It is important for oncologists to understand the factors that underpin shared decision making. This article explores real‐world experiences of patients with advanced melanoma receiving pembrolizumab, with a focus on factors that were important to patients when deciding to start immunotherapy.
Keywords: Melanoma, Immunotherapy, Decision‐making, Oncology
Abstract
Background.
Immunotherapy has resulted in unprecedented improvements in survival and maintained quality of life for many patients with advanced melanoma. However, durable responses are observed in only a minority of patients, and severe treatment side effects are experienced by 5%–30%. There are no reliable tests that can differentiate between patients who are likely to respond to immunotherapy and those who will not. Hence, new challenges have arisen as clinicians try to facilitate patients in their decision‐making regarding immunotherapy. Furthermore, little is known about the real‐world patients’ experience and understanding of immunotherapy outside the clinical trial setting. Here, we explore the perspectives of patients undergoing immunotherapy for melanoma and focus on factors that influenced their treatment decision‐making.
Materials and Methods.
Twenty‐three in‐depth semistructured interviews were conducted with patients receiving pembrolizumab for stage IV melanoma at an Australian public cancer hospital. Patients were recruited at a range of time points after commencing therapy, and their experience of treatment was explored. Interviews were audio recorded, transcribed verbatim, coded, and analyzed thematically.
Results.
Immunotherapy is viewed as a symbol of hope, with high‐profile anecdotes reinforcing this perception. Only a minority of patients expressed a good understanding of the likely efficacy and potential treatment side effects. Patients are reliant on their clinicians’ recommendation regarding immunotherapy treatment decisions.
Conclusion.
Novel treatments such as immunotherapy provide significant hope for patients. This may influence their preference for immunotherapy over and above the usual considerations of the trade‐off between efficacy and toxicity. Careful counsel and individualized patient resources may further facilitate treatment decision‐making.
Implications for Practice.
This study highlighted some of the misconceptions held by patients that need to be addressed when discussing the possibility of receiving treatment with immunotherapy for advanced melanoma. Patients placed a lot of importance on high‐profile anecdotes rather than truly understanding likely outcomes of treatment based on personal circumstances. The majority of patients had a poor understanding of the potential side effects and long‐term implications of treatment with immunotherapy. Careful counsel is required in order to facilitate informed decision‐making about treatment and to ensure possible side effects are known and appreciated. Further research is needed to develop tools to aid decision‐making in everyday clinical practice.
Introduction
The treatment of advanced melanoma has changed radically in the past few years. Traditionally, advanced melanoma was associated with poor survival of 6–9 months without treatment [1]. Novel therapies such as immunotherapy (anti‐cytotoxic T lymphocyte antigen‐4, [anti‐CTLA4] or anti‐programmed cell death protein 1 [PD1] monoclonal antibodies) and targeted therapies such as BRAF and MEK inhibitors have revolutionized this, resulting in improved survival and quality of life for many [2], [3], [4], [5], [6], [7], [8]. Furthermore, a minority of patients treated with immunotherapy derive durable response, which can last years [9]. However, immunotherapies with their novel mechanisms of action can result in immune‐mediated side effects including rash, endocrinopathies, and, less frequently, severe toxicities involving pneumonitis, hepatitis, colitis, and myocarditis [4], [10]. Significant challenges have arisen in the clinic for health care providers to balance hope with realistic expectations as patients are counselled on these new treatments [11], [12], [13].
In the oncology setting, it is important for health care providers to understand the factors that underpin shared decision‐making: This allows patients to be autonomous and understand the balance between risks and benefits of different treatment options. There is evidence that patients who engage are more satisfied with the clinical interaction and that experience improved psychosocial and physical outcomes [14], [15]. Given the rapid pace at which these immunotherapies have entered the clinic, little is known about the real‐world experience for patients undergoing these treatments outside of clinical trials. Furthermore, it is not known how well patients understand the treatment decision they are making, and whether there are additional factors patients may find helpful.
To our knowledge, this study is the first qualitative study that uses semistructured interviews to explore real‐world experiences of patients with advanced melanoma currently receiving pembrolizumab (Keytruda; Merck, Kenilworth, NJ), an anti‐PD1 monoclonal antibody. This paper focuses on factors identified as important by patients when deciding to start immunotherapy.
Materials and Methods
Participants
Purposive sampling was used to recruit patients from a specialist cancer center in Melbourne, Australia, between August 2016 and June 2017. Eligibility criteria included a confirmed diagnosis of stage IV melanoma; being treated with pembrolizumab (minimum of two cycles, but there was no limit on the maximum number of cycles received); and age 18 years or over. Patients receiving pembrolizumab in an adjuvant setting were excluded. Patients were ineligible if they had a cognitive or psychological impairment or exhibited signs of distress, as determined by the treating doctor or specialist nurse; had insufficient spoken English or ability to read; were receiving nivolumab; or after receiving cycle one of pembrolizumab at the study site then had subsequent treatments at another health care facility.
Demographic Questionnaire
A brief demographic and clinical data questionnaire was developed for the study. Demographic information was collected on age, sex, marital status, highest level of education completed, living arrangements, current employment situation, occupation, and country of birth. The clinical information included date and stage of initial melanoma diagnosis; date of diagnosis with stage IV melanoma; sites of metastatic disease, as determined by latest imaging; BRAF mutation status; Eastern Cooperative Oncology Group Performance Status; and number of cycles of pembrolizumab received and details of any prior systemic treatment. These data were collected at the beginning of the interview.
Interview
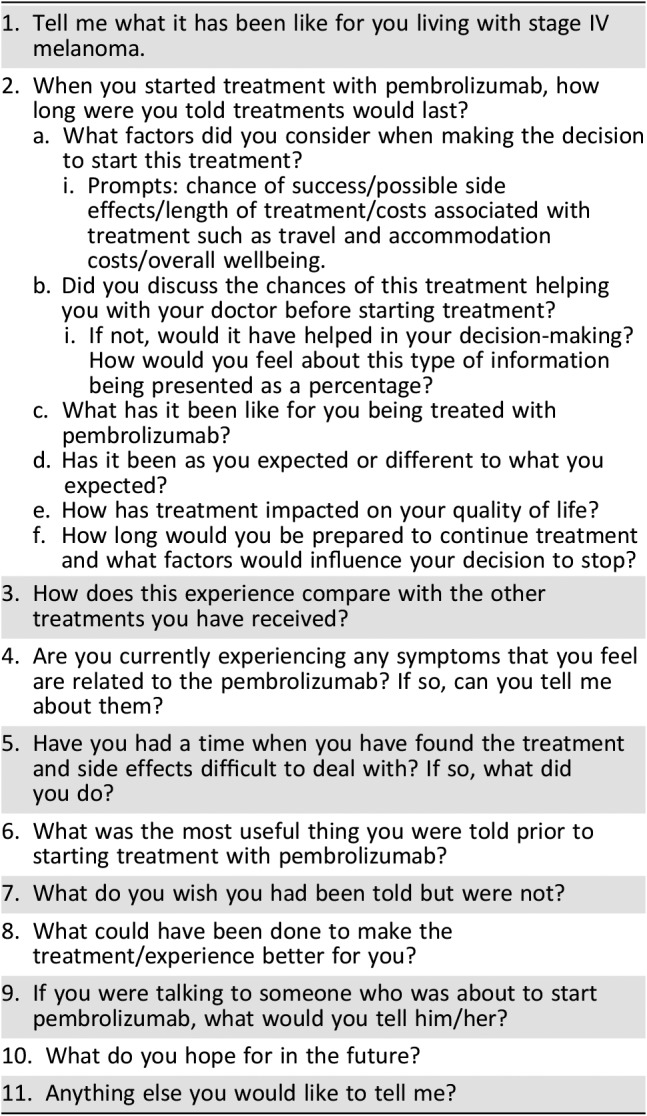
The semistructured interview questions were open‐ended to allow patients to direct the content of the interview. Prompts were included for the interviewer to use to probe and elicit further responses when necessary. Table 1 specifies the questions asked about treatment decision‐making and experience over the course of treatment.
Table 1. Semistructured interview questions.
Recruitment
Patients were identified from outpatient clinic lists, and eligibility was confirmed with the treating doctor or specialist nurse. Patients were approached during planned hospital appointments and recruited at a range of time points (as shown in Table 2) after commencing therapy to ensure a breadth of insight was obtained. Consenting patients were given the option to complete the interview in person or over the phone at a time and date that suited them. Support persons accompanying the patient were also invited to participate in the interview; however, their demographic details were not collected. Patients who did not consent on the day of approach returned written consent via mail. Following this, the researcher called to schedule an appropriate date and time to complete the interview.
Table 2. Demographic and clinical characteristics.
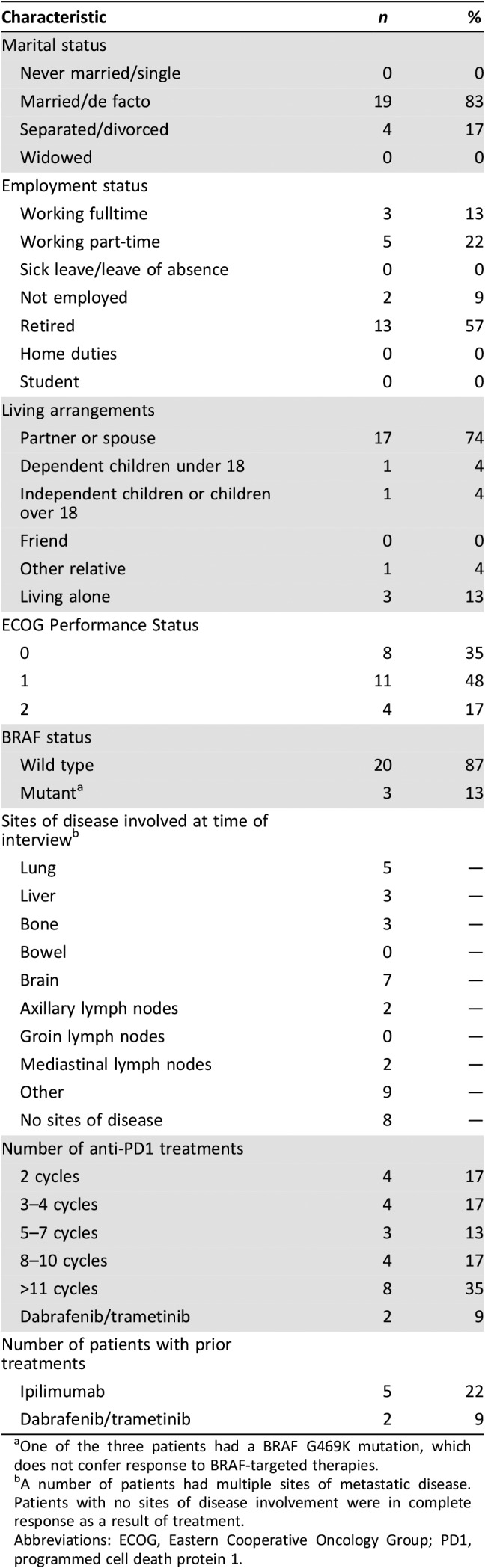
One of the three patients had a BRAF G469K mutation, which does not confer response to BRAF‐targeted therapies.
A number of patients had multiple sites of metastatic disease. Patients with no sites of disease involvement were in complete response as a result of treatment.
Abbreviations: ECOG, Eastern Cooperative Oncology Group; PD1, programmed cell death protein 1.
Qualitative Data Analysis
Interviews were audio‐recorded and transcribed verbatim, with identifying information removed. To ensure the interpretive reliability of the analysis, all transcripts were coded, and analyzed thematically by two independent qualitative researchers (A.W. and D.M.). An inductive approach to analysis was used. Findings were generated from the data rather than imposing a predetermined structure for the analysis. Analysis commenced with listening to audio recordings and reading all interview transcripts. Analysis of the text was then used to generate the initial categories (open coding) and then grouped into subthemes of related categories. Subthemes were sorted, synthesized, and organized to develop broader themes. All authors met to discuss the findings and to clarify and reach consensus on themes. Quotes were selected by A.W., A.B., and D.M. to highlight recurring themes.
Results
Twenty‐three in‐depth semistructured interviews were conducted by two interviewers (A.W. and A.B.) with patients receiving pembrolizumab for stage IV melanoma at a specialist cancer center in Melbourne, Australia. Of the 65 eligible patients, 35 were approached and 29 consented to participate (83% consent rate). Interviews lasted an average of 24 minutes, (range 11–43 minutes). Reasons for refusing or not completing the interview included changing treatments (n = 1), being lost to follow‐up (n = 3), withdrawing at time of interview (n = 1), and dying before the interview was completed (n = 1). Reasons for not being approached despite being eligible included the patient not attending their appointment, the patient being missed in clinic, and data saturation being reached for a particular group (i.e., >11 doses of Keytruda) and thus requiring no further interviews. The average age of patients was 68 years (SD = 12 years; range = 34–92 years). The majority (87%) were male. Additional demographic and clinical characteristics are detailed in Table 2.
Concepts That Influenced Decision‐Making
Four key concepts were identified from the data and will be discussed in turn: (a) The need for hope, (b) Perceptions of toxicity, (c) Clinician recommendation, and (d) Health literacy.
The Need for Hope.
Most patients perceived immunotherapy as a symbol of hope, and many reported reading about immunotherapy in the media. There had been several high‐profile anecdotes of politicians, businessmen, and sporting celebrities who have had prolonged responses to immunotherapy, and patients were hopeful that their disease would respond in the same way.
Interviewer: Were you told about how likely it was that this treatment was going to work? Did the absolute percent make any difference to you?
Patient: “I don't know whether it was 70% or 30% I can't really remember. I think the shock of that was the [diagnosis] and I suppose the Keytruda it does give you the hope. That's the main thing is having hope. That eventually, they [melanoma metastases] will all clear up or something and then I can look after my daughter…again.” – Female, 70 years of age, six cycles.
“Jimmy Carter ‐ sometimes it's those anecdotes that really stick in your mind yeah.” – Male, 73 years of age, >11 cycles.
“Oh no just that they were very, very confident of it…the success they've had with it has been terrific…it's a huge breakthrough they reckon.” – Male, 74 years of age, two cycles.
Most patients reported the availability of treatment that could potentially provide them with longer survival as the most important thing they were told prior to starting treatment. Again, most patients reported that they would tell other patients who are about to embark on treatment that they should just start the treatment, and that it provides hope.
Interviewer: If you were talking to someone else who was about to start Keytruda, what would you tell them?
Patient: “Well I'd just tell them it's like a miracle really.” – Female, 79 years of age, four cycles.
Perception of Toxicity.
Patients perceived immunotherapy to be very safe, and some patients were not able to recall any of the potential toxicities described by their medical oncologist or cancer nurse. Some patients still referred to immunotherapy as “chemotherapy” with reference to the nausea they experienced.
Interviewer: Do you remember getting told any numbers of how likely it was that this drug would work for you?
Patient: “No they just said that it's got no really known bad side effects.” – Male, 74 years of age, two cycles.
“I think they said you know it was skin irritation. I can't think of much else that they um talked about. I think that was them [potential side effects], that seems to be the main thing.” – Male, 72 years of age, four cycles.
“They gave me that booklet thing. I've read that through and through probably 10 times. It's says there maybe a few like minor side effects…mine's loss of appetite. Tiredness it does mention.” – Male, 74 years of age, two cycles.
A number of patients did not see the connection between their symptoms and treatment with immunotherapy; this raises concerns about the effectiveness of patient education, which emphasizes early reporting of symptoms, thereby allowing early intervention.
“I put the diarrhea and belly pain down to Thai food the day before; I was shocked when they talked about putting me in hospital.” – Male, 60 years of age, eight cycles.
“It's hard to tease out what is the heart problems and what is the Keytruda.” – Male, 84 years of age, >11 doses.
“Oh I haven't had any real side effects besides rash.” Then over the course of the interview describes headache, dizziness, daily diarrhea. – 54 years of age, >11 cycles.
Patients commonly reported their oncology team or their nurse specialist as being the first port of call if they experienced side effects to the treatment. Although patients commonly reported having a good rapport with their general practitioner, this did not translate into confidence in their knowledge of immunotherapy or expertise in dealing with side effects. This lack of confidence also extended to the local hospital.
“I think they're just out of their depth with it…[the local hospital] would be a last resort.” – Male, 62 years of age, eight cycles.
Interestingly, two patients who had previous severe immune toxicities from ipilimumab (an anti‐CTLA4 monoclonal antibody) were still prepared to start an anti‐PD1 agent because it represented hope, and would try it even if there was a reasonable possibility of reactivating colitis or polymyositis to the same degree of severity (both patients required hospitalization to manage toxicity, including intensive care admission to treat polymyopathy and neuropathy after ipilimumab). Following treatment with Keytruda, the patient with colitis experienced only a minor rash, whereas the patient with polymyositis had recurrent weakness and a new rash. The quote below was from his wife:
Wife: Doctor said that the Keytruda would [be] less aggressive but unfortunately after he'd had it he started to lose the use of everything again. The only thing, the only way I coped was…I was determined he wasn't going to die.
Clinician Recommendation.
Patients also reported their clinicians’ recommendation about treatment as being very important when it came to their decision. Some noted it was the way the treatment was portrayed by the clinician, whereas others expressed faith that their clinician would have their best interest in mind.
“I just go on the advice of the doctors, what they said was best.” – Male, 60 years of age, four cycles.
Interviewer: Did the likelihood of pembrolizumab working or not working and the side‐effect profile affect your decision?
Patient: “Um no not really no no I just…sort of I had read about the treatment um how it had been fairly successful compared to some of the other ones so I was quite happy to go onto that.” – Male, 60 years of age, four cycles.
“I just do whatever the doctors told me ‘cos they know, I don't…me wife goes into it more than me…I'm basically just putting me life in their hands…They're not going to lie to you or anything…I feel you know they've got your best [interests] at heart…I've talked to me doctor ‘cos, you see on TV all the time all these new treatments.” – Male, 52 years of age, >11 cycles.
“One of the professors said it's [Keytruda] a no brainer.” – Male, 59 years of age, two doses.
Health Literacy.
The majority of patients reported not wanting any additional information other than what was provided to them. Some patients reported not wanting to know the details of efficacy or toxicity because they would not understand the information. Others pointed out that they would prefer to have information that was personalized and included the impact on their comorbid health conditions.
“So you go through all the treatment and specialists, which I must admit confuses me. I just listened to all the specialists and they told me this and that and I said well really there's no good explaining it to me cos I don't understand all that lingo. I said because the simple fact is if I ask them they're going to tell me big layman words which I'm not going to understand…so I mean I walk out there none the wiser.” – Male, 63 years of age, four cycles.
“You know medications, you could sit there 24 hours a day reading material but it has to be put into perspective in terms of each individual client or patient not you know a broad brush stroke and what if you've got this or that.” – Male, 59 years of age, two cycles.
Out of the whole cohort, only two patients (one patient and one family member) were able to correctly recall the percentages of efficacy they were told prior to commencing treatment. Both of these patients reported that it aided them to “prepare for the worst.”
“I read up about the Keytruda, 40% failure rate and because I wasn't feeling lucky…not as hopeful, no no because I thought knowing my luck I'll be amongst the 40%. I made a will and sorted out all me affairs” – Male, 75 years of age, >11 cycles.
Discussion
Immunotherapy has rapidly become the standard of care for patients with advanced melanoma and is now being used extensively to treat other cancers. However, the real‐world experience of patients outside the clinical trials setting is not well characterized. This poses a number of challenges, particularly for health practitioners when counselling patients about choosing treatment with immunotherapy.
These novel therapies have filled an unmet medical need after decades of ineffective therapies for advanced melanoma. Clinicians and media have highlighted success stories, often associated with high‐profile individuals, leading to these therapies being held up as a symbol of hope, not only in melanoma but also in other cancers without effective therapeutic options. Hence, there is growing interest from patients and carers to pursue these treatments, even in patients who may be at risk of low response rates and significant toxicities, such as patients with poor baseline performance status or multiple comorbidities [16]. Communicating trade‐offs between efficacy and toxicity of a treatment is not a new concept in oncology. However, in the case of immunotherapy, this discussion is complicated both by our inability to discern responders from nonresponders a priori and by the perceived efficacy that is emphasized by the media and clinicians. Our patients described perceived hope and held high expectation of efficacy, yet most were unable to provide specific details on likely success rates. Given such high expectations, clinicians have the challenge of providing realistic and balanced counsel regarding the efficacy of these treatments [11], [12]. Some researchers have advocated the use of pictographs to present this sort of information [17], [18]. Even so, many patients in our cohort reported that percentages presented by the clinician were less important than the notion of hope the treatment represented. Given the value patients place on anecdotes, it may be helpful for clinicians to describe “best case/worse case” patient scenarios when discussing treatment options. It was interesting to note that the two patients who were able to accurately recall efficacy statistics found them useful in planning for the worst outcome.
The clinicians’ recommendation was frequently reported as an important factor when considering treatment options. It is difficult to know whether the clinician's recommendation included consideration of the trade‐off between risk and benefit, for that particular patient. Several studies have shown a discrepancy between clinicians’ perceived goal of therapy versus that of the patient [19], [20], [21], [22]; consequently, it would be bold to assume the clinicians were fully aware of any patient's values and preferences when discussing treatment options. The patients’ low recall of both efficacy and toxicity information in our study suggests clinicians may need a range of techniques to aid their communication and highlights the need for individualized educational resources. Patient education needs to be tailored to the individual's health literacy level and learning style, and needs to be delivered at multiple time points (before and throughout the treatment course such as at subsequent clinic visits). The cancer nurse specialist is well placed to do this.
There is growing interest in providing health information not only verbally and in written format but also via other media such as videos or interactive links. Members of our research team have developed a suite of videos called Immunotherapy: what to expect and have made them available on YouTube, with the intent of providing reliable and easily understood information in a different format for patients and their families. In contrast to the notion of providing “general” information, one of our patients with other comorbidities highlighted the need for specific information on the impact of immunotherapy on existing health problems. This requires the clinician to provide individualized information including toxicity estimations, which is challenging given most clinical trials excluded patients with particular comorbidities. Therefore, encouraging and facilitating early reporting of symptoms together with careful monitoring for possible toxicities is important, particularly for patients with multiple comorbidities or underlying autoimmune conditions.
Patients’ perception that immunotherapy has very few side effects may influence their ability to accurately ascribe their symptoms to the treatment. Although the rate of severe side effects (grade 3/4) are indeed lower for anti‐PD1 treatments than for ipilimumab (approximately 10% compared with 19.9%, respectively) in clinical trials [4], patients still need to be aware of these immune toxicities for both treatment decision‐making and monitoring during treatment. Alarmingly, a number of patients did not attribute their side effects to their treatment and only contacted their medical team as a result of this interview. The patients’ inability to link side effects to treatment illustrates their preconceived notions of immunotherapy as causing low levels of toxicity. Again, this highlights the importance of appropriate patient education that will facilitate close monitoring by family and the multidisciplinary oncology team. Unfortunately, some immunotherapy side effects can be subtle and seemingly unrelated; for example, hypopituitarism can be associated with fatigue, headache, and dizziness, indicating hormonal failure. These symptoms can also be associated with cancer itself, so careful monitoring of the patient's baseline symptomatology with prompt reporting of change to a health professional will assist in early diagnosis and management of side effects.
Patients also report their cancer nurse specialist as a source of support when trying to identify and manage toxicities. This highlights the importance of real‐time documentation and good communication between different team members. The nurse specialists at our center attend the patient's appointment with their medical specialist prior to treatment commencing, to facilitate the patient's understanding of the consultation and answer questions. The nurses consult patients via phone on a regular basis or as required due to the patients’ psychosocial situation. Patients and family members commonly report this as helpful and reassuring. These frequent points of contact between the patient and their care team provide opportunities to reinforce toxicity monitoring and appropriate management of side effects.
Some patients, particularly patients living in more remote regional areas, reported a reluctance to attend their local doctor or local hospital as they did not perceive their local health professionals as having sufficient expertise in these novel cancer treatments. Efforts could be made to improve interdisciplinary education on immunotherapy and toxicity profiles and their management. Patients find it helpful and reassuring to have documentation about immunotherapy and early management of toxicities to provide to their local practitioner, particularly as a few continued to describe their treatment as chemotherapy.
Implications for Practice
This study adds to the expanding knowledge about immunotherapy for advanced melanoma. It is, to our knowledge, the first to explore the factors that influence patient decision‐making. It is important for clinicians to be aware of these factors, as patients may have preconceived, and perhaps inaccurate, understanding of treatment. Given the perceived high level of efficacy portrayed by media, coupled with low perceived toxicity rates, it is important for clinicians to specifically discuss these issues when describing their rationale for treatment recommendations. Practical suggestions have been provided to facilitate this decision‐making process as well as monitoring of possible toxicities.
Limitations
Patients were recruited from the outpatient setting at a single hospital; consequently, patients who were unwell and requiring inpatient care were excluded from the study. Furthermore, patients who remain on treatment after a significant number of cycles are those who have benefited from treatment, and are likely to be experiencing only mild side effects, so their responses are likely to be biased in favor of the treatment. It would be interesting for future studies to explore decision‐making regarding not only immunotherapy but also targeted therapies for patients where access to both are available. Nonetheless, this study provides insight into real‐world patients’ experience of anti‐PD1 immunotherapy and some of the factors that are important when considering treatment.
Conclusion
Patients with advanced melanoma report a number of factors that influence their decision to commence immunotherapy: These include a high level of hope, low perceived toxicity, and clinician recommendation. Patients reported a limited understanding of efficacy and potential toxicities related to treatment. Individualized patient information in a range of formats is needed to promote informed decision‐making and accurate and comprehensive reporting and monitoring of side effects.
Acknowledgments
We thank the patients and families for their contribution to this work. Thanks to Bronwyn Sherman for proofreading the manuscript. Annie Wong received a PhD stipend from the Royal Australasian College of Physicians. This study has received funding by Merck. The study and manuscript have been conducted independently to the funder.
This study protocol was approved by the Peter MacCallum Cancer Centre Human Research Ethics Committee (LNR/16/PMCC/44L).
Author Contributions
Conception/design: Annie Wong, Alex Billett, Donna Milne
Provision of study material or patients: Annie Wong, Alex Billett, Donna Milne
Collection and/or assembly of data: Annie Wong, Alex Billett
Data analysis and interpretation: Annie Wong, Alex Billett, Donna Milne
Manuscript writing: Annie Wong, Alex Billett, Donna Milne
Final approval of manuscript: Annie Wong, Alex Billett, Donna Milne
Disclosures
The authors indicated no financial relationships.
References
- 1.Balch CM, Gershenwald JE, Soong Sj. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol 2009;27:6199–6206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hodi FS, Oeday SJ, McDermott DF et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 2010;363:711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ribas A, Puzanov I, Dummer R et al. Pembrolizumab versus investigator‐choice chemotherapy for ipilimumab‐refractory melanoma (KEYNOTE‐002): A randomised, controlled, phase 2 trial. Lancet Oncol 2015;16:908–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robert C, Schachter J, Long GV et al. Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med 2015;372:2521–2532. [DOI] [PubMed] [Google Scholar]
- 5.Long GV, Atkinson V, Ascierto PA et al. Effect of nivolumab on health‐related quality of life in patients with treatment‐naive advanced melanoma: Results from the phase III CheckMate 066 study. Ann Oncol 2016;27:1940–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schadendorf D, Dummer R, Hauschild A et al. Health‐related quality of life in the randomised KEYNOTE‐002 study of pembrolizumab versus chemotherapy in patients with ipilimumab‐refractory melanoma. Eur J Cancer 2016;67:46–54. [DOI] [PubMed] [Google Scholar]
- 7.Long GV, Stroyakovskiy D, Gogas H et al. Dabrafenib and trametinib versus dabrafenib and placebo for Val600 BRAF‐mutant melanoma: A multicentre, double‐blind, phase 3 randomised controlled trial. Lancet 2015;386:444–451. [DOI] [PubMed] [Google Scholar]
- 8.Ascierto PA, McArthur GA, Dreno B et al. Cobimetinib combined with vemurafenib in advanced BRAF(V600)‐mutant melanoma (coBRIM): Updated efficacy results from a randomised, double‐blind, phase 3 trial. Lancet Oncol 2016;17:1248–1260. [DOI] [PubMed] [Google Scholar]
- 9.McDermott D, Lebbe C, Hodi FS et al. Durable benefit and the potential for long‐term survival with immunotherapy in advanced melanoma. Cancer Treat Rev 2014;40:1056–1064. [DOI] [PubMed] [Google Scholar]
- 10.Daud AI, Wolchok JD, Robert C et al. Programmed death‐ligand 1 expression and response to the anti–programmed death 1 antibody pembrolizumab in melanoma. J Clin Oncol 2016;34:4102–4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong A, Fullerton S, Spruyt O et al. Integration of immuno‐oncology and palliative care. J Clin Oncol 2016;34:1561–1562. [DOI] [PubMed] [Google Scholar]
- 12.Temel JS, Gainor JF, Sullivan RJ et al. Keeping expectations in check with immune checkpoint inhibitors. J Clin Oncol 2018;36:1654–1657. [DOI] [PubMed] [Google Scholar]
- 13.Wong A, Williams M, Milne D et al. Clinical and palliative care outcomes for patients of poor performance status treated with antiprogrammed death‐1 monoclonal antibodies for advanced melanoma. Asia Pac J Clin Oncol 2017;13:385–390. [DOI] [PubMed] [Google Scholar]
- 14.Katz SJ, Belkora J, Elwyn G. Shared decision making for treatment of cancer: challenges and opportunities. Journal of oncology practice. 2014;10(3):206‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griffin SJ, Kinmonth AL, Veltman MW et al. Effect on health‐related outcomes of interventions to alter the interaction between patients and practitioners: A systematic review of trials. Ann Fam Med 2004;2:595–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Menzies AM, Johnson D, Ramanujam S et al. Anti‐PD‐1 therapy in patients with advanced melanoma and preexisting autoimmune disorders or major toxicity with ipilimumab. Ann Oncol 2016;28:368–376. [DOI] [PubMed] [Google Scholar]
- 17.Fagerlin A, Wang C, Ubel PA. Reducing the influence of anecdotal reasoning on people's health care decisions: Is a picture worth a thousand statistics? Med Decis Making 2005;25:398–405. [DOI] [PubMed] [Google Scholar]
- 18.Zikmund‐Fisher BJ, Ubel PA, Smith DM et al. Communicating side effect risks in a tamoxifen prophylaxis decision aid: The debiasing influence of pictographs. Patient Educ Couns 2008;73:209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Temel JS, Greer JA, Admane S et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non–small‐cell lung cancer: Results of a randomized study of early palliative care. J Clin Oncol 2011;29:2319–2326. [DOI] [PubMed] [Google Scholar]
- 20.Weeks JC, Catalano PJ, Cronin A et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Monga V, Kaleem H, Mott SC et al. Discrepancy between treatment goals documentation by oncologists and their understanding among cancer patients. J Clin Oncol 2015;33(suppl 15):e20574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gramling R, Fiscella K, Xing G et al. Determinants of patient‐oncologist prognostic discordance in advanced cancer. JAMA Oncol 2016;2:1421–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]


