To the Editor—We read with great interest the recent article by Klein and colleagues [1] regarding the impact of methicillin-resistant Staphylococcus aureus (MRSA) infections compared with methicillin-susceptible Staphylococcus aureus (MSSA) infections on hospitalization costs and mortality. As the authors correctly noted, the epidemiology of MRSA and MSSA, as well as prescribing patterns of physicians, have changed greatly in the last decade, necessitating studies on this important subject using more recent data.
However, the interpretation of a propensity score analysis requires careful attention to the details of the covariates used to derive the propensity score, a point made in a recent letter to Clinical Infectious Diseases [2]. Although the inclusion of baseline subject characteristics such as age, race, hospital region, and Charlson comorbidity index was appropriate in the study by Klein et al, the inclusion of characteristics that occur downstream from the acquisition of MRSA or MSSA infection may lead to difficulty in interpreting the results. Specifically, because length of stay and number of procedures performed were used as covariates to derive the propensity score with the outcome of cost of hospitalization, the results should be assessed with caution. Length of stay, in addition to possibly being associated with medical comorbidities [3], may serve as a primary mechanism by which a MRSA infection would lead to healthcare costs that are higher than costs of a MSSA infection [4], although the impact on costs of prolonging length of stay remains controversial [5]. Adjusting for these intermediate variables, known as mediators [6], in studies that use propensity scores complicates the interpretation of results.
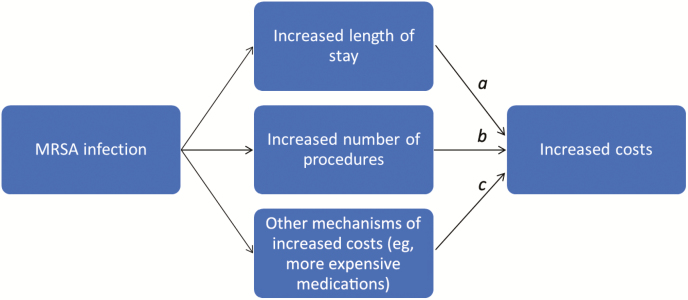
Causal diagrams are frequently used in epidemiology to clarify complex relationships between covariates and to identify variables to include in or exclude from adjusted analyses [7]. We depict proposed relationships between MRSA infections, length of stay, increased number of procedures, other mechanisms of increased costs, and the costs themselves in Figure 1.
Figure 1.
Causal diagram showing proposed relationships between MRSA infections, length of stay, increased number of procedures, other mechanisms of increased costs, and the costs of hospitalization. Abbreviation: MRSA, methicillin-resistant Staphylococcus aureus.
Adjustment for increased length of stay and increased number of procedures leads to an analysis in which the estimate of the effect of MRSA infection on costs only includes c, the effect of mechanisms that lead to increased costs that do not relate to increased length of stay or increased number of procedures.
To illustrate the concept with a different hypothetical example, suppose that the use of vancomycin for MRSA infections leads to increased vancomycin-induced nephrotoxicity and subsequent increased length of stay due to the need to manage acute kidney injury. In a study of vancomycin compared with another antimicrobial for the treatment of MRSA infections in inpatients, suppose that a researcher used a propensity score analysis. The inclusion of length of hospital stay in the propensity score would adjust away the effect on the cost of vancomycin, resulting in increased length of hospital stay.
In the study by Klein et al, adjustment for potential mediators in the propensity score analysis leads to an analysis the outcome of which is the extent to which MRSA infection, compared with MSSA infection, leads to increased or decreased healthcare costs not associated with length of stay, need for procedures, or severity of illness. However, we do not believe that this was the authors’ intent.
The presence of confounders of these intermediate variables (such as baseline comorbidities and their effect on both MRSA risk as well as length of stay) further complicates the analysis; a recent review discusses analytic methods for the problem of confounded intermediates [8].
We would be curious to see the results of an analysis that excludes from the propensity score derivation potential mediators of cost such as increased length of stay and increased number of procedures.
Notes
Financial support. M. Z. D. acknowledges support from the National Institutes of Health (grant 1R01AI139188).
Potential conflicts of interest. M. Z. D. reports grants from GlaxoSmithKline and personal fees from Baxter, outside the submitted work. Both authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Klein EY, Jiang W, Mojica N, et al. . National costs associated with methicillin-susceptible and methicillin-resistant Staphylococcus aureus hospitalizations in the United States, 2010–2014. Clin Infect Dis 2019; 68:22–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Roth JA, Juchler F, Widmer AF, Battegay M. Plea for standardized reporting and justification of propensity score methods. Clin Infect Dis 2019; 68:710–1. [DOI] [PubMed] [Google Scholar]
- 3. Matsui K, Goldman L, Johnson PA, Kuntz KM, Cook EF, Lee TH. Comorbidity as a correlate of length of stay for hospitalized patients with acute chest pain. J Gen Intern Med 1996; 11:262–8. [DOI] [PubMed] [Google Scholar]
- 4. Fine MJ, Pratt HM, Obrosky DS, et al. . Relation between length of hospital stay and costs of care for patients with community-acquired pneumonia. Am J Med 2000; 109:378–85. [DOI] [PubMed] [Google Scholar]
- 5. Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg 2000; 191:123–30. [DOI] [PubMed] [Google Scholar]
- 6. Corraini P, Olsen M, Pedersen L, Dekkers OM, Vandenbroucke JP. Effect modification, interaction and mediation: an overview of theoretical insights for clinical investigators. Clin Epidemiol 2017; 9:331–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology 1999; 10:37–48. [PubMed] [Google Scholar]
- 8. Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. International Journal of Epidemiology 2013;42(5): 1511–9. doi: 10.1093/ije/dyt127. [DOI] [PubMed] [Google Scholar]