Abstract
Background
The rise in the number and earlier age of onset of obese persons has raised critical concerns about consequences of obesity; however, recent evidence suggests that the impact of obesity on health outcomes may have changed. This study aims to assess the change of the impact of obesity on active life expectancy among Americans aged 70 years and older over almost two decades, 1993–1998 to 2010–2014.
Methods
For each period, we use three waves of data from the Health and Retirement Study to estimate age-specific transition probabilities between health states. The average number of years active and disabled is calculated with Interpolated Markov Chain software based on estimated transition probabilities.
Results
Overall obesity and severe obesity increased markedly over time yet active life expectancy expanded for all individuals and the increases are greater among the obese and women. Increases in total and active life expectancy occurred because of the changing association of obesity with disability and mortality.
Conclusions
Individuals at age 70 years in the later period in each weight group could expect to live a smaller proportion of remaining life with activities of daily living disability than those in the earlier period. High levels of obesity continue to have significant adverse effects on the quality of life. The increasing prevalence of severe obesity and the growing number of older persons may result in substantial additional health care needs and costs. Continued effort to improve cardiovascular health is required to control the burden of obesity in later life in an era of rising obesity.
Keywords: Multistate life tables, Health trends, Health expectancy, IMaCh
There has been a striking rise in the number of obese older persons. In 2014, the prevalence of obesity (defined as body mass index, BMI ≥ 30) reached almost 40% among Americans aged 60 and older, rising from about 20% in the early 1990s (1,2). Americans are more likely to become obese at younger ages and to experience a greater duration of life with obesity over the life course (3), which could have a pronounced adverse effect on health. Coupled with advanced age, obesity can exacerbate functioning declines and the progression of chronic diseases, resulting in concerns about an increasing burden associated with obesity among older persons, which could be linked to increasing healthcare expenditures (4). Understanding the impact of obesity on changes in active life expectancy among the older population has important implications for forecasting the potential demand for health care and social services in the context of population aging and an obesity epidemic. In this study, we use national samples of Americans aged 70 years and older to provide a comprehensive picture of how obesity links to years spent with and without disability at two times to summarize changes over recent years in the burden of obesity in terms of years of total life and years with disability, metrics that can be readily understood by the public and policymakers (5).
The impact of obesity on active life expectancy may have changed in recent decades as a consequence of increasing obesity and changing associations of obesity with disability and mortality. Fueled by the large reduction in cardiovascular mortality, life expectancy at older ages has been improving (6). For instance, stroke death rates decreased by almost 40% from 2000 to 2015 (7). During the same time period, life expectancy at age 70 increased from 14.4 to 15.6 (8,9). After the year 2000, the decline in the prevalence of disability in the older population seems to have plateaued (10,11). With increasing life expectancy and small changes in disability, older persons may now live longer but also may spend more years of life in disability compared to their peers in the past.
Over time, a substantial weakening of the association between obesity and mortality has been reported. Mehta and Chang used data for two time periods from the Framingham Heart Study, the National Health and Nutrition Examination Survey (NHANES), and the National Health Interview Survey and found that Class I obesity (30 ≤ BMI < 35) was significantly associated with higher mortality relative to mortality for those with normal weight in earlier years but the excess risk was eliminated in more recent years; higher levels of obesity (BMI ≥ 35) remained significantly associated with mortality in the later periods, but a decline in the excess mortality associated with BMI at least 35 relative to normal weight was observed in the National Health Interview Survey data (12). The declining obesity–mortality association is likely to be related to the reduction of cardiovascular risk factors, such as high cholesterol, high blood pressure, and smoking, particularly among obese individuals (13–16). These positive trends are largely attributed by the increased use of antihypertensive and cholesterol-lowering medications, and the reduction in untreated hypertension and dyslipidemia, perhaps more so in obese persons (16,17). It is also possible that increased surgical management of obesity has contributed to a weakening of the obesity–mortality relationship (18,19). Studies have reported the positive effects of bariatric surgery on most cardiovascular risk factors (20), incidence of cardiovascular events (19), and mortality (19,21). The weakening relationship between obesity and mortality suggests that life expectancy may have a larger increase among obese older adults compared with nonobese older adults over time.
Reports on relationships between obesity and disability also indicate some change in recent years. Analysis of the NHANES data found that the odds of activities of daily living (ADL) disability declined significantly among nonobese persons aged 60 and older but did not change among obese older persons from 1988 to 2004 (22); a subsequent study showed moderate-to-severe disability among the obese declined in the 2005–2012 period, indicating the trend of an increasing gap in disability between the obese and nonobese has leveled off in recent years and may be improving for certain measures of disability (23).
Active life expectancy combines effects of both mortality and disability. Earlier work on the impact of obesity on active life expectancy using national data from 1993 to 1998 found that obesity had little effect on total life expectancy after age 70, but it was linked to shorter active life expectancy and longer disabled life expectancy (24). The differential influence of obesity on disability and mortality, the recent changes in the trends of health and mortality, and rising obesity indicate the value of revisiting the relationship between obesity and active life expectancy and examining change in this relationship over time. We build on earlier work using data from the Health and Retirement Study (HRS) for the population aged 70 and older in the United States (24) to extend the analysis to the 2010–2014 period from the 1993–1998 period to examine how the links between obesity, mortality, disability, and subsequent active life expectancy have changed over approximately two decades. We are limited to the population more than age 70 because of the way cohorts were added to the HRS and our desire to focus on change over time. We examine two categories of obesity, more moderate and higher, which were not considered separately in the earlier analysis. We expect that in the later period, older persons with obesity may live longer but they may live more years with disability compared with their peers at the earlier time, approximately 17 years ago.
Methods
Data
Data for this analysis come from the HRS, an ongoing nationally representative longitudinal study of older Americans with data for the population aged more than 70 available from 1993 onward. Details on the HRS survey design and procedures are available from the University of Michigan (http://hrsonline.isr.umich.edu). In this analysis, we examine individuals aged 70 and older at two time points: 1993–1998 and 2010–2014. Analysis for the 1993–1998 period uses the first three waves of data after the population aged more than 70 was added to the HRS in 1993. Analysis for the later period used the HRS sample for the population aged more than 70 from 2010 to 2014. Because the baseline sample in 1993 represented community-dwelling adults aged 70 and older, institutionalized persons were excluded from the initial samples used in our analysis for both time periods; however, those who resided in households but moved into institutions were included at subsequent waves. Initially, there are 7,339 individuals in the early period and 8,042 individuals in the later period. We excluded individuals with missing data on ADL disability or BMI at baseline (77 were excluded for the 1993–1998 period; 103 were excluded for the 2010–2014 period). We excluded an additional 188 persons (2.5%) from the 1993–1998 period and 203 persons (2.5%) in the 2010–2014 period because they only appeared at baseline and did not provide information after the first interview. Respondents who were lost to follow-up were less likely to be disabled at the baseline in the 1993–1998 period, but obesity status was not associated with loss to follow-up at either date. The final analytic sample consisted of 7,174 persons at baseline for the 1993–1998 period and 7,736 persons at baseline for the 2010–2014 period.
Measures
Mortality
HRS ascertains mortality from the National Death Index and reports of survivors. Weir (25) assessed the completeness of mortality ascertainment by comparing the HRS mortality to U.S. life tables and concluded that mortality ascertainment in the HRS is effectively complete. For both periods, date of death provided by the National Death Index was used when available; when not available from the National Death Index, the date provided by survivors in the HRS exit interview was used. If the date of death was unknown, it was assumed to be the midpoint of the interval.
Active and disabled life
Disability was indicated by having difficulty or being unable to perform at least one of the six ADLs: walking across a room, bathing or showering, eating, dressing, toileting, and transferring in or out of bed. Active life is defined as time without difficulty performing any of the ADLs; disabled life as time with difficulty performing one or more of the ADLs. Those living in nursing homes or other types of long-term care facilities were considered as disabled.
Obesity
BMI at the first wave of observation indicated weight status. BMI was calculated using self-reported weight and height. Obesity was defined according to the World Health Organization cutoff criteria of BMI of 30 or over. Obesity was further separated into two categories to examine whether increased health risk was differentially associated with moderate and higher levels of obesity: 30 ≤ BMI < 35 and BMI ≥ 35.
Statistical Analyses
We use a multistate life table approach to estimate total, active, and disabled life expectancies. Three health states were defined at each of three points in time for the cohort members: active, disabled, and dead. The method takes into account age-related state changes that reflect both movement into and movement out of disability among the obese and nonobese as well as the different mortality profiles characteristic of disability state by obesity (26). Obesity status and initial disability status (active or disabled) were determined using data from the baseline interview. Each person has three possible states at the two subsequent waves: active, disabled, and dead. There were six possible transitions between each interview: active to active, active to disabled (onset), active to dead, disabled to disabled, disabled to active (recovery), and disabled to dead (Figure 1). Death is an absorbing state from which there is no further transition. Age-specific transition probabilities between the health states were estimated by multinomial logistic regression models conditioned on age. The average number of years lived in each health state was calculated with Interpolated Markov Chain (IMaCh, version 0.99r16) software based on the estimated transition probabilities. IMaCh is designed to incorporate multiple waves of data, different interval lengths between survey waves, and cases with missing data (27). Interval length is constructed from information on the date of interview. Covariates include gender and two dummy variables indicating the level of obesity: 30 ≤ BMI < 35 and BMI ≥ 35. All analyses were weighted with sample weights so that the results are representative of the community-dwelling population aged 70 and older at baseline.
Figure 1.
States and transitions estimated in the multistate life table.
The probability of moving in and out of disability and of dying in the two time periods is presented in graphic form. Point estimates along with 95% confidence intervals (CIs) are shown in Supplementary Tables A1–A16. Estimates of the average total, active, and disabled life expectancies for obese and nonobese older adults are presented in tabular form, with 95% confidence intervals.
We then decompose the changes in health expectancies over time into the effect of change in weight composition of the population and the effect of the changing associations of obesity with disability and mortality. We first assume that the prevalence of BMI classes changed over time as observed but the associations between weight and disability and mortality stayed as observed in the earlier period. We then assume that the prevalence of BMI classes stayed as observed in the earlier period but that the associations of weight with disability and mortality changed as observed.
Results
Prevalence of Obesity
Table 1 presents the distribution of BMI for two periods. In 1993, about 11% (30 ≤ BMI < 35: 9.18%, BMI ≥ 35: 1.84%) of men and 15% (30 ≤ BMI < 35: 11.34%, BMI ≥ 35: 3.46%) of women aged 70 and older were obese; this prevalence increased to about 25% for both men and women in 2010. Older women were more likely than men to be obese in 1993; whereas in 2010, the prevalence of obesity was similar for men and women, reflecting more rapid increases in obesity prevalence among older men. The percentage of persons with 30 ≤ BMI < 35 increased by about nine percentage points for men and about five percentage points for women over these 17 years. In 1993, less than 2% of older men and 3.5% of older women had a BMI of at least 35; this number increased to almost 7% for men and 8% for women by 2010.
Table 1.
Distribution of Obesity, Aged More Than 70, the Health and Retirement Study 1993–1998 and 2010–2014
| 1993–1998 (N = 7,174) |
2010–2014 (N = 7,736) |
Change | |||
|---|---|---|---|---|---|
| Male | |||||
| BMI < 30 | 88.97 | (87.56–90.24) | 75.32 | (73.53–77.02) | –13.65 |
| 30 ≤ BMI < 35 | 9.18 | (8.04–10.47) | 18.07 | (16.65–19.59) | +8.89 |
| BMI ≥ 35 | 1.8 | (1.36–2.49) | 6.61 | (5.73–7.61) | +4.77 |
| Female | |||||
| BMI < 30 | 85.20 | (83.60–86.67) | 75.27 | (73.83–76.65) | –9.93 |
| 30 ≤ BMI < 35 | 11.34 | (10.26–12.51) | 16.50 | (15.39–17.67) | +5.16 |
| BMI ≥ 35 | 3.46 | (2.80–4.27) | 8.24 | (7.30–9.28) | +4.78 |
Transition Probabilities
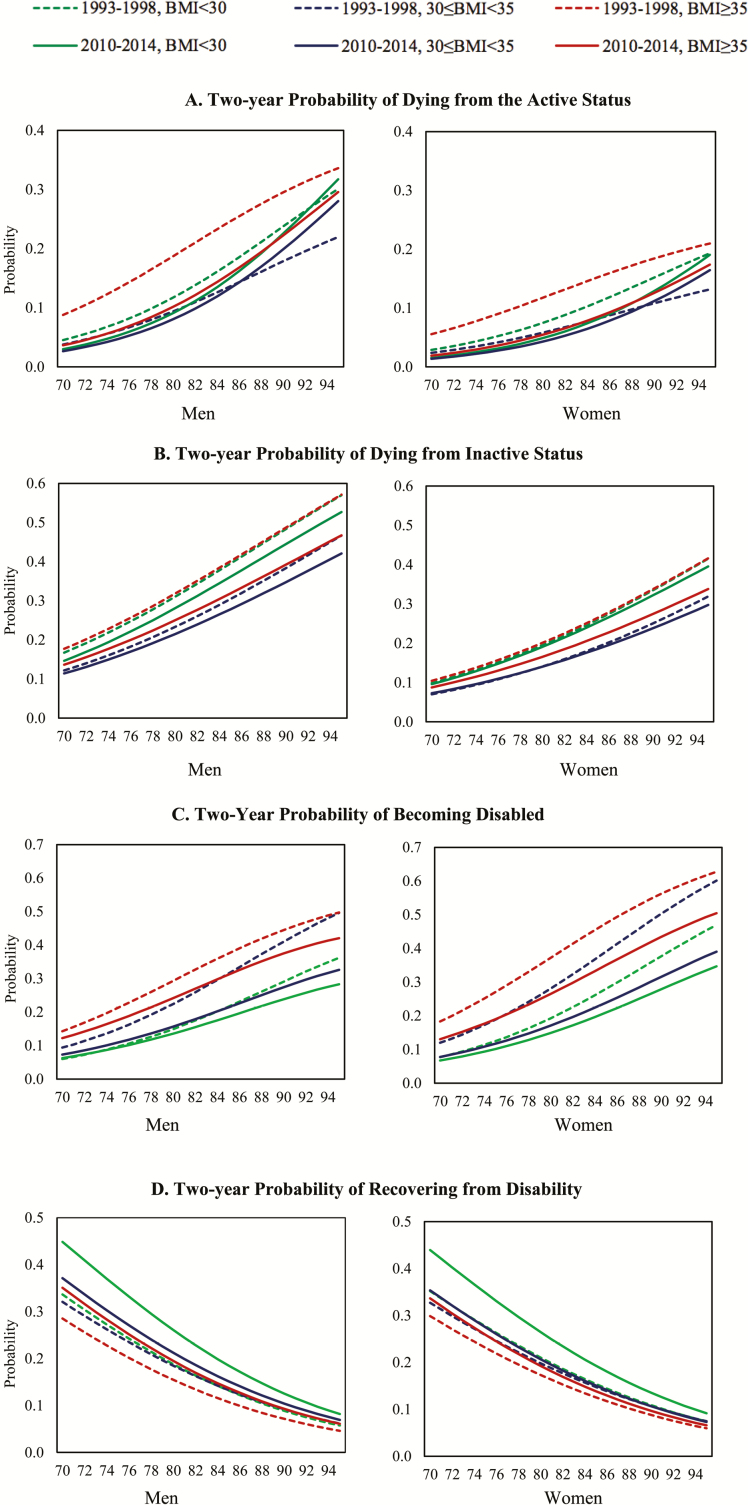
Figure 2 depicts 2-year probabilities of making health transitions for three BMI classes at each age: dying from either the active or disabled state and becoming disabled or recovering from disability.
Figure 2.
Two-year probability of health transitions for three weight classes. (A) Two-year probability of dying from the active status. (B) Two-year probability of dying from inactive status. (C) Two-year probability of becoming disabled. (D) Two-year probability of recovering from disability.
In the earlier period, nondisabled men with BMI of at least 35 had a statistically significantly higher risk of mortality at age 70–77 than their peers with 30 ≤ BMI < 35. This is the only group for whom the likelihood of dying among the three BMI groups is significantly higher at either date.
The probability of dying among the nondisabled has declined over time for almost all weight groups across the entire age range. The exception is nonobese men with BMI less than 30 at advanced old ages. The decline is significant for nonobese men aged between 70 and 82, nonobese women aged 70–87, and women aged 70–78 with BMI at least 35. In the earlier period, at age 70, the 2-year probability of dying was 0.045 (CI: 0.038–0.052) for nonobese men, 0.038 (CI: 0.027–0.049) for men with 30 ≤ BMI < 35, and 0.088 (CI: 0.050–0.126) for men with a BMI at least 35. These numbers decreased in the second period to 0.030 (CI: 0.024–0.036) for nonobese men, 0.027 (CI: 0.020–0.034) for men with 30 ≤ BMI < 35, and 0.036 (CI: 0.023–0.049) for men with BMI at least 35. The difference among the three BMI groups has become markedly smaller over time. The patterns of difference and changes in mortality risk are similar for women, although women’s mortality risk in each BMI class is lower than men’s at each age.
Figure 2B shows the 2-year probability of dying from the disabled status. Both for men and women who were disabled at the baseline interview, the likelihood of dying is not significantly associated with BMI. Although mortality risk is lower for the later period at each age, the reduction in mortality is not significant for any group.
The likelihood of becoming disabled for obese and nonobese persons at each age is presented in Figure 2C. Obese men and women had a significantly greater chance of becoming disabled compared with those who were not obese—these results are true for both periods, except for the oldest age (ages 93–95) group of men in 1993–1998 due to the wide confidence intervals for men with BMI at least 35. The probability of developing disability decreased significantly for less obese men, or those with 30 ≤ BMI < 35, after age 77 and nonobese men after age 90. Nonobese women aged 75 and older and women with moderate obesity (30 ≤ BMI < 35) at any age experienced significant reductions in the probability of becoming disabled. At the higher level of obesity, the likelihood of disability did not decline for either men or women. The decrease in the likelihood of becoming disabled is greater in obese than nonobese persons, and in women than in men.
The likelihood of recovering from disability or moving from the disabled to the able state is shown in Figure 2D. No significant differences over time in the probability of recovering were observed for obese persons. Only nonobese men between age 70 and 87 and nonobese women between age 74 and 84 experienced a statistically significant increase in the probability of recovering from disability to active over the two periods.
Health Expectancies
Table 2 presents the total, active, and disabled life expectancies at age 70 estimated based on the probabilities of making health transitions described earlier. Total life expectancy at age 70 is greatest among persons with 30 ≤ BMI < 35. The difference in total life expectancy is not significant between the nonobese and those with 30 ≤ BMI < 35. In 1993–1998, life expectancy at age 70 was significantly shorter for persons with BMI at least 35; however, the difference between those with high levels of obesity and others has been reduced and become nonsignificant in 2010–2014. All groups experienced increases over time in total life expectancy at age 70. Increases in total life expectancy were greatest among those with the higher level of obesity. The increase in total life expectancy for persons with 30 ≤ BMI < 35 was not significant.
Table 2.
Years of Total, Active, and Disabled Life Expectancy at Age 70, and Percent of Remaining Life Disabled at Age 70: the Health and Retirement Study 1993–1998 and 2010–2014
| 1993–1998 | 2010–2014 | |||||||
|---|---|---|---|---|---|---|---|---|
| Total | Active | Disabled | Disabled, % | Total | Active | Disabled | Disabled, % | |
| Male | ||||||||
| BMI < 30 | 12.7 | 10.0 | 2.7 | 21.3 | 14.5* | 11.6* | 2.9 | 20.0 |
| (12.2–13.2) | (9.5–10.4) | (2.5–3.0) | (13.9–15.0) | (11.1–12.1) | (2.6–3.1) | |||
| 30 ≤ BMI < 35 | 13.7 | 9.1 | 4.5 | 32.8 | 15.3 | 11.2* | 4.1 | 26.8 |
| (12.4–14.9) | (8.2–10.0) | (3.7–5.3) | (14.2–16.4) | (10.4–12.1) | (3.4–4.7) | |||
| BMI ≥ 35 | 9.4 | 5.8 | 3.6 | 38.3 | 13.0* | 8.5* | 4.5 | 34.6 |
| (7.8–11.0) | (4.6–7.1) | (2.5–4.6) | (11.6–14.4) | (7.4–9.6) | (3.6–5.4) | |||
| Female | ||||||||
| BMI < 30 | 15.5 | 10.7 | 4.8 | 31.0 | 17.9* | 13.3* | 4.6 | 25.7 |
| (15.0–16.0) | (10.3–11.1) | (4.5–5.2) | (17.3–18.5) | (12.7–13.8) | (4.3–5.0) | |||
| 30 ≤ BMI < 35 | 17.0 | 9.4 | 7.6 | 44.7 | 19.1 | 12.5* | 6.6 | 34.6 |
| (15.6–18.4) | (8.5–10.3) | (6.4–8.7) | (17.8–20.3) | (11.6–13.4) | (5.6–7.5) | |||
| BMI ≥ 35 | 12.4 | 6.3 | 6.2 | 50.0 | 16.5* | 9.5* | 7.0 | 42.4 |
| (10.6–14.3) | (5.0–7.6) | (4.6–7.7) | (14.9–18.1) | (8.3–10.6) | (5.8–8.3) |
*Indicates significant change from 1993–1998 to 2010–2014.
Individuals in all groups experienced significant increases in active life expectancy over time. Active life expectancy has extended from 10.0 to 11.6 years for nonobese men, 9.1 to 11.2 for obese men with 30 ≤ BMI < 35, 5.8 to 8.5 for obese men with BMI ≥ 35, 10.7 to 13.3 for nonobese women, 9.4 to 12.5 for obese women with 30 ≤ BMI < 35, and 6.3 to 9.5 for obese women with BMI ≥ 35. The increase is 1.6 for nonobese men, 2.1 for obese men with 30 ≤ BMI < 35, 2.7 for obese men with BMI of 35 or higher, 2.6 for nonobese women, 3.1 for obese women with 30 ≤ BMI < 35, and 3.2 for obese women with BMI of 35 and higher—indicating that the increase in active life is greater for women and for obese persons.
Disabled life expectancy increased 0.2 years for nonobese men and 0.9 years for obese men with BMI at least 35 and decreased 0.4 years for obese men with 30 ≤ BMI < 35, but none of the changes was statistically significant. Women with BMIs of lower than 35 had some insignificant reductions in disabled life expectancy—a 0.2 year decrease for nonobese women and 1-year decrease for obese women with 30 ≤ BMI < 35.
We also calculated the percent of total life that is disabled. For both generations, the proportion of disabled life is greater with higher BMI, and women spend a higher percentage of their remaining years in disability. Compared with the earlier time, older people in more recent years can expect to spend a smaller proportion of life with disability after age 70. The reduction is more substantial for obese persons than for nonobese persons. Nonobese men at age 70 in the later period can expect to spend 20% of their remaining years of life in disability, about a 1 percentage point reduction from the earlier period; obese men with 30 ≤ BMI < 35 could expect to spend 26.8% of their expected life disabled, a 6 percentage point decrease from their counterparts in the earlier period; and obese men with BMI of at least 35 could expect to spend 34.6% of their expected life disabled, a 3.7 percentage point reduction compared with their peers in the earlier period. The pattern of the change in the proportion of life lived with disability is similar in women, except that decrease in disabled time is larger for women than for men.
Effect of Change in BMI Composition and Links Between BMI and Disability and Mortality on Change in Total, Active, and Disabled Life Expectancy for the Entire Population
To this point, we have examined life expectancy within BMI classes. Changes in total, active, and disabled life expectancies for the total population can result from the compositional shift in BMI classes in the population and/or the changing links of BMI classes to disability and mortality. We calculate the hypothetical effect of the compositional change in weight and the change in mortality by BMI class on health expectancies at age 70 for the total population assuming either that only the distribution of weight changed or that only the weight-mortality/disability associations changed between the two periods (Table 3). To do this, we estimate the total, active, and disabled life expectancy for the entire population of men and women aged 70 in 1993–1998 and 2010–2012. The results, along with the hypothetical changes in these estimates, are given in Table 3 (labeled as “1993–1998 (observed)”, “2010–2014 (observed)”, and changes observed and with hypothetical changes). The overall level of life expectancy at age 70 increased by about 1.7 years for men and 2.3 years for women in this period. Most of the increase was in active life expectancy for men (1.5 years); for women, the increase in active life expectancy (2.4 years) exceeded that in total life expectancy. Assuming the transition schedules for weight with disability and mortality did not change from 1993–1998 to 2010–2014 but only the BMI composition of the population aged 70 and older changed, we calculate health expectancies for the 2010–2014 period. For instance, the total life expectancy in 2010–2014 assuming only BMI composition changed is the sum of the weighted total life expectancy for each BMI category for the 1993–1998 period, using the 2010–2014 BMI distribution as population weights. The results are presented in the column that labeled as “2010–2014 (assume only BMI composition change)” in Table 3. Our calculation shows that changing BMI composition has little effect on total life expectancy; it would have reduced active life by 0.2 years and extended disabled life by 0.2 years for both men and women. We also examined the change in life expectancy that would have occurred with only the changes in the associations between BMI and mortality and disability but no change in the prevalence of BMI classes. Large changes in total, active, and disabled life expectancies over time would have resulted from the changes in the links of obesity to disability and mortality (Labeled as “change”- “due to changes in associations of BMI with disability and mortality” in Table 3). These changes explained the observed increases in total and active life expectancy and would have led to even larger increases in the length of active life.
Table 3.
Changes in Total, Active, and Disabled Life Expectancy for the Entire Population at Age 70: the Health and Retirement Study 1993–1998 and 2010–2014: Actual and with Assumptions About Changing Body Mass Index (BMI) Composition and Changing Associations of BMI with Disability and Mortality
| 1993–1998 (Observed) | 2010–2014 (Observed) | 2010–2014 (assume only BMI composition change) | Changes | |||
|---|---|---|---|---|---|---|
| Observed change | Assuming only changes in BMI composition | Assuming only changes in associations of BMI with disability and mortality | ||||
| Male | ||||||
| Total | 12.7 | 14.4 | 12.7 | +1.7 | 0.0 | +1.7 |
| Active | 9.8 | 11.3 | 9.6 | +1.5 | –0.2 | +1.7 |
| Disabled | 2.9 | 3.2 | 3.1 | +0.3 | +0.2 | +0.1 |
| Female | ||||||
| Total | 15.5 | 17.8 | 15.5 | +2.3 | 0.0 | +2.3 |
| Active | 10.3 | 12.7 | 10.1 | +2.4 | –0.2 | +2.6 |
| Disabled | 5.2 | 5.1 | 5.4 | –0.1 | +0.2 | –0.3 |
Sensitivity Analysis
Low body weight and involuntary weight loss at old ages can indicate underlying health deterioration and are highly predictive of mortality (28). To examine the potential effect of illness on our results, we explored the sensitivity of our results to eliminating those who had been diagnosed with cancer before the initial interview, to eliminating those who were underweight at the first interview (BMI <18.5), to using lifetime maximum weight rather than current weight at the first interview for the second period, and to separating overweight from the normal weight category. Although the total, active, disabled life expectancy estimates from each analysis differ slightly from those presented here, almost no differences are statistically significant. Our observations on changes over time are not affected in a meaningful way. Details on the sensitivity analyses are provided in Supplementary Appendix B.
Discussion
Using a large nationally representative sample of older Americans aged 70 years and older, this article examined the dynamic impact of obesity on active life expectancy in two periods, 1993–1998 and 2010–2014. Our findings provide support for our hypotheses. Although obesity overall and obesity at higher levels increased markedly over this 17-year period; mortality declined for both obese and nonobese men and women over this period, and those with the highest level of obesity had the most substantial reduction. As a result, the mortality differences across BMI class have decreased. Changes in health transitions resulted in significant increases in total life expectancy in those with BMI less than 30 and BMI at least 35 for both men and women, and some increases for those with 30 ≤ BMI < 35. Active life expectancy expanded significantly for all individuals—the increases are greater among the obese and women. Changes in disabled life expectancy within BMI groups were not significant. Overall, individuals at age 70 in the later period in each of the BMI groups could expect to live a smaller proportion of remaining life with ADL disability. The reduction is more substantial among women and strongest among persons with 30 ≤ BMI < 35. The change in the distribution of BMI has bad a minor effect on overall and active life expectancy. Our results, about the declines in the association between obesity and mortality, are consistent with those from other recent studies (12,29). As cardiovascular health is the major pathway in which obesity is linked to mortality, the weakening association between obesity and cardiovascular mortality has been suggested as the dominant driving force for the declining association between BMI and mortality. Analysis using the NHANES from 1971 to 1994 identified that 19% of cardiovascular deaths were associated with obesity in the 1971–1975 survey and the number reduced to 10% in the 1976–1980 survey and further decreased to 5% in the 1988–1994 survey (30). It is also important to note that there is some evidence that significant reductions in cardiovascular mortality have slowed or even been eliminated in the last couple of years (31,32). If this trend continues, the favorable changes in the burden of obesity observed in this study will potentially diminish in the near future.
In addition to the improvement in medical conditions, recognizing the social and environmental context of disability and mortality is essential for understanding changes in associations between weight and disability and mortality. First, older populations in the more recent generation generally have a higher level of education than those in earlier time periods. Higher education has been associated with many favorable health outcomes including better functioning and lower mortality. The changes in the educational composition of older populations could contribute to the reduction in the associations of obesity with disability and mortality (33) and therefore weaken the negative impact of obesity on active life expectancy. Second, the physical and service environments in which older adults conduct daily activities have changed (34). Relative to their counterparts in the earlier period, older adults who are obese in the later period may be less likely to be ADL disabled because they use assistive technology and residential modifications to improve their ability to perform ADL activities (34,35).
There are several limitations to this study. First, our calculation of BMI was based on self-reported height and weight. Because the HRS started measuring height, weight, and waist circumference for a random half-sample at each wave since 2006, we cannot use measured BMI to assess the change in the impact of obesity over the long time period. We compared measured height and weight in 2010 to reported height and weight. Respondents overestimated height by 0.03 m and underestimated weight by 1.1 kg. We then recomputed our life tables using BMI based on measured height and weight for the 2010–2014 period. We do not observe meaningful differences in the active life expectancy estimates. Because reporting bias is unlikely to change in the short time period in which we are looking at the link between obesity and outcomes, it seems unlikely that our conclusions about change are affected by using self-reports.
Second, it has been suggested that BMI may be a suboptimal indicator of visceral fat in older populations because body fat redistributes from subcutaneous regions to intra-abdominal and intra-hepatic regions at old ages, but BMI cannot account for the fat distribution and its change (36). In addition, BMI could underestimate total adiposity in older adults as fat mass increases and lean mass decreases (37). However, this may ultimately have little effect on our analysis because increase in fat mass in older ages would make BMI underestimate fatness whereas height shrinkage would overestimate fatness and be a compensating factor (38). Waist circumference has been suggested to be a better indicator of abdominal adiposity than BMI (39). However, because waist circumference has been measured in the HRS only since 2006, it is not possible to assess time trends over the long time period. Third, because of the small number of highly obese individuals, particularly in the earlier period and at the oldest ages, our analysis for obese persons at the higher level of obesity may lack statistical power. Our analytic approach based on the IMaCh program is relatively conservative in assessing the significance of change because we compare the two point estimates using confidence intervals. It seems valuable to include this weight category even though the sample is relatively small in the first interval.
We believe this to be the first study to examine how the impact of obesity on active life expectancy has changed over time. Our results suggest that high levels of obesity continue to have significant adverse effects on the quality of life. Older people at the higher level of obesity should expect to spend 35% to 40% of their remaining life with disability at age 70 with a lower likelihood of recovering from disability than others. The nonobese at age 70 could expect to spend about 20% to 25% of remaining life with disability with a lower possibility of becoming disabled and a higher possibility of recovery. The increasing prevalence of severe obesity, along with the growing number of older persons, may result in substantial additional health care needs and costs. Although there has been some reduction in the impact of obesity on active life expectancy, continued effort to improve cardiovascular health will likely be required to control the burden of obesity in later life in an era of rising obesity.
Funding
This work was supported by grants P30AG17265 and T32AG000037 from the National Institute on Aging. The Health and Retirement Study (HRS) is sponsored by the National Institute on Aging (U01AG009740) and the Social Security Administration.
Conflict of Interest
None.
Supplementary Material
References
- 1. Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord. 1998;22:39–47. doi:10.1038/sj.ijo.0800541 [DOI] [PubMed] [Google Scholar]
- 3. Lee JM, Pilli S, Gebremariam A, et al. . Getting heavier, younger: trajectories of obesity over the life course. Int J Obes.. 2009;34:614. doi: 10.1038/ijo.2009.235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wee CC, Phillips RS, Legedza AT, et al. . Health care expenditures associated with overweight and obesity among US adults: importance of age and race. Am J Public Health. 2005;95:159–165. doi: 10.2105/AJPH.2003.027946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Robine JM, Cambois E, Nusselder W, Jeune B, Oyen HV, Jagger C; JA: EHLEIS team The joint action on healthy life years (JA: EHLEIS). Arch Public Health. 2013;71:2. doi: 10.1186/0778-7367-71-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mathers CD, Stevens GA, Boerma T, White RA, Tobias MI. Causes of international increases in older age life expectancy. Lancet. 2015;385:540–548. doi: 10.1016/S0140-6736(14)60569-9 [DOI] [PubMed] [Google Scholar]
- 7. Yang Q, Tong X, Schieb L, et al. . Vital signs: recent trends in stroke death rates — United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;66:933–939. doi: 10.15585/mmwr.mm6635e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arias E. United States Life Tables, 2000. Natl Vital Stat Reports. 2002;51(3):1–42. [PubMed] [Google Scholar]
- 9. Arias E, Xu J. United States life tables, 2015. Natl Vital Stat Rep. 2018;67:1–64. [PubMed] [Google Scholar]
- 10. Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability trends among older Americans: national health and nutrition examination surveys, 1988–1994 and 1999–2004. Am J Public Health.. 2010;100(1):100–107. doi: 10.2105/AJPH.2008.157388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Freedman VA, Spillman BC, Andreski PM, et al. . Trends in late-life activity limitations in the United States: an update from five national surveys. Demography. 2013;50:661–671. doi: 10.1007/s13524-012-0167-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mehta NK, Chang VW. Secular declines in the association between obesity and mortality in the United States. Popul Dev Rev. 2011;37:435–451. doi: 10.1111/j.1728-4457.2011.00429.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Crimmins EM. Trends in mortality, disease, and physiological status in the older population. In: Hayward MD, Majmundar MK, ed. Future Directions for the Demography of Aging: Proceedings of a Workshop. Washington, DC: The National Academies Press; 2018:3–30. doi: 10.17226/25064 [DOI] [PubMed] [Google Scholar]
- 14. Gregg EW, Cheng YJ, Cadwell BL, et al. . Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–1874. doi: 10.1001/jama.293.15.1868 [DOI] [PubMed] [Google Scholar]
- 15. Kramarow E, Lubitz J, Lentzner H, Gorina Y. Trends in the health of older Americans, 1970–2005. Health Aff (Millwood). 2007;26(5):1417–1425. doi: 10.1377/hlthaff.26.5.1417 [DOI] [PubMed] [Google Scholar]
- 16. Martin LG, Schoeni RF, Andreski PM. Trends in health of older adults in the United States: past, present, future. Demography. 2010;47 Suppl:S17–S40. doi: 10.1353/dem.2010.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Saydah S, Bullard KM, Cheng Y, et al. . Trends in cardiovascular disease risk factors by obesity level in adults in the United States, NHANES 1999–2010. Obesity (Silver Spring). 2014;22(8):1888–1895. doi: 10.1002/oby.20761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016;387:1947–1956. doi: 10.1016/S0140-6736(16)00271-3 [DOI] [PubMed] [Google Scholar]
- 19. Sjöström L, Peltonen M, Jacobson P, et al. . Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65. doi: 10.1001/jama.2011.1914 [DOI] [PubMed] [Google Scholar]
- 20. Sjöström L. Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS study. Int J Obes.. 2009;32:S93. doi: 10.1038/ijo.2008.244 [DOI] [PubMed] [Google Scholar]
- 21. Sjöström L, , Narbro K, , Sjöström CD, , et al. Effects of bariatric surgery on mortality in Swedish obese subjects. New Engl J Med. 2007;357(8):741–752. doi:10.1056/NEJMoa066254 [DOI] [PubMed] [Google Scholar]
- 22. Alley DE, Chang VW. The changing relationship of obesity and disability, 1988–2004. JAMA. 2007;298(17):2020–2027. doi: 10.1001/jama.298.17.2020 [DOI] [PubMed] [Google Scholar]
- 23. Chang VW, Alley DE, Dowd JB. Trends in the relationship between obesity and disability, 1988–2012. Am J Epidemiol. 2017;186(6):688–695. doi: 10.1093/aje/kwx092 [DOI] [PubMed] [Google Scholar]
- 24. Reynolds SL, Saito Y, Crimmins EM. The impact of obesity on active life expectancy in older American men and women. Gerontologist. 2005;45:438–444. doi: 10.1093/geront/45.4.438 [DOI] [PubMed] [Google Scholar]
- 25. Weir DR. Validating Mortality Ascertainment in the Health and Retirement Study. Ann Arbor, Michigan: Survey Research Center, Institute for Social Research, University of Michigan; 2016. [Google Scholar]
- 26. Crimmins EM, Hayward MD, Saito Y. Changing mortality and morbidity rates and the health status and life expectancy of the older population. Demography. 1994;31:159–175. doi:10.2307/2061913 [PubMed] [Google Scholar]
- 27. Lièvre A, Brouard N, Heathcote C. The estimation of health expectactancies from cross-longitudinal survyes. Math Popul Stud.. 2003;10(4):211–248. doi: 10.1080/713644739 [DOI] [Google Scholar]
- 28. Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–1867. doi: 10.1001/jama.293.15.1861 [DOI] [PubMed] [Google Scholar]
- 29. Flegal KM, Graubard BI, Williamson DF, Gail MH.. Excess Deaths Associated With Underweight, Overweight, and Obesity: An Evaluation of Potential Bias. Vital Health Statistics. 2018;June(42):1–21. [PubMed] [Google Scholar]
- 30. Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–2037. doi: 10.1001/jama.298.17.2028 [DOI] [PubMed] [Google Scholar]
- 31. Ma J, Ward EM, Siegel RL, Jemal A. Temporal trends in mortality in the United States, 1969–2013. JAMA. 2015;314(16):1731–1739. doi: 10.1001/jama.2015.12319 [DOI] [PubMed] [Google Scholar]
- 32. Sidney S, Quesenberry CP Jr, Jaffe MG, et al. . Recent trends in cardiovascular mortality in the United States and Public Health Goals. JAMA Cardiol. 2016;1:594–599. doi: 10.1001/jamacardio.2016.1326 [DOI] [PubMed] [Google Scholar]
- 33. Freedman VA, Martin LG. The role of education in explaining and forecasting trends in functional limitations among older Americans. Demography. 1999;36:461–473. doi: 10.2307/2648084 [DOI] [PubMed] [Google Scholar]
- 34. Freedman VA. The demography of late-life disability. In: Hayward MD, Majmundar MK, eds. Future Directions for the Demography of Aging: Proceedings of a Workshop. Washington, DC: The National Academies Press; 2018:269–305. [PubMed] [Google Scholar]
- 35. Verbrugge LM, Sevak P. Use, type, and efficacy of assistance for disability. J Gerontol B Psychol Sci Soc Sci. 2002;57:S366–S379. doi: 10.1093/geronb/57.6.s366 [DOI] [PubMed] [Google Scholar]
- 36. Alley DE, Ferrucci L, Barbagallo M, Studenski SA, Harris TB. A research agenda: the changing relationship between body weight and health in aging. J Gerontol A Biol Sci Med Sci. 2008;63:1257–1259. doi: 10.1093/gerona/63.11.1257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Batsis JA, Mackenzie TA, Bartels SJ, Sahakyan KR, Somers VK, Lopez-Jimenez F. Diagnostic accuracy of body mass index to identify obesity in older adults: NHANES 1999–2004. Int J Obes. 2016;40(5):761. doi: 10.1038/ijo.2015.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Villareal DT, Apovian CM, Kushner RF, Klein S; American Society for Nutrition; NAASO, The Obesity Society Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res. 2005;13:1849–1863. doi: 10.1038/oby.2005.228 [DOI] [PubMed] [Google Scholar]
- 39. Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–384. doi: 10.1093/ajcn/79.3.379 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.