ABSTRACT
Background: The WHO International Classification of Diseases, 11th version (ICD-11), includes a trauma-related diagnosis of complex posttraumatic stress disorder (CPTSD) distinct from posttraumatic stress disorder (PTSD). Results from previous studies support the validity of this distinction. However, no studies to date have evaluated the ICD-11 model of PTSD and CPTSD in treatment-seeking military veterans.
Objective: To determine if the distribution of symptoms in treatment-seeking Danish veterans was consistent with the ICD-11 PTSD and CPTSD symptom profiles. Based on previous studies, we hypothesized that separate classes representing PTSD and CPTSD would be found that membership of a potential CPTSD-class would be predicted by a larger number of childhood traumas, and that a potential distinction between PTSD and CPTSD would be supported by differences in sociodemographic and functional outcomes.
Method: Participants (N = 1,541) were formerly deployed Danish soldiers who completed proxy measures of ICD-11 PTSD and disturbances in self-organization (DSO) symptoms, along with self-report measures of traumatic life events, prior to starting treatment at the Military Psychology Department of the Danish Defence.
Results: All hypotheses were supported. Latent profile analysis (LPA) revealed separate classes representing PTSD and CPTSD. In comparison to the PTSD-class, membership of the CPTSD-class was predicted by more childhood traumatic experiences, and members of this class were more likely being single/divorced/widowed and more likely to use psychotropic medication. Besides a PTSD-class and a CPTSD-class, LPA revealed a Low Symptoms-class, a Moderate DSO-class, a Hyperarousal-class, and a High DSO-class, with clear differences in functional outcomes between classes.
Conclusion: Findings replicate previous studies supporting the distinction between ICD-11 PTSD and CPTSD. In addition, there seem to be groups of treatment-seeking military veterans that do not fulfil full criteria for a trauma-related disorder. Further research should explore subsyndromal PTSD and CPTSD profiles in veterans and other populations.
KEYWORDS: ICD-11, posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD), military veterans, treatment-seeking persons, latent profile analysis
Antecedentes: La Clasificación Internacional de Enfermedades de la OMS, 11ª versión (CIE-11), incluye un diagnóstico relacionado con el trauma para el trastorno de estrés postraumático complejo (TEPT-C) distinto del trastorno de estrés postraumático (TEPT). Los resultados de los estudios anteriores respaldan la validez de esta distinción. Sin embargo, ningún estudio hasta la fecha ha evaluado el modelo CIE-11 del TEPT y TEPT-C en veteranos militares en busca de tratamiento.
Objetivo: Determinar si la distribución de los síntomas en los veteranos daneses en busca tratamiento fue consistente con los perfiles de los síntomas del TEPT y TEPT-C de la CIE-11. Basados en estudios previos, planteamos la hipótesis de que se encontrarían clases separadas que representan el TEPT y TEPT-C, que la pertenencia a la clase potencial del TEPT-C sería predicha por un mayor número de traumas infantiles, y que una posible distinción entre el TEPT y TEPT-C sería apoyada por las diferencias en los resultados sociodemográficos y funcionales.
Método: Los participantes (N = 1,541) fueron soldados daneses desplegados anteriormente, que completaron medidas indirectas del TEPT CIE-11 y la alteración en los síntomas de autoorganización (DSO en su sigla en inglés), junto con medidas de autoinforme de los eventos traumáticos de la vida, antes de comenzar el tratamiento en el Departamento de Psicología Militar de la Defensa Danesa.
Resultados: Todas las hipótesis fueron sustentadas. El análisis de perfil latente (APL) reveló clases separadas que representan el TEPT y TEPT-C. En comparación con la clase del TEPT, la pertenencia a la clase del TEPT-C fue predicha por más experiencias traumáticas infantiles, y los miembros de esta clase eran más propensos a ser solteros/divorciados/viudos y más propensos a usar medicamentos psicotrópicos. Además de una clase del TEPT y una clase del TEPT-C, el APL reveló una clase de Síntomas Bajos, una clase de DSO Moderado, una clase de Hiperactivación y una clase de DSO Alto, con claras diferencias en los resultados funcionales entre las clases.
Conclusión: Los resultados replican los estudios previos que respaldan la distinción entre el TEPT y TEPT-C del CIE-11. Adicionalmente, parece haber grupos de veteranos militares en busca de tratamiento que no cumplen con los criterios completos para un trastorno relacionado con el trauma. Los estudios futuros deben explorar los perfiles del TEPT y TEPT-C sub-sindrómico en veteranos y otras poblaciones.
PALABRAS CLAVE: CIE-11, Trastorno de Estrés Postraumático (TEPT) y Trastorno de Estrés Postraumático Complejo (TEPT-C), veteranos militares, personas en busca de tratamiento, análisis de perfil latente
背景:世界卫生组织《国际疾病分类》(第11版)(ICD-11)包括一项创伤相关并有别于创伤后应激障碍(PTSD)的复杂创伤后应激障碍(CPTSD)的诊断。前人研究结果支持这种区分的有效性。但是,至今尚无研究在寻求治疗的退伍军人中评估PTSD和CPTSD的ICD-11模型。
目的:确定寻求治疗的丹麦退伍军人中的症状分布是否与ICD-11 PTSD和CPTSD症状剖面一致。基于前人的研究,我们假设可以找到分别代表PTSD和CPTSD的类别,可以通过更多的童年期创伤来预测潜在CPTSD类的成员,并且可以在社会人口学和功能性的结果差异上支持PTSD和CPTSD间的潜在区别。
方法: 1541名参与者曾是丹麦部署士兵,他们在开始丹麦国防部军事心理学部门的治疗之前,完成了ICD-11 标准下PTSD和自我组织障碍(DSO)症状的间接测量,及针对创伤性生活事件的自我报告式测量。
结果:所有假设均得到支持。潜在剖面分析(LPA)结果呈现了分别代表PTSD和CPTSD的类别。相较于PTSD类,属于CPTSD类可由更多的童年期创伤经历预测,且此类人群更可能是单身/离婚/丧偶的,并且更可能服用精神药物。除PTSD类和CPTSD类外,LPA结果还包括低症状类, 中度DSO类, 高唤起类和高DSO类,且各类间的功能性结果存在明显差异。
结论:研究结果重复了前人的研究,支持了ICD-11 中PTSD和CPTSD间的区别。此外,似乎有一些寻求治疗的退伍军人不完全满足创伤相关疾病的标准。进一步的研究应探究退伍军人和其他人群中的亚综合征性PTSD和CPTSD剖面。
关键词: ICD-11, 创伤后应激障碍(PTSD)和复杂性创伤后应激障碍(CPTSD), 退伍军人, 寻求治疗者, 潜在剖面分析
HIGHLIGHTS: • The present study evaluated the ICD-11 model of PTSD and CPTSD in a sample of treatment-seeking military veterans. • Latent profile analysis revealed a CPTSD-class, a PTSD-class, a High DSO-class, a Hyperarousal-class, a Moderate DSO-class, and a Low Symptoms-class. • CPTSD is a more debilitating condition than PTSD. • Compared to the PTSD-class, membership of the CPTSD-class was predicted by increased exposure to childhood traumatic experiences.
1. Introduction
The newly released WHO International Classification of Diseases version 11 (ICD-11) includes two ‘sibling disorders’ within the section on Disorders Specifically Associated with Stress: posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD; Maercker et al., 2013). The ICD-11 model of PTSD is construed as a fear-based response to a specific traumatic event and consists of three symptoms' clusters: (1) re-experiencing of the trauma in the present, (2) avoidance of traumatic reminders, and (3) a persistent sense of threat manifesting as increased arousal and hypervigilance. CPTSD includes the symptoms of PTSD as well as persistent and pervasive ‘disturbances in self-organization’ (DSO) that describe 1) affective dysregulation, 2) negative self-concept, and 3) disturbances in relationships (Maercker et al., 2013).
Herman (1992a, 1992b) first introduced the term complex PTSD, proposing that extreme traumatic or prolonged stress (e.g. childhood abuse, domestic violence, torture) negatively impacted self-organization independently of PTSD symptoms. In the DSM-IV field trials, CPTSD was operationalized under the name ‘disorders of extreme stress not otherwise specified’ (DESNOS; Roth, Newman, Pelcovitz, van der Kolk, & Mandel, 1997). The DSM-IV field trial results indicated that those who had experienced severe or chronic trauma (e.g. torture or childhood abuse) reported higher symptom rates representative of DSO compared to those with a less severe trauma history (van der Kolk, Roth, Pelcovitz, Sunday, & Spinazzola, 2005). Several clinical studies of posttraumatic reactions in samples defined by childhood trauma have confirmed a symptom cluster characterized by disturbances in these domains (e.g. Briere & Rickards, 2007; Dorrepaal et al., 2014; Karatzias et al., 2017).
Since the WHO ICD is the most widely used diagnostic system worldwide, a thorough empirical assessment of the forthcoming ICD-11 models of trauma-based disorders is required. The ICD-11 model of CPTSD predicts that there should be evidence of a CPTSD profile characterized by high endorsement of both PTSD and DSO-symptoms, and a PTSD profile characterized by high endorsement of PTSD symptoms only.
The ICD-11 model of CPTSD has been tested in several studies, usually using mixture models, such as latent class analysis and latent profile analysis (LPA), which identify different homogenous sub-populations that share similar patterns of symptom endorsement (Nylund, Asparouhov, & Muthén, 2007). To the best of our knowledge, 12 mixture model studies on ICD-11 PTSD and CPTSD have been published to date (Böttche et al., 2018; Cloitre, Garvert, Brewin, Bryant, & Maercker, 2013; Cloitre, Garvert, Weiss, Carlson, & Bryant, 2014; Elklit, Hyland, & Shevlin, 2014; Karatzias, Hyland, Ben-Ezra, & Shevlin, 2018; Karatzias et al., 2017; Kazlauskas, Gegieckaite, Hyland, Zelviene, & Cloitre, 2018; Knefel, Garvert, Cloitre, & Lueger-Schuster, 2015; Murphy, Elklit, Dokkedahl, & Shevlin, 2016; Palic et al., 2016; Sachser, Keller, & Goldbeck, 2017; Wolf et al., 2015). All except one (Wolf et al., 2015), previous studies identified the presence of at least two distinct symptom profiles; one describing a group of individuals reporting high levels of CPTSD symptoms in both PTSD and DSO-symptom clusters, another endorsing high levels of PTSD symptoms only.
Consistent with the findings concerning DESNOS in the DSM-IV field trials, several of the above-mentioned studies indicate that childhood trauma experience gives a greater risk for CPTSD development than PTSD (Cloitre et al., 2013, 2014; Hyland et al., 2017; Karatzias et al., 2017; Knefel et al., 2015; Murphy et al., 2016). Moreover, studies have indicated there are sociodemographic and functional correlates which distinguish CPTSD and PTSD (Cloitre et al., 2013, 2014; Karatzias et al., 2017; Perkonigg et al., 2016). A recent study by Karatzias et al. (2017) found that individuals with CPTSD relative to PTSD profiles were more likely to be unemployed, less likely to be married, and more likely to live alone.
To the best of our knowledge, only two studies to date have tested the ICD-11 model of PTSD or CPTSD in veteran samples. Hansen et al. (2017) investigated the diagnostic rates of PTSD based on the DSM-5 and ICD-11 across three trauma samples. Within a Danish veteran sample (N = 321), recruited through an online survey 6-months post-deployment to the Middle East or Afghanistan, PTSD rates according to the DSM-5 were almost twice that of the ICD-11 (9,6% versus 5,3%), but the difference was statistically non-significant (Hansen et al., 2017). In an internet-based study of U.S. military veterans (N = 323), most of whom served in operations Enduring and Iraqi Freedom, Wolf et al. (2015) reported ICD-11 PTSD and CPTSD prevalence to be 21.4% and 13.0%, respectively (Wolf et al., 2015).
No studies to date have tested the ICD-11 model of CPTSD in treatment-seeking military veterans. Based on a large Danish veterans sample seeking treatment for distress following military deployment, the present study aimed to determine if the naturally occurring distribution of symptoms was consistent with the ICD-11 PTSD and CPTSD specifications. In the present study, a veteran is defined according to the definition provided by the Danish Ministry of Defence, as a person who has been deployed to an international mission with the armed forces of their country and may or may not have left the military for a civilian career/education (Danish Ministry of Defence, 2016).
Based on previous studies in other trauma populations, as described above, we hypothesized that qualitatively different groups of participants would emerge reflecting PTSD and CPTSD according to the ICD-11. Specifically, we hypothesized that 1) separate classes representing PTSD and CPTSD would be found, and 2) membership of a potentially occurring CPTSD class would be predicted by more traumatic life events, particularly in childhood, and 3) a potential distinction between PTSD and CPTSD would be associated with differences in sociodemographic and functional outcomes.
2. Methods
2.1. Participants
Data were collected between May 2014 and October 2018 in the Military Psychology Department of the Danish Defence. At intake, all veterans are invited to fill out an on-line administered questionnaire pertaining to their current symptomatology, trauma experience, medication use, and sociodemographic information. For this study, we considered everyone who referred themselves to the Department in the inclusion period (N = 2,561) and filled out the questionnaire (N = 2,248). In total 543 participants were not referred on to treatment after their intake consultation. This might be because their problems were unrelated to their deployment. We therefore excluded these individuals. Finally, 164 individuals referred themselves for treatment more than once during the inclusion period. We included these individuals at their first referral. The final sample consisted of 1,541 individuals. Since we included only participants who completed the questionnaire, we have virtually no missing data (between 0 and 2 missing data points for each item).
2.2. Measures
2.2.1. PTSD and CPTSD
For the main analysis, we used proxy measures resembling the items of the International Trauma Questionnaire (ITQ; Cloitre et al., 2018) that has been developed to measure PTSD and CPTSD as defined in ICD-11. Since the ITQ was not available when the data collection for this project commenced, we used items from the PTSD-checklist, Civilian Version IV (PCL-C; Weathers, Litz, Herman, Huska, & Keane, 1993) and the Depression, Anxiety and Stress Scales with 42 items (DASS; Lovibond & Lovibond, 1995) that closely resemble the ITQ items. Items used and how these compare with respective ITQ items can be seen in Table 1. There has not been an item that corresponds to the ITQ-item ‘I find it hard to stay emotionally close to people’. Furthermore, there was no exact match for the ITQ-item ‘I feel like a failure’. For this item ‘I felt I was pretty worthless’ from DASS was used. The ITQ-item ‘I feel worthless’ was matched with another DASS-item ‘I felt I wasn’t worth much as a person’. Given the difference in semantics between the two items it was decided to keep both. Since the PCL and DASS have different response scales (PCL: 1–5; DASS: 1–4), we rescaled both scales to range from 0 to 1 in order to make them comparable. Hence, for items from both scales, 0 is the lowest possible score, while 1 is the highest possible score. For PCL-items, there are three intermediate scores while for DASS-items, there are two intermediate scores. Cronbach’s alpha for the total scale was 0.90, for the PTSD-subscale it was 0.87 and for the DSO-subscale 0.83.
Table 1.
Items in ITQ and their corresponding items in PCL and DASS.
| Factor | Short names | ITQ items | Test items |
|---|---|---|---|
| PTSD | DREAMS | P1. Having upsetting dreams that replay part of the experience or are clearly related to the experience? | PCL2. Repeated, disturbing dreams of a stressful experience from the past? |
| INTTHOUGHTS | P2. Having powerful images or memories that sometimes come into your mind in which you feel the experience is happening again in the here and now? | PCL1. Repeated, disturbing memories, thoughts, or images of a stressful experience from the past? | |
| AVOTHOUGHT | P3. Avoiding internal reminders of the experience (for example, thoughts, feelings, or physical sensations)? | PCL6. Avoid thinking about or talking about a stressful experience from the past or avoid having feelings related to it? | |
| AVOSIT | P4. Avoiding external reminders of the experience (for example, people, places, conversations, objects, activities, or situations)? | PCL7. Avoid activities or situations because they remind you of a stressful experience from the past? | |
| HYPERVIG | P5. Being ‘super-alert’, watchful, or on guard? | PCL16. Being ‘super alert’ or watchful on guard? | |
| STARTLE | P6. Feeling jumpy or easily startled? | PCL17. Feeling jumpy or easily startled? | |
| CPTSD | UPSET | C1. When I am upset, it takes me a long time to calm down. | DASS29. I found it hard to calm down after something upset me. |
| EMONUMB | C2. I feel numb or emotionally shut down. | PCL11. Feeling emotionally numb or being unable to have loving feelings for those close to you? | |
| WORTHLESS | C3. I feel like a failure. | DASS34. I felt I was pretty worthless. | |
| NOTMUCHWORTH | C4. I feel worthless. | DASS17. I felt I wasn’t worth much as a person. | |
| DISTANT | C5. I feel distant or cut off from people. C6. I find it hard to stay emotionally close to people. |
PCL10. Feeling distant or cut off from other people? |
2.3. Covariates
For prediction of class membership, we investigated the role of lifetime trauma assessed with the Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000). TLEQ lists 19 traumatic events that might have happened during a person’s lifetime, and each item score is the number of times a particular trauma had occurred with an upper limit of six, indicating that the trauma happened six or more times. Three of the 19 TLEQ-items concern childhood trauma; witnessing violence in the family, physical punishment, and sexual abuse. For the purpose of this study, we calculated two sum scores; one for adult trauma (range 0–96) and one for childhood trauma (range 0–18). Given the different range of these two scores, we Z-score transformed them to arrive at meaningful and comparable odds ratios when predicting class membership. In addition to these two trauma variables, we included age and gender as potential class membership predictors. Furthermore, we estimated differences between latent classes in terms of marital status (single/divorced/widowed vs. in a relationship/cohabiting/married), occupational status (Employed/studying vs. Unemployed vs. Sickness benefits), and use of psychotropic medication (Y/N). Psychotropic medication was identified by categorizing self-reported medication using the anatomical therapeutic chemical (ATC) classification system and included psycholeptica (N05) and psychoanaleptica (N06).
2.4. Analyses
Classes were identified by application of LPA as implemented in Mplus version 8.2 (Muthén & Muthén, 1998). In this methodology, classes with differing profiles on the included indicators (here: symptoms of PTSD and CPTSD) are identified in a data-driven manner (McCutcheon, 1987). Common practice in LPA is to initially fit a model to the data with one class, followed by the estimation of models with the continuous addition of extra classes (Nylund et al., 2007). Final model selection is based on theoretical meaningfulness, class sizes, parsimony, and importantly, fit indices expressing how well a model fits the data (Nylund et al., 2007). When evaluating model fit we used the Akaike Information Criteria (AIC; Akaike, 1998), the Bayesian Information Criteria (BIC; Schwarz, 1978), and the sample size adjusted BIC (SSA-BIC) as well as two model comparison tests, the Lo-Mendel-Rubin likelihood ratio test (LMR-LRT; Lo, Mendell, & Rubin, 2001), and the bootstrapped likelihood ratio test (BLRT; McLachlan & Peel, 2000). After selecting the final model based on these criteria, we present the model entropy (classification accuracy measure).
We introduced covariates with two different aims: 1) to explore if membership of the identified classes is predicted by age, gender, and trauma in childhood and adult life, and 2) to estimate differences across classes in terms of marital status, employment status, and use of psychotropic medication. For these aims, we applied a 3-step method where class formation and covariate estimation are done in successive steps while accounting for class assignment insecurity (van de Schoot, Sijbrandij, Winter, Depaoli, & Vermunt, 2017; Vermunt, 2010) twice: once for predicting class membership, and once for testing class differences. For the first aim, we used the CPTSD group as reference (results presented as odds ratios (OR) with a 95% confidence interval (CI)). The nominal statistical level was set to p < 0.05 except for the test of class differences, where we, due to the high number of individual comparisons (15 for each outcome), Bonferroni-corrected the results by adjusting the p-value to 0.003 (0.05/number of comparisons).
3. Results
3.1. Descriptive statistics
The mean (M) sample age was 37 years (standard deviation (SD) = 9.8) and 93.8% were males. Participants experienced on average 6.13 (SD = 3.02, median = 6) unique lifetime traumatic events (range 0–19). In total, 30% (n = 461) endorsed at least one TLEQ-item describing childhood trauma (witnessing violence in the family; 15.7% (n = 242); physical punishment; 22.8% (n = 351); and sexual abuse; 4.3% (n = 67)). The most common index traumatic events were: ‘Combat or war’ (57.2%, n = 882), ‘Sudden unexpected death of someone close’ (8.5%, n = 131), and ‘Other traumatic event’ (7.8%, n = 120).
3.2. LPA results
Table 2 shows fit indices of models with 1–7 classes. AIC, BIC and SSA-BIC are reduced with the addition of every new class, even though the reduction decreases with more classes. Although the LMR-LRT was highly statistically significant with the addition of new classes, with the addition of class seven, LMR-LRT was no longer statistically significant. BLRT was significant with the addition of each new class but could not be computed for the seventh class. The size of the smallest class was reasonable for all estimated models, and for models including up to six classes, the classes were theoretically meaningful and substantially different, indicating a parsimonious model. The addition of the seventh class, however, indicated a non-parsimonious model. Hence, combining perspectives of theoretical meaningfulness and indices of how well the estimated models fit the data, a 6-class model was selected. For this model, the entropy was 0.873. Figure 1 shows the class plot. It was found that 27.3% of the sample belongs to a group with low score on all symptoms (‘Low Symptoms’), while 8.8% score low on the PTSD-symptoms but moderate on the DSO-symptoms (‘Moderate DSO’). Two groups show a medium level of PTSD-symptoms, one of them in combination with medium DSO-symptoms and specifically high hypervigilance (‘Hyperarousal’; 17.2%), the other in combination with high DSO-symptoms (‘High DSO’; 15.4%). Two groups show high levels of PTSD-symptoms; one of them scores high only on PTSD-symptoms (‘PTSD’; 14.1%), the other one score high on PTSD as well as DSO-symptoms (‘CPTSD’; 17.3%).
Table 2.
Fit indices, likelihood ratio tests, and class proportions.
| AIC | BIC | SSA-BIC | LMR-LrT | BLRT | Class proportions (%) | |
|---|---|---|---|---|---|---|
| 1 class | 12,999.5 | 13,117.0 | 13,047.1 | – | – | – |
| 2 classes | 7389.2 | 7570.8 | 7462.7 | p < 0.0001 | p < 0.0001 | 53/47 |
| 3 classes | 6169.0 | 6414.6 | 6268.5 | p < 0.0001 | p < 0.0001 | 34/34/32 |
| 4 classes | 5390.0 | 5700.0 | 5515.8 | p < 0.0001 | p < 0.0001 | 35/23/22/20 |
| 5 classes | 4964.7 | 5338.5 | 5116.1 | p = 0.0021 | p < 0.0001 | 29/20/19/18/14 |
| 6 classes | 4606.2 | 5044.1 | 4783.6 | p = 0.0005 | p < 0.0001 | 27/17/17/15/14/9 |
| 7 classes | 4443.1 | 4945.1 | 4646.4 | p = 0.6882 | – | 27/17/16/15/12/8/5 |
Notes: AIC = Akaike Information Criteria; BIC = Bayesian Information Criteria; SSA-BIC = Sample size adjusted BIC; LMR-LRT = Lo-Mendell-Rubin Likelihood Ratio Test; BLRT = Bootstrapped Likelihood Ratio Test.
Figure 1.
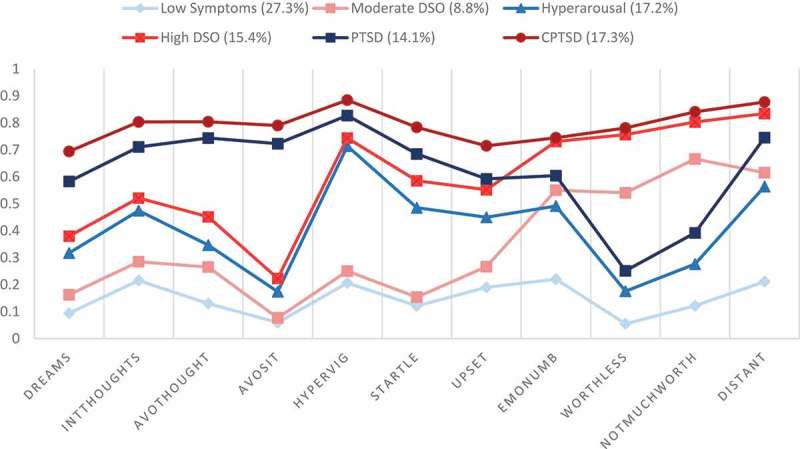
Plot of the 6-class model.
Notes: For readability, classes with low DSO-symptoms are plotted in blue, while classes with elevated DSO-symptoms are plotted in red.
3.3. Prediction of class membership
The results of the multinomial logistic regression analysis with prediction of class membership are reported in Table 3. It was found that older age decreases the risk of belonging to the four classes with lowest symptom levels: Low Symptoms, Moderate DSO, Hyperarousal and High DSO in comparison to the CPTSD class. For gender, it was found that females are less likely to belong to the High DSO class compared to the CPTSD class (OR: 0.23; 95% CI: 0.07–0.71). Childhood trauma decreases the risk of belonging to the PTSD class compared to the CPTSD class (OR: 0.77; 95% CI: 0.64–0.93), while it is not predictive of membership in any other class. Adult life trauma decreases the risk of belonging to the Low Symptoms (OR: 0.51; 95% CI: 0.44–0.61) and the Moderate DSO (OR: 0.54; 95% CI: 0.42–0.71) classes compared to the CPTSD class, while it is not predictive of membership in any other class.
Table 3.
Multinomial regression analysis of being in different classes with the CPTSD class as reference. Results are presented as odds ratios with 95% confidence intervals, * = p < 0.01, **p < 0.001.
| Age | Gender | Childhood traumatic events | Adult life traumatic events | |
|---|---|---|---|---|
| Low Symptoms | 0.66** (0.57–0.77) |
0.92 (0.53–1.57) |
0.90 (0.78–1.03) |
0.51** (0.44–0.61) |
| Moderate DSO | 0.60** (0.58–0.77) |
1.19 (0.60–2.37) |
0.90 (0.72–1.12) |
0.54** (0.42–0.71) |
| Hyperarousal | 0.68** (0.57–0.80) |
0.58 (0.28–1.20) |
0.92 (0.79–1.07) |
0.90 (0.77–1.05) |
| High DSO | 0.74* (0.63–0.88) |
0.23** (0.07–0.71) |
1.01 (0.87–1.18) |
0.86 (0.73–1.01) |
| PTSD | 0.96 (0.82–1.13) |
0.47 (0.20–1.11) |
0.77* (0.64–0.93) |
1.00 (0.86–1.18) |
3.4. Difference in sociodemographic and functional outcomes
Differences between classes in marital status, use of psychotropic medication, and employment are illustrated in Figure 2. The overall comparison of marital status reveals differences across classes (p <0.0001), with the DSO-symptom cluster (Moderate DSO, High DSO, CPTSD) consistently displaying higher risk of being single/divorced/widowed compared to the classes with low DSO-symptoms (Low Symptoms, Hyperarousal, PTSD). For use of psychotropic medication, an overall difference between classes (p <0.0001) was found with higher symptom level (be it symptoms of PTSD or DSO) to be associated with increased proportion of individuals using psychotropic medication (from 5% in the Low Symptoms-class to 40% in the CPTSD-class). All individual class comparisons are statistically significant except Low Symptoms vs. Moderate DSO, Moderate DSO vs. Hyperarousal, Moderate DSO vs. PTSD, High DSO vs PTSD, High DSO vs. CPTSD, and Hyperarousal vs PTSD. Finally, for employment status, an overall difference between classes (p <0.0001) was found. While the unemployment level is relatively stable across groups (from 2%-6%), the proportion of individuals in the group who received sickness benefits is generally increasing with the symptom severity level (from 2% in the Low Symptoms-class to 25% in the CPTSD-class). Specifically, we find that all individual class comparisons are statistically significant except Low Symptoms vs. Moderate DSO, Moderate DSO vs. Hyperarousal, Hyperarousal vs. High-DSO, High-DSO vs. PTSD, High-DSO vs. CPTSD, Hyperarousal vs. PTSD and PTSD vs. CPTSD.
Figure 2.
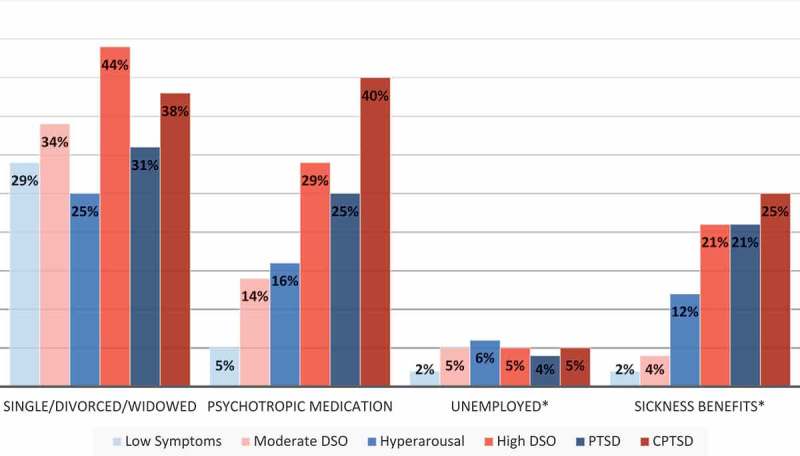
Proportion of individuals in each class who are single/divorced/widowed, uses psychotropic medication, are unemployed or receives sickness benefits.
Notes: For readability, classes with low DSO-symptoms are plotted in blue, while classes with elevated DSO-symptoms are plotted in red. *Unemployed and sickness benefits are coded as a three-category variable (unemployed, sickness benefits, in some way occupied (work, student, etc.)).
4. Discussion
This study aimed to determine if the naturally occurring symptom distribution in treatment-seeking military veterans was consistent with the ICD-11 PTSD and CPTSD specifications. Based on previous studies in other trauma populations, it was hypothesized that qualitatively different groups of participants would emerge with symptom endorsement that reflects PTSD and CPTSD according to ICD-11. Secondly, we hypothesized that membership of a potential CPTSD class would be predicted by higher rates of traumatic life events, particularly in childhood. Finally, we hypothesized that a potential distinction between PTSD and CPTSD would be further supported by differences in sociodemographic and functional outcomes.
All hypotheses were supported. LPA results indicated that a CPTSD-class (17.3%) was clearly distinguishable from a PTSD-class (14.1%). Compared to the PTSD-class, membership of the CPTSD-class was predicted by more childhood traumatic events, and members of the CPTSD-class were more likely of being single/divorced/widowed, and more likely of using psychotropic medication than members of the PTSD-class. In addition to the PTSD and CPTSD classes, we found a Low Symptoms-class (27.3%), a Moderate DSO-class (8.8%), a Hyperarousal-class (17.2%) and a High DSO-class (15.4%). Across all six classes, we found differences in sociodemographic and functional outcomes.
The distinction between two latent classes of participants with high PTSD scores, one scoring high only on PTSD symptoms, the other scoring high on both PTSD and DSO-symptoms, maps onto the ICD-11 specification of CPTSD and replicates findings from previous studies (Böttche et al., 2018; Cloitre et al., 2013, 2014; Elklit et al., 2014; Karatzias et al., 2018, 2017; Kazlauskas et al., 2018; Knefel et al., 2015; Murphy et al., 2016; Palic et al., 2016; Sachser et al., 2017). Consistent with the ICD-11 model of CPTSD, childhood interpersonal trauma was a statistically significant predictor of CPTSD, as compared to PTSD. Several authors have proposed that the DSO symptoms (i.e. affective dysregulation, negative self-concept and disturbances in relationships) be understood as the long-term sequela of childhood trauma. Results of the DSM-IV field trial suggested that traumatic events have the most pervasive impact on an individual during their first decade of life, while those who experience trauma in adulthood are more likely to develop PTSD than CPTSD (van der Kolk et al., 2005). Whilst emerging evidence suggest that childhood trauma is indeed strongly associated with adult CPTSD (Cloitre et al., 2013, 2014; Karatzias et al., 2017; Knefel et al., 2015; Murphy et al., 2016), CPTSD may also develop in adults exposed to extreme circumstances such as combat (Brewin et al., 2017; Cloitre et al., 2013). In this way, trauma history should be viewed as a risk factor rather than a requirement for CPTSD (Brewin et al., 2017). The fact that childhood trauma was not predictive of any other class than the PTSD-class relative to the CPTSD-class indicates that this might be unique to CPTSD risk factor.
Our finding of differences in sociodemographic and functional outcomes between the CPTSD and PTSD classes is in line with and further adds to previous literature. A study by Karatzias et al. (2017) identified a small PTSD-class and a larger CPTSD-class in a clinical sample of treatment-seeing adults and found CPTSD-class members were more likely to be unemployed, less likely to be married and more likely to live alone. In our treatment-seeking military veteran-sample, we find no significant differences between the CPTSD and the PTSD-class with regard to employment status. The unemployment level was generally low in the present sample (from 2% in the Low Symptoms-Class to 6% in the Hyperarousal-class) which corresponds to findings suggesting that Danish soldiers display a good labour market affiliation post-deployment (Elrond, Stoltenberg, Nissen, Nielsen, & Pedersen, 2019). However, veterans with CPTSD, relative to PTSD, were more likely of being single/divorced/widowed, and more likely to use psychotropic medication; supporting the distinction between CPTSD and PTSD in regards to differences in severity of functional impairment, which may have implications for the nature and duration of treatment.
The identification of six qualitatively different classes in our study is somewhat surprising given that previous studies typically identified a PTSD profile, a CPTSD profile, and occasionally a Low Symptoms profile. This might be explained in terms of our study sample size since smaller samples tend to have solutions with fewer classes, while more broadly representative samples tend to have larger number of classes (Brewin et al., 2017). However, there are similarities of our identified classes with those identified by others: for example, the class labelled ‘High DSO’, resembles a profile labelled ‘DSO’ in a LPA community study of 229 predominantly male adult survivors of childhood institutional (Knefel et al., 2015) which identified four latent classes; a PTSD-class, a CPTSD-class, a Low Symptoms-class and a DSO-class, consisting of individuals reporting medium PTSD symptoms and high DSO-symptoms (Knefel et al., 2015). Similar to Knefel et al. (2015) we could speculate that the ‘High DSO’-class in our study might represent individuals with a distinct class of subthreshold CPTSD.
Individuals in the Hyperarousal-class in our study reported elevated levels of hypervigilance, startle response, and affect dysregulation, and no or limited elevation on the DSO-symptoms. This might illustrate that given their training to be hypervigilant, veterans might have specific difficulties letting go of this hypervigilance when they return from deployment (Kimble, Fleming, & Bennion, 2013). It might also be that this group is described most adequately in the context of anxiety and fear disorders, given the symptoms profile of these individuals (elevated sense of threat and affective dysregulation). Finally, we identified a small group of individuals who reported low PTSD symptoms and medium symptoms of emotional numbing, negative self-concept and feeling distant or cut off from other people. We labelled this group Moderate DSO.
Since our study is the first among the LPA-studies to identify six distinct classes, the comparison of all classes warrants a little more attention: Interestingly, when comparing the classes on sociodemographic and functional outcomes, we found statistically significant differences across all classes, indicating that the LPA-derived classes are not spurious, but indeed relevant symptom profiles capturing diverging psychopathologies. While unemployment level was relatively stable across classes, the proportion of individuals receiving sickness benefit generally increased with symptom level. A similar tendency was seen for psychotropic medication use; classes with higher symptom levels also reported use of more psychotropic medication. Remarkably, comparisons between classes revealed that regarding marital status, classes with high DSO-symptoms (Moderate DSO, High DSO, and CPTSD) consistently displayed higher risk of being single/divorced/widowed compared to classes with low DSO-symptom counterparts (Low Symptoms, Hyperarousal, and PTSD). Together, these findings indicate CPTSD not only has higher number of symptoms but also greater functional impairment than any other group of treatment-seeking veterans. Moreover, it is important to highlights that individuals with high DSO-symptoms generally displayed greater functional impairment than individuals with low DSO-symptoms.
In summary, our results provide evidence for a distinct group in our sample that is more accurately captured by the proposed diagnostic category of ICD-11 CPTSD than PTSD. LPA identified three additional symptomatic groups of treatment-seeking veterans; a High DSO profile, a Hyperarousal profile, and a Moderate DSO profile. These groups do not fulfil the criteria for a trauma-related disorder, although they present with some of the symptoms of PTSD/CPTSD. These groups present with clinically significant pathology that would require appropriate support and treatment.
Our results should be considered in light of the following limitations; Firstly, we used proxy measures of ICD 11 PTSD and DSO symptoms. Hence, this measure might have been limited in its ability to measure affective dysregulation, negative self-concept, and disturbances in relationships. Given the finding that individuals with high DSO-items consistently displayed greater functional impairment than individuals with low DSO-symptoms, we do, however, believe that the chosen test items did capture closely enough the DSO-symptom clusters. Future studies in veteran samples should employ disease-specific measures of ICD-11 PTSD and CPTSD in order to validate current results. Second, self-report data were used regarding the occurrence of symptoms and exposure to traumatic events. Therefore, recall-bias cannot be excluded. Third, lifetime trauma was measured with the TLEQ, which only includes three items concerning childhood trauma, and does not include items concerning emotional abuse, emotional neglect or physical neglect in childhood. Furthermore, no military-specific traumatic exposure was measured. Fourth, the study was based on cross-sectional data and it is not known whether the sociodemographic and functional characteristics are causes or consequences (or both) of CPTSD. Finally, in the present study, we did not consider diagnostic comorbidities such as depression, anxiety or substance abuse.
5. Conclusion
Notwithstanding its limitations, this is the first study that demonstrates that the distinction in ICD-11 of PTSD and CPTSD is clinically relevant in a sample of treatment-seeking military veterans. Our findings support the ICD-11 model of CPTSD by 1) identifying distinct groups, or classes, of PTSD and CPTSD, 2) confirming childhood trauma to increase the risk of belonging to the CPTSD class, as compared to the PTSD class, and 3) providing evidence that CPTSD is associated with increased likelihood of being single/divorced/widowed and using psychotropic medication, as compared to PTSD. Because proxy measures were used to measure ICD-11 PTSD and CPTSD criteria, future studies in veteran samples should employ disease-specific measures of ICD-11 PTSD and CPTSD in order to validate these results.
Implications
Compared to PTSD, CPTSD has different types of symptoms, greater severity and greater functional impairment. Therefore, treatments for CPTSD might require a greater number of interventions and/or longer duration to provide CPTSD patients with an end-state health status equal to that obtained by PTSD patients (Karatzias et al., 2019). Future research should aim at developing and testing new treatment approaches for patients with CPTSD. Future research should also explore subsyndromal profiles of ICD-11 PTSD and CPTSD in military and other populations.
Acknowledgments
The authors wish to thank all veterans who filled out the PCL, DASS and TLEQ questionnaires prior to starting treatment at the Military Psychology Department within the Danish Defence.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Akaike H. (1998). Information theory and an extension of the maximum likelihood principle In Parzen E., Tanabe K., & Kitagawa G. (Eds.), Selected papers of Hirotugu Akaike (pp. 199–10). New York, NY: Springer. [Google Scholar]
- Böttche M., Ehring T., Krüger-Gottschalk A., Rau H., Schäfer I., Schellong J., … Knaevelsrud C. (2018). Testing the ICD-11 proposal for complex PTSD in trauma-exposed adults: Factor structure and symptom profiles. European Journal of Psychotraumatology, 9(1), 1512264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin C. R., Cloitre M., Hyland P., Shevlin M., Maercker A., Bryant R. A., … Reed G. M. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–15. [DOI] [PubMed] [Google Scholar]
- Briere J., & Rickards S. (2007). Self-awareness, affect regulation, and relatedness: Differential sequels of childhood versus adult victimization experiences. The Journal of Nervous and Mental Disease, 195(6), 497–503. [DOI] [PubMed] [Google Scholar]
- Cloitre M., Garvert D. W., Brewin C. R., Bryant R. A., & Maercker A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4(SUPPL), 20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M., Garvert D. W., Weiss B., Carlson E. B., & Bryant R. A. (2014). Distinguishing PTSD, complex PTSD, and borderline personality disorder: A latent class analysis. European Journal of Psychotraumatology, 5, 25097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M., Shevlin M., Brewin C. R., Bisson J. I., Roberts N. P., Maercker A., … Hyland P. (2018). The international trauma questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. [DOI] [PubMed] [Google Scholar]
- Danish Ministry of Defence (2016). The veteran policy of Denmark. Copenhagen, Denmark: The Danish Ministry of Defence. [Google Scholar]
- Dorrepaal E., Thomaes K., Hoogendoorn A. W., Veltman D. J., Draijer N., & van Balkom A. J. L. M. (2014). Evidence-based treatment for adult women with child abuse-related Complex PTSD: A quantitative review. European Journal of Psychotraumatology, 5(1), 23613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elklit A., Hyland P., & Shevlin M. (2014). Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology, 5(SUPPL). doi: 10.3402/ejpt.v5.24221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elrond A., Stoltenberg C., Nissen L., Nielsen A., & Pedersen J. (2019). Labor market affiliation after deployment: Danish soldiers fare well, but face increased risk of long-term sickness absence when returning from Afghanistan. Scandinavian Journal of Work, Environment & Health, 45(3), 289–297. [DOI] [PubMed] [Google Scholar]
- Hansen M., Hyland P., Karstoft K.-I., Vaegter H. B., Bramsen R. H., Nielsen A. B. S., … Andersen T. E. (2017). Does size really matter? A multisite study assessing the latent structure of the proposed ICD-11 and DSM-5 diagnostic criteria for PTSD. European Journal of Psychotraumatology, 8(sup7), 1398002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman J. L. (1992a). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5(3), 377–391. [Google Scholar]
- Herman J. L. (1992b). Trauma and recovery. New York: Basic Books. [Google Scholar]
- Hyland P., Murphy J., Shevlin M., Vallières F., McElroy E., Elklit A., … Cloitre M. (2017). Variation in post-traumatic response: The role of trauma type in predicting ICD-11 PTSD and CPTSD symptoms. Social Psychiatry and Psychiatric Epidemiology, 52, 727–736. [DOI] [PubMed] [Google Scholar]
- Karatzias T., Hyland P., Ben-Ezra M., & Shevlin M. (2018). Hyperactivation and hypoactivation affective dysregulation symptoms are integral in complex posttraumatic stress disorder: Results from a nonclinical Israeli sample. International Journal of Methods in Psychiatric Research, 27(4), e1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias T., Murphy P., Cloitre M., Bisson J., Roberts N., Shevlin M., … Hutton P. (2019). Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine, 49(11), 1761–1775. [DOI] [PubMed] [Google Scholar]
- Karatzias T., Shevlin M., Fyvie C., Hyland P., Efthymiadou E., Wilson D., … Cloitre M. (2017). Evidence of distinct profiles of posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD) based on the new ICD-11 trauma questionnaire (ICD-TQ). Journal of Affective Disorders, 207, 181–187. [DOI] [PubMed] [Google Scholar]
- Kazlauskas E., Gegieckaite G., Hyland P., Zelviene P., & Cloitre M. (2018). The structure of ICD-11 PTSD and complex PTSD in Lithuanian mental health services. European Journal of Psychotraumatology, 9(1), 1414559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimble M. O., Fleming K., & Bennion K. A. (2013). Contributors to hypervigilance in a military and civilian sample. Journal of Interpersonal Violence, 28(8), 1672–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knefel M., Garvert D. W., Cloitre M., & Lueger-Schuster B. (2015). Update to an evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse by Knefel & Lueger-Schuster (2013): A latent profile analysis. European Journal of Psychotraumatology, 6(1), 25290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany E. S., Leisen M. B., Kaplan A. S., Watson S. B., Haynes S. N., Owens J. A., & Burns K. (2000). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The traumatic life events questionnaire. Psychological Assessment, 12(2), 210–224. [DOI] [PubMed] [Google Scholar]
- Lo Y., Mendell N. R., & Rubin D. B. (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. [Google Scholar]
- Lovibond P. F., & Lovibond S. H. (1995). The structure of negative emotional states: Comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behaviour Research and Therapy, 33(3), 335–343. [DOI] [PubMed] [Google Scholar]
- Maercker A., Brewin C. R., Bryant R. A., Cloitre M., Reed G. M., van Ommeren M., & Saxena S. (2013). Proposals for mental disorders specifically associated with stress in the ICD-11. Lancet, 381, 1683––1685.. doi: 10.1016/S0140-6736 [DOI] [PubMed] [Google Scholar]
- McCutcheon A. (1987). Latent class analysis. doi: 10.4135/9781412984713 [DOI] [Google Scholar]
- McLachlan G. J., & Peel D. (2000). Finite mixture models. New York: Wiley. [Google Scholar]
- Murphy S., Elklit A., Dokkedahl S., & Shevlin M. (2016). Testing the validity of the proposed ICD-11 PTSD and complex PTSD criteria using a sample from Northern Uganda. European Journal of Psychotraumatology, 7(1), 32678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., & Muthén B. O. (1998). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nylund K. L., Asparouhov T., & Muthén B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. [Google Scholar]
- Palic S., Zerach G., Shevlin M., Zeligman Z., Elklit A., & Solomon Z. (2016). Evidence of complex posttraumatic stress disorder (CPTSD) across populations with prolonged trauma of varying interpersonal intensity and ages of exposure. Psychiatry Research, 246, 692–699. [DOI] [PubMed] [Google Scholar]
- Perkonigg A., Höfler M., Cloitre M., Wittchen H.-U., Trautmann S., & Maercker A. (2016). Evidence for two different ICD-11 posttraumatic stress disorders in a community sample of adolescents and young adults. European Archives of Psychiatry and Clinical Neuroscience, 266(4), 317–328. [DOI] [PubMed] [Google Scholar]
- Roth S., Newman E., Pelcovitz D., van der Kolk B., & Mandel F. S. (1997). Complex PTSD in victims exposed to sexual and physical abuse: Results from the DSM-IV field trial for posttraumatic stress disorder. Journal of Traumatic Stress, 10(4), 539–555. [DOI] [PubMed] [Google Scholar]
- Sachser C., Keller F., & Goldbeck L. (2017). Complex PTSD as proposed for ICD-11: Validation of a new disorder in children and adolescents and their response to trauma-focused cognitive behavioral therapy. Journal of Child Psychology and Psychiatry, 58(2), 160–168. [DOI] [PubMed] [Google Scholar]
- Schwarz G. (1978). Estimating the dimension of a model. The Annals of Statistics, 6(2), 461–464. [Google Scholar]
- van de Schoot R., Sijbrandij M., Winter S. D., Depaoli S., & Vermunt J. K. (2017). The GRoLTS-Checklist: Guidelines for reporting on latent trajectory studies. Structural Equation Modeling: A Multidisciplinary Journal, 24(3), 451–467. [Google Scholar]
- van der Kolk B. A., Roth S., Pelcovitz D., Sunday S., & Spinazzola J. (2005). Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress, 18(5), 389–399. [DOI] [PubMed] [Google Scholar]
- Vermunt J. K. (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18(4), 450–469. [Google Scholar]
- Weathers F. W., Litz B. T., Herman D. S., Huska J. A., & Keane T. M. (1993). The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. Annual Convention of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Wolf E. J., Miller M. W., Kilpatrick D., Resnick H. S., Badour C. L., Marx B. P., … Friedman M. J. (2015). ICD–11 complex PTSD in U.S. National and veteran samples: Prevalence and structural associations with PTSD. Clinical Psychological Science, 3(2), 215–229. [DOI] [PMC free article] [PubMed] [Google Scholar]


