A 14-year-old girl with no unusual past medical history presented to the emergency department (ED) at Yale-New Haven Children’s Hospital with a 2-day history of slurred speech, morbid thoughts, aggressiveness, and seizures that were tonic-clonic by description. On arrival, she was febrile to 101.5°F with a pulse of 111 beats per minute and blood pressure of 141/81 mm Hg. Initially, she was anxious with inappropriate speech and poor attention. The remainder of her examination in the ED was normal. Her parents reported a history of exposure to a bat with no actual bat contact in their house approximately 1 year prior, for which the patient did not seek medical attention.
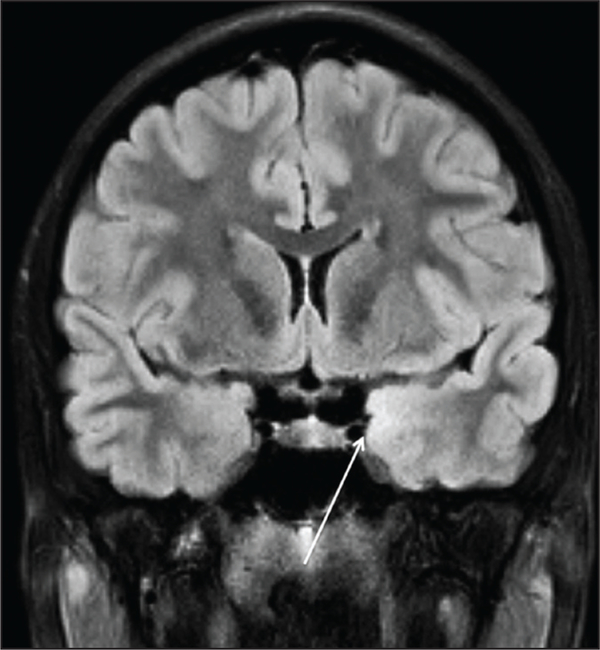
Her initial testing was significant for a cerebrospinal fluid (CSF) with a white blood cell count of 26/mcL. The patient’s CSF had a predominance of lymphocytes (96%), a red blood cell count of 22/mcL, and normal glucose and protein. She had a urine toxicology screen, complete blood count, electrolyte determination, and liver function tests, all of which were normal. She had a normal computed tomography scan, and a magnetic resonance image (MRI) scan of the brain that demonstrated unilateral temporal tip enhancement that was concerning for herpes simplex virus (HSV) encephalitis (Figure 1).
Figure 1.
Magnetic resonance imaging scan of the brain (coronal section) demonstrating a subtle signal abnormality along the medial temporal lobe.
She was treated with acyclovir, but on hospital day 5 her mental status rapidly declined and she was subsequently intubated. She became hypertensive, tachycardic, and hyperthermic. This was associated with hypersalivation and jaw clenching. Additional tests were conducted, which included antibody or Polymerase chain reaction testing for HAV, enteroviruses, mycoplasma, West Nile virus, Powassan virus, eastern equine virus, Borrelia burgdorferi, lymphocytic choriomeningitis virus, human herpes virus 6, and rabies virus. All of these tests were negative. An additional diagnostic test was performed.
In a search for alternative etiologies of the encephalitis, a test for antibodies to anti-N-methyl-D-aspartate (anti-NMDA) receptor was conducted and returned positive. An abdominal MRI was subsequently obtained as an adjunct for this diagnosis. The MRI revealed a left ovarian cyst. The patient was then taken to the operating room for a left ovarian cystectomy. Gross dissection of the mass revealed hair and sebum, and the histology confirmed a mature ovarian teratoma, which is characteristic of this diagnosis.
After 10 days of hospitalization, the patient was diagnosed with anti-NMDA receptor antibody encephalitis, because she had a positive serum titer of 1:320. Her clinical outcome was poor, with a clinical picture consistent with static encephalopathy. She has had minimal neurologic improvement despite the use of high-dose steroids, intravenous immune globulin, a complete unilateral oophorectomy, plasmapheresis, and cyclosporine, each of which has been reported to have benefit in anti-NMDA receptor antibody encephalitis.
DISCUSSION
Since its discovery in 2005, anti-NMDA receptor encephalitis has gained recognition in the medical field.1 It is characterized by a prodrome of fever, headaches, and behavioral changes, and it progresses to autonomic instability, hypoventilation, and a coma-like state.2 About 40% of cases are associated with a tumor, almost all of which are ovarian teratomas.3 Clinical decline is rapid; therefore, early recognition is crucial to a favorable outcome.
The diagnosis of anti-NMDA receptor encephalitis is challenging because it can mimic many conditions ranging from infectious etiologies to psychiatric disorders to pharmacologic effects. In the case of this patient, a diagnosis of rabies was temporarily pursued (and then ruled out) due to the many similarities between the two conditions. Both entities are characterized by a period of agitation and hyperexcitability followed by rapid deterioration. Interestingly, studies with animal models have suggested that the NMDA receptor plays a role in the pathogenesis of rabies.4
HSV encephalitis and anti-NMDA encephalitis also share common features, particularly in neuroimaging. Temporal lobe enhancement, commonly seen in patients with HSV encephalitis, has been described to occur in 25% of patients with anti-NMDA encephalitis.5 Additionally, there have been many reports of patients initially diagnosed with psychiatric disorders who were subsequently found to have anti-NMDA receptor encephalitis.6 The behavioral changes of aggression and excitability, in contrast to the symptoms of decreased verbal output and catatonia, have been compared to the positive and negative effects of schizophrenia, respectively.7
Lastly, drugs that interact with the NMDA receptor produce symptoms similar to anti-NMDA receptor encephalitis. Phencyclidine (PCP) and ketamine are noncompetitive NMDA receptor antagonists. At a low level of NMDA receptor blockade, patients experience psychosis and agitation as seen in PCP abuse and early anti-NMDA receptor encephalitis. Higher levels of blockade lead to decreased responsiveness, as seen with ketamine.7
According to the available literature, treatment of this condition generally consists of tumor removal along with steroids and intravenous immune globulin. Second-line treatment includes immunomodulators such as cyclosporine.2 Prognosis is generally favorable. In a recent study of 577 patients with anti-NMDA encephalitis, at 2 years after the diagnosis, 81% of patients had a favorable outcome, 7% had died, and the remaining had severe neurologic sequelae.3
CONCLUSION
Given the complexity of this condition and the importance of early identification, pediatricians should have a low threshold for evaluating children with rapidly evolving psychiatric symptoms or encephalitis for anti-NMDA receptor encephalitis.
Diagnosis:
Anti-N-Methyl-D-Aspartate Receptor Antibody Encephalitis
Footnotes
Disclosure: The authors have no relevant financial relationships to disclose.
Contributor Information
Kelly Joseph, Department of Pediatrics, Yale School of Medicine..
Carlos R. Oliveira, Department of Pediatrics, Yale School of Medicine..
Robert S. Baltimore, Department of Pediatrics and Department of Epidemiology and Public Health, Yale School of Medicine..
REFERENCES
- 1.Vitaliani R, Mason W, Ances B, et al. Paraneoplastic encephalitis, psychiatric symptoms, and hypoventilation in ovarian teratoma. Ann Neurol. 2005;58:598–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Florance-Ryan N, Dalmau J. Update on anti-N-methyl-D-aspartate receptor encephalitis in children and adolescents. Curr Opin Pediatr. 2010;22:739–744. [DOI] [PubMed] [Google Scholar]
- 3.Titulaer MJ, McCracken L, Gabilondo I, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013;12;157–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weli SC, Scott CA, Ward CA, et al. Rabies virus infection of primary neuronal cultures and adult mice: failure to demonstrate evidence of excitotoxicity. J Virol. 2006;80:10270–10273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dalmau J, Tuzun D, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61:25–3636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barry H, Hardiman O, Healy DG, et al. Anti-NMDA receptor encephalitis: an important differential diagnosis in psychosis. Br J Psychiatry. 2011;99:508–509. [DOI] [PubMed] [Google Scholar]
- 7.Dalmau J, Lancaster E, Martinez-Hernandez E, et al. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011;10:63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]