of surgical need from the population's perspective is needed. A large population‐based survey was conducted in 2014 inventorising basic demographic properties and perceived unmet needs and disabilities of the populations of Nepal, Rwanda and Sierra Leone. Various cross‐sections based on this data set were described and published before 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, mainly focusing on Nepal. The aim was to evaluate the unmet surgical needs and perceived disabilities of the people of Nepal. Disability is an important promotor of vulnerability of individuals in society resulting in poorer health outcomes, lower educational achievements, less economic participation, higher rates of poverty, and an increased dependency and restricted participation 32. Often disabilities can be mitigated surgically. Thus, it is important to understand surgical conditions or impairments that cause perceived disabilities but are not surgically met.
Successful future efforts to improve access to, affordability of and availability of surgical care for those disabling conditions or impairments will enable people to have surgery and empower them to participate in society again and therefore, have high impact on their personal well‐being. Not every combination of factors, such as affected anatomical area, disease specifics, affected locations or injury type leading to perceived disabilities, will occur at the same frequency or show the same unmet surgical needs. If future work is to effectively address surgically treatable disabilities, then the most common combinations of factors and their unmet needs must be identified. Therefore, the aim of this study is to visualise which combinations of factors and their categories show high frequencies of unmet needs and perceived disability, and consequently, where to focus future work to maximise its impact.
Methods
Data acquisition
Surgeons OverSeas Assessment of Surgical need (SOSAS) is a cluster‐randomised cross‐sectional countrywide survey with two components described in detail previously 33, 34 conducted in Nepal in 2014. Briefly, the SOSAS survey is divided into two sections. The first section collects demographic data regarding household access to health care and recent deaths in the household. If there was a death in the household within the past year, questions regarding health care received, access to surgical care, barriers to surgical care and specifics of death were asked. The second section randomly selected two household members who each underwent a verbal head‐to‐toe examination of 6 anatomical regions: (i) face, head and neck; (ii) chest and breast; (iii) abdomen; (iv) groin and genitalia; (v) back; and (vi) extremities. All household members were included, except those noted to be mentally disabled or cognitively impaired. If a randomly selected person was not available, an appointment was made for later that day or the following day. From each respondent, symptoms or experiences associated with a general spectrum of potentially surgical conditions were elicited; and access to care or reasons for lack of access to care were determined. The dominant reason for not having accessed care was used in the analysis. Respondents could grade the perceived disability of their indicated condition to the impact on their daily life: (i) the condition is not disabling; (ii) the individual feels ashamed after sustaining the injury; (iii) the individual is unable to work as he or she used to; (iv) the individual needs help with transportation; and (v) the individual needs help with daily living.
Ethical aspects
Institutional Review Board (IRB) approval was obtained from the Nepal Health Research Council in Kathmandu, Nepal and Nationwide Children s Hospital in Columbus, Ohio, USA. All heads of households and selected household members verbally consented before being interviewed or examined. For individuals younger than 8 years of age, parental consent was obtained; for individuals between ages 8 and 17, oral assent and parental permission were obtained.
Data analysis
The data were analysed using MATLAB R2018B (The MathWorks, Inc., Natick, Massachusetts, United States). Various cross‐sections of the data were formulated and histograms and bivariate histograms computed and visualised. For bivariate histograms, data were filtered to exclude ‘no, the condition is not disabling’ from the factor ‘disability’. Thus, all data included in the bivariate analysis reflected some experienced degree of disability. As a normal histogram counts the frequency of values in each bin along one dimension of the data set, a bivariate histogram counts the frequency of values in each bin along two dimensions, thus counting the occurrence of combinations of categories. Bivariate histograms represent the frequency of certain combinations of categories in the data. A chi‐square test was performed on the combined factors excluding empty levels. The resulting p‐value is depicted in the figures.
Results
Figure 1 provides a general overview of the SOSAS data. A total of 2695 individuals were interviewed, of whom 986 (36.6%) had or had had a medical condition. Half the study population with a condition suffered from one at the time. 52.3% (516/986) indicated that they likely would benefit from surgical care to address this condition. 61.8% of the conditions (609/985) were not due to an injury or accident; 26.5% (259/976) were experienced as disabling. The main reasons for having an unmet need were no need (198/516–38.4%), not available (115/516–22.3%), fear or no trust (88/516–17.1%) and no money for health care (93/516–18.0%). A detailed demographic description of the study population is given elsewhere 18. Agreement between verbal self‐assessment and visual expert assessment was 94.6% across the full population and 83.1% for the subgroup indicating an unmet surgical need.
Figure 1.

General overview of the study population. [Colour figure can be viewed at http://wileyonlinelibrary.com]
Figure 2 explores the subset of the study population that indicated a condition, and that had a met or unmet need and/or disability. The top panel visualises the met and unmet surgical need per anatomical area as percentage of the study population, assuming a condition is either met or unmet. The most common unmet needs arose from the head (6.7%), extremities (5.9%), abdomen (2.2%) and the groin (2.0%). The second panel shows per anatomical area the resulting type of disability. Extremities (3.6%), head (2.8%) and groin (1.3%) were the anatomical areas with conditions inflicting the most disability. The third panel shows the reasons for unmet surgical need per anatomical area. The bottom panel combines overall unmet needs and disabilities as percentage of the study population. Although many people (5.6%) who indicated no need experienced their condition as not disabling, there was a rather large proportion (1.7%) of people who did experience a disability but also indicated no need for surgery. Not available (1.5%), no money for health care (1.9%), and fear or no trust (1.5%) were the main reasons for having an unmet surgical need whilst experiencing a disability.
Figure 2.

Exploring met and unmet surgical needs and disabilities. All numbers as percentage of the study population. (a) Prevalence: met and unmet surgical needs per anatomical area. (b) Disability per anatomical area. (c) Reasons for unmet surgical needs per anatomical area. (d) Combinations of reasons of unmet need and disability. [Colour figure can be viewed at http://wileyonlinelibrary.com]
Figure 3 combines reasons for having an unmet surgical need with various levels of experienced disability for each separate anatomical area in the data set. The colour scale relates each combination to a percentage of population. The panels’ chest, back and abdomen represent a very small subset (0.7%, 0.8% and 1.1%, respectively). For abdomen, the most occurring combination is not able to work combined with no money and not available. The top left panel head represents 3.9% of the population. The most frequent combination for the disability not able to work is no money followed by fear and not available and no need. For the bottom middle panel groin (2.2%), the most common disability is shame and the dominant reason is fear. For bottom right panel extremities (3.6%), the most occurring disability is not able to work combined with reasons no need and followed by no money and not available.
Figure 3.

Bivariate histogram combining Reasons for unmet surgical need and experienced levels of Disability for the different anatomical areas. The colour scale relates to the percent of population. Disability factor ‘not disabling’ is removed from the data set. (a) Head; (b) chest; (c) back; (d) abdomen; (e) groin; and (f) extremities.
Figures 4, 5, 6 visualise the occurrence of different combinations of two factors for the anatomical areas head, groin and extremities, indicated by colour. Figure 4 shows the combinations of factors for anatomical area head. The top left panel shows deformity acquired and mass/growth that are not due to injury/accident as the most common combinations. The top middle panel shows that eye and ear/nose/throat are the most afflicted locations. Most issues with eyes come from deformity acquired and wound due to injury (top right panel). Eye is also the most contributing factor to disabling conditions work or shame (middle right), but this is not due to injuries or accidents (middle middle) but rather to acquired deformity (middle left). When it comes to acquired deformity, fear is an important reason for unmet care, as is no money (bottom left). Other specifics associated with no money are wound due to injury and mass/growth. The bottom middle panel shows that for conditions not due to injury or accident, no money, fear and not available are dominant reasons. The bottom right shows that these conditions mostly relate to the eye.
Figure 4.
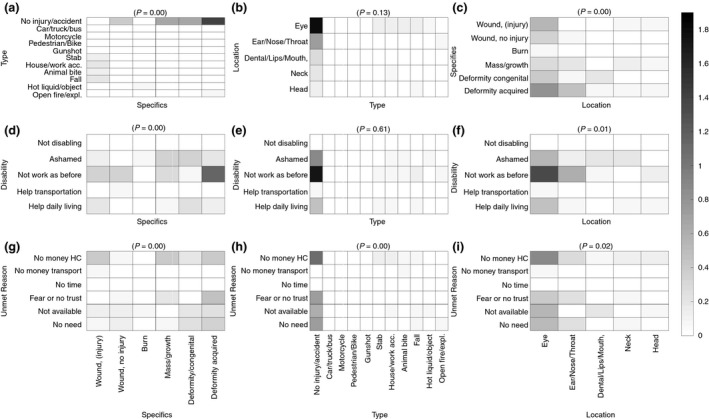
Bivariate histograms combining multiple factors relating to disabling unmet needs for anatomical area ‘Head’. The colour scale relates to the percent of population. (a) Type vs specifics; (b) location vs specifics; (c) specifics vs location; disability vs (d) specifics; (e) type; (f) location; unmet reason vs (g) specifics; (h) type; (i) location.
Figure 5.

Bivariate histograms combining multiple factors relating to disabling unmet needs for anatomical area ‘Groin’. The colour scale relates to the percent of population. (a) Type vs specifics; disability vs (d) specifics; (e) type; unmet reason vs (g) specifics; (h) type.
Figure 6.

Bivariate histograms combining multiple factors relating to disabling unmet needs for anatomical area ‘Extremities’. The colour scale relates to the percent of population. (a) Type vs Specifics; (b) Location vs Specifics; (c) Specifics vs location; disability vs (d) specifics; (e) type; (f) location; unmet reason vs (g) specifics; (h) type; (i) locations.
Figure 5 shows the different combinations of factors for anatomical area groin. As the more specific factor of location was not investigated, this figure has fewer panels. The middle right panel shows clearly that most cases relate to a combination of disability shame and a condition not due to injury or accident. The middle left panel shows that the category of shame is mainly due to three specific conditions: rectal bleeding, mass/growth and leaking of urine/faeces. The bottom left panel shows that those conditions are not treated mainly because of fear or no trust, and in case of rectal bleeding to a lesser extent also due to not being available.
Figure 6 shows the different combinations of factors for extremities. The top left panel shows that wounds due to injury are mainly wounds from falls, house/work accidents and car/truck/bus accidents. Types of injuries not due to injury/accident were mainly mass/growths, acquired or congenital deformity. The top middle panel shows that lower leg is the most affected location, followed by upper arm, upper leg and foot. The top right panel shows that lower leg is often combined with deformity acquired. The middle left panel shows that wounds due to injury (e.g., fall, house/accidents, car or truck accidents) are the most dominant cause of unmet disability. Also mass/growth and deformity acquired are major contributors to disability, whereas acquired deformity causes a need for help with daily living. Mass/growth and burn are dominant causes of shame. The middle panel shows that besides wounds not due to injury, falls are also a main contributor to disability. The middle right panel shows that upper/lower arm, foot and upper/lower leg are the main disabling locations, with lower leg as the most affected location. The bottom left panel shows that no money and not available are important reasons for receiving no surgical care for wounds due to injury, mass/growths and deformities. It also shows that deformity acquired is frequently combined with no need. Bottom right panel shows that surgical care for upper arm and lower leg are mostly combined with health care not being available and lower leg with no need.
Discussion
The aim of this study was to understand which combinations of factors relate to high occurrences of unmet surgical needs and resulting disability, and consequently, how to focus future work to maximise impact. Clearly, the anatomical areas head (3.9%), extremities (3.6%) and groin (2.2%) faced the largest combined unmet need and perceived disability (as percentage of the Nepalese population). Back problems were surprisingly rare compared to levels in high‐income countries. Each anatomical area showed different combinations of level of disability and reasons for unmet surgical needs. Hence, the focus of the solutions provided may need to be different depending on the anatomical area and factors involved. The detailed interactions of the specifics of diseases, affected locations, types of injury as well as their interaction with unmet surgical needs and disabilities show that within each anatomical area different mechanisms (accidents, injuries and progressive diseases) explain the unmet needs and disabilities. Subsequently, the character of health care needed to mitigate the unmet need varies as well, from planned corrective procedures to unplanned, immediate trauma procedures. The consequences will be explored below for each anatomical area.
Head
According to our data, 3.9% of the Nepali population has a disabling unmet surgical need relating to a condition of the anatomical head area. Those conditions are mainly non‐traumatic deformities and masses/growths of the eye and are associated with inability to work as before and with shame. Dominant reasons for the unmet need are having no money, care not being available, having fear or no trust, and having no need. Fear seems to be mainly associated with acquired deformities of the eye and might be addressed by education, explanation of medical procedures, or adopting culturally and contextually appropriate design and procedures to increase cultural acceptability 9. A potential area to focus capacity building on would thus be the area of deformities of the eye. The goal would be to evaluate current procedures and devices and determine whether better ones that are contextually appropriate 8, 9, 11, 35, 36, 37 are needed to increase availability and reduce costs of ownership. Patients declaring themselves as having no need are a difficult category. From Figure 3, it becomes clear that even patients with a disability opted for no need as major reason for not receiving care. This might be because of cultural/religious values where one has to bear and not fight what fate brings to you, or to avoid the shame of indicating fear or no money. Further detailed analysis of eye conditions as well as resources needed to cure the conditions is needed.
Groin
The groin area comprises a disabling unmet surgical need for 2.2% of the Nepali population. Again, these conditions are mainly non‐traumatic. Mass/growth, rectal bleeding and leaking of urine/faeces are dominant specifics of the conditions. They hardly cause any disability that leads to inability to work, but mostly cause shame, thus increasing the vulnerability of the patients. The reason for having an unmet need is mainly fear/no trust and a little unavailability of care. Capacity building should focus on increasing education and explanation of medical procedures as well as adopting culturally and contextually appropriate designs of devices and procedures to build trust and enhance acceptance. Those conditions and their associated mechanisms of care should be analysed in greater detail.
Extremities
Based on this study, it is expected that 3.6% of the population have a disabling condition in the anatomical region of the extremities that is surgically unmet. An important excuse for having no health care is having no need. Again, this might be because of cultural values, or to avoid shame to indicate fear or no money. In contrast to the areas of head and groin, the extremities show a greater mixture of traumatic and non‐traumatic conditions.
Extremities: non‐traumatic conditions
Non‐traumatic conditions are mainly mass/growths and acquired deformities and dominantly relate to lower leg (although every part of the extremities is involved). For non‐traumatic conditions, the dominant reasons for unmet needs are clearly no need, followed by no money for health care and care being not available. Again, no need for disabling conditions because of deformities acquired might be because of cultural values and/or shame. These can only be addressed by education, advocacy, and explanation of medical procedures as well as adopting culturally and contextually appropriate designs of devices and procedures to build trust and enhance acceptance. Capacity building should focus on ways to increase availability and reduce costs for surgical care that addresses mass/growth and deformities. Further work is needed to pinpoint the specific needs and issues of those conditions and associated procedures.
Extremities: traumatic conditions
For traumatic conditions, the main type of injury is because of falls, followed by house/work accidents, burns caused by hot liquids/objects and road traffic incidents with motorised vehicles. The injury affects mainly lower and upper arms, foot and lower legs. Falls yield the highest degree of disability, and the main reason for having an unmet need is unavailability of health care, and to a lesser extent, fear/no trust and having no money. Capacity building should focus on increasing the availability of trauma care, especially those addressing falls, burns and motorised vehicle accidents. Increasing knowledge and cultural acceptance of care are also needed as the unmet reasons have a component of fear/trust.
Limitations
This study is subject to a number of limitations. Firstly, only 15 of the 75 districts were sampled, selected proportional to population. Urban living might be overrepresented, and an over‐ or underestimation might have been the result. Secondly, the study is based on self‐reporting of conditions; however, visual examination showed a 94.6% match between expert evaluation and self‐reporting across the whole study population, and 83.1% across the subgroup indicating an unmet surgical need. Thirdly, the visual examination did not include palpation, invasive checks or advanced visualisation methods. It is therefore unknown what percentage of the study population would actually benefit from surgery. Finally, the interaction between the different factors is visualised across several subcategories using bivariate histograms. This scatters the data, meaning that we lose power. Therefore, the bivariate histograms should be interpreted as relative and explorative figures that indicate where peaks are located that require attention, but care should be taken when extrapolating the exact percentages to country‐level prevalence. Nevertheless, the analysis clearly visualises key factors, issues, barriers and their interactions for meeting specific surgical needs in the Nepali population.
Conclusion
The aim of this study was to understand which combinations of factors relate to high occurrences of unmet surgical needs and resulting disability, and consequently, how to focus future work to maximise impact. Four focus areas that need strengthening in terms of affordability, availability and acceptability could be defined. Firstly, strengthen surgical care for non‐traumatic disabling conditions such as deformities and mass/growths of the eye. Secondly, strengthen surgical care to non‐traumatic disabling conditions of extremities such as mass/growths and deformities in mainly legs and arms. Thirdly, strengthen surgical care to traumatic disabling conditions of extremities resulting from falls, house/work accidents, burns and road traffic incidents. Finally, strengthen surgical care for non‐traumatic conditions such as mass/growth in groin and genital areas, rectal bleeding and leaking of urine/faeces mainly by increasing acceptability of care, as fear/no trust was the main reason for receiving no surgical care despite the resulting shame. A more detailed analysis of these focus areas is needed to pinpoint the exact needs.
Acknowledgements
This study would not have been possible without the help of the Nepali enumerators and field supervisors. Particular thanks go to S. Gurung, J. Pathak, V. Varadaraj, P. Ghimire, S. Nepal, S. Devkota, R. Shrestha and S. Bastola for their enthusiasm and dedication to this study; also to Dr. Benedict Nwomeh and Dr. Marie Diener West for their professional guidance and continuous support.
References
- 1. Human SA. Development Indices and Indicators: 2018 Statistical Update. United Nations Development Programme; : New York, 2018. [Google Scholar]
- 2. National Planning Commission, Oxford Poverty and Human Development Initiative . Nepal Multidimensional Poverty Index 2018 ‐. Analysis Towards Action. Government of Nepal: Nepal, 2018. [Google Scholar]
- 3. Orthopaedic cases from all over country, but sole hospital in Valley [Internet]. The Himalayan Times. 2006. (Available from: https://thehimalayantimes.com/nepal/orthopaedic-cases-from-all-over-country-but-sole-hospital-in-valley/) [cited 20 May 2019] [Google Scholar]
- 4. Eide AH, Neupane S, Hem G. Living conditions among people with disability in Nepal. 2016; 198.
- 5. Lawson Jacobs N Studies in religion, theology, and disability In: Schumm DY, Stoltzfus M. (eds). Disability and World Religions: An Introduction. Baylor University Press: Waco, Texas, 2016; 258. [Google Scholar]
- 6. Ng‐Kamstra JS, Greenberg SLM, Abdullah F et al. Global Surgery 2030: a roadmap for high income country actors. BMJ Glob Health 2016: 1: e000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grimes CE, Bowman KG, Dodgion CM, Lavy CBD. Systematic review of barriers to surgical care in low‐income and middle‐income countries. World J Surg 2011: 35: 941–950. [DOI] [PubMed] [Google Scholar]
- 8. Malkin RA. Barriers for medical devices for the developing world. Expert Rev Med Devices. 2007: 4: 759–763. [DOI] [PubMed] [Google Scholar]
- 9. Howitt P, Darzi A, Yang G‐Z et al. Technologies for global health. Lancet 2012: 380: 507–35. [DOI] [PubMed] [Google Scholar]
- 10. Oosting RM, Wauben LSGL, Groen RS, Dankelman J. Equipment for essential surgical care in 9 countries across Africa: availability, barriers and need for novel design. Health Technol 2018: 9: 269‐275. [Google Scholar]
- 11. World Health Organization , ed. Medical Devices: Managing the Mismatch: An Outcome of the Priority Medical Devices Project. World Health Organization: Geneva, 2010; 129. [Google Scholar]
- 12. Free M. Achieving appropriate design and widespread use of health care technologies in the developing world. Overcoming obstacles that impede the adaptation and diffusion of priority technologies for primary health care. Int J Gynecol Obstet 2004: 85: S3–S13. [DOI] [PubMed] [Google Scholar]
- 13. Spiegel DA, Shrestha OP, Rajbhandary T et al. Epidemiology of Surgical Admissions to a Children s Disability Hospital in Nepal. World J Surg 2010: 34: 954–962. [DOI] [PubMed] [Google Scholar]
- 14. Yadav SK, Mandal BK, Karn A, Sah AK. Maxillofacial trauma with head injuries at a tertiary care hospital in Chitwan, Nepal: clinical, medico‐legal, and critical care concerns. Turk J Med Sci 2012: 42: 1505–1512. [Google Scholar]
- 15. World Health Organization . WHO Generic Essential Emergency Equipment List. :2. [Google Scholar]
- 16. Shah MT, Bhattarai S, Lamichhane N et al. Assessment of the availability of technology for trauma care in Nepal. Injury 2015: 46: 1712–1719. [DOI] [PubMed] [Google Scholar]
- 17. Gupta S, Shrestha S, Ranjit A et al. Conditions, preventable deaths, procedures and validation of a countrywide survey of surgical care in Nepal. Br J Surg 2015: 102: 700–707. [DOI] [PubMed] [Google Scholar]
- 18. Chawla SS, Khanal S, Ghimire P et al. Musculoskeletal disease in Nepal: a countrywide cross‐sectional survey on burden and surgical access. Int J Surg 2016: 34: 122–126. [DOI] [PubMed] [Google Scholar]
- 19. Gupta S, Ranjit A, Shrestha R et al. Surgical needs of Nepal: Pilot Study of Population Based Survey in Pokhara, Nepal. World J Surg 2014: 38: 3041–3046. [DOI] [PubMed] [Google Scholar]
- 20. Gupta S, Gupta SK, Devkota S et al. Fall injuries in Nepal: A Countrywide Population‐based Survey. Ann Glob Health 2015: 81: 487–494. [DOI] [PubMed] [Google Scholar]
- 21. Gupta S, Wong EG, Nepal S et al. Injury prevalence and causality in developing nations: results from a countrywide population‐based survey in Nepal. Surgery 2015: 157: 843–849. [DOI] [PubMed] [Google Scholar]
- 22. Gupta S, Groen TA, Stewart BT et al. The spatial distribution of injuries in need of surgical intervention in Nepal. Geospat Health 2016: 11: 77–82. [DOI] [PubMed] [Google Scholar]
- 23. Gupta S, Mahmood U, Gurung S et al. Burns in Nepal: a population based national assessment. Burns 2015: 41: 1126–1132. [DOI] [PubMed] [Google Scholar]
- 24. Boeck MA, Nagarajan N, Gupta S et al. Assessing access to surgical care in Nepal via a cross‐sectional, countrywide survey. Surgery 2016: 160: 501–508. [DOI] [PubMed] [Google Scholar]
- 25. Forrester JD, Forrester JA, Kamara TB et al. Self‐reported determinants of access to surgical care in 3 developing countries. JAMA Surg 2016: 151: 257–263. [DOI] [PubMed] [Google Scholar]
- 26. Nagarajan N, Gupta S, Shresthra S et al. Unmet surgical needs in children: a household survey in Nepal. Pediatr Surg Int 2015: 31: 389–395. [DOI] [PubMed] [Google Scholar]
- 27. Stewart BT, Wong E, Gupta S et al. Surgical need in an ageing population: a cluster‐based household survey in Nepal. Lancet 2015: 27: 5. [DOI] [PubMed] [Google Scholar]
- 28. Stewart BT, Wong E, Gupta S et al. Surgical need in an aging population: a cluster‐based household survey in Nepal. Surgery 2015: 157: 857–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stewart BT, Kushner AL, Kamara TB et al. Backlog and burden of fractures in Sierra Leone and Nepal: Results from nationwide cluster randomized, population‐based surveys. Int J Surg 2016: 33: 49–54. [DOI] [PubMed] [Google Scholar]
- 30. Tessler R, Gupta S, Pathak J et al. Rectal bleeding and implications for surgical care in Nepal. J Surg Res 2015: 197: 12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. van Loenhout JAF, Delbiso TD, Gupta S et al. Barriers to surgical care in Nepal. BMC Health Serv Res 2017: 17: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chan DM, Zoellick MRB. World Report on Disability. World Health. Organization: Geneva, 2011; 24. [Google Scholar]
- 33. Petroze RT, Groen RS, Niyonkuru F et al. Estimating operative disease prevalence in a low‐income country: Results of a nationwide population survey in Rwanda. Surgery 2013: 153: 457–464. [DOI] [PubMed] [Google Scholar]
- 34. Groen RS, Samai M, Stewart K‐A et al. Untreated surgical conditions in Sierra Leone: a cluster randomised, cross‐sectional, countrywide survey. Lancet 2012: 380: 1082–1087. [DOI] [PubMed] [Google Scholar]
- 35. Malkin RA. Design of health care technologies for the developing world. Annu Rev Biomed Eng 2007: 9: 567–587. [DOI] [PubMed] [Google Scholar]
- 36. Malkin R, von Oldenburg Beer K. Diffusion of novel healthcare technologies to resource poor settings. Ann Biomed Eng 2013: 41: 1841–1850. [DOI] [PubMed] [Google Scholar]
- 37. Malkin R. Medical Instrumentation in the Developing World. Engineering World Health: Memphis, 2006;154. [Google Scholar]


