Abstract
Objectives:
Atrial fibrillation (AF) is the most common arrhythmia treated in clinical practice and the association of this arrhythmia with stroke has long been recognized. The combination of associated factors to identify stroke risk is still unclear; therefore, we aimed to determine the association between additional risk factors for non-valvular AF (NVAF) and the first onset stroke patients and investigate the predictive ability of additional risks factors such as cardiac biomarkers and AF status for odds of incident stroke.
Materials and Methods:
We included 455 patients who suffered from NVAF divided into two distinct groups (case–control observational study). Those two groups were based on whether the patients were having a first onset stroke (stroke group) or not having a stroke (non-stroke group). We made the baseline characteristic of our sample group from the substantial evidence of risk factors, lifestyle, and type of AF; to controversial risk described in the new international guideline of AF.
Results:
Statistically revealed that heart failure, coronary disease, cigarette smoking, type of AF, warfarin treatment, high sensitive troponin, and B-type natriuretic peptide (BNP) are associated with stroke in NVAF patients (P < 0.05). Otherwise, age, sex, hypertension, kidney disease, diabetes, thyroid disease, alcohol intake, season, aspirin, and D-dimer medication were not associated with stroke (P > 0.05). Multivariate analysis of age, smokers, coronary heart disease, heart failure, high sensitive troponin level, BNP, permanent AF, and warfarin was associated (P < 0.05). The combination of biomarkers with the clinical features can be useful (CHA2DS2-VASC/BS) for the prediction of stroke than CHA2DS2-VASC alone (P < 0.05).
Conclusion:
Impact of all associated factors and biological markers as additional risk factors may carry a synergy in this life-threatening event. In addition, may hold a clinical role to redefine and predict stroke events better than the current CHA2DS2-VASC.
Keywords: Cardiac biomarker, non-valvular atrial fibrillation, stroke, troponin
Introduction
Atrial fibrillation (AF) is the most common arrhythmia treated in clinical practice and the association of this arrhythmia with stroke has long been recognized. There are clinical schemas such as CHA2DS2-VASC score, incompletely accounted to predict thromboembolic risk (stroke). This score combines common clinical risk factors for stroke such as congestive heart failure, hypertension, age, diabetes, previous stroke/transient ischemic attack (TIA), vascular disease, and sex. AF, CHA2DS2-VASC score, cardiac biomarkers, and echocardiography parameters have been separately shown to be associated with stroke risk. The combination of these factors to identify stroke risk is still unclear, as some studies have realized the association with stroke risk for each factor individually. Our study will investigate three biomarkers and assess additional risk factor independently associated alone and in combination with risk factors in non-valvular AF (NVAF) and strokes. The significance of the study of cardiovascular diseases (CCDs) and their risk factors cannot be overstated. Arrhythmia is a crucial element, both risk factor and symptom of the disease. The European Society of Cardiology (ESC) states that 12% of the population older than 50 years have chronic cardiac arrhythmias.[1,2]
AF remains the most prevalent arrhythmia treated in emergency departments.[3] Hospitalizations due to AF account for one-third of all admissions for cardiac arrhythmias.[4] While prevalence increases with age, incidence also shows increases for the same reason. After the age of 40, the time risk of developing AF is 25%.[5-10] It is a distinct cardiovascular event related to cerebrovascular complications. Many studies indicate that AF leads to significant adverse outcomes, including a five-fold increase in the risk of stroke. Stroke is a challenging event to treat, likely to result, even at the best of time, in challenging outcomes; and emotionally difficult for sufferers and families.[2,7] Many patients, even with exemplary care, will face a reduced quality of life and impaired productivity at least. Besides, stroke is a costly occurrence to treat, a major social and medical problem for the Western world. On the other hand, stroke is also a global epidemic; worldwide, more than 15 million people suffer from stroke each year, and 85% of all stroke-related deaths occur in low- and middle-income countries. These countries account for 87% of the total loss due to stroke regarding disability-adjusted life years. Stroke is currently the number one cause of death in many emerging economies including China;[11] it is the number 4 cause of death, and the leading cause of long-term disability in the USA.[12,13] Recent studies have shown the impact of extracellular matrix protein measurable in the plasma in correlation with AF risk suggesting a potential value as a biomarker. Cardiac biomarkers are involved in different pathways such as coagulation, myocardial damage, inflammation, and also fibrosis substrate production, which lead to arrhythmogenic changes sustaining AF, and thromboembolic event. While this study will look at the first onset stroke, it is important to note the significant (per CHA2-DS2-VASC/Has-bled) likelihood of further thrombotic events related to stroke. While relationships between biological markers and thrombotic events are evident, the exact correlation between each tag individually and in combination has yet to be proven. It is also likely that further diagnostic tools, including biological markers, need to be developed for improving clinical outcomes.
In the present study, the combination of cardiac biomarkers: High sensitive troponin, B-type natriuretic peptide (BNP), and D-dimer with clinical features can enhance the prediction of the high stroke incidence. Our study aimed to investigate those three cardiac biomarkers, assesses and determines the degree of association between risk factors, CHA2DS2-VASC, and incidences of strokes in patients without heart valves diseases. In addition, we compare the impact of a new risk score model and the previous in a short-term follow-up, and investigate the predictive ability of cardiac biomarkers and AF status for odds of incident stroke in patients to provide a key recommendation to reduce the burden of CCD.
Materials and Methods
Study population and description of methods
We enrolled in a retro-prospective case–control observational study of more than 2000 cases of AF continuously hospitalized in different internal medicine services of the Second Affiliated Hospital of Dalian Medical University Liaoning, China, from January 2015 to December 2017 and the study was approved by the Institutional Ethics Committee of Dalian Medical University. We excluded patients with prior stroke, valvular heart diseases as known to increase thromboembolism and stroke outcome, and finally included 455 patients suffered from NVAF divided into two distinct groups. Those two groups were based on whether the patients were having a first onset stroke (stroke group) or not having a stroke (non-stroke group). We made a baseline characteristic from the substantial evidence of risk factors (CHA2DS2-VASC), lifestyle (cigarette smoking and alcohol intake) to controversial risk (cardiac biomarkers: High sensitive troponin, BNP, and D-dimer) described in the new guideline of the American College of Cardiology/American Heart Association (AHA), and the ESC. Biomarkers have been assessed 24 h following a Holter report of AF patients. Our covariates of interest were the cardiac biomarkers; plasma troponin level was determined with high sensitivity chemiluminescent immunoassay based on Loci® technology (Siemens Healthcare Diagnostic Inc., USA), ARCHITECT BNP assay, a chemiluminescent microparticle immunoassay (Abbott diagnostics Inc., USA) determined plasma BNP level, and latex immunoturbidimetry determined D-dimer from the blood test following admission according to the instruction of the manufacturer.
Assessment of AF
ECG or Holter defined AF; valvular AF was excluded using ultrasound. We also divided patients into three categories according to the duration of AF: Paroxysmal (<7 days duration), persistent (≥7days <1 year), and permanent (≥1 year) AF.[1,14,15]
Ascertainment of stroke
TIA defined patients with the first onset of neurological deficit <24 h, ischemic or hemorrhagic stroke according to the computed tomography or magnetic resonance imaging (MRI) defined deficit longer than 24 h following an AF event.[1,14,15] The experts in both radiology department and neurology department confirmed the diagnosis.
Assessment of variables
Demographic characteristics have included age, sex, medical history of hypertension, heart failure, chronic kidney disease, diabetes mellitus, coronary heart disease, AF, and lifestyle factors including self-reported smoking and alcohol use. The diagnosis of underlying diseases was according to the International Classification of Disease 10. We considered cigarette smoking as consumption of two or more cigarettes per day and exposure to environmental tobacco smoke for at least 1 year; we also considered alcohol intake if a patient consumed one or more drinks per day for at least 1 year. In addition, we also examined the four seasons in which the stroke occurred. Heart failure was defined as a patient having a left ventricular ejection fraction <0.5 and was categorized into three different groups based on the ESC criteria: Heart failure with preserved ejection fraction (≥50%), heart failure with mid-range ejection fraction (4049%), and heart failure with reduced ejection fraction (<40%).[14,15]
Statistical analysis
We used the Statistical Package for the Social Sciences, version 23.0 software for Windows (IBM SPSS Statistics, Chicago, IL, USA.) for statistical analysis of the study data at 95% confidence interval (CI), and P < 0.05 was considered statistically significant. Normally distributed variables were described as mean ± standard deviation and categorical data as percentages. Chi-square and Kruskal–Wallis H test was performed to compare categorical data and continuous variables, respectively, between the two groups. Multivariate (binary) logistic regression model was performed to identify risk factors independently associated with the first onset stroke. The receiver operating characteristic (ROC) curve was drawn to evaluate the predictive value of these risk factors.
Results
The baseline characteristics data analysis
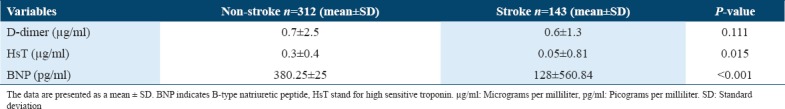
A total of 455 NVAF patients, aged 74 ± 10 years, were enrolled, baseline characteristics and outcomes of the two groups (non-stroke group, n = 312, 68.87%; and stroke group, n = 143, 31.42%) are presented in Tables 1 and2. Table 1 revealed that heart failure and coronary disease were statistically associated with stroke occurrence. The others risk factors for AF, include age, sex, hypertension, diabetes, kidney disease, and thyroid disease did not show statistically association with stroke. Chi-square test in Table 2 revealed that cigarette smoking, types of AF, and anticoagulation medication were statistically associated with stroke in NVAF patients. However, alcohol intake, aspirin medication, and seasons were not statistically associated with stroke. Furthermore, Kruskal–Wallis H test for biomarkers in Table 3 revealed that high troponin level and high BNP level (absolute value) were statistically associated with stroke in NVAF patients. However, D-dimer level was not statistically significant associated with stroke.
Table 1.
Clinical characteristics and outcome in two groups (I)
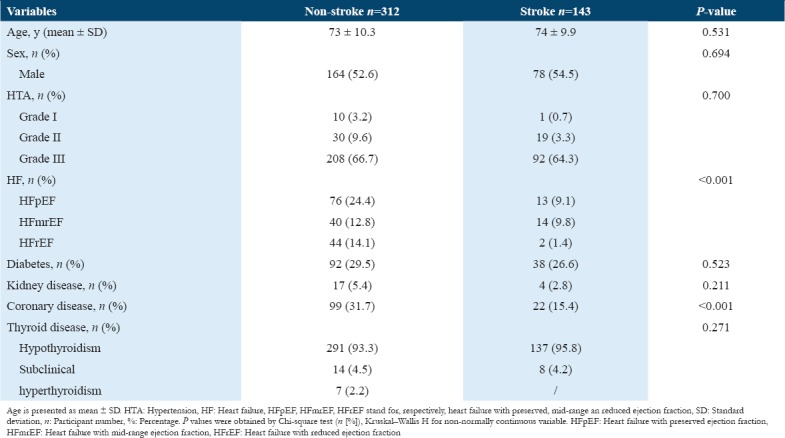
Table 2.
Clinical characteristics and patients outcome in two groups (II)
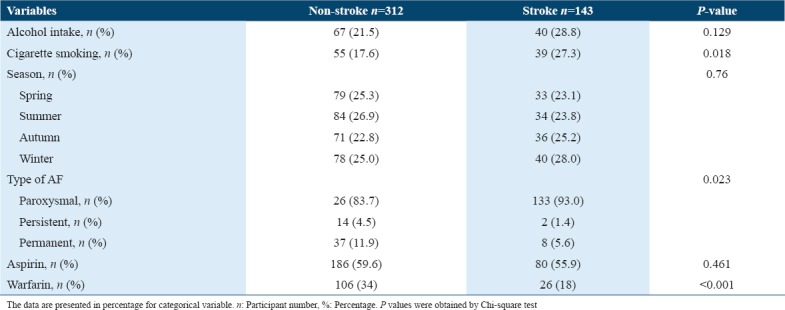
Table 3.
Comparison of biomarkers in two groups (mean±SD)
The clinical and biological impact among patients groups
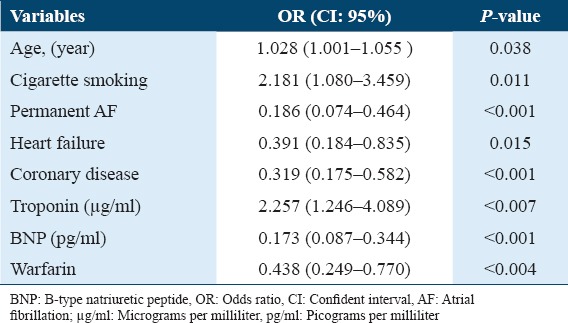
We ran the multivariate (binary) logistic regression analysis to assess the association of risks factors of AF with stroke, as shown in Table 4. Multivariate analysis reveals that age (odds ratio [OR] = 1.465, 95% CI [1.168–1.900], P = 0.009), smoking (OR = 3.200, 95% CI [1.080–5.000], P = 0.006), coronary heart disease (OR = 0.394, 95% CI [0.220–0.706], P = 0.002), heart failure (OR = 0.477, 95% CI [0.371–0.673], P = 0.000], high sensitive troponin (OR = 1.000, 95% CI [0.9991.001], P = 0.010], BNP (OR = 0.999, 95% CI [0.999–1.000], P = 0.001), permanent AF (OR = 0.453, 95% CI [0.192–1.073], P = 0.042), and warfarin treatment (OR = 0.429 95% CI [0.238–0.773], P = 0.005) were independently associated with a high stroke risk outcome in NVAF patients; therefore, we can see in our study especially that after adjustment of various factors, BNP might be less predictive of stroke outcome if considered alone. However, sex, alcohol intake, paroxysmal AF, kidney disease, and D-dimer level, aspirin medication, and four seasons were not independently risk factors of stroke. We put only the independent factors, including age, smoking, coronary heart disease, heart failure, permanent AF, warfarin treatment, high sensitive troponin and BNP, in the multivariate (binary) logistic regression equation again. These factors were still statistically independently associated with stroke, as shown in Table 5.
Table 4.
Impact of risk factors of atrial fibrillation and stroke (multivariate logistic regression analysis)
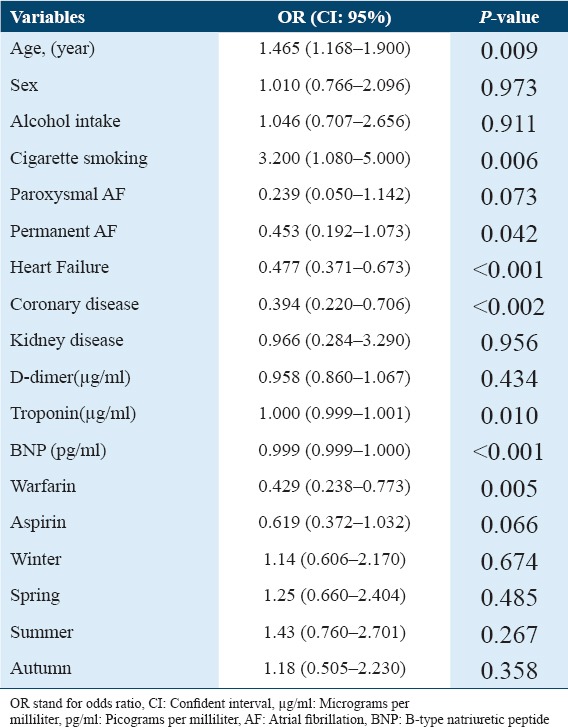
Table 5.
Multivariate analysis of significant variables from the Table 4
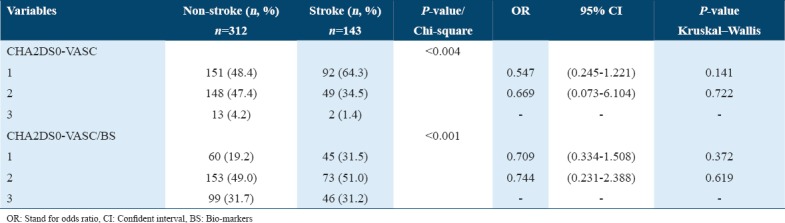
Redefining of the CHA2DS2-VASC score model
We further analyzed both CHA2DS2-VASC score and CHA2DS2-VASC/BS score in the two groups. CHA2DS2-VASC score followed the ESC/AHA/HRS guideline. CHA2DS2-VASC/BS score equaled to CHA2DS2-VASC score plus biomarker, each positive biomarker meant 1 score, and we did not consider D-dimer as less sensitive. The results, as shown in Table 6, of variables combination were as follows: The higher was CHA2DS2-VASC score and CHA2DS2-VASC/BS score, the higher was the risk of stroke. Both scores were statistically significant, P = 0.044 and P = 0.010, respectively. However, there were no statistically significant in different score groups between the stroke group and the non-stroke group. Multivariate analysis showed that higher CHA2DS2-VASC/BS Score, 4 score (P = 0.047, OR = 0.063 [0.0040.966], 95% CI) and 6 score (P = 0.040. OR = 0.042 [0.002–0.863], 95% CI) were statistically significant. We may assume that the higher the CHA2DS2-VASC/BS score, the higher the stroke risk (outcome). Based on our inclusion criteria, patients had first onset stroke; therefore, CHA2DS2-VASC score became CHA2DVASc and CHA2DVASc/BS score meaning that patients lacked two points. We refine the score as CHA2D-VASc = 1 if CHA2DS2-VASC ≤3 is the same for CHA2D-VASc/BS, CHA2D-VASC = 2 if CHA2DS2-VASC[4,5] is CHA2DVASc/BS, and CHA2D-VASc = 3 if CHA2DS2-VASC >5 is CHA2D-VASc/BS. The results presented in Table 7 redefined the score risk based on Table 6, after score modification (explained over the table), we can see that participants with CHA2DS0 VASc/BS scored 2 (95% CI, OR = 0.744 [0.231–2.388], [51%], P = 0.001) were more likely to develop a stroke than the group of CHA2DS2-VASC scored 2 (95% CI, OR = 0.669 [0.073–6.104], [34.5%], P = 0.004). The combination of biomarkers with clinical features as a new score system may better predict stroke outcome in AF patients. Our study shows that higher biomarkers level in combination with CHA2DS2-VASC may better predict stroke outcome than CHA2DS2-VASC alone; therefore, these factors can be used to redefine a new tool for the management of CCDs, also these factors may hold clinical impact and they can probably play a key role in redefining score risk assessment in patients with NVAF.
Table 6.
Impact of cardiac biomarkers in combination with CHA2DS2-VASC score
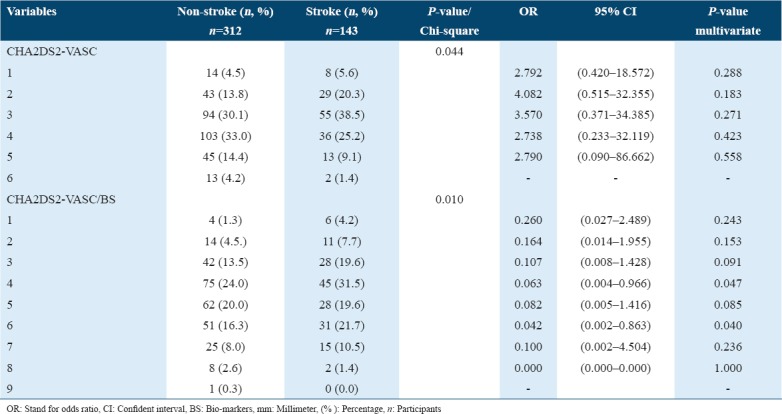
Table 7.
Redefining of the CHA2DS2-VASC score and CHA2DS2-VASC/BS score
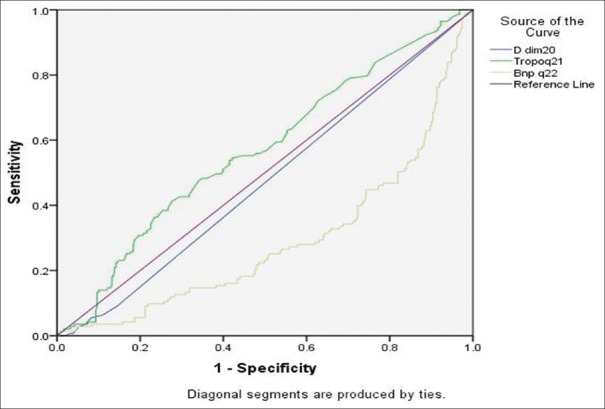
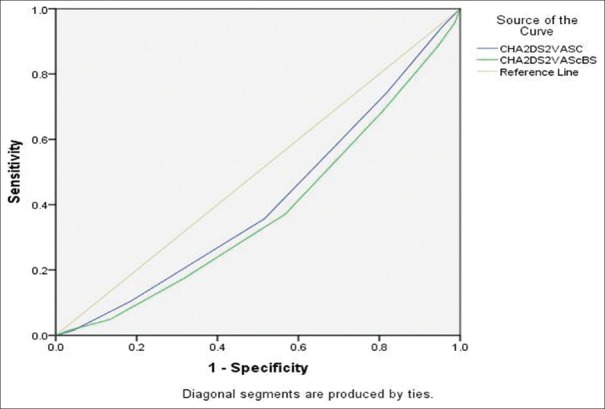
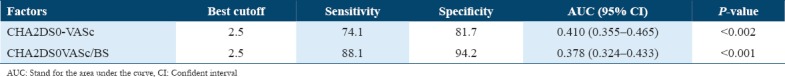
The receiver operator characteristic analysis
The ROC curves showed that Troponin and BNP were the independent risk factor for stroke, as shown in Table 8 and Figure 1. The optimal cutoff points were0.019 µg/ml and 100.150 pg/ml, respectively. For predicting the prevalence of stroke;troponin, BNP displayed an excellent area under the ROC (AUROC) curve, respectively: (x ± 0.029], P = 0.010 AUROC = [0.288 ± 0.026], P = 0.001). TheROC curves showed in Figure 2 and prediction strength of CHA2DS2-VASC and CHA2DS2-VASC/BS score expressed in Table 9. The combination ofbiomarkers with the clinical features can be useful (CHA2DS0-VASc/BS) indicators for the prediction of stroke than CHA2DS0-VASc alone, respectively (AUROC = [0.378 ± 0.028], P = 0.000; AUROC = [0.410 ± 0.028], P = 0.002). CHA2DS0-VASc/BS score had both higher sensitivity and specificity than CHA2DS0-VASc score.
Table 8.
Cardiac biomarker and predictive value of the outcome
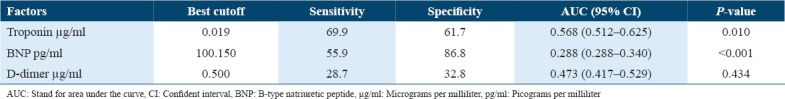
Figure 1.
Receiver operating characteristic curves for predicting stroke in atrial fibrillation patients (biomarkers)
Figure 2.
Receiver operating characteristic curves for predicting stroke in atrial fibrillation patients (CHA2DS2-VASC and CHA2DS2-VASC/BS)
Table 9.
Prediction strength of CHA2DS2-VASC and CHA2DS2-VASC/BS score
Discussion
The significant finding of this retrospective study shows that most modifiable risk factors for AF are significantly associated with increased stroke risk even after adjusting for potential confounding factors. The risk factors found are similar to those reported in several studies claiming that aging increases the risk of stroke while it is a well-known non-modifiable cardiovascular risk factor, relatively common in the Chinese population report of the national center for CCD China.[16-18] A significant risk factor shown in this study is cigarette smoking; changing this lifestyle is vital in the management of CCD and can create better outcomes in reducing the burden of these conditions. Our study shows that the majority of patients were smokers, few of them reported their real status; therefore, this later has been variously reported by different studies.[19,20] Some research concerning the association between smoking and incident AF is in contradiction with some epidemiological studies finding no association and others demonstrating an elevation in risk ranging from 32% to more than double in current smokers and 32–49% in former smokers.[21,22] Mechanisms involved in the contribution of smoking to AF risk may include increased inflammation, atrial fibrosis, and oxidative stress.[23,24] Cigarette smoking is also involved in the atherogenesis, endothelial dysfunction, and promote a heightened prothrombotic state with enhanced platelet activation and raised fibrinogen levels and all of which are unfavorable in AF.[20] Smoking is strongly associated with thromboembolic risk in patients with established AF with one study citing a >2-fold increase in risk in smokers and another showing a stronger association for a combination of thromboembolic danger and death in women than men reported Albertsen et al.[25,26] Our study reveals that high blood pressure in NVAF patients is not associated with a higher stroke incidence, this statement is not in line with many others studies. Moreover, this finding may reflect the improvements in the management of modifiable risk factors describes in a recent meta-analysis of hypertensive patients reporting that anti-hypertensive treatment reduced the risk of recurrent stroke by 27%, disabling or fatal stroke by 29%, and cerebrovascular death by 15%.[27] Furthermore, we performed different ablation procedure during our study; we do not know very well the impact of medical versus interventional management in our research which is reported by previous studies showing how catheter ablation is associated with lower stroke incidence.[28,29] Thromboembolic events are most reported in patients with permanent atrial fibrillation in our study, This description is in line with the review of Kamioka et al. reporting that patient with paroxysmal AF suffered fewer thromboembolic events and death compared with those patients that have persistent and permanent AF, also a study of fibrosis in the left atrial tissue of patients with AF with and without underlying mitral valve disease reported by Gan et al., and Zirlik and Bode.[30-33] Recent advance study described the impact of fibrosis on the detection and the quantification of a fibrotic substrate using gadolinium-enhanced MRI. Direct histological evidence of increased atrial fibrosis and indirect evidence of reduced atrial voltage from electro-anatomical mapping have been demonstrated in humans with heart conditions.[34] These new techniques of detection and quantification of the fibrotic substrate need to be performed in patients with AF, but methodological challenges limit its use. Our study finds few case reports of cardiac MRI in line with our research design, unfortunately.
We can find the pathophysiology description of this new concept in the second part of this study. The second important finding of the present study is the association between the cardiac biomarker and stroke event in NVAF patients. The present case–control study demonstrates an association between troponin level and stroke occurrence. The elevation in cardiac troponin above the standard 99th percentile defined hypertroponinemia. High troponin levels reflect myocardial damage associated with heart failure and predict poor prognosis in various cardiomyopathy and stroke conditions. Following previous studies, we found that high troponin levels are significantly associated with increased stroke risk even after adjusting for confounding factors. Despite the fact that the sample size is not the same in both groups (non-stroke and stroke group in AF patients), we can states that our results are in line with the BEST risk score study;[35] also in line with the study of high sensitivity troponin T (hsTnT) and stroke in AF reporting that elevated hsTnT remains an independent predictor of stroke in AF patients.[30,36] The results of our research contradict a recent study based on the age, biomarker, clinical (ABC history) risk and CHA2DS2-VASC scores study, in long-term prediction of stroke occurrence.[33] This latest study states that the ABC risk did not provide more accurate result in predicting stroke event than CHA2DS2VASC score.[33] The increased D-dimer level is not associated with stroke occurrence; our finding is in controversy with others. Different studies show how high D-dimer levels in AF patients with multiple risk factors for embolism are associated with a high risk of cardiovascular events.[30]
In patients with NVAF D-dimer levels may be helpful in predicting the absence of left atrial appendage (LAA) thrombi involved in stroke, so this marker is useful in the management of patients with NVAF.[37] D-dimer is a thrombosis marker for various types of infarction related conditions such as CCD, thromboembolism, and cardio-embolism stroke. In our study, we did not check for additional comorbidities, such as cancer.[38,39] Increased level of BNP was also reported in the majority of patients in this study and is significantly associated with stroke occurrence as also indicated by Shibazaki et al.[32,40] Several studies describe using BNP levels to exclude or confirm diagnoses of heart failure. Plasma BNP level is thought to be a useful biological marker for the detection of paroxysmal AF in patients with cryptogenic stroke.[40] The results of our research have shown that plasma level BNP is 4 times elevated than the normal value in the stroke group than in the non-stroke group. Broadly, this present study provided evidence of an association between lifestyle, some modifiable risk factors, higher cardiac biomarker levels, and strokes in NVAF patients. Previous investigations focused on the association between clinical cardiovascular risks factors and stroke; clinical practice and various studies well support these studies with substantial evidence in the general population are shown in this discussion. The results shown in this present study notably reveal the impact of cardiac biomarkers, and lifestyle predicting stroke event when they are considered in combination with other risk factors. These results can lead us to provide a better tool for the management of AF, by making not only early detection of different cardiac biomarkers (e.g., Galectin-3 and fibrosis biomarker) also the detection and quantification of atrial fibrosis by new technology such as delayed enhancement (DE)-magnetic resonance and electro-anatomical mapping of fibrosis in the future.
Our study shows the impact of cardiac biomarkers in NVAF; mainly they seem to be substantial as they may constitute powerful predictors of increased risk and provide significant improvements to incompletely (CHA2DS2-VASc) used clinically based risk stratification models. Biomarker-based risk stratification in NVAF may help improve care and prevents thromboembolic and cardiovascular events. Although typically it is difficult to draw firm conclusions concerning causality and the involvement of a biomarker in the etiology of a disease, biological markers may hold clinical impact and will probably play a key role in redefining clinical risk assessment in patients with NVAF as presented in this small sample group. The result of our study is useful in a sense that patients with NVAF who lack a history of stroke or TIA but have other risk factors have an intermediate stroke risk, and the absolute stroke risk in this group has been difficult to estimate. As a consequence, although multiple risk score tools are available for estimating the absolute stroke risk of a patient with NVAF with varying risk factor combinations, the absolute stroke risk estimated and generated by these tools vary widely. Thus, it seems to be clear that NVAF patient with a first onset stroke (CHA2DS0-VASC/BS) but elevated plasma biomarkers level may have a similar stroke risk score with those of a second onset stroke(CHA2DS2-VASC). It is not possible to precisely determine their absolute stroke risks state in the American Academy of Neurology in their guideline on the prevention of stroke in NVAF. The concentration of biomarkers may provide further guidance regarding the selection of specific treatments. They are potentially useful in the efforts of improving outcome in AF as a decision support tools of anticoagulation strategy. Information from biomarkers may provide substantial information beyond clinical data concerning both clinically silent and apparent disease process and the degree of organ dysfunction in patients with AF. Thereby, the concentrations of biomarkers may provide further guidance regarding the selection of specific treatments. Elevation of cardiac biomarkers concentration is indicators of myocardial stress and dysfunction and increased thrombogenicity, and may, therefore, strengthen the indication for rhythm and rate regulation, strict blood pressure control (ACE Inhibitor) and effective anticoagulation.
Limitation of the study
Our study provided results regarding the impact of cardiac biomarkers, and lifestyle on NVAF patients, with the following limitations: This retro-prospective study design limited analysis of continuous hospitalized patients with NVAF in one hospital, so we do not yet know if we can extend our observation in the general population. Second, our study does not show cardiac biomarkers modification over a long-term follow-up; we considered laboratory results following Holter analysis according to the instruction of the manufacturer. In the screening of CCD biological marker help to rule out different biomarker while the low level of troponin, BNP, D-dimer can be due to medical treatment (oral anticoagulation) catheter ablation of AF; this situation cannot prevent any proper management (LAA closure and catheter ablation) based on risk score in the long-term follow-up. The detection and quantification of a fibrotic substrate with DE – MRI are not yet performed in many hospitals, the imaging acquisition with this new technology is still a challenging situation. The need for more studies including the level of inflammatory and cardiac biomarker over the time using Kaplan–Meier analysis with large sample size is critical to realize and provide global management and therefore to reduce the burden of CCD.
Conclusion
We conclude that coronary heart disease, heart failure, cigarette smoking, type of AF, warfarin medication, high sensitive troponin, and BNP level are associated with elevated stroke risk in patients with NVAF. Impact of biological risk factors may carry a synergy in this life-threatening event. In addition, may hold a clinical role to redefine and predict stroke events better than the current CHA2DS2-VASc. Application of new ablation procedure like cryoballoon, LAA closure with appropriate device following the international guideline recommendations can also be considered to reduce the burden of CCD.
Conflicts of Interest
None declared including specific, related, and/or affiliated financial interests.
Funding/Support
No fund.
References
- 1.Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary:A report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society. Circulation. 2018;138:421. doi: 10.1161/CIR.0000000000000548. [DOI] [PubMed] [Google Scholar]
- 2.Camm J. Antiarrhythmic drugs for the maintenance of sinus rhythm:Risks and benefits. Int J Cardiol. 2012;155:362–71. doi: 10.1016/j.ijcard.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 3.Jackson SL, Tong X, Yin X, George MG, Ritchey MD. Emergency department, hospital inpatient, and mortality burden of atrial fibrillation in the United States 2006 to 2014. Am J Cardiol. 2017;120:1966–73. doi: 10.1016/j.amjcard.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apenteng PN, Gao H, Hobbs FR, Fitzmaurice DA UK GARFIELD-AF Investigators and GARFIELD-AF Steering Committee. Temporal trends in antithrombotic treatment of real-world UK patients with newly diagnosed atrial fibrillation:Findings from the GARFIELD-AF registry. BMJ Open. 2018;8:018905. doi: 10.1136/bmjopen-2017-018905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naser N, Dilic M, Durak A, Kulic M, Pepic E, Smajic E, et al. The impact of risk factors and comorbidities on the incidence of atrial fibrillation. Mater Sociomed. 2017;29:231–6. doi: 10.5455/msm.2017.29.231-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenberg MA, Shores MM, Matsumoto AM, Bůžková P, Lange LA, Kronmal RA, et al. Serum androgens and risk of atrial fibrillation in older men:The cardiovascular health study. Clin Cardiol. 2018;41:830–6. doi: 10.1002/clc.22965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oto E, Okutucu S, Katircioglu-Öztürk D, Güvenir HA, Karaagaoglu E, Borggrefe M, et al. Predictors of sinus rhythm after electrical cardioversion of atrial fibrillation:Results from a data mining project on the flec-SL trial data set. Europace. 2017;19:921–8. doi: 10.1093/europace/euw144. [DOI] [PubMed] [Google Scholar]
- 8.Stewart S, Carrington MJ, Marwick T, Davidson PM, Macdonald P, Horowitz J, et al. The WHICH?Trial:Rationale and design of a pragmatic randomized, multicentre comparison of home vs Clinic-based management of chronic heart failure patients. Eur J Heart Fail. 2011;13:909–16. doi: 10.1093/eurjhf/hfr048. [DOI] [PubMed] [Google Scholar]
- 9.Ishii M, Ogawa H, Unoki T, An Y, Iguchi M, Masunaga N, et al. Relationship of hypertension and systolic blood pressure with the risk of stroke or bleeding in patients with atrial fibrillation:The fushimi AF registry. Am J Hypertens. 2017;30:1073–82. doi: 10.1093/ajh/hpx094. [DOI] [PubMed] [Google Scholar]
- 10.Chamberlain AM, Alonso A, Gersh BJ, Manemann SM, Killian JM, Weston SA, et al. Multimorbidity and the risk of hospitalization and death in atrial fibrillation:A population-based study. Am Heart J. 2017;185:74–84. doi: 10.1016/j.ahj.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joo H, Liang D. Economic burden of informal care attributable to stroke among those aged 65 years or older in China. Int J Stroke. 2017;12:205–7. doi: 10.1177/1747493016675501. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Q, Li Z, Wang C, Liu Y, Yang Y, Bussell S, et al. Acomparison of DALYs for periodontal disease in China between 1990 and 2013:Insights from the 2013 global burden of disease study. BMC Oral Health. 2017;17:74. doi: 10.1186/s12903-017-0356-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hankey GJ. Stroke. Lancet. 2017;389:641–54. doi: 10.1016/S0140-6736(16)30962-X. [DOI] [PubMed] [Google Scholar]
- 14.Zamorano JL, Lancellotti P, Rodriguez Muñoz D, Aboyans V, Asteggiano R, Galderisi M, et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC committee for practice guidelines:The task force for cancer treatments and cardiovascular toxicity of the European society of cardiology (ESC) Eur J Heart Fail. 2017;19:9–42. doi: 10.1002/ejhf.654. [DOI] [PubMed] [Google Scholar]
- 15.Blomström-Lundqvist C, Scheinman MM, Aliot EM, Alpert JS, Calkins H, Camm AJ, et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias--executive summary. A report of the American college of cardiology/American heart association task force on practice guidelines and the European society of cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42:1493–531. doi: 10.1016/j.jacc.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 16.Chen WW, Gao RL, Liu LS, Zhu ML, Wang W, Wang YJ, et al. China cardiovascular diseases report 2015:A summary. J Geriatr Cardiol. 2017;14:1–10. doi: 10.11909/j.issn.1671-5411.2017.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.López-López JA, Sterne JA, Thom HH, Higgins JP, Hingorani AD, Okoli GN, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation:systematic review, network meta-analysis, and cost effectiveness analysis. BMJ. 2017;359:5058. doi: 10.1136/bmj.j5058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest. 2010;137:263–72. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 19.Suzuki S, Otsuka T, Sagara K, Semba H, Kano H, Matsuno S, et al. Effects of smoking on ischemic stroke, intracranial hemorrhage, and coronary artery events in Japanese patients with non-valvular atrial fibrillation. Int Heart J. 2017;58:506–15. doi: 10.1536/ihj.16-228. [DOI] [PubMed] [Google Scholar]
- 20.Pikija S, Trkulja V, Malojcic B, Mutzenbach JS, Sellner J. A high burden of ischemic stroke in regions of eastern/Central Europe is largely due to modifiable risk factors. Curr Neurovasc Res. 2015;12:341–52. doi: 10.2174/1567202612666150731105554. [DOI] [PubMed] [Google Scholar]
- 21.Ruperti Repilado FJ, Doerig L, Blum S, Aeschbacher S, Krisai P, Ammann P, et al. Prevalence and predictors of atrial fibrillation type among individuals with recent onset of atrial fibrillation. Swiss Med Wkly. 2018;148:14652. doi: 10.4414/smw.2018.14652. [DOI] [PubMed] [Google Scholar]
- 22.Watanabe I. Smoking and risk of atrial fibrillation. J Cardiol. 2018;71:111–2. doi: 10.1016/j.jjcc.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Messner B, Bernhard D. Smoking and cardiovascular disease:Mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34:509–15. doi: 10.1161/ATVBAHA.113.300156. [DOI] [PubMed] [Google Scholar]
- 24.Morris PB, Ference BA, Jahangir E, Feldman DN, Ryan JJ, Bahrami H, et al. Cardiovascular effects of exposure to cigarette smoke and electronic cigarettes:Clinical perspectives from the prevention of cardiovascular disease section leadership council and early career councils of the American college of cardiology. J Am Coll Cardiol. 2015;66:1378–91. doi: 10.1016/j.jacc.2015.07.037. [DOI] [PubMed] [Google Scholar]
- 25.Nguyen HK, Humber D, Checkoway H, Blanchard D, Watanabe JH. Anticoagulant use in high stroke-risk patients with nonvalvular atrial fibrillation. Consult Pharm. 2018;33:521–30. doi: 10.4140/TCP.n.2018.521. [DOI] [PubMed] [Google Scholar]
- 26.Albertsen IE, Rasmussen LH, Lane DA, Overvad TF, Skjøth F, Overvad K, et al. The impact of smoking on thromboembolism and mortality in patients with incident atrial fibrillation:Insights from the Danish diet, cancer, and health study. Chest. 2014;145:559–66. doi: 10.1378/chest.13-1740. [DOI] [PubMed] [Google Scholar]
- 27.Katsanos AH, Filippatou A, Manios E, Deftereos S, Parissis J, Frogoudaki A, et al. Blood pressure reduction and secondary stroke prevention:A Systematic review and metaregression analysis of randomized clinical trials. Hypertension. 2017;69:171–9. doi: 10.1161/HYPERTENSIONAHA.116.08485. [DOI] [PubMed] [Google Scholar]
- 28.Kamioka M, Hijioka N, Matsumoto Y, Nodera M, Kaneshiro T, Suzuki H, et al. Uncontrolled blood pressure affects atrial remodeling and adverse clinical outcome in paroxysmal atrial fibrillation. Pacing Clin Electrophysiol. 2018;41:402–10. doi: 10.1111/pace.13311. [DOI] [PubMed] [Google Scholar]
- 29.Friberg L, Tabrizi F, Englund A. Catheter ablation for atrial fibrillation is associated with lower incidence of stroke and death:Data from Swedish health registries. Eur Heart J. 2016;37:2478–87. doi: 10.1093/eurheartj/ehw087. [DOI] [PubMed] [Google Scholar]
- 30.Yucel O, Yucel H, Zorlu A. D-dimer is a predictor of cardiovascular death, and new-onset atrial fibrillation in patients with systolic heart failure. Int J Cardiol. 2017;247:39. doi: 10.1016/j.ijcard.2017.04.065. [DOI] [PubMed] [Google Scholar]
- 31.Gan L, Yu L, Xie M, Feng W, Yin J. Analysis of real-time three dimensional transesophageal echocardiography in the assessment of left atrial appendage function in patients with atrial fibrillation. Exp Ther Med. 2016;12:3323–7. doi: 10.3892/etm.2016.3745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zirlik A, Bode C. Vitamin K antagonists: Relative strengths and weaknesses vs. Direct oral anticoagulants for stroke prevention in patients with atrial fibrillation. J Thromb Thrombolysis. 2017;43:365–79. doi: 10.1007/s11239-016-1446-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rivera-Caravaca JM, Roldán V, Esteve-Pastor MA, Valdés M, Vicente V, Lip GY, et al. Long-term stroke risk prediction in patients with atrial fibrillation:Comparison of the ABC-stroke and CHA2DS2-VASc scores. J Am Heart Assoc. 2017;6:e006490. doi: 10.1161/JAHA.117.006490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stiles MK, John B, Wong CX, Kuklik P, Brooks AG, Lau DH, et al. Paroxysmal lone atrial fibrillation is associated with an abnormal atrial substrate: Characterizing the “second factor”. J Am Coll Cardiol. 2009;53:1182–91. doi: 10.1016/j.jacc.2008.11.054. [DOI] [PubMed] [Google Scholar]
- 35.Hijazi Z, Lindbäck J, Alexander JH, Hanna M, Held C, Hylek EM, et al. The ABC (age, biomarkers, clinical history) stroke risk score:A biomarker-based risk score for predicting stroke in atrial fibrillation. Eur Heart J. 2016;37:1582–90. doi: 10.1093/eurheartj/ehw054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu J, Wang D, Xiong Y, Liu B, Wei C, Ma Z, et al. High-sensitivity cardiac troponin T levels and risk of cerebral microbleeds in acute ischemic stroke patients with atrial fibrillation and/or rheumatic heart disease. J Neurol Sci. 2016;369:15–8. doi: 10.1016/j.jns.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 37.Bai W, Chen Z, Tang H, Wang H, Cheng W, Rao L, et al. Assessment of the left atrial appendage structure and morphology:Comparison of real-time three-dimensional transesophageal echocardiography and computed tomography. Int J Cardiovasc Imaging. 2017;33:623–33. doi: 10.1007/s10554-016-1044-4. [DOI] [PubMed] [Google Scholar]
- 38.Radu RA, Terecoasă EO, Băjenaru OA, Tiu C. Etiologic classification of ischemic stroke:Where do we stand? Clin Neurol Neurosurg. 2017;159:93–106. doi: 10.1016/j.clineuro.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 39.Gran OV, Brækkan SK, Paulsen B, Skille H, Hansen JB. D-dimer measured at first venous thromboembolism is associated with future risk of cancer. Haematologica. 2016;101:473–5. doi: 10.3324/haematol.2016.151712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shibazaki K, Kimura K, Fujii S, Sakai K, Iguchi Y. Brain natriuretic peptide levels as a predictor for new atrial fibrillation during hospitalization in patients with acute ischemic stroke. Am J Cardiol. 2012;109:1303–7. doi: 10.1016/j.amjcard.2011.12.022. [DOI] [PubMed] [Google Scholar]