Abstract
Background
Postpartum depression is a non-psychotic disorder that happens during the first 1year after childbirth. It affects both the mother’s health and child’s development and is given significant public health concern in developed countries. However, in developing countries including Ethiopia, postnatal care is mainly concerned with obstetric problems and the baby’s health, while the psychological well-being of the mother is given little attention. Therefore, this study was aimed to assess the magnitude and associated factors of postpartum depression among women in Nekemte town, East Wollega zone, West Ethiopia, 2019.
Methods
Community-based cross-sectional study was conducted on 295 postnatal women, from May 15 to June 5, 2019, in Nekemte town. The study participants were selected by a simple random sampling method and interviewed using structured questionnaires. Multivariable logistic regression was used to find the independent variables which are associated with postnatal depression. All associations between dependent and independent variables and statistical significance were measured using odds ratio at 95% confidence interval and p-value less than 0.05.
Results
From the total of 295 women sampled, 287 were participated in the study. Out of these 287 women participated, 20.9% had developed postnatal depression. Unplanned pregnancy (AOR = 7.84, 95% CI: 3.19, 19.26), Being first time mother (AOR = 4.99, 95% CI: 1.54, 16.09), History of previous depression (AOR = 3.06, 95% CI: 1.06, 8.82), Domestic violence (AOR = 5.92, 95% CI: 2.44, 14.40), History of substance use (AOR = 3.95, 95% CI: 1.52, 10.30) and poor social support (AOR = 6.59, 95% CI: 2.25, 19.29) were significantly associated with postnatal depression.
Conclusion
In this study, the magnitude of postnatal depression was found moderate compared to other studies. Perinatal depression screening and intervention need to be integrated with maternal health care services, especially for mothers at risk of postnatal depression.
Background
The postpartum period is an increased time of risk for serious mood disorders [1]. Postpartum depression is a non-psychotic condition that happens during the first 1year after childbirth [2]. It usually begins within 1 month of childbirth and may continue for several months [3]. However, it may continue for 4 years after birth [4]. Postpartum depression is manifested by symptoms such as the feeling of unworthy to live, having negative thoughts about the baby, low self-worth and interest, sadness, guilt, anxiety, deeming oneself insubstantial in taking care of the baby, sleeping and eating disorders [5]. In most women, symptoms are transient; however, 10–15% of women experience a persistent form of mood disturbance [6]. Globally, the prevalence of postpartum depression ranges from 0.5% to 60.8% [7]. In developed countries, the prevalence of PPD is about 6–13% [8]. A meta-analysis, including 59 studies from North America, Europe, Australia, and Japan showed the prevalence of postpartum depression as 13% [9]. In low- and middle-income countries, the prevalence of postpartum depression is approximately 20% [10]. In Ethiopia, the prevalence of postnatal depression is about 22.4% [11].
Postnatal depression (PND) is a public health problem affecting both the mother’s health and the child’s development. It has the potential to negatively affect a new mother’s health and her ability to nurture the infant [12]. Postpartum depression can affect the mother’s capacity to care for and bond with her new-born and may react negatively towards the child. [13]. Postpartum depression can lead to poor infant feeding practices, leading to malnutrition and reduced infant growth [14, 15]. PPD can also decrease interaction and bonding between the mother and child, leading to the inadequate social, emotional and cognitive development of the child [16]. PPD occurs at a period when infant development is happening; causing children to have behavioral, cognitive, and emotional problems [17]. Postpartum depression contributes to more than 12.3% disability-adjusted life years [18].
Studies showed that the ill health of a baby, mothers of preterm baby and very low birth weight infants are at increased risk of postnatal depression [19]. Illiteracy, poor socioeconomic status, lack of social support, obstetric complication, previous history of depression, poor marital relationship, history of domestic abuse and unintended pregnancies are also contributing factors of postpartum depression [20–23]. In developed countries, PPD is given significant public health concern. However; in developing countries, it is often neglected and under-diagnosed. In Ethiopia, postnatal care is mainly concerned with obstetric problems and the baby’s health, while the social and psychological well-being of the mother is given little attention. Consequently, little is known about the magnitude of the postpartum depression and contributing factors. Therefore, this study was aimed to assess the magnitude and associated factors of postpartum depression in Nekemte town, west Ethiopia.
Methods
Study design and setting
This study was conducted in Nekemte town from May 15 to June 5, 2019. Nekemte town is the largest town in East Wollega Zone located at a distance of 328 kilometers from capital city Addis Ababa. This town has an estimated total population of 84,506 of whom 42,121 were males and 42, 385 were females. The total number of households in this town is about 16,901 and the number of postpartum women with an infant less than 12 months are estimated to be 2414. The community based cross-sectional study design was employed in this study. All postpartum women in Nekemte town who gave birth within 12 months before data collection were the source population and sampled postpartum women were the study population. All women who gave birth within the last 12 months prior to data collection were included in the study. Postpartum women who are eligible but not willing to take part in the study were excluded from the study.
Sample size determination and sampling techniques
The sample size of the study was calculated using the formula for estimation of a single population proportion with the assumptions of 95% Confidence Level (CL) and marginal error (d) of 0.05. Twenty-two-point four percent (22.4%) of proportion of postpartum women with depression was taken from the previous study done in Mizan Aman town, Bench Maji zone, Southwest Ethiopia [11]. After adding a non-response rate of 10%, a total of 295 postpartum women were enrolled in the study. A simple random sampling method was used to select the study participants. First, postpartum women with an infant less than 12 months of age living in Nekemte town were identified with the help of local extension workers. The data collectors physically visited all households of the town and searched the postpartum women according to our inclusion criteria. The local extension worker assisted the data collectors in the door to door searching of postpartum women. Then, by using simple random sampling methods, a total of 295 postpartum women living in Nekemte town were recruited to be participated in the study.
Measurement and data collection procedure
Data was collected using a validated, pre-tested structured questionnaire and a face-to-face interview was used for data collection. Edinburgh postnatal depression scale (EPDS), 3-item Kansas Marital Satisfaction Scale and 3-item Oslo Social Support Scale were used to assess postpartum depression, level of marital satisfaction and level of social support respectively. EPDS has 10 items and each item has 4 Likert scales and it has a maximum score of 30 and minimum scores of zero. Postpartum women were categorized in to depressed (total sum score ≥10) and not depressed (total sum score <10) [24]. Women with Kansas Marital Satisfaction scale score ≥17 was considered as satisfied and those <17 indicates dissatisfaction with marital status [25]. Women with 3- Items Oslo Social Support Scale score of 3–8 is considered as having poor support, 9–11 is moderate support and 12–15 is strong support [26]. Mothers were considered as a victim of domestic violence when they experienced any of physical, psychological or sexual harm within their intimate relationship. Women were considered as using substances when using any kind of addictive substance during pregnancy or after childbirth measured by yes or no items with at least one yes response. Data was collected by six trained nurses and three senior midwives as a supervisor for a duration of approximately 20 days.
Data processing and analysis
The data were coded, checked, cleaned and entered into Epi data version 3.1 and then exported to SPSS window version 20.0 for analysis. Descriptive statistics such as frequencies and percentages were performed. Bivariate analysis was done to find an association between each independent variable with postpartum depression. Finally, multivariable logistic regression was used to find out the independent variables which influence postpartum depression. All associations between dependent and independent variables and statistical significance were measured using odds ratio at 95% confidence interval and p-value less than 0.05.
Data quality control
The questionnaire was prepared in English language and then translated to local language Afan Oromo and then translated back to English by expertise to check for consistency. Five percent (5%) of the questionnaire was pre-tested on postpartum women living in Gimbi town which is found at about 87 kilometers distance from Nekemte town. Data collectors and supervisors were trained for two days on the clarity of tools and overall data collection procedures. Each day after completion of data collection, data collectors meeting was held and filled questionnaires were cross-checked for possible errors.
Ethical consideration
The study was reviewed and approved by the Institutional Review Boards of Wollega University Ethical review board. A formal letter was submitted to Nekemte town administrative office and Nekemte town health bureau. After getting permission from the Nekemte town administrative office, all participants of the study were provided written consent, clearly stating the objectives of the study and their right to refuse. Participants were interviewed after clearly informing the consent and signing the consent form written in local language. After the mothers signed the written consent form, the data collectors commenced the interview. Filled out questionnaires of the study were also carefully handled and all access to results was kept strictly within the author to prevent unnecessary exposure by third parties.
Results
Socio-demographic characteristics
Out of the total of 295 postnatal women sampled, 287 were participated in the study; making a response rate of 97.28%. From the total of 287 postnatal women who participated in the study, 150 (52.3%) lie in the age group between 25–34 years, and the mean age of the women was 29.6 years with +/- 9.45 standard deviation. Regarding marital status of the women, the majority of the women were married and have husband, which accounts 247 (86.1%). Concerning educational status of the women, 103 (35.9%) were completed grade 9–12, and 95 (33.1%) were completed grade 1–8. The majority of the study participants were Oromo 209 (72.8%), followed by Amhara 50 (17.4%). Regarding the occupation status of the women, 112 (39.0%) were private employees followed by a daily worker, 90 (31.4%). Regarding the monthly income of women, 83 (28.9%) gets a monthly income of 500–100 EB followed by monthly income 1001–1500 EB which accounts for 76 (26.5%) (Table 1).
Table 1. Distribution of study participants by socio-demographic characteristics among postnatal women in Nekemte town, West Ethiopia, 2019 (n = 287).
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| 15–24 | 71 | 24.7 | |
| 25–34 | 150 | 52.3 | |
| >34 | 66 | 23.0 | |
| Total | 287 | 100 | |
| Marital status | Married | 247 | 86.1 |
| Single | 13 | 4.5 | |
| Divorced | 16 | 5.6 | |
| Widowed | 11 | 3.8 | |
| Total | 287 | 100 | |
| Educational status | Can’t read and write | 35 | 12.2 |
| 1–8 grade | 95 | 33.1 | |
| 9–12 grade | 103 | 35.9 | |
| Diploma | 38 | 13.2 | |
| Degree and above | 16 | 5.6 | |
| Total | 287 | 100 | |
| Ethnicity | Oromo | 209 | 72.8 |
| Amhara | 50 | 17.4 | |
| Tigre | 18 | 6.3 | |
| Others | 10 | 3.5 | |
| Total | 287 | 100 | |
| Occupational status | Government employee | 71 | 24.7 |
| Private employee | 112 | 39.0 | |
| Daily worker | 90 | 31.4 | |
| Others | 14 | 4.9 | |
| Total | 287 | 100 | |
| Monthly income | < 500 EB | 44 | 15.3 |
| 500–1000 EB | 83 | 28.9 | |
| 1001–1500 EB | 76 | 26.5 | |
| 1501–2000 EB | 60 | 20.9 | |
| >2000 EB | 24 | 8.4 | |
| Total | 287 | 100 |
Obstetrics and behavioral characteristics
From a total of 287 mothers participated in the study, 81 (28.2%) had an unplanned pregnancy, 18 (6.3%) had a history of preterm birth or death of the infant, 27 (9.4%) had experienced an obstetric complication, and 90 (31.4%) had a history of abortion. Among the respondents, 35 (12.2%) had history of previous depression, 84 (29.3%) were not satisfied with their current marital status, 68 (23.7%) had domestic violence, 38 (13.2%) had experienced stressful life event during pregnancy, and 46 (16.0%) had medical illness during pregnancy. Seventy-one (24.7%) of the study participants had poor social support, 46 (16.0%) had history of substance use, 67 (23.3%) loss job due to pregnancy, 21 (7.3%) had delivered by caesarian section and 45 (15.7%) delivered their baby at home (Table 2).
Table 2. Distribution of study participants by obstetrics and behavioral variables among postnatal women in Nekemte town, West Ethiopia, 2019 (n = 287).
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Pregnancy type | Planned | 206 | 71.8 |
| Unplanned | 81 | 28.2 | |
| Total | 287 | 100 | |
| Preterm/death of infant | Yes | 18 | 6.3 |
| No | 269 | 93.7 | |
| Total | 287 | 100 | |
| Obstetric complication | Yes | 27 | 9.4 |
| No | 260 | 90.6 | |
| Total | 287 | 100 | |
| Postnatal week | <3 months | 62 | 21.6 |
| 3–5 months | 90 | 31.4 | |
| 6–8 months | 85 | 29.6 | |
| 9–12 months | 50 | 17.4 | |
| Total | 287 | 100 | |
| Number of parities | 1 | 64 | 22.3 |
| 2–4 | 154 | 53.7 | |
| >4 | 69 | 24.0 | |
| Total | 287 | 100 | |
| Mode of delivery | Vaginal | 205 | 71.4 |
| Caesarian section | 21 | 7.3 | |
| Instrumental delivery | 61 | 21.3 | |
| Total | 287 | 100 | |
| History of abortion | Yes | 90 | 31.4 |
| No | 197 | 68.6 | |
| Total | 287 | 100 | |
| Place of delivery | Health facility | 242 | 84.3 |
| Home | 45 | 15.7 | |
| Total | 287 | 100 | |
| Presence of chronic illness | Yes | 36 | 12.5 |
| No | 251 | 87.5 | |
| Total | 287 | 100 | |
| History of previous depression | Yes | 35 | 12.2 |
| No | 252 | 87.8 | |
| Total | 287 | 100 | |
| Current marital satisfaction | Yes | 203 | 70.7 |
| No | 84 | 29.3 | |
| Total | 287 | 100 | |
| Domestic violence | Yes | 68 | 23.7 |
| No | 219 | 76.3 | |
| Total | 287 | 100 | |
| Jobless due to pregnancy | Yes | 67 | 23.3 |
| No | 220 | 76.7 | |
| Total | 287 | 100 | |
| Substance use | Yes | 46 | 16.0 |
| No | 241 | 84.0 | |
| Total | 287 | 100 | |
| Social support | Poor | 71 | 24.7 |
| Moderate | 144 | 50.2 | |
| Strong | 72 | 25.1 | |
| Total | 287 | 100 | |
| Stressful life event | Yes | 38 | 13.2 |
| No | 249 | 86.8 | |
| Total | 287 | 100 | |
| Presence of medical illness | Yes | 46 | 16.0 |
| No | 241 | 84.0 | |
| Total | 287 | 100 |
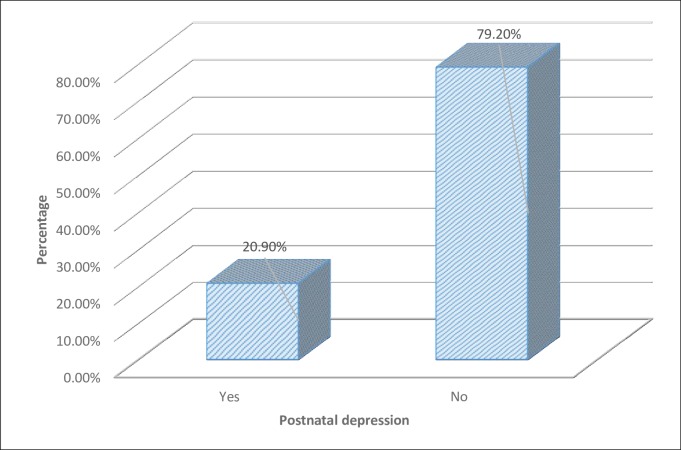
Magnitude of postnatal depression
The magnitude of postnatal depression was assessed by the Edinburgh postnatal depression scale (EPDS) which has 10 items. Postpartum women were categorized into depressed (total sum score ≥10) and not depressed (total sum score <10). Accordingly, out of the total of 287 study participants participated in the study, 60 (20.9%) had developed postnatal depression and 227 (79.1%) hadn’t developed postnatal depression (Fig 1).
Fig 1. Magnitude of postnatal depression among women in Nekemte town, East Wollega zone, West Ethiopia, 2019.
Bivariate logistic regression analysis
In bivariate logistic regression analysis, socio-demographic variables such as age and monthly income showed a significant association with postnatal depression. Obstetric variables such as pregnancy type, the postnatal week during an interview, history of abortion, number of parities, preterm birth or death of an infant, presence of medical illness during last pregnancy, mode, and place of delivery showed significant association with postnatal depression. Behavioral and social variables such as current marital satisfaction, domestic violence, jobless due to pregnancy, social support, history of previous depression, stressful life event and substance use showed significant association with postnatal depression (Table 3).
Table 3. Bivariate logistic regression analysis of factors associated with postnatal depression among women in Nekemte town, West Ethiopia, 2019 (n = 287).
| Variables | Postnatal depression | COR (95%) CI | P value | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Age of mother | ||||
| 15–24 | 32 (45.1%) | 39 (54.9%) | 5.95 (2.48, 14.26) | 0.000* |
| 25–34 | 20 (13.3%) | 130 (86.7%) | 1.12 (0.46, 2.68) | 0.807 |
| >34 | 8 (12.1%) | 58 (87.9%) | 1 | |
| Marital status | ||||
| Married | 51 (20.6%) | 196 (79.4%) | 1 | |
| Single | 2 (15.4%) | 11 (84.6%) | 0.69 (0.15, 3.25) | 0.64 |
| Divorced | 5 (31.2%) | 11 (68.8%) | 1.75 (0.58, 5.25) | 0.32 |
| Widowed | 2 (18.2%) | 9 (81.8%) | 0.85 (0.18, 4.07) | 0.84 |
| Educational status | ||||
| Unable to read and write | 10 (28.6%) | 25 (71.4%) | 1.20 (0.31, 4.62) | 0.79 |
| 1–8 grade | 14 (14.7%) | 81 (85.3%) | 0.52 (0.15, 1.83) | 0.30 |
| 9–12 grade | 27 (26.2%) | 76 (73.8%) | 1.06 (0.32, 3.58) | 0.91 |
| Diploma | 5 (13.2%) | 33 (86.8%) | 0.45 (0.10, 1.98) | 0.29 |
| Degree and above | 4 (25.0%) | 12 (75.0%) | 1 | |
| Ethnicity | ||||
| Oromo | 42 (20.1%) | 167 (79.9%) | 1 | |
| Amhara | 11 (22.0%) | 39 (78.0%) | 1.12 (0.53, 2.37) | 0.76 |
| Tigre | 5 (27.8%) | 13 (72.2%) | 1.53 (0.52, 4.53) | 0.44 |
| Others | 2 (20.0%) | 8 (80.0%) | 0.99 (0.24, 4.85) | 0.99 |
| Occupation | ||||
| Government employee | 12 (16.9%) | 59 (83.1%) | 1 | |
| Private employee | 26 (23.2%) | 86 (76.8%) | 1.48 (0.69, 3.12) | 0.30 |
| Daily worker | 20 (22.2%) | 70 (77.8%) | 1.40 (0.63, 3.11) | 0.40 |
| Others | 2 (14.3%) | 12 (85.7%) | 0.82 (0.16, 4.14) | 0.81 |
| Monthly income | ||||
| <500 EB | 16 (36.4%) | 28 (63.6%) | 2.85 (0.83, 9.84) | 0.09* |
| 500–1000 EB | 18 (21.7%) | 65 (78.3%) | 1.38 (0.42, 4.56) | 0.59 |
| 1001–1500 EB | 16 (21.1%) | 60 (78.9%) | 1.33 (0.39, 4.45) | 0.64 |
| 1501–200 EB | 6 (10.0%) | 54 (90.0%) | 0.55 (0.14, 2.17) | 0.39 |
| >2000 EB | 4 (16.7%) | 20 (83.3%) | 1 | |
| Pregnancy type | ||||
| Planned | 22 (10.7%) | 184 (89.3%) | 1 | |
| Unplanned | 38 (46.9%) | 43 (53.1%) | 7.39 (3.97, 13.75) | 0.000* |
| Preterm/death of infant | ||||
| Yes | 5 (27.8%) | 13 (72.2%) | 1.49 (0.51, 4.37) | 0.46 |
| No | 55 (20.4%) | 214 (79.6%) | 1 | |
| Obstetric complication | ||||
| Yes | 8 (29.6%) | 19 (70.4%) | 1.68 (0.69, 4.06) | 0.25 |
| No | 52 (20.0%) | 208 (80.0%) | 1 | |
| Postnatal week | ||||
| <3 months | 21 (33.9%) | 41 (61.1%) | 2.68 (1.07, 6.75) | 0.03* |
| 3–5 months | 15 (16.7%) | 75 (83.3%) | 1.05 (0.41, 2.68) | 0.92 |
| 6–8 months | 16 (18.8%) | 69 (81.2%) | 1.21 (0.48, 3.09) | 0.67 |
| 9–12 months | 8 (16.0%) | 42 (84.0%) | 1 | |
| Number of parities | ||||
| 1 | 23 (35.9%) | 41 (64.1%) | 2.95 (1.30, 6.73) | 0.01* |
| 2–4 | 26 (16.9%) | 128 (83.1%) | 1.07 (0.49, 2.31) | 0.86 |
| >4 | 11 (15.9%) | 58 (84.1%) | 1 | |
| Mode of delivery | ||||
| Vaginal | 42 (20.5%) | 163 (79.5%) | 1 | |
| Cesarean section | 7 (33.3%) | 14 (66.7%) | 1.94 (0.73, 5.11) | 0.18* |
| Instrumental delivery | 11 (18.0%) | 50 (82.0%) | 0.85 (0.40, 1.78) | 0.67 |
| History of abortion | ||||
| Yes | 20 (22.2%) | 70 (77.8%) | 1.12 (0.61, 2.05) | 0.71 |
| No | 40 (20.3%) | 157 (79.7%) | 1 | |
| Place of delivery | ||||
| Health facility | 45 (18.6%) | 197 (81.4%) | 1 | |
| Home | 15 (33.3%) | 30 (66.7%) | 2.18 (1.08, 4.40) | 0.02* |
| Presence of chronic illness | ||||
| Yes | 12 (33.3%) | 24 (66.7%) | 2.11 (0.98, 4.52) | 0.05* |
| No | 48 (19.1%) | 203 (80.9%) | 1 | |
| History of previous depression | ||||
| Yes | 13 (37.1%) | 22 (62.9%) | 2.57 (1.21, 5.48) | 0.01* |
| No | 47 (18.7%) | 205 (81.3%) | 1 | |
| Current marital satisfaction | ||||
| Yes | 37 (18.2%) | 166 (81.8%) | 1 | |
| No | 23 (27.4%) | 61 (72.6%) | 1.69 (0.93, 3.07) | 0.08* |
| Domestic violence | ||||
| Yes | 33 (48.5%) | 35 (51.5%) | 6.70 (3.59, 12.50) | 0.000* |
| No | 27 (12.3%) | 192 (87.7%) | 1 | |
| Jobless due to pregnancy | ||||
| Yes | 18 (26.9%) | 49 (73.1%) | 1.55 (0.82, 2.94) | 0.17* |
| No | 42 (19.1%) | 178 (80.9%) | 1 | |
| Substance use | ||||
| Yes | 23 (50.0%) | 23 (50.0%) | 5.51 (2.80, 10.83) | 0.000* |
| No | 37 (15.4%) | 204 (84.6%) | 1 | |
| Social support | ||||
| Poor | 34 (47.9%) | 37 (52.1%) | 7.35 (3.08, 17. 54) | 0.000* |
| Moderate | 18 (12.5%) | 126 (87.5%) | 1.14 (0.47, 2.77) | 0.76 |
| Strong | 8 (11.1%) | 64 (88.9%) | 1 | |
| Stressful life event | ||||
| Yes | 11 (28.9%) | 27 (71.1%) | 1.66 (0.77, 3.58) | 0.19* |
| No | 49 (19.7%) | 200 (80.3%) | 1 | |
| Presence of medical illness | ||||
| Yes | 13 (28.3%) | 33 (71.7%) | 1.62 (0.79, 3.33) | 0.18* |
| No | 47 (19.5%) | 194 (80.5%) | 1 |
Notes * shows significant at P-value <0.25.
Multivariate logistic regression analysis
In the final model of logistic regression analysis, pregnancy type, number of parities, history of previous depression, domestic violence, substance use, and social support were significantly associated with postnatal depression. Mothers who had unplanned pregnancy were 7.84 times more likely to develop postnatal depression than those who had planned pregnancy (AOR = 7.84, 95% CI: 3.19, 19.26). Mothers who gave birth for the first time were 4.99 times more likely to develop postnatal depression than those who gave birth more than four times (AOR = 4.99, 95% CI: 1.54, 16.09). Mothers who had a history of previous depression were 3.06 times more likely to develop postnatal depression than those who had no history of previous depression (AOR = 3.06, 95% CI: 1.06, 8.82). Mothers who had experienced domestic violence were 5.92 times more likely to develop postnatal depression than those who had not experienced domestic violence (AOR = 5.92, 95% CI: 2.44, 14.40). Mothers who had a history of substance use were 3.95 times more likely to develop postnatal depression than those who had no history of substance use (AOR = 3.95, 95% CI: 1.52, 10.30). Mothers who had poor social support were 6.59 times more likely to develop postnatal depression than those who had strong social support (AOR = 6.59, 95% CI: 2.25, 19.29) (Table 4).
Table 4. Multivariate logistic regression analysis of factors associated with postnatal depression among women in Nekemte town, West Ethiopia, 2019 (n = 287).
| Variables | Postnatal depression | AOR (95%) CI | P value | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Age of mother | ||||
| 15–24 | 32 (45.1%) | 39 (54.9%) | 0.11 (0.01, 0.99) | 0.05 |
| 25–34 | 20 (13.3%) | 130 (86.7%) | 0.16 (0.07, 3.94) | 0.26 |
| >34 | 8 (12.1%) | 58 (87.9%) | 1 | |
| Marital status | ||||
| Married | 51 (20.6%) | 196 (79.4%) | 1 | |
| Single | 2 (15.4%) | 11 (84.6%) | 1.09 (0.13, 8.90) | 0.93 |
| Divorced | 5 (31.2%) | 11 (68.8%) | 0.17 (0.02, 1.46) | 0.10 |
| Widowed | 2 (18.2%) | 9 (81.8%) | 0.19 (0.01, 3.57) | 0.27 |
| Educational status | ||||
| Unable to read and write | 10 (28.6%) | 25 (71.4%) | 2.16 (0.27, 16.85) | 0.46 |
| 1–8 grade | 14 (14.7%) | 81 (85.3%) | 0.50 (0.08, 3.07) | 0.45 |
| 9–12 grade | 27 (26.2%) | 76 (73.8%) | 1.67 (0.26, 10.60) | 0.58 |
| Diploma | 5 (13.2%) | 33 (86.8%) | 0.69 (0.08, 5.56) | 0.73 |
| Degree and above | 4 (25.0%) | 12 (75.0%) | 1 | |
| Ethnicity | ||||
| Oromo | 42 (20.1%) | 167 (79.9%) | 1 | |
| Amhara | 11 (22.0%) | 39 (78.0%) | 0.85 (0.24, 2.95) | 0.80 |
| Tigre | 5 (27.8%) | 13 (72.2%) | 1.84 (0.24, 13.74) | 0.55 |
| Others | 2 (20.0%) | 8 (80.0%) | 0.20 (0.01, 2.64) | 0.22 |
| Occupation | ||||
| Government employee | 12 (16.9%) | 59 (83.1%) | 1 | |
| Private employee | 26 (23.2%) | 86 (76.8%) | 1.24 (0.34, 4.48) | 0.73 |
| Daily worker | 20 (22.2%) | 70 (77.8%) | 1.30 (0.35, 4.87) | 0.69 |
| Others | 2 (14.3%) | 12 (85.7%) | 0.82 (0.06, 10.05) | 0.87 |
| Monthly income | ||||
| <500 EB | 16 (36.4%) | 28 (63.6%) | 1.19 (0.17, 8.08) | 0.85 |
| 500–1000 EB | 18 (21.7%) | 65 (78.3%) | 1.51 (0.22, 10.45) | 0.67 |
| 1001–1500 EB | 16 (21.1%) | 60 (78.9%) | 0.96 (0.15, 6.06) | 0.97 |
| 1501–200 EB | 6 (10.0%) | 54 (90.0%) | 0.61 (0.07, 4.94) | 0.65 |
| >2000 EB | 4 (16.7%) | 20 (83.3%) | 1 | |
| Pregnancy type | ||||
| Planned | 22 (10.7%) | 184 (89.3%) | 1 | |
| Unplanned | 38 (46.9%) | 43 (53.1%) | 7.84 (3.19, 19.26) | 0.000* |
| Preterm/death of infant | ||||
| Yes | 5 (27.8%) | 13 (72.2%) | 0.51 (0.03, 6.88) | 0.61 |
| No | 55 (20.4%) | 214 (79.6%) | 1 | |
| Obstetric complication | ||||
| Yes | 8 (29.6%) | 19 (70.4%) | 3.02 (0.77, 11.74) | 0.11 |
| No | 52 (20.0%) | 208 (80.0%) | 1 | |
| Postnatal week | ||||
| <3 months | 21 (33.9%) | 41 (61.1%) | 3.02 (0.85, 10.66) | 0.085 |
| 3–5 months | 15 (16.7%) | 75 (83.3%) | 0.82 (0.23, 2.88) | 0.75 |
| 6–8 months | 16 (18.8%) | 69 (81.2%) | 1.78 (0.50, 6.22) | 0.36 |
| 9–12 months | 8 (16.0%) | 42 (84.0%) | 1 | |
| Number of parities | ||||
| 1 | 23 (35.9%) | 41 (64.1%) | 4.99 (1.54, 16.09) | 0.007* |
| 2–4 | 26 (16.9%) | 128 (83.1%) | 1.01 (0.38, 2.72) | 0.97 |
| >4 | 11 (15.9%) | 58 (84.1%) | 1 | |
| Mode of delivery | ||||
| Vaginal | 42 (20.5%) | 163 (79.5%) | 1 | |
| Cesarean section | 7 (33.3%) | 14 (66.7%) | 1.86 (0.46, 7.48) | 0.37 |
| Instrumental delivery | 11 (18.0%) | 50 (82.0%) | 0.44 (0.13, 1.49) | 0.18 |
| History of abortion | ||||
| Yes | 20 (22.2%) | 70 (77.8%) | 0.95 (0.33, 2.70) | 0.92 |
| No | 40 (20.3%) | 157 (79.7%) | 1 | |
| Place of delivery | ||||
| Health facility | 45 (18.6%) | 197 (81.4%) | 1 | |
| Home | 15 (33.3%) | 30 (66.7%) | 2.09 (0.73, 5.98) | 0.16 |
| Presence of chronic illness | ||||
| Yes | 12 (33.3%) | 24 (66.7%) | 2.62 (0.59, 11.54) | 0.20 |
| No | 48 (19.1%) | 203 (80.9%) | 1 | |
| History of previous depression | ||||
| Yes | 13 (37.1%) | 22 (62.9%) | 3.06 (1.06, 8.82) | 0.03* |
| No | 47 (18.7%) | 205 (81.3%) | 1 | |
| Current marital satisfaction | ||||
| Yes | 37 (18.2%) | 166 (81.8%) | 1 | |
| No | 23 (27.4%) | 61 (72.6%) | 1.51 (0.52, 4.39) | 0.45 |
| Domestic violence | ||||
| Yes | 33 (48.5%) | 35 (51.5%) | 5.92 (2.44, 14.40) | 0.000* |
| No | 27 (12.3%) | 192 (87.7%) | 1 | |
| Jobless due to pregnancy | ||||
| Yes | 18 (26.9%) | 49 (73.1%) | 0.97 (0.29, 3.20) | 0.96 |
| No | 42 (19.1%) | 178 (80.9%) | 1 | |
| Substance use | ||||
| Yes | 23 (50.0%) | 23 (50.0%) | 3.95 (1.52, 10.30) | 0.005* |
| No | 37 (15.4%) | 204 (84.6%) | 1 | |
| Social support | ||||
| Poor | 34 (47.9%) | 37 (52.1%) | 6.59 (2.25, 19.29) | 0.001* |
| Moderate | 18 (12.5%) | 126 (87.5%) | 1.51 (0.52, 4.37) | 0.44 |
| Strong | 8 (11.1%) | 64 (88.9%) | 1 | |
| Stressful life event | ||||
| Yes | 11 (28.9%) | 27 (71.1%) | 0.74 (0.17, 3.10) | 0.68 |
| No | 49 (19.7%) | 200 (80.3%) | 1 | |
| Presence of medical illness | ||||
| Yes | 13 (28.3%) | 33 (71.7%) | 1.84 (0.57, 5.97) | 0.30 |
| No | 47 (19.5%) | 194 (80.5%) | 1 | |
Notes * shows significant at P-value <0.05
Discussion
This study examined the magnitude of postnatal depression and associated factors among mothers who gave birth within 12 months in Nekemte town, West Ethiopia. The magnitude of postnatal depression among postnatal women in this study is 20.9%. This level of postnatal depression is almost similar with study done in Udupi Taluk, India (21.5%) [27], public hospitals of Addis Ababa (23.3%) [28], Benchi Maji Zone, Ethiopia (22.4%) [29] and Kenya (18.7%) [30]. However; it is lower than a study done in Southwest Ethiopia (33.82%) [31], Vietnam (27.6%) [32], China (30%) [33] and Bangladesh (39.4%) [34]. On the other hand, the level of postnatal depression in this study is higher than study done in Netaji Subhash medical college, India (12.8%) [35], Ghana (7%) [36], Sudan (9.2%) [37] and Eastern province capital of Saudi Arabia (17.8%) [38]. The difference might be due to variation in data collection tool (different measurement scale for measuring depression), use of different cutoff points of EDPS score, sample size, sampling methods, study setting and study participant’s variation.
In this study, factors such as pregnancy type, number of parities, history of previous depression, domestic violence, substance use, and social support were significantly associated with postnatal depression. Mothers who had unplanned pregnancy were found to be more likely to develop postnatal depression than those who had planned pregnancy. This might be due to the fact that inadequate preparation for pregnancy and childbirth make the mothers unable to cope with the challenges and feel anxious. An unplanned pregnancy may also lead to economic burden and social judgment on the women which may be responsible for postnatal depression. This finding is consistent with the study done in South West Ethiopia [31], Bangladesh [34], public hospitals of Addis Ababa [28] and Benchi Maji Zone, Ethiopia [29]. In this study, mothers who gave birth for the first time were more likely to develop postnatal depression than those who gave birth more than four times This finding is consistent with a study done in Vietnam [32] and contradict with study done in Udupi Taluk, India [27]. Majorities of other studies done in different parts of countries don’t support this finding [29, 31, 34, 36, 38].
The finding of this study also showed that those who had a history of previous depression were more likely to develop postnatal depression than those who had no history of previous depression. This finding showed that postnatal depression is not only a problem which occurs during the postpartum period and indicated the importance of intervention in the prenatal period to prevent postnatal depression. This result is consistent with the study done in the Benchi Maji Zone, Ethiopia [29], China [33], Bangladesh [34], Eastern province capital of Saudi Arabia [38]. However; this result is not supported by study done in Kenya [30], Southwest Ethiopia [31], Vietnam [32] and Ghana [36]. In this study, study participants who had domestic violence were more likely to develop postnatal depression than those who had no domestic violence. The possible reason for this result is that domestic violence has an overwhelming physical, behavioral and psychological effect on the mothers and might leads to depression. Therefore, screening for domestic violence during the prenatal period could help to identify pregnant women at risk of later depression. This finding is similar to the study done in Benchi Maji zone, Ethiopia [29], Kenya [30], Bangladesh [34] and Sudan [37]. But the finding of studies done in Vietnam [32], China [33] and Saudi Arabia [38] don’t support this finding.
Mothers who had a history of substance use were more likely to develop postnatal depression than those who had no history of substance use. This might be due to the fact that substance use during the postnatal period could affect women’s emotions and behaviors, which could be responsible for the development of postpartum depression. This finding is supported by the study done in public hospitals of Addis Ababa [28] and Benchi Maji zone, Ethiopia [29]. However; this finding is not supported by study done in Kenya [30] and Bangladesh [34]. The finding of this study also illustrated that mothers who had poor social support were more likely to develop postnatal depression than those who had strong social support which is consistent with studies done in Benchi Maji zone, Ethiopia [29] and Netaji Subhash medical college, India [35]. However; this finding is not supported by many other studies [31, 32, 34, 37]. Lack of husband or family support during the stressful perinatal period would make the woman feel helpless and susceptible to postnatal depression.
Conclusion
In this study, the magnitude of postnatal depression was found moderate compared to other studies conducted in different parts of the world. Pregnancy type, number of parities, history of previous depression, domestic violence, substance use, and social support were significantly associated with postnatal depression. Perinatal depression screening and intervention need to be integrated with maternal health care services, especially for mothers at risk of postnatal depression. Increasing access to contraceptive options, giving prompt health education to avoid substance use before pregnancy and after child birth, creating and strengthening support groups for emotional support during pregnancy and after childbirth is crucial to prevent postnatal depression.
Acknowledgments
I would like to acknowledge the Nekemte town administrative office and Nekemte town health bureau for their cooperation. I am also grateful to the study participants who voluntarily agreed to be interviewed and participated in the study.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author received no specific funding for this work.
References
- 1.Stewart DE, Robertson E, Dennis C-L, Grace SL, Wallington T. Postpartum depression. Literature review of risk factors and interventions. 2003. http://www.who.int/mental_health/prevention/suicide/lit_review_postpartum_depression.pdf. Accessed 20 Jan 2017. [Google Scholar]
- 2.Guille C, Newman R, Fryml LD, Lifton CK, Epperson CN. Management of postpartum depression. J Midwifery Women’s Health. 2013; 58:643–53 (PUBMED). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller LJ. Postpartum depression. JAMA 2002; 287 (6): 762–765. 10.1001/jama.287.6.762 [DOI] [PubMed] [Google Scholar]
- 4.Mauthner NS. Re-assessing the importance and role of the marital relationship in postnatal depression: Methodological and theoretical implications. Journal of Reprod Infant Psychol. 1998;16(2–3):157–75. [Google Scholar]
- 5.Spinelli MG. Postpartum psychosis: Detection of risk and management. American Journal of Psychiatry 2009; 166(4): 405–408. 10.1176/appi.ajp.2008.08121899 [DOI] [PubMed] [Google Scholar]
- 6.Craske MG. Origins of phobias and anxiety disorders. Elsevier; 2003. p. 13. [Google Scholar]
- 7.Halbreich U, Karkun S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. Journal of affective disorders. 2006; 91(2):97–111. [DOI] [PubMed] [Google Scholar]
- 8.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstetrics & Gynecology. 2005; 106(5, Part 1):1071–83. [DOI] [PubMed] [Google Scholar]
- 9.O’Hara MW, Swain AM. Rates and risk of postpartum depression: A meta-analysis. Int Rev Psychiatry 1996; 8:37–54. [Google Scholar]
- 10.Fisher J, Mello MCd, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries. A systematic review. 2012; 90(2):139– 149H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Toru T, Chemir F, Anand S. Magnitude of postpartum depression and associated factors among women in Mizan Aman town, Bench Maji zone, Southwest Ethiopia. BMC Pregnancy and Childbirth (2018) 18:442 10.1186/s12884-018-2072-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oklahoma State Department of Health. Recognizing Postpartum Depression. Oklahoma City; 2011.
- 13.World Health Organization. (2008). Maternal mental health and child health and development in low- and middle-income countries: report of the meeting, Geneva, Switzerland, 30 January—1 February, 2008. World Health Organization. https://apps.who.int/iris/handle/10665/43975
- 14.Rahman A., Harrington R., and Bunn J., “Can maternal depression increase infant risk of illness and growth impairment in developing countries?” Child: Care, Health and Development, vol. 28, no. 1, pp. 51–56, 2002. View at Publisher · View at Google Scholar · View at Scopus [DOI] [PubMed] [Google Scholar]
- 15.Anoop S, Saravanan B, Joseph A, Cherian A, Jacob K. Maternal depression and low maternal intelligence as risk factors for malnutrition in children: a community-based case-control study from South India. Archives of Disease in Childhood. 2004; 89(4):325–9. 10.1136/adc.2002.009738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hammen C. Social stress and women’s risk for recurrent depression. Archives of Women’s Mental Health. 2003; 6(1):9–13. 10.1007/s00737-002-0160-4 [DOI] [PubMed] [Google Scholar]
- 17.Cooper PJ, Murray L. Postnatal depression. British Medical Journal 1998; 316:1884–6. 10.1136/bmj.316.7148.1884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lester SW, Turnley WH, Bloodgood JM, Bolino MC. Not seeing eye to eye: differences in supervisor and subordinate perceptions of and attributions for psychological contract breach. Journal of Organizational Behavior. 2002;23(1):39–56. [Google Scholar]
- 19.McCoy SJ, Beal JM, Shipman SB, Payton ME and Watson GH. Risk factors for postpartum depression: a retrospective investigation at 4-weeks postnatal and a review of the literature. J Am Osteopath Assoc. 2006; 106 (4): 193–198. [PubMed] [Google Scholar]
- 20.Leathers SJ, Kelley MA. Unintended pregnancy and depressive symptoms among first-time mothers and fathers. American Journal of Orthopsychiatry, 2000; 70 (4): 523 10.1037/h0087671 [DOI] [PubMed] [Google Scholar]
- 21.Vigod S, Villegas L, Dennis C‐ L, Ross L. Prevalence and risk factors for postpartum depression among women with preterm and low‐birth‐weight infants: a systematic review. BJOG 2010; 117:540–550. 10.1111/j.1471-0528.2009.02493.x [DOI] [PubMed] [Google Scholar]
- 22.Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, et al. Antenatal risk factors for postnatal depression: A large prospective study. Journal of Affective Disorders. 2008; 108 (1–2):147–57. 10.1016/j.jad.2007.10.014 [DOI] [PubMed] [Google Scholar]
- 23.Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. General hospital psychiatry. 2004; 26(4):289–95. 10.1016/j.genhosppsych.2004.02.006 [DOI] [PubMed] [Google Scholar]
- 24.Santos IS, Matijasavech A, Taveres BF, Barros AJ, Botelho IP, Lapolli C, et al. Validation of the Edinburgh postnatal depression Scale (EPDS) in a sample of mothers from the 2004 Pelotas birth cohort study. Cadernos de Saúde Pública. 2007; 23:2577–88 10.1590/s0102-311x2007001100005 [DOI] [PubMed] [Google Scholar]
- 25.Crane D, Middleton C, Kenneth A, Bean R. Establishing criterion scores for the Kansas marital satisfaction scale (KMSS) and the revised dyadic adjustment scale (RDAS). Am J Fam Ther. 2000; 28:53–60 [Google Scholar]
- 26.Bøen H, Dalgard OS, Bjertness E. The importance of social support in the associations between psychological distress and somatic health problems and socio-economic factors among older adults living at home: a cross sectional study. BMC Geriatrics. 2012; 12:27 (PUBMED). 10.1186/1471-2318-12-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agarwala A, Rao PA, Narayanan P. Prevalence and predictors of postpartum depression among mothers in the rural areas of Udupi Taluk, Karnataka, India: A cross-sectional study, Clinical Epidemiology and Global Health (2018), 10.1016/j.cegh.2018.08.009 [DOI] [Google Scholar]
- 28.Fantahun A, Cherie A, Deribe L. Prevalence and Factors Associated with Postpartum Depression Among Mothers Attending Public Health Centers of Addis Ababa, Ethiopia. Clinical Practice & Epidemiology in Mental Health. 2018; 14: 196–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Toru T, Chemir F, Anand S. Magnitude of postpartum depression and associated factors among women in Mizan Aman town, Bench Maji zone, Southwest Ethiopia. BMC Pregnancy and Childbirth (2018) 18:442 10.1186/s12884-018-2072-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ongeri L, Wanga V, Otieno P, Mbui J, Juma E, Stoep AV, et al. Demographic, psychosocial and clinical factors associated with postpartum depression in Kenyan women. BMC Psychiatry (2018) 18:318 10.1186/s12888-018-1904-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kerie S, Menberu M, Niguse W. Prevalence and associated factors of postpartum depression in Southwest, Ethiopia, 2017: a cross-sectional study. BMC Res Notes (2018) 11:623 10.1186/s13104-018-3730-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Do Thi Kim Ly, Nguyen Thi Thanh Huong, and Pham Thi Thu Huong. Postpartum Depression and Risk Factors among Vietnamese Women. BioMed Research International. Volume 2018, Article ID 4028913, 5 pages. 10.1155/2018/4028913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chi X, Zhang P, Wu H and Wang J (2016) Screening for Postpartum Depression and Associated Factors Among Women in China: A Cross-Sectional Study. Front. Psychol. 7:1668 10.3389/fpsyg.2016.01668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Azad R, Fahmi R, Shrestha S, Joshi H, Hasan M, Khan ANS, et al. (2019) Prevalence and risk factors of postpartum depression within one year after birth in urban slums of Dhaka, Bangladesh. PLoS ONE 14(5): e0215735 10.1371/journal.pone.0215735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guin G, Rawat S. Prevalence of postpartum depression and association with risk factors in a tertiary care hospital. Int J Reprod Contracept Obstet Gynecol 2018; 7:1094–100. [Google Scholar]
- 36.Anokye R, Acheampong E, Badu-Ainooson A, Obeng EI, Akwasi AG. Prevalence of postpartum depression and interventions utilized for its management. Ann Gen Psychiatry (2018) 17:18 10.1186/s12991-018-0188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khalifa DS, Glavin K, Bjertness E, Lien L. Determinants of postnatal depression in Sudanese women at 3 months postpartum: a cross-sectional study. BMJ Open 2016;6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alasoom LI, Koura MR. Predictors of postpartum depression in the eastern province capital of Saudi Arabia. J Fam Med Primary Care 2014; 3:146–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.