Abstract
Background:
Alpha-fetoprotein (AFP) has been used as a predictor of recurrence for hepatocellular carcinoma (HCC) and disease-free survival post-resection. Studies in East Asia have shown that serum AFP per total tumor volume ratio is a better prognostic indicator than AFP alone. Similar studies in the United States evaluating serum AFPto total tumor volume ratio have not been conducted. Its relevance is incompletely understood.
Methods:
Consecutive patients undergoing resection for HCCat a single tertiary center between 2000 and 2013 were identified for inclusion in this retrospective cohort study. Patient demographics, associated liver disease, Child-Pugh and Model for End-Stage Liver Disease (MELD) scores, pre-operative imaging, surgical pathology, AFPat diagnosis (AFP1), last AFPbefore surgery (AFP2), and peak AFPlevels were recorded. Actual tumor volume by imaging volumetrics was used when available (n=70). For the remaining cases, total tumor volume was calculated using the sum of the volumes of all the tumors ((4/3)πr3) where “r” is the mean radius of each lesion. Peak serum AFPwas used to calculate the AFPto total tumor volume ratio.
Results:
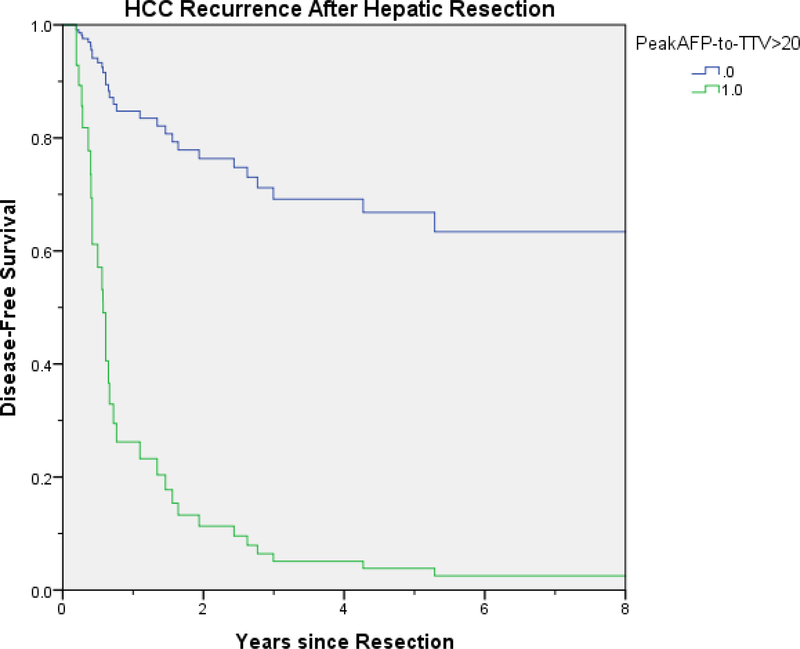
A total of 124 patients resected for HCC between 2000 and 2013 were identified. Overall 1, 3, and 5-year survival post resection was 76%, 53%, and 35%, respectively. On multivariate analysis, peak AFP to TTV ratio > 20 (p<.001, HR=3.72, 95% CI [1.82–7.58]) (Figure 2) and LVSI (lymphovascular space invasion) (p=.002, HR=3.30, 95% CI [1.57–6.94]) were found to affect HCC recurrence-free survival.
Conclusions:
A variety of prognostic values predict the recurrence of HCCpost-resection. Peak pre-operative AFP to TTV ratio > 20 and LVSI has been shown to predict recurrence of HCC. Our study confirms findings from East Asian studies. butlarger series are needed to establish this correlation in patients with HCC not treated by resection.
Keywords: alpha-fetoprotein, hepatocellular carcinoma, hepatectomy, recurrence
Introduction
Alpha-fetoprotein (AFP) has been used as a predictor of recurrence for hepatocellular carcinoma (HCC) and disease-free survival (DFS) post-resection. Serum AFP levels are used commonly as a prognostic indicator of treatment response as well as to estimate the severity of tumor burden 1 Increased AFP levels tend to predict a poor prognosis, as well as HCC recurrence post resection 2,3. A pre-operative AFP greater than 200 ng/ml has been shown previously to be a significant predictor of post-operative recurrence 4, but AFP levels may be increased in conditions other than HCC, including viral hepatitis, increasing age, and inflammation, as well as other neoplastic processes 5,6.
Recurrence of HCC after hepatic resection is an important factor affecting the survival of patients with HCC 7. A variety of factors have been shown to impact the recurrence of HCC post-resection including increases in serum AFP pre-operatively, large tumor size, multifocal HCC, portal vein invasion, cirrhosis, and hepatitis C virus (HCV) positivity 7,8. Studies in East Asia suggest the AFP to tumor volume ratio may be a better prognostic indicator of HCC recurrence than AFP alone. Specifically, the AFP to tumor volume ratio has been shown to negatively correlate with overall survival (OS) and DFS 9.
The primary objective of this study was to determine the utility of AFP to total tumor volume (TTV) ratio as a predictor of HCC recurrence post-resection in a Western population. Secondarily, this study sought to identify factors predicting HCC recurrence in patients followed at a large tertiary academic medical center.
Materials and Methods:
Patient Population
We identified all adult patients (>18 years old) with resected HCC between 2000 and 2013. During this study period, 124 patients were identified using a prospectively maintained database. There were no specific exclusion criteria.
Data Collection
The electronic medical record was used to collect patient data. Patient demographics, associated liver disease, Child-Pugh and Model for End-Stage Liver Disease (MELD) scores, pre-operative imaging, pre-resection treatment, surgical pathology, AFP at diagnosis (AFP1), last AFP before resection (AFP2), and peak AFP levels were recorded. The presence of cirrhosis was evaluated by findings on pathology. The volume of the tumors was calculated with 1) radiologic volumetrics or 2) using the formula ((4/3) πr3) where “r” is the mean radius of each lesion. When original preoperative computed tomography (CT) or magnetic resonanc imaging (MRI) were available (n=70), tumor volume was assessed using VitreaCore 6.7 Vital Images (Figure 1). Each imaging set was reviewed and the phase of contrast providing the greatest distinction between tumor and background was selected. The sculpting tool was used to segment each tumor in a semi-automated fashion to provide a measure of tumor volume in milliliters. When original images were not available, the above formula was used, and tumor radius was derived from the imaging or pathology report. When both imaging and pathologyre[orts were available, the dimensions on the imaging report were used. The TTV was calculated as the sum of the volumes of all tumors for an individual patient. Peak serum AFP levels were used to calculate the AFP to TTV ratio. Pathology reports were reviewed to assess for tumor differentiation and LVSI. Tumor recurrence was defined as pathologically proven, recurrent HCC or imaging evidence of recurrence on subsequent visits.
Figure 1: Tumor volume assessments using VitreaCore 6.7.
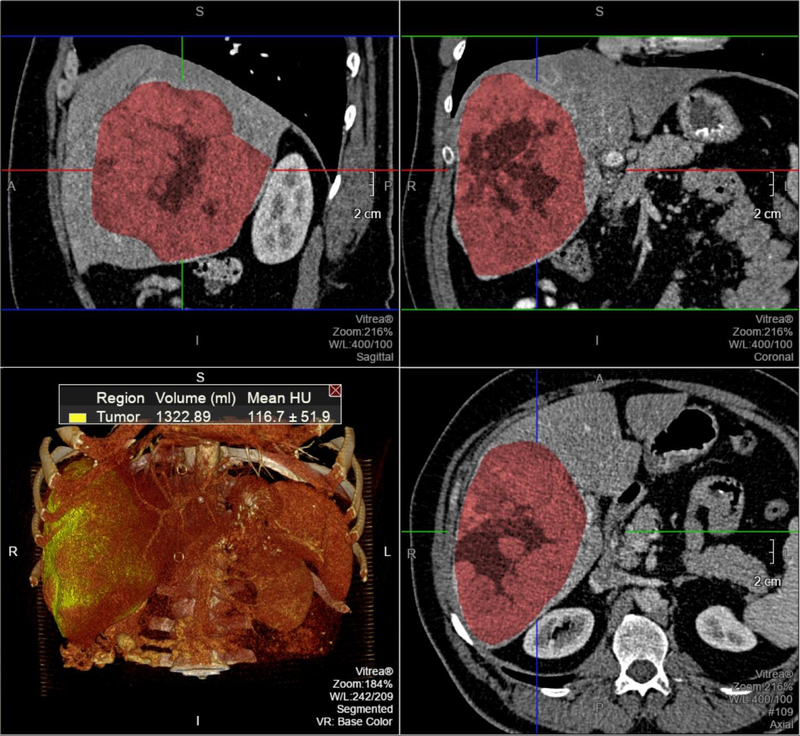
Semi-automated assessment of tumor volume. The tumor was segmented in a semi-automated fashion using VitreaCore, which displays the segmented volume superimposed over the multiplanar reformatted images (top left, top right, and bottom right) and within the volumetric dataset (bottom left).
Statistical Analysis
All statistical analyses were done using SPSS version 22 (IBM SPSS Statistics, IBM Corporation, Armonk, NY). Descriptive statistics for continuous variables (e.g. age) included mean, standard deviation, median, and range whenever appropriate. Categorical variables (e.g. sex) were summarized in frequency distribution. Survival statistics were plotted using the Kaplan-Meier curves and analyzed using the Log-Rank test. Cox regression model was applied for regression analysis. For all comparisons, a p value of <0.05 was considered statistically significant.
Results
Patient Demographics
A total of 124 patients resected for HCC between 2000 and 2013 were identified and included in the analysis (Table 1). The mean patient age at the time of resection was 62.7 ± 13 years.
Table 1.
Baseline characteristics of patients undergoing HCC resection
| Characteristics | Patients with HCC (n= 124) |
|---|---|
| Age (y)* | 62.7 ± 13 |
| Sex (M/F) | 73/51 |
| Ethnicity | |
| Caucasian | 102 |
| Other | 22 |
HCC, hepatocellular carcinoma; M, male; F, female
Mean (standard deviation)
Liver Disease
Cirrhosis was present in 21 patients (16.9%). Hepatitis C- (HCV) related cirrhosis was present in 10 patients, 1 had HBV- (hepatitis B virus) related cirrhosis, and 2 had HBV and HCV-related cirrhosis; 13(10.5%) additional patients had HCV without cirrhosis, and 5 (4.0%) had HBV without cirrhosis (Table 2). The remaining 63.6% of patients had no evidence of pre-existing liver disease. Of the 21 patients with cirrhosis, 16 (76.2%) were Child-Pugh Class A, 4 (19%) were Class B, and one was Class C, as assessed at the time ofresection. The mean calculated MELD score was 9 ± 3, at the time offesection. None of the patients had a history of encephalopathy, and only one had evidence of ascites at the time of resection.
Table 2.
Associated liver disease and tumor characteristics
| Liver Disease/Tumor Characteristics | Patients with HCC (n= 124) |
|---|---|
| Cirrhosis | 21 |
| Chronic HCV | 25 |
| Chronic HBV | 8 |
| Calculated MELD Score* | 9 ± 3 |
| Patients with Solitary Tumors | 106 |
| Mean Largest Tumor Diameter (cm)* | 7.2 ± 4.5 |
| Mean Total Tumor Volume (cm3)* | 327.1 ± 647.3 |
| Poor Tumor Differentiation | 18 |
| Tumor Pre-Treatment | |
| TACE | 15 |
| RFA | 1 |
| TACE+RFA | 1 |
| Lymphovascular Space Invasion | 56 |
| Positive Tumor Margins | 17 |
HCV, Hepatitis C virus; HBV, Hepatitis B virus; MELD, Model For End-Stage Liver Disease; TACE, Transarterial chemoembolization; RFA, Radiofrequency ablation
Mean (standard deviation)
Tumor Volume
The majority of patients (106, 85.5%) had solitary tumors. The mean largest tumor diameter was 7.2 cm (range 1.5–25.5 cm). Mean total tumor volume was 327 cm3 (range 1.2–4905 cm3). Preoperative MRI or CT images were available in 70 (56.5%) patients. In those patients, we performed Bland-Altman analysis and found that tumor volume estimated using average radius and maximum radius had a mean difference of −24.6 ± 1922 cm3 and 168.3 ± 653.6 cm3, respectively, as compared to volumetric assessment (p= 0.289 and p=0.035, respectively). Thus, for patients in whom preoperative imaging was not available, we estimated tumor volume using average radius rather than maximum radius.
A total of 16 (12.9%) patients underwent neoadjuvant treatment. Of those patients, 15 underwent transarterial chemoembolization (TACE) alone, 1 underwent both TACE and radiofrequency ablation (RFA), and 1 had only RFA performed. In terms of resection in the 124 patients, 52 (42%) patients underwent a right hepatectomy, 34 (27%) underwent a left hepatectomy, 30 (24%) underwent segmental resections, 7 (6%) underwent wedge resections, and in one patient underwent extended right hepatectomy. None of the patients had a prior resection for HCC.
On post-resection surgical pathology reports, the tumor was found to be poorly differentiated in 20 (16.1%) cases, well-differentiated in 36 (29%), and moderately differentiated in 63 (51%). Only 3 cases (2.4%) had the fibrolamellar variant and one had undifferentiated pathology;differentiation was not indicated in one case. LVSI by the tumor was reported in 56 (45.2%) cases and positive tumor margins were noted in 17 (13.7%) cases. Based on surgical pathology, 70.1% of the tumors were outside the Milan criteria (39.5% were BCLC class B and 30.6% were BCLC class C).
Alpha-Fetoprotein Levels
Preoperative AFP levels were available in 98 (78%) cases. Mean AFP was 6,744 ng/ml (range 2–160,000) at the time of diagnosis (AFP1), and 6,237 ng/ml (range 2–160,000) closest to the date of resection (AFP2). Peak AFP was 8,609 ± 29,018 ng/ml, with a wide range (2–193,112 ng/ml). Mean AFP1 to TTV ratio was 119 ng/ml/cm3 (range 0.002–7,297), whereas mean AFP2 to TTV ratio was 42.8 ± 163.4 ng/ml/cm3 (range 0.002–1,342). The range for peak AFP to TTV ratio was 0.002 to 48,262.
Analysis of Tumor Recurrence
Of the 124 patients in the study, 48 patients had HCC recurrence. For the management of recurrence, 2 patients underwent salvage liver transplantation, 8 underwent re-resection, 10 underwent TACE, 1 underwent RFA, 1 underwent Y90 radioembolization, 2 underwent combination of RFA and TACE, 2 underwent TACE and Y90, 1 underwent TACE, RFA and Y90, 5 were administered sorafenib, 3 were given unspecified chemotherapy, and 12 were either lost to follow up, placed in hospice. or had death after recurrence.
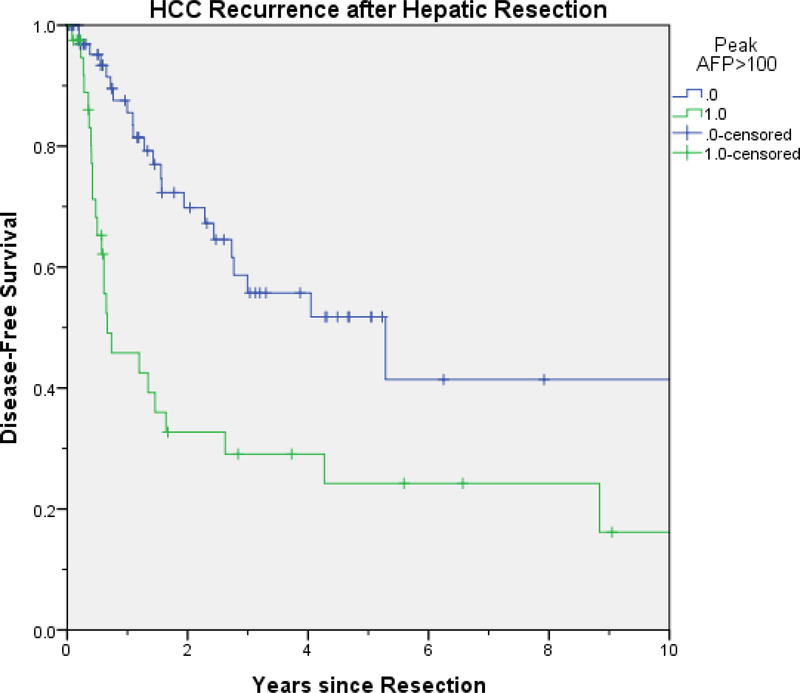
On univariate analysis (Table 3), peak AFP > 100 ng/ml (p<.001), LVSI (p.001), peak AFP to TTV ratio > 20 (p=.001), chronic HCV (p=.001), AFP2 > 100 ng/ml (p=.007), cirrhosis (p=.013), AFP1 > 100 ng/ml (p=.015) and poor tumor differentiation (p=.029) were predictive of disease recurrence; however, on multivariate analysis, only peak AFP to TTV ratio > 20 (p<.001, HR=3.72, 95% CI [1.82–7.58]) (Figure 2 and 3) and LVSI (p=.002, HR=3.30, 95% CI [1.57–6.94]) were found to affect HCC recurrence-free survival (Table 4). One, three, and five-year OSwere 76 %, 53% and 35 %, respectively. HCC recurrence rates were 29%, 54%, and 58 % at one, three, and five years.
Table 3.
Univariate analysis of tumor recurrence
| P Value | |
|---|---|
| Peak AFP > 100 | <.001 |
| Lymphovascular Space Invasion | .001 |
| Peak AFP/TTV > 20 | .001 |
| HCV Liver Disease | .001 |
| AFP2>100 | .007 |
| Cirrhosis | .013 |
| AFP1>100 | .015 |
| Poor Tumor Differentiation | .029 |
| AFP1/TTV > 20 | .051 |
| AFP2/TTV > 20 | .057 |
| Age>65 | .166 |
| Caucasian Race | .217 |
| Gender | .302 |
| HCC Pre-treatment | .364 |
| Tumor Diameter > 5cm | .376 |
| Positive Tumor Margins | .761 |
| HBV Liver Disease | .838 |
| Obesity | .852 |
| Multiple tumors | .872 |
AFP, Alpha-fetoprotein; TTV, Total tumor volume; HCV, Hepatitis C virus; cm, centimeter; HBV, Hepatitis B virus
Figure 2:
Peak AFP/TTV > 20 (green line) predicted HCC recurrence free survival
Figure 3:
Peak pre-operative AFP>100 ng/ml predicted recurrence free survival (green line) on univariate analysis but lost significance on multivariate analysis
Table 4.
Multivariate analysis of tumor recurrence
| P Value | Hazard Ratio | 95% Confidence Interval |
|
|---|---|---|---|
| Peak AFP/TTV >20 | .001 | 3.717 | 1.815–7.576 |
| LVSI | .002 | 3.300 | 1.570–6.944 |
| Cirrhosis | .336 | 1.686 | .582–4.878 |
| AFP1/TTV > 20 | .383 | 1.758 | .495–6.237 |
| AFP1>100 | .451 | 1.734 | .415–7.250 |
| Poor Tumor | .513 | 1.437 | .485–4.255 |
| Differentiation | |||
| HCV Liver Disease | .628 | 1.306 | .444–3.845 |
| Peak AFP>100 | .709 | 1.311 | .316–5.435 |
AFP, Alpha-fetoprotein; LVSI, Lymphovascular space invasion; HCV, Hepatitis C virus
Other parameters tested were AFP1 to TTV ratio > 20 (p=.051), AFP2 to TTV ratio > 20 (p=.057), age > 65 (p=.17), Caucasian race (p=.22), sex (p=.30), HCC pre-treatment (p=.36), largest tumor diameter > 5 cm (p=.376), tumor margins positive for the tumor (p=.761), HBV liver disease (p=.838), obesity (p=.85) and multiple tumors (p=.87); none of these factors affected tumor recurrence on univariate analysis.
The rates of recurrence were also analyzed in patients with peak pre-operative AFP > 100 (35%), and compared to those who were non-secretors (65%). Non-secretors were defined as patients with AFP<100. While 30% of non-secretors developed recurrence, 63% of secretors had recurrent disease (p<0.002). In patients with peak pre-op AFP level and LVSI data available, LVSI was seen in 24/70 (34%) of non-secretors vs, 28/37 (76%) secretors of AFP (p<0.0001).
Discussion
Our study consisting of a large Western population showed that peak AFP to TTV ratio > 20 predicted HCC recurrence post resection. It has been suggested that serum AFP directly correlates to tumor size and that AFP-positive HCC has greater cell proliferative activity than AFP-negative HCC 10,11 In our study, a greater rate of recurrence was seen in patients who were secretors of AFP (AFP>100). These factors likely account for the prognostic significance of peak AFP to TTV ratio. Other factors were assessed to evaluate the risk of HCC recurrence afterresection. This study confirms previous research identifying LVSI as a risk factor for HCC recurrence. We observed greater rates of LVSI in patients who were secretors of AFP, suggesting that secretion of AFP correlates potentially with more aggressive tumor.
Studies in Asia have evaluated the correlation of AFP in the context of HCC resection and recurrence. One study of patients with a perioperative AFP > 400 ng/ml who underwent hepatic resection showed disease recurrence in patients with post-op AFP levels > 20 ng/ml 12. Similar studies assessed patients with pre-operative AFP levels > 100 ng/ml, with follow up levels three months afterresection. Subjects with AFP < 20 ng/ml had a significantly greater DFS(84% vs 18%) one-year after resection 13. These studies were small and included only 66 and 58 patients, respectively. A larger study involving 568 patients showed AFP was a highly reliable index for the disease free state and OSwhen measured pre-resection 14. Finally, a study evaluated 126 patients and showed preoperative AFP > 400 ng/ml, tumor size > 5 cm, and multiple tumors as independent risk factors predicting decreased OS. In addition, vascular invasion was an independent risk factor for OS and DFS post-resection 7. While the clinical efficacy of using preoperative AFP alone to predict post resection recurrence remains controversial, one study sought to identify other means of predicting post resection HCC recurrence. Specifically, an AFP to TTV ratio > 20 was predictive of recurrence within 6 months of resection and may be a better prognostic indicator than AFP alone 9. Until now, no study has been conducted in the United States evaluating the clinical importance or predictive value of preoperative AFP to TTV ratio as a predictor of HCC recurrence.
Our study demonstrated that a preoperative peak AFP to TTV ratio > 20 was a predictive marker of HCC recurrence after resection. Prior studies have demonstrated a correlation between ethnicity and HCC. The Asian population has a greater predisposition to develop HCC 15. Different ethnicities, however, were not assessed. In the future, studies including a more diverse ethnic profile should be conducted. Whether this correlation is applicable to patients treated with chemoradiation rather than resection has not been studied but is another sub-population needing analysis.
Our study consisted of a predominantly Western population and confirmed the results seen in the Asian study. The risk factors for development of HCC in our population, however, were different. . In Asia, the predominant risk factor was HBV, whereas in our Western population this was not the case. Chronic HCV is the leading risk factor for HCC in the United States. In addition, studies have suggested an increasing incidence of obesity and non-alcoholic fatty liver disease (NAFLD) with the development of HCC in the Western population 16. Due to the differences in risk factors and etiology of HCC in the two patient populations, these differences could result in different prognoses.
Our study has several limitations, including the retrospective design and the need to estimate tumor volume rather than being able to measure tumor volume directly in a large portion of our population. As an internal control, however, we compared the estimation of tumor volume against direct measurement with volumetrics in the subset of patients who had imaging available, and we attempted to control for faulty estimation by applying a systematic adjustment. A minority of our patients underwent neoadjuvant therapy. It would be of interest to evaluate the effect of altering the AFP to TTV ratio through neoadjuvant therapy to determine if outcomes improve in future studies. Finally, not all patients have increased serum levels of AFP, and the role of AFP in detecting recurrences in these patients is not well documented.
Despite the availability of new treatments for HCC and therapies to treat the common risk factors for HCC, it is important to evaluate parameters to screen for recurrence. With the help of such parameters, patients can be risk-stratified in terms of follow up. Our study demonstrates patients with a preoperative peak AFP to TTV ratio > 20 or evidence of LVSI on pathology are at a greater risk for recurrence and require closer monitoring. Further studies are needed in this patient population to consider the use of intervention (locoregional or chemotherapy) rather than curative resection.
In conclusion, a variety of prognostic values predict the recurrence of HCC post-resection. On multivariate analysis, only peak pre-operative AFP to TTV ratio >20 and LVSI predicted HCC recurrence post-resection. Our study, consisting of a Western population confirmed the results from prior East Asian studies.
Footnotes
Presented at Digestive Disease Week. May 23rd, 2016. San Diego, California
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arrieta O, Cacho B, Morales-Espinosa D, et al. The progressive elevation of alpha-fetoprotein for the diagnosis of hepatocellular carcinoma in patients with liver cirrhosis. BMC Cancer. 2007;7:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sherman M. Serological surveillance for hepatocellular carcinoma: time to quit. J Hepatol 2010;52:614–615. [DOI] [PubMed] [Google Scholar]
- 3.Kim HS, Park JW, Jang JS, et al. Prognostic values of alpha-fetoprotein and protein induced by vitamin K absence or antagonist-II in hepatitis B virus-related hepatocellular carcinoma: a prospective study. J Clin Gastroenterol 2009;43(5):482–8. [DOI] [PubMed] [Google Scholar]
- 4.Masuda T, Beppu T, Ishiko T, et al. Doubling time of preoperative serum alpha-fetoprotein level can predict recurrence and prognosis after hepatic resection of hepatocellular carcinoma. Journal of Clinical Oncology 2007;28(18):15118. [Google Scholar]
- 5.Tai WC, Hu TH, Wang JH, et al. Clinical implications of alpha-fetoprotein in chronic hepatitis C. J Formos Med Assoc 2009;108(3):210–8. [DOI] [PubMed] [Google Scholar]
- 6.Lee IC, Huang YH, Chan CC, et al. Correlation between clinical indication for treatment and liver histology in HBeAg-negative chronic hepatitis B: a novel role of α-fetoprotein. Liver Int 2010;30(8):1161–8. [DOI] [PubMed] [Google Scholar]
- 7.Park S, Jung Y, Chung D, et al. Factors influencing hepatocellular carcinoma prognosis after hepatectomy: a single-center experience. Korean J Intern Med. 2013;28:428–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Portolani N, Coniglio A, Ghidoni S, et al. Early and later recurrence after liver resection for hepatocellular carcinoma. Ann Surg. 2006;243:229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Furihata T, Sawada T, Kita J, et al. Serum alpha-fetoprotein level per tumor volume reflects prognosis in patients with hepatocellular carcinoma after curative hepatectomy. Hepatogastroenterology. 2008;55:1705–1709. [PubMed] [Google Scholar]
- 10.Toso C, Trotter J, Wei A. Total tumor volume predicts risk of recurrence following liver transplantation in patients with hepatocellular carcinoma. Liver Transplantation. 2008. July; 14 (8): 1107–1115. [DOI] [PubMed] [Google Scholar]
- 11.Toro A, Ardiri A, Mannino M, et al. Effect of pre- and post-treatment α-fetoprotein levels and tumor size on survival of patients with hepatocellular carcinoma treated by resection, transarterial chemoembolization or radiofrequency ablation: a retrospective study. BMC Surgery. 2014;14:40. doi: 10.1186/1471-2482-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shin WY, Suh KS, Kim T, et al. Could patients who underwent hepatic resection due to hepatocellular carcinoma with high alpha-fetoprotein be monitored for recurrence by alpha-fetoprotein level? Korean Journal of Hepatology. 2010. June; 16(2):168–75. [DOI] [PubMed] [Google Scholar]
- 13.Shirabe K, Takenaka K, Gion T, et al. Significance of alpha-fetoprotein levels for detection of early recurrence of hepatocellular carcinoma after hepatic resection. Journal of Surgical Oncology. 1997. February; 64(2):143–6. [DOI] [PubMed] [Google Scholar]
- 14.Kudo A, Matsumura S, Ban D, et al. Does the preoperative alpha-fetoprotein predict the recurrence and mortality after hepatectomy for hepatocellular carcinoma without macrovascular invasion in patients with normal liver function? Hepatology Research. 2014. December; 44 (14): E437–46. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen M, Whittemore A, Garcia R, et al. Role of ethnicity in risk for hepatocellular carcinoma in patients with chronic hepatitis C and cirrhosis. Clin Gastroenterol Hepatol. 2004;2:820–824. [DOI] [PubMed] [Google Scholar]
- 16.Mittal Sahil, and El-Serag Hashem B. “Epidemiology of HCC: Consider the Population.” Journal of clinical gastroenterology 47.0 (2013): S2–S6. PMC. Web. 20 Jan. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]