Abstract
Objectives
To explore the changes of morphology and internal airflow in upper airways (UA) after the use of oral appliances (OAs) in patients with obstructive sleep apnea hypopnea syndrome (OSAHS), and investigate the mechanisms by which OAs function as a therapy for OSAHS.
Methods
Eight OSAHS patients (all male, aged 37–58, mean age 46.25) underwent CT scans before and after OA use. Then, computational fluid dynamics(CFD) models were built on the base of the CT scans using Mimics and ANSYS ICEM CFD software. The internal airflow of the upper airways was simulated using ANSYS-FLUENT and the results were analyzed using ANSYS-CFD-Post. The data were analyzed to identify the most important changes of biomechanical properties between patients with and without OA intervention. Upper airway morphology and the internal airflow changes were compared using t-tests and Spearman correlation coefficient analysis.
Results
The narrowest area of upper airways was found to be located in the lower bound of velopharynx, where the volume and pressure were statistically significantly increased (P<0.05) and the air velocity was statistically significantly decreased (P<0.05) in the presence of the OA(P<0.05). After wearing OA, pharyngeal resistance was significantly decreased (P<0.05), from 290.63 to 186.25Pa/L, and the airflow resistance of the pharynx has reduced by 35.9%.
Conclusion
The enlargement of the upper airway after wearing the OA changed its airflow dynamics, which decreased the negative pressure and resistance in narrow areas of the upper airways. Thus, the collapsibility of the upper airways was reduced and patency was sustained.
Introduction
The obstructive sleep apnea-hypopnea syndrome (OSAHS) is a common respiratory sleep disorder that is characterized by repeated partial or complete obstruction of upper airway at the end-expiratory phase during sleep [1]. OSAHS is a highly prevalent disorder which can have serious effects on daily functioning, social life and general health and may even have potentially life-threatening consequences. Prevalence studies estimate that 24% of men and 9% of women in middle age are affected by OSAHS [2]. Furthermore, the prevalence of OSAHS increases with age and in older persons (≥ 65 years) there is a 2- to 3-fold higher prevalence compared with those in middle age (30–64 years) [3]. There is increasing evidence that untreated OSAHS is associated with ischemic heart disease, arterial hypertension stroke [4,5], hypertension [6], daytime sleepiness, and road traffic accidents [7]. Thus, it is now recognized that OSAHS is a serious public health problem.
Treatment modalities for OSAHS includes non-surgical treatments such as weight loss, nasal continuous positive airway pressure (CPAP) and oral appliance (OA) [8–10], as well as surgical treatments such as uvulopalatopharyngoplasty (UPPP), hyoid myotomy and suspension, mandibular osteotomy with genioglossus advancement, adenotonsillectomy and maxillomandibular surgery [11–12]. Since Sullivan et al. first reported the use of CPAP therapy in OSAHS in1981 [9], CPAP has been considered as an effective method for the treatment of OSAHS. However, its clinical effectiveness is limited by poor acceptance and tolerance, as well as suboptimal compliance of patients [13–14]. Disadvantages of UPPP surgery include the pain and expense of the procedure, but also a relatively poor long-term success rate [15]. Since Robin et al. first introduced an intraoral appliance to treat upper airway obstruction in 1934 [10], OAs have increasingly been used in the treatment of OSAHS as a viable alternative to CPAP. While the curative effect of OAs was affirmed by increasing numbers of studies [16], the recent research on the specific mechanism by which OAs affect OSAHS is mainly limited to morphological descriptions [17–19]. It is generally believed that after wearing an OA, the tissue surrounding the upper airways of OSAHS patients is pulled out, and the upper airways are expanded, so that local stenosis is released or entirely abrogated. Hence, the patient can breathe easily and have a higher blood oxygen saturation, a lower snoring sound or even no snoring. However, what happens to the flow dynamics of the upper airways after wearing the OA is still not clear. This study therefore probed the flow dynamics of the upper airways of patients with OSAHS in order to understand the relationship between the morphology of upper airways and their function. Ultimately, the data gathered here improves the understanding of the pathogenesis of OSAHS and the therapeutic mechanism of OA.
Materials and methods
Participants
This study protocol was approved by the Ethics Review Committee at the College of Stomatology, Fourth Military Medical University. It conforms to relevant national and international guidelines. Written informed consent was obtained from each patient. In this study 8 Chinese adult OSAHS patients, aged 37 to 58 years (mean age 46.25 years), were selected. All OSAHS patients had an apnea and hypopnea index (AHI) higher than 5 and lower than 40 per hour on standard polysomnography. Apnea-Hypopnea Index(AHI) is a total number of apneas and hypopneas per hour of sleep. And an AHI>5 events per hour is Obstructive Sleep Apnea(OSA). Those who had active temporo-mandibular disfunction were excluded from the study as well as patients suffering from untreated caries and periodontal disease, completely edentulous patients and those having an insufficient number of remaining teeth.
Three-dimensional reconstruction of upper airways
All patients underwent a PSG detection and a CT scan before and three months after wearing the OAs. CT scans from the lower rim of the epiglottis to the supraorbital margin were performed with a spatial resolution of 512×512 pixels and zero space, 1.25mm thickness, to obtain DICOM (Digital Imaging and Communication in Medicine) format images. Scanning was performed with the patients awake, in supine and neutral position during one breath hold at the end of a normal inspiration. All patients were scanned by the same radiology technicians in the Department of Radiology, Fourth Military Medical University, Xi’an, China. The CT scans were used to construct three-dimensional models for the analysis of fluid dynamics.
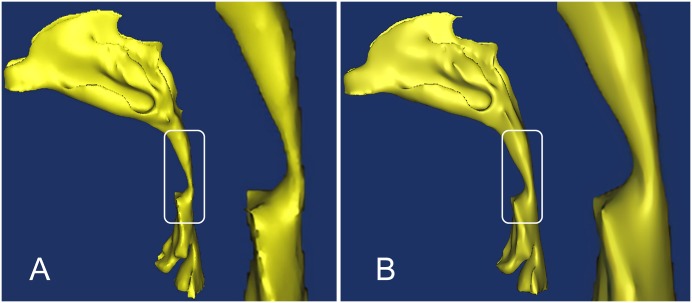
The DICOM image data of the patients was then loaded into Mimics 10.0 (Materialise NV, Leuven, Belgium). Subsequently, a segmentation of the upper airways was done based on the Hounsfield unit (HU), a measure of the electron density of the tissue, assigned to each pixel in the series of DICOM images. The HU had values from 1024 to 3071. For the upper airways, a range of HU between -1024 to -400 is regarded as very good results [20]. The segmented region was successfully converted to a 3D model, smoothed in Magics9.9 (Materialise, Leuven, Belgium), and finally exported for further analysis (Fig 1).
Fig 1. Three-dimensional reconstruction of a patient’s upper airways.
(A) Three-dimensional reconstruction of a patient’s upper airways without an oral appliance, with a focus on the pharynx region. (B) The same patient’s upper airways with an oral appliance, with a focus on the pharynx region.
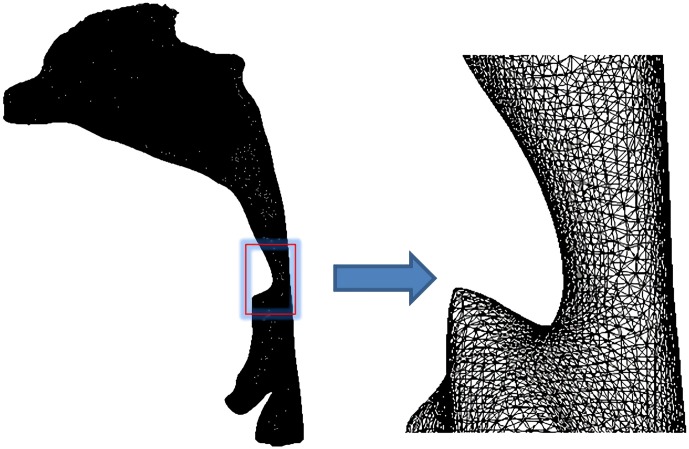
Three-dimensional mesh model building
To prepare the segmented upper airway model for CFD calculations, a computational grid was created using ICEM-CFD 14.0 (ANSYS, Canonsburg, PA, USA), in which both global and local mesh controls were used to improve mesh quality (Fig 2), followed by a mesh-independent test. The upper respiratory tract model was, respectively, by a grid of 600,000, 1.21 million, 1.65 million, 2 million, and 2.3 million, and the gas flow field data in the upper respiratory tract under each grid size was obtained. Then the pressure difference of the pharynx under different mesh sizes and the change of the pressure distribution of the nasal vestibular end section were compared. As a result, when the number of grids reached above 1.65 million, the calculation results no longer change as the number of grids increases. Therefore, in this experiment, a tetrahedral unstructured mesh with a grid number of more than 1.65 million and less than 2 million is selected. This mesh density can capture the subtle parameter changes of the gas flow in the upper respiratory tract.
Fig 2. Three-dimensional mesh model of the upper airways.
A tetrahedral unstructured mesh with a grid number of more than 1.65 million and less than 2 million was created for CFD calculations. This mesh density can capture the subtle parameter changes of the gas flow in the upper respiratory tract.
Numerical simulation of the upper airways
The ANSYS 14.0-Fluid Dynamics-FLUENT 14.0 commercial code was used to solve the Reynolds averaged Navier–Stokes equations for the steady airflow simulation. The flow was assumed to be steady, homogeneous, incompressible, adiabatic and Newtonian. The density of air was set at 1.225 kg m–3, and the viscosity was assumed to be 1.789 x10−5 kg m–1 s–1. We applied the Reynolds averaged Navier-Stokes equation (RNG k-epsilon turbulence model) to simulate the airflow status. A second-order pressure discretization scheme was used for the pressure calculations, and a second-order upwind scheme was used for the momentum and turbulence transport equations. We used the SIMPLE algorithm to solve the pressure–velocity coupling. Atmospheric pressure was imposed at both nostrils, and a constant flow rate of 200 ml/s was applied at the planes in the pharynx. The upper airway wall was assumed to be no-slip (u = v = 0). The wall function uses a standard wall function; the lower edge of the throat is defined as the flow boundary condition. To obtain a better initialization field and convergence acceleration, multigrid initialization was used to optimize the flow field.
The results obtained using Fluent were post-processed using CFD-Post (ANSYS, Canonsburg, PA, USA) to obtain the contours and vectors, and the function calculator was used to acquire values for the pressure gradient, pressure and velocity in cross-sectional planes at specified points in the upper airways.
Cross-sections selection of the CFD model
The magnitude of airflow velocity in the upper airways was calculated at the five different cross-sections shown in Fig 3. Section 1 constitutes the beginning of the nasopharynx, section 2 is located at the lower bound of the nasopharynx (upper bound of the palatopharynx), and section 3 at the lower bound of the palatopharynx (upper bound of the glossopharynx). Sections 4 and 5 are located the top and the base of the epiglottis, respectively.
Fig 3. Selected sections of the CFD model.
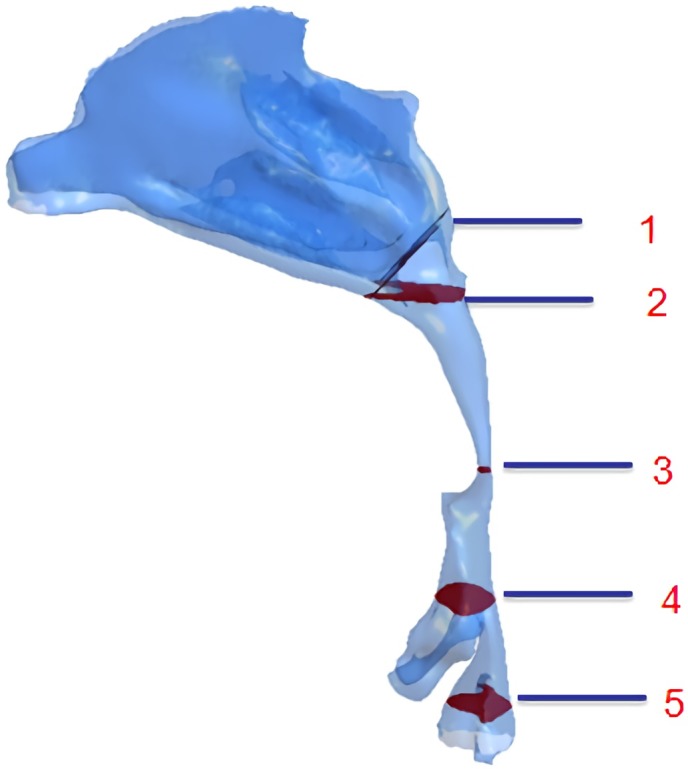
(1) the beginning of the nasopharynx; (2) the upper bound of the palatopharynx; (3) the upper bound of the glossopharynx; (4) the top of the epiglottis; (5) the base of the epiglottis.
Statistical analyses
Statistical analysis was performed using SPSS 17.0 (IBM Corp., Armonk, NY, USA). The paired t-test was adopted to compare the changes of the cross-sectional area, volume, velocity, pressure and resistance before and three months after wearing the OAs. The association between AHI change, volume change and resistance change were analyzed using the coefficient of product moment correlation (Pearson’s correlation coefficient). For all analyses, a probability value of P <0.05 was considered to indicate differences that are statistically significant.
Results
Morphological changes in the upper airways after use of the OAs
As shown in Tables 1 and 2, the volume of the nasopharynx region of patients with and without OAs use showed no significant difference (P>0.05), while that of the palatopharynx, glossopharynx and hypopharynx increased significantly(P<0.05). Prominent changes occurred mainly in the palatopharynx (increased by 39.54%) and glossopharynx (increased by 44.48%). The narrowest region of the upper airway was located at section 3 (the lower bound of the palatopharynx). Notably, its cross-sectional area increased significantly by 129.06% with the OAs(P<0.05).
Table 1. Volumetric changes in the airways with and without the OAs (cm3).
| region | Without OAs | With OAs | p-value | Deformation rate |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| nasopharynx | 2.3333±0.7377 | 2.3523±0.8019 | 0.542 | 0.81 |
| palatopharynx | 2.4482±0.8352 | 3.4161±0.5426 | < 0.001** | 39.54 |
| glossopharynx | 2.2759±0.3638 | 3.2882±0.6140 | 0.001** | 44.48 |
| hypopharynx | 3.6281±0.8202 | 4.0505±0.6589 | 0.047* | 11.64 |
| total volume | 10.6854±2.2740 | 13.1071±2.180 | < 0.001** | 22.67 |
* P<0.05;
** P<0.01
Table 2. Changes in the cross-sectional area of selected upper airway sections from patients with and without OAs (cm2).
| Section | Without OAs | With OAs | p-value | Deformation rate |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| A | 3.1441±0.7028 | 3.1643±0.6017 | 0.283 | 0.64 |
| B | 2.1608±0.9456 | 2.3389±0.5536 | 0.058 | 8.24 |
| C | 0.2150±0.1032 | 0.4925±0.1018 | 0.001** | 129.06 |
| D | 1.6430±0.6109 | 2.5817±0.5691 | 0.018* | 57.13 |
| E | 2.3573±0.4370 | 2.6032±0.4092 | 0.035* | 10.43 |
* P<0.05;
** P<0.01
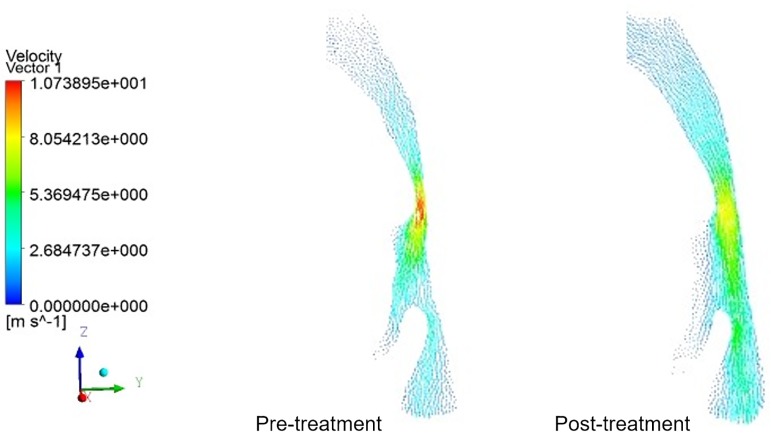
Airflow velocity changes in the upper airways
The change tendencies of airflow velocity in the UAs of 8 patients were similar to those illustrated in Fig 4. Without the OA, the airflow velocity was turbulent, while it became smooth and steady after using OAs. The maximum airflow velocity in the narrowest part of the pharynx, i.e. the palatopharyngeal region, was determined both pre- and post-treatment. As can be seen in Table 3, there was no difference in the airflow velocity in the nasopharynx and epiglottis pre- and post-treatment (P>0.05), while that of palatopharynx and glossopharynx decreased significantly(p<0.05), from 11.55 m/s to 8.81 m/s post-treatment, representing a decline of 23.7%. The difference was especially significant in the lower bound of palatopharynx (p<0.01).
Fig 4. Velocity vectors in the mid–sagittal plane of a patient’s upper airways.
Before treatment, the airflow velocity was turbulent, while it became smooth and steady after using OAs. The maximum airflow velocity in the lower boundary of the palatopharyngeal, the narrowest part of the pharynx, was determined both pre- and post-treatment.
Table 3. Airflow velocity changes in different selected sections of the upper airways form patients with and without the OAs (m/s).
| section | Without OAs | With OAs | p-value | Deformation rate |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| A | 0.84±0.31 | 0.78±0.24 | 0.183 | -7.14 |
| B | 1.24±0.43 | 1.03±0.55 | 0.048* | -16.94 |
| C | 11.55± 2.18 | 8.81±2.47 | 0.007** | -23.72 |
| D | 4.86±1.17 | 4.34±1.53 | 0.036* | -10.70 |
| E | 2.75±0.74 | 2.60±0.40 | 0.095 | -5.45 |
* P<0.05;
** P<0.01
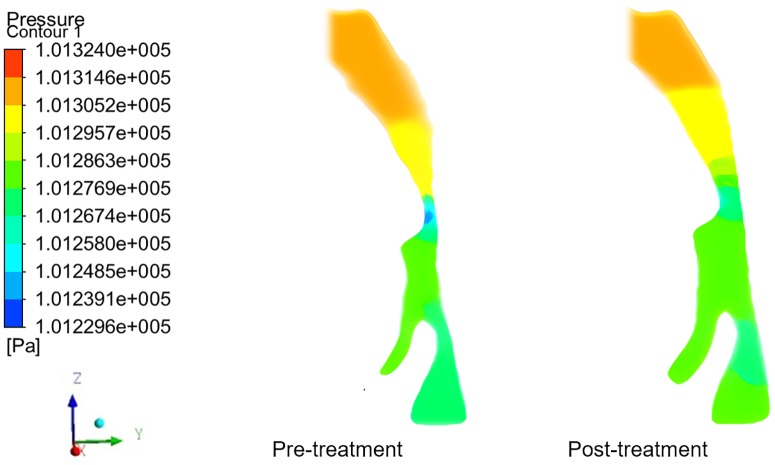
Pressure changes in the upper airways of patients before and after using OAs
The pressure change trends in the UA of 8 subjects were similar to what was outlined in Fig 5. The pressure distribution in the UA became steady with OA. Both the initial and final minimum pressure was detected at the lower boundary of the palatopharynx, a narrow region in the UA. Moreover, the maximum flow rate was observed at this point, conforming with Bernoulli’s equation. As shown in Table 4, after wearing the OAs, no statistically significant difference of pressure was observed in the nasopharynx and epiglottis (P<0.05), while pressure in the palatopharynx and glossopharynx increased remarkably(P<0.05), especially at the lower boundary of the palatopharynx(P<0.01), rising from 101240.25 to 101264.13Pa. The pressure in the inlet of the nasal cavity was defined as the baseline (the practical atmospheric pressure is 101325Pa), the pressure at the lower boundary of the palatopharynx without AOs was calculated as -84.75Pa, and it transformed into -60.87Pa with the AOs, thus denoting a pressure drop of 28.2% in the narrowest part of the UAs.
Fig 5. Pressure contours in the mid–sagittal plane of a patient’s upper airways.
The pressure distribution in the upper airway became steady after treatment. Both the initial and final minimum pressure was detected at the narrow region in the upper airway, i.e. the lower boundary of the palatopharynx.
Table 4. Pressure changes in different sections of the upper airways from patients with and without OAs(Pa).
| Section | Without OAs | With OAs | p-value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| A | 101303.61±18.37 | 101305.24±16.79 | 0.093 |
| B | 101308.52±8.46 | 101313.48±6.37 | 0.065 |
| C | 101240.25±16.24 | 101264.13±23.10 | 0.005** |
| D | 101263.49±12.12 | 101272.34±13.47 | 0.039* |
| E | 101255.58±20.66 | 101261.73±18.36 | 0.063 |
* P<0.05;
** P<0.01
Changes of resistance in the upper airways
For patients with OSAHS, the pressure difference in upper airway is usually large, and the changes are mainly concentrated in the constricted part. A sharp increase or decrease in pressure in a small range would lead to an increase resistance in airway, aggravating the degree of constriction and obstruction. In clinical, airflow resistance is used to reflect the degree of airway ventilation. Airflow resistance denotes the specific pressure needed to push a defined volume of gas over a designated distance in a defined time. It can be described using the formula: R = ΔP/Q, where R indicates airflow resistance, ΔP indicates the pressure difference of the airway, Q indicate the gas flow, which had a set value of 200ml/s. As shown in Table 5, with the effect of the OAs, the resistance in the upper airways decreased significantly(p<0.05), from 290.99Pa·s/L to 186.25Pa·s/L, a decline of 36.0%.
Table 5. Changes of resistance in the pharynx of patients with and without OAs.
| Patient | Without OAs | With OAs | ||
|---|---|---|---|---|
| ΔP(Pa) | R (Pa·s/L) | ΔP(Pa) | R (Pa·s/L) | |
| 1 | 50.35 | 251.75 | 28.82 | 144.10 |
| 2 | 41.64 | 208.20 | 35.29 | 176.45 |
| 3 | 85.16 | 425.80 | 31.56 | 157.80 |
| 4 | 58.24 | 291.20 | 55.80 | 279.00 |
| 5 | 81.91 | 409.55 | 53.34 | 266.70 |
| 6 | 36.42 | 182.10 | 32.61 | 163.05 |
| 7 | 42.76 | 213.80 | 31.49 | 157.45 |
| 8 | 69.11 | 345.55 | 29.09 | 145.45 |
| Mean ± SD | - | 290.99±87.62 | - | 186.25±50.98 |
Note: t = 3.182 p = 0.015
Correlations among AHI, pharyngeal volume and resistance changes in the pharynx with and without OAs
The detailed data on AHI, pharyngeal volume and pharyngeal resistance changes which was collected before and after the 8 patients used OAs is shown in Table 6. Fig 6 shows that there was a negative correlation between pharyngeal resistance changes and pharyngeal volume changes (r = -0.786 p = 0.0218, Fig 6A) as well as pharyngeal volume changes and AHI changes (r = -0.81 p = 0.0158, Fig 6B), while there was a positive correlation between pharyngeal resistance changes and AHI changes (r = 0.976 p = 0.0008, Fig 6C).
Table 6. The changes of AHI, pharyngeal volume and pharyngeal resistance in OSAHS Patients with and without OAs.
| patient | Without OAs | With OAs | Deformation rate of pharyngeal volume with OAs (%) | Deformation rate of pharyngeal resistance with OAs (%) |
|---|---|---|---|---|
| AHI | AHI | |||
| 1 | 21.3 | 2.2 | 35.45 | -42.00 |
| 2 | 23.2 | 5.1 | 28.08 | -16.67 |
| 3 | 27.6 | 1.8 | 29.82 | -62.35 |
| 4 | 16.1 | 16.0 | 13.73 | -3.45 |
| 5 | 21.8 | 3.4 | 17.32 | -35.37 |
| 6 | 14.3 | 12.1 | 10.31 | -8.33 |
| 7 | 17.5 | 1.9 | 20.45 | -27.9 |
| 8 | 24.2 | 1.4 | 34.46 | -57.97 |
Fig 6. The correlation analysis among AHI, pharyngeal volume and pharyngeal resistance changes.
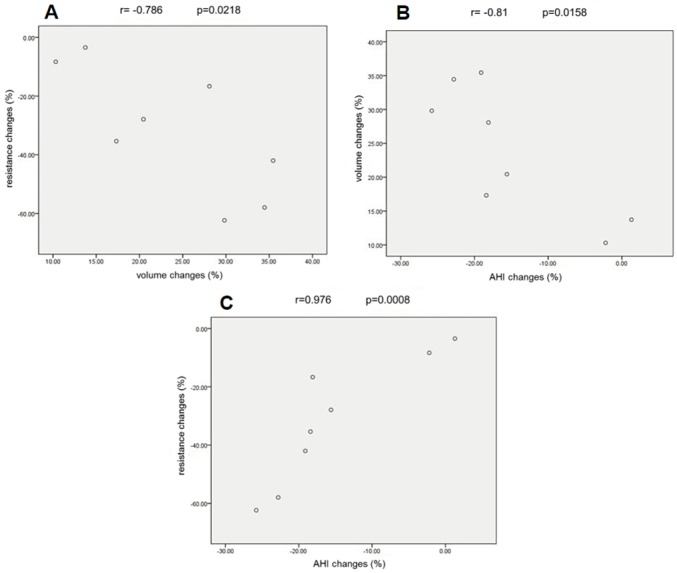
(A) There was a negative correlation between pharyngeal resistance changes and pharyngeal volume changes (r = -0.786 p = 0.0218). (B) There was a negative correlation between pharyngeal volume changes and AHI changes (r = -0.81 p = 0.0158). (C) There was a positive correlation between pharyngeal resistance changes and AHI changes (r = 0.976 p = 0.0008).
Discussion
Discussion of the computational fluid dynamics
This study was to stimulate the morphology and internal flow of the upper airway for patients with OSAHS under quiet breathing through CFD, and the computational domain was from anterior nares to the root of epiglottis. The walls of the upper airway were assumed to be rigid, and airflow as steady, ignoring the influence of nose hairs, temperature field and humidity. According to the previous research, the simplifications are reasonable [21]. Airflow inside a human nasal cavity is in a dynamic state; i.e. it decelerates and accelerates from a resting state during normal breathing. Experimental studies indicate that the flow is laminar when the half nasal flow rate is less than 200m/s. We further simplified the analysis by treating the flow as quasi-steady, rather than fully unsteady. The importance of the unsteadiness of developing flows in finite length tubes can be estimated by the magnitude of the Strouhal number (S = wL/U) based on the axial length, L, from the entrance. For quiet restful breathing frequency of 0.25 Hz (15breaths per minute) and half-nasal flow rate of less-than-200ml/s, the Strouhal number is less than 0.2, indicating that the quasi-steady approximation is reasonable [22]. Considering the existence of the low Strouhal number (<0.2) in quiet restful breathing, we can assume that as long as the airway does not deform, the error of ignoring the pulsating flow and treating the airflow as steady is very small. Previous studies have also concluded that nasal flow can be considered as steady in most cases [23].
Airflow in the human upper airways is mostly the transitional flow regime; thus, it is likely that portions of flow could be locally laminar, and other portions could be locally turbulent. Particularly, as flow accelerates through upper nasopharynx and into oropharynx, pressure drops rapidlly. Downstream of velopharynx, the area expansion causes deceleration, unfavorable pressure gradient, separation, and a turbulent jet characterized by high velocity and turbulence intensity. Therefore, it is questioned whether employing only laminar or turbulent computations can yield useful results for physiologic situation. It is known that the Reynolds number, Re, in the trachea varies from 800 in light breathing (200 ml/s) to about 9300 in heavy breathing (100 l/min). Flows in the human airway have many characteristics (e.g. curved streamlines, stenosis and a recirculation region) that are known to necessitate the use of traditional two-equation turbulence models, such as the k–ε model. The standard k–ε model is a high Reynolds number model that has been used for investigating flow characteristics in the airway, but with poor performance for considering the airflow as turbulences [24–25]. The renormalization group(RNG) k-ε turbulence model has many similarities with the standard k-ε turbulence model, but when the RNG k-ε turbulence model calculates the turbulent dissipation rate (ε), it has particular conditions [26]. The RNG k-ε turbulence model is a low Reynolds number model, and it reproduces the important transition from laminar to turbulent flow in the pharyngeal airway. The performance of a low Reynolds number turbulence model in predicting transitional turbulence flows, which are the pre-dominant flow characteristics in the pharyngeal airway. Therefore, in this study the RNG k-ε model is adopted.
Airflow dynamics of the upper airways and OA
The nasopharyngeal airways almost remained unchanged after using OAs, while the cross-section of the glossopharyngeal and palatopharyngeal airways significantly increased, and that of the hypopharyngeal airway increased slightly. These results demonstrate that OAs mainly act on the glossopharyngeal and palatopharyngeal airways. In the narrow region behind the soft palate, the CSA increased obviously by 129.06% (P<0.05). Airway enlargement decreased the possibility of a collapse and obstruction of the UAs during the respiratory process, thus providing better flow conditions. This was confirmed by the analysis of velocity and pressure.
After wearing the appliance, the respiratory flow rate becomes more balanced, especially in the palatopharynx and glossopharynx, where it decreased from 11.55 m/s to 8.81 m/s, resulting in a reduced impact of the airflow on the pharyngeal cavity wall and thus preventing damage to the airway mucosa. The reduced impact will correspondingly reduce the patient’s snoring which arises from high frequency vibrations of soft tissue under the conditions of violent airflow impact on the pharyngeal cavity wall. In the presence of the OA, negative pressure in the narrow area of the palatopharynx decreased significantly from -84.75Pa to -60.87Pa. Within the entire upper respiratory tract, only the palatopharyngeal region consists of soft tissue without bone support, and thus can collapse under the effect of negative pressure. Reducing the negative pressure diminishes airway compliance, and therefore reduces the collapsibility of airways and improves the patients’ symptoms.
Air resistance in the upper respiratory tract is an important index for the evaluation of the ventilation degree, and the resistance value determines the difficulty of inspiration. High resistance indicates that it is difficult for gas to flow in the upper airways, while the converse indicates that it is easy. Resistance in the pharynx decreased significantly by 36.0% (P<0.05), which eased the air circulation in the UAs, further reducing the probability of airway collapse.
By enlarging the upper airways, the OA altered the dynamic characteristics of airflow in the upper respiratory tract, and bringing the morphology into correspondence with function is the fundamental element for the success of OSAHS therapy. Therefore, when devising an OA, one should consider how to achieve changes in airflow pressure and resistance, not merely changes of morphology.
AHI, total volume and resistance of the pharynx
Polysomnography is the golden standard for the diagnosis of OSAHS, and the main measurement index is AHI, which is a total number of apneas and hypopneas per hour of sleep. If AHI value is less than 5, then the patient is within normal limits. Obstructive Sleep Apnea is mild when the AHI reflects 5 to 15 episodes per hour of sleep, moderate when the AHI reflects 15 to 29 episodes per hour of sleep, and severe when the AHI reflects 30 and higher episodes per hour of sleep. AHI, introduced in the 1980s, is widely applied as an important indicator in the diagnosis, classification and efficiency evaluation of OSAHS, both in clinical and academic settings. However, investigators found some deficiencies in using AHI to assess efficiency. A study indicates that, after the use of OA, different patients obtained the same AHI, but they suffered from different degrees of hypoxemia [27]. Similar studies have also shown that although patients obtain the same AHI after the use of OA, the probability of cardiovascular disease events was actually different [28]. Hence, we aimed to identify auxiliary indicators to inspect OA efficacy. We conducted a correlation analysis among the AHI, total volume and resistance of the pharynx before and after the use of OA. There was a negative relationship between pharyngeal volume changes and AHI changes in patients with OA, as well as a positive relationship between pharyngeal resistance changes and AHI changes. Therefore, we extrapolated that the changes of pharyngeal volume and resistance may be auxiliary indicators to test the effect of OAs on OSAHS. Nevertheless, a multitude of clinical data still needs to be gathered and a thorough correlation analysis between these indicators and clinical outcomes needs to be conducted to verify this deduction.
Limitations of the study
Nevertheless, some deficiencies of this study should also be considered. Firstly, the CT data was obtained with patients in the waking state, while respiratory collapse in OSAHS patients mainly occurs during sleep. Secondly, the study ignores the influence of soft tissues, such as muscle tension, which is vital for the stability of the respiratory tract during sleep, as well as changes and movement of the soft palate, tongue root and other soft tissues related to the respiratory tract may be important factors related to the pathophysiology of OSAHS. While in this study we failed to take the effect of soft tissue into consideration, the most likely site of collapse in the respiratory tract depends on respiratory compliance, a certain degree of muscularization, the so-called “tissue stress” and internal respiratory pressure. Therefore, high-resolution CT data and fluid-structure interaction (FSI) numerical simulation technology can be used to further support the present results. However, FSI technology is still in the early research phase and has been applied only to two-dimensional models [29]. To be applied in practical research on the oropharyngeal tract, FSI technology needs to overcome a major problem of data availability for particular material properties of tissues such as tongue and soft palate. In addition, the elastic modulus and Poisson’s ratio of tissues measured in vitro may not have a close correlation with tissue deformability in vivo. Therefore, recording CT images of patients in the sleeping state and attaining reliable soft tissue material properties for use in conjunction with Fluid-structure interaction technology(FSI) could enable the analysis of the impact coefficient of soft tissue surrounding the airways and air in the respiratory tract. The effects of these properties on respiratory stability will be the focus of our future research.
In spite of these limitations, our results show that analyzing the dynamic airflow changes in the upper airways in the presence of OAs by applying CFD technology helps us to recognize the mechanism by which OAs exert their effect in OSAHS treatment and the interactive relationship between structure and function of the upper airways, providing theoretical basis for clinical application of OA in OSAHS treatment.
Conclusions
In OSAHS that received OA treatment, changes in the morphology and flow dynamics of the upper airways were mainly observed in the palatopharyngeal and glossopharyngeal region. When wearing the OA, the upper airway was enlarged, dynamic airflow characters were changed, and negative pressure as well as resistance in the narrow area of the UAs was diminished, thus making the upper airways more resilient to collapse as well as maintaining their patency.
Supporting information
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002;360(9328):237–245. 10.1016/S0140-6736(02)09464-3 [DOI] [PubMed] [Google Scholar]
- 2.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The Occurrence of Sleep-Disordered Breathing Among Middle-Aged Adults. New England Journal of Medicine. 1993;328(17):1230–1235. 10.1056/NEJM199304293281704 [DOI] [PubMed] [Google Scholar]
- 3.Bixler EO, Vgontzas AN, Ten-Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. American Journal of Respiratory & Critical Care Medicine. 1998;157(1):144–148. [DOI] [PubMed] [Google Scholar]
- 4.Barbé F, Durán-Cantolla J, Sánchez-de-la-Torre M, Martínez-Alonso M, Carmona C, Barceló A, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. Journal of the American Medical Association. 2012;307(20):2161–2168. 10.1001/jama.2012.4366 [DOI] [PubMed] [Google Scholar]
- 5.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005. March;365(9464):1046–1053. 10.1016/S0140-6736(05)71141-7 [DOI] [PubMed] [Google Scholar]
- 6.Peppard PE, Young T, Palta M, Skatrud J. Prospective Study of the Association between Sleep-Disordered Breathing and Hypertension. New England Journal of Medicine. 2000;342(19):1378–1384. 10.1056/NEJM200005113421901 [DOI] [PubMed] [Google Scholar]
- 7.Naegele B, Pepin JL, Levy P, Bonnet C, Pellat J, Feuerstein C. Cognitive executive dysfunction in patients with obstructive sleep apnea syndrome (OSAS) after CPAP treatment. Sleep. 1998;21(4):392–397. 10.1093/sleep/21.4.392 [DOI] [PubMed] [Google Scholar]
- 8.Awad KM, Malhotra A, Barnet JH, Quan SF, Peppard PE. Exercise Is Associated with a Reduced Incidence of Sleep-disordered Breathing. The American Journal of Medicine. 2012;125(5):485–490. 10.1016/j.amjmed.2011.11.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;317(8225):862–865. [DOI] [PubMed] [Google Scholar]
- 10.Cartwright RD, Samelson CF. The effects of a nonsurgical treatment for obstructive sleep apnea. The tongue-retaining device. The Journal of the American Medical Association. 1982;248(6):705–709. [PubMed] [Google Scholar]
- 11.Fujita S, Conway W, Zorick F, Roth T. Surgical Correction of anatomical azbnormalities in obstructive sleep apnea syndrome: Uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 1981;89(6):923–934. 10.1177/019459988108900609 [DOI] [PubMed] [Google Scholar]
- 12.Riley RW, Powell NB, Guilleminault C. Inferior sagittal osteotomy of the mandible with hyoid myotomy-suspension: a new procedure for obstructive sleep apnea. Otolaryngol Head Neck Surg. 1986;94(5):589–593. 10.1177/019459988609400510 [DOI] [PubMed] [Google Scholar]
- 13.Engleman HM, Asgari-Jirhandeh N, Mcleod AL, Ramsay CF, Deary IJ, Douglas NJ. Self-Reported Use of CPAP and Benefits of CPAP Therapy: A Patient Survey. Chest. 1996;109(6):1470–1476. 10.1378/chest.109.6.1470 [DOI] [PubMed] [Google Scholar]
- 14.Weaver TE, Kribbs NB, Pack AI, Kline LR, Chugh DK, Maislin G, et al. Night-to-night variability in CPAP use over first three months of treatment. Sleep. 1997;20(4):278–283. 10.1093/sleep/20.4.278 [DOI] [PubMed] [Google Scholar]
- 15.Larsson H, Carlsson-Nordlander B, Svanborg E. Long-time Follow-up after UPPP for Obstructive Sleep Apnea Syndrome: Results of Sleep Apnea Recordings and Subjective Evaluation 6 Months and 2 Years after Surgery. Acta Oto-Laryngologica. 1991;111(3):582–590. 10.3109/00016489109138387 [DOI] [PubMed] [Google Scholar]
- 16.Wilhelmsson B, Tegelberg A, Walker-Engström ML, Ringqvist M, Andersson L, Krekmanov L, et al. A Prospective Randomized Study of a Dental Appliance Compared with Uvulopalatopharyngoplasty in the Treatment of Obstructive Sleep Apnoea. Acta Oto-laryngologica. 1999;119(4):503–509. 10.1080/00016489950181071 [DOI] [PubMed] [Google Scholar]
- 17.Haskell JA, McCrillis J, Haskell BS, Scheetz JP, Scarfe WC, Farman AG. Effects of Mandibular Advancement Device (MAD) on Airway Dimensions Assessed with Cone-Beam Computed Tomography. Seminars in Orthodontics. 2009;15(2):132–158. [Google Scholar]
- 18.Kyung SH, Park YC, Pae EK. Obstructive sleep apnea patients with the oral appliance experience pharyngeal size and shape changes in three dimensions. Angle Orthod. 2005;75(1):15–22. [DOI] [PubMed] [Google Scholar]
- 19.Sam K, Lam B, Ooi CG, Cooke M, Ip MS. Effect of a non-adjustable oral appliance on upper airway morphology in obstructive sleep apnoea. Respir Med. 2006;100(5):897–902. 10.1016/j.rmed.2005.08.019 [DOI] [PubMed] [Google Scholar]
- 20.Ferretti GR, Bricault I, Coulomb M. Virtual tools for imaging of the thorax. European Respiratory Journal. 2001. August;18(2):381–392. 10.1183/09031936.01.00217701 [DOI] [PubMed] [Google Scholar]
- 21.Hahn I, Scherer PW, Mozell MM. Velocity profiles measured for airflow through a large-scale model of the human nasal cavity. J Appl Physiol (1985). 1993;75(5):2273–2287. [DOI] [PubMed] [Google Scholar]
- 22.Keyhani K, Scherer PW, Mozell MM. Numerical simulation of airflow in the human nasal cavity. J Biomech Eng. 1995;117(4):429–441. 10.1115/1.2794204 [DOI] [PubMed] [Google Scholar]
- 23.Yang C, Woodson BT. Upper airway physiology and obstructive sleep-disordered breathing. Otolaryngol Clin North Am. 2003;36(3):409–421. [DOI] [PubMed] [Google Scholar]
- 24.Katz IM, Davis BM, Martonen TB. A numerical study of particle motion within the human larynx and trachea—Physical and Biological Basis for Therapy. Journal of Aerosol Science. 1999;30(2):173–183. [Google Scholar]
- 25.Luo XY, Hinton JS, Liew TT, Tan KK. LES modelling of flow in a simple airway model. Med Eng Phys. 2004;26(5):403–413. 10.1016/j.medengphy.2004.02.008 [DOI] [PubMed] [Google Scholar]
- 26.Jeong SJ, Kim WS, Sung SJ. Numerical investigation on the flow characteristics and aerodynamic force of the upper airway of patient with obstructive sleep apnea using computational fluid dynamics. Med Eng Phys. 2007;29(6):637–651. 10.1016/j.medengphy.2006.08.017 [DOI] [PubMed] [Google Scholar]
- 27.Series F, Marc I, Cormier Y, La Forge J. Utility of Nocturnal Home Oximetry for Case Finding in Patients with Suspected Sleep Apnea Hypopnea Syndrome. Ann Intern Med. 1993;119(6):449–453. 10.7326/0003-4819-119-6-199309150-00001 [DOI] [PubMed] [Google Scholar]
- 28.Berman EJ, Dibenedetto RJ, Causey DE, Mims T, Conneff M, Goodman LS,et al. Right Ventricular Hypertrophy Detected by Echocardiography in Patients with Newly Diagnosed Obstructive Sleep Apnea. Chest. 1991;100(2):347–350. 10.1378/chest.100.2.347 [DOI] [PubMed] [Google Scholar]
- 29.Malhotra A, Huang Y, Fogel RB, Pillar G, Edwards JK, Kikinis R, et al. The male predisposition to pharyngeal collapse: importance of airway length. Am J Respir Crit Care Med. 2002;166(10):1388–1395. 10.1164/rccm.2112072 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.