Abstract
The Netherlands’ system for occupational exposure limits (OELs) encompasses two kinds of OELs: public and private. Public OELs are set by the government. Private OELs are derived by industry and cover all substances without a public OEL. In parallel, the regulation concerning the Registration, Evaluation, Authorisation and Restriction of Chemicals (REACH) has introduced an exposure guidance value similar to the OEL, namely the Derived No-Effect Level (DNEL) for workers’ inhalation exposure. This study aimed to investigate issues encountered by occupational health professionals regarding private OELs, and how they perceive the DNELs for workers in relation to private OELs. Towards this aim, we sent out a web-based questionnaire to the members of the Dutch professional organization for occupational hygienists (Nederlandse Vereniging voor Arbeidshygiëne [NVVA], n = 513) and to members of the Dutch professional organization for safety engineers (NVVK, n = 2916). Response rates were 27% (n = 139) and 7% (n = 198), respectively. More occupational hygienists (59%) than safety engineers (17%) reported to derive private OELs themselves. Our respondents reported several challenges with the derivation of private OELs. Fifty-one percent of the occupational hygienists and 20% of the safety engineers stated to see a role of REACH Registrants’ worker DNELs as private OELs. However, more than half of our respondents were undecided or unfamiliar with worker DNELs. In addition, stated opinions on where worker DNELs fit in the hierarchy of private OELs varied considerably. To conclude, both these professional groups derive private OELs and stated that they need more guidance for this. Furthermore, there is a lack of clarity whether worker DNELs may qualify as private OELs, and where they would fit in the hierarchy of private OELs.
Keywords: chemical risk management, health risk assessment, industrial hygiene, maximum allowable concentration, occupational health
Introduction
In 2007, the Netherlands introduced a new system for occupational exposure limits (OELs), encompassing two kinds of OELs: public and private. Public OELs are set by the government and cover about 190 substances. These include the substances for which the European Union (EU) requires OELs, unintentionally produced substances (‘substances without owners’, such as sawdust and diesel exhaust particles), and substances considered to pose a high risk (determined on a case-by-case basis). Private OELs cover all other substances used at Dutch workplaces, and the responsibility to derive and substantiate them lies on the individual companies (see also Schenk and Palmen, 2013).
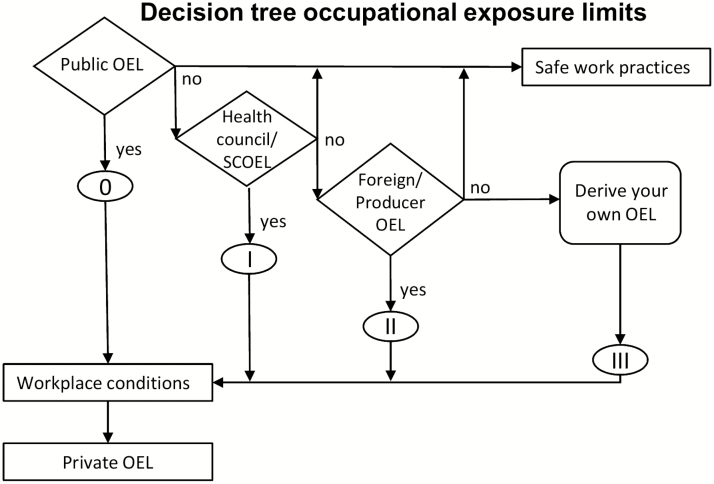
To aid companies in the implementation of the dual system of OELs a hierarchy of OELs was developed, outlining a stepwise approach on how to identify private OELs (Consortium TNO, Bureau KLB and Royal Haskoning, 2008). As shown in Figure 1, Step 0 and I in this approach is to adapt the public OELs (e.g. modify for longer exposure duration) and to adopt recommendations for OELs from the Commission's Scientific Committee on Occupational Exposure Limits (SCOEL) or the Dutch Health Council. Step II is to adopt OELs from other sources, such as foreign countries’ OELs or OELs described in the safety data sheet (SDS) provided by the producer of the substance. A ranking of potential sources for step II OELs (i.e. other countries’ lists of OELs) was also laid out, based on an evaluation of the general scientific quality of the OELs and the OEL-setters’ policy on weight of socioeconomic and technical factors. Step III is to derive an OEL de novo, using available toxicological hazard information. Step III OELs may also be derived from hazard banding approaches’ target airborne concentration ranges. The top section of Figure 1 refers to safe work practices. A safe work practice is defined as a clearly described activity/method in which, under defined circumstances, it is demonstrated for a specific (group of) substance(s) that the exposure does not cause any health damage (Terwoert, 2017). Although we note that it is unclear how this can be ascertained without an assessment of safe exposure (analogue to an OEL), we did not investigate further how respondents interpret this pathway.
Figure 1.
Schematic overview of hierarchy of private OELs in the Netherlands. Adapted from Consortium TNO, Bureau KLB and Royal Haskoning (2008). SCOEL, Scientific Committee on Occupational Exposure Limits.
In 2007, the European regulation concerning the Registration, Evaluation, Authorisation and Restriction of Chemicals (REACH) entered into force, introducing the Derived No-Effect Level (DNEL), among others also set for workers’ inhalation exposures. DNELs are derived by industry in their role as REACH Registrants or by the European Chemical Agency’s Risk Assessment Committee (ECHA RAC). The DNELs are intended to represent levels at which no harmful effects to health are to be expected, i.e. for threshold effects. For non-threshold effects, for which a DNEL cannot be established, the REACH guidance (ECHA, 2012) recommends a Derived Minimal Effect Level (DMEL). However, as DMELs are not defined under REACH, this article will focus solely on DNELs. Although worker inhalation DNELs and OELs are derived for different purposes and under different legislation, the form and overall aim of these values are similar (Schenk and Johanson, 2011, 2019; Schenk et al., 2015). In 2005, we investigated the motivations and purposes behind the introduction of the dual system of OELs in the Netherlands, interviewing government officials. There were no intentions to equate private OELs and DNELs (Schenk and Palmen, 2013). However, in practice occupational hygienists seemed to draw parallels between the two. For instance, in a questionnaire sent out to Dutch occupational hygienists, 21% reported to apply the ECHA REACH guidance when deriving private OELs (Schenk and Palmen, 2013).
This study aimed to investigate the use of private OELs by occupational health and safety professionals in the Netherlands and the issues they are confronted with when deriving private OELs. A second aim was to scope these professionals’ opinions on whether, and how, worker DNELs may function as private OELs.
Methods
Questionnaire
A questionnaire was developed to explore issues around the identification and use of public and private OELs. The questionnaire consisted of a mix of single choice, multiple-choice and open-ended questions, developed in an iterative process between the authors and feedback from colleagues in occupational hygiene. The design was also informed by previous works on OELs and REACH implementation (Schenk and Palmen, 2013; Schenk and Antonsson, 2015) and a summary of a workshop on OELs held at the annual meeting of the Dutch professional organization for occupational hygienists (Nederlandse Vereniging voor Arbeidshygiëne [NVVA]) in 2018 (NVvA, 2018). The questionnaire followed the same order of topics as presented in the results section with the following exceptions: (i) A section regarding public OELs (not reported herein). (ii) Usability of the decision tree (Figure 1), not reported as the reported issues were overlapping with the more specific issues raised in relation to step II and step III OELs. In addition, each topic as well as the questionnaire in full had a free-text comment field.
An invitation to participate was sent out to the mailing lists of the NVvA (513 members) and the Dutch professional organization for occupational safety engineers (Nederlandse Vereniging voor Veiligheidskunde [NVVK], 2916 members) in May 2018, with ~65 individuals being members of both organizations. The NVVK questionnaire was sent out 2 weeks after the NVvA questionnaire, and the NVVK invitation requested dual members to reply only to the first invitation if having received two. The questionnaire was open for 1.5 months and a reminder was sent out 2 weeks before the closing of the questionnaires. The questionnaire was anonymous; no personal identification data were collected.
We received 139 responses from NVvA members (response rate 27%) and 198 responses from NVVK members (response rate 7%).
Analysis
Categories for the coding of the open-ended questions were identified inductively through repeated close readings by all three authors independently. A joint set of categories was then agreed on for each question. Two of the authors (L.S. and N.P.) used the agreed on coding scheme to code the answers independently, and the third author (M.V.) resolved any disagreements in coding between the first two.
Statistical analyses were performed using cross-tabulation and descriptive statistics, using the R-3.3.2 software.
Results
In the following sections, we will refer to members of NVvA as occupational hygienists and members of NVVK as safety engineers. Most respondents stated to use both public and private OELs, whereas some stated to use only public or only private OELs (Table 1). Occupational hygienists to a larger extent used both public and private OELs, whereas safety engineers to a larger degree used only public OELs (Fisher’s Exact Test, P < 0.0001). A lower percentage of respondents stated to derive private OELs de novo, compared to those applying private OELs from other sources. Also, safety engineers to a lesser extent than occupational hygienists stated to derive private OELs themselves (Table 1) and were more likely to refer to public OELs and to consult an external expert (χ 2 = 11.43, df = 4, P = 0.022).
Table 1.
Use and derivation of private OELs. Percentagesa apply to number of respondents (in italics) per question (in bold)
| Occupational hygienists count (%) | Safety engineers count (%) | Combined count (%) | |
|---|---|---|---|
| Kind of OELs applied | |||
| Sum respondents | 139 (100) | 198 (100) | 337 (100) |
| Both public and private OELs | 126 (91) | 137 (69) | 263 (78) |
| Only public OELs | 12 (9) | 56 (28) | 68 (20) |
| Only private OELs | 1 (1) | 5 (3) | 6 (2) |
| Derive private OELs themselves? | |||
| Yes | 82 (59) | 37 (17) | 119 (35) |
| No | 57 (41) | 161 (83) | 218 (65) |
| Main reason for not deriving private OELs | |||
| Sum respondents | 57(100) | 161(100) | 218(100) |
| Consult an expert on OEL derivation | 14 (25) | 61 (38) | 75 (34) |
| Currently only public OELs needed | 15 (26) | 59 (37) | 74 (34) |
| Apply established safe work practices | 15 (26) | 17 (11) | 32(15) |
| OELs are determined at the company | 7 (12) | 15 (9) | 22 (10) |
| Other | 4 (7) | 8 (5) | 12 (6) |
| No answer | 2 (4) | 1 (1) | 3 (1) |
| Used sources for identifying potential step II OELs b | |||
| Sum respondents c | 82 (100) | 35 (100) | 117 (100) |
| OEL databases | 64 (78) | 11 (31) | 75 (64) |
| International OELs directly | 23 (28) | 8 (23) | 31 (26) |
| Producer and/or safety data sheet | 8 (10) | 10 (29) | 18 (15) |
| ECHA/REACH/DNEL | 13 (16) | 2 (6) | 15 (13) |
| Other | 8 (10) | 7 (20) | 15 (13) |
| Applied rules of thumb for selecting among several potential step II OELs b | |||
| Sum respondents c | 82 (100) | 35 (100) | 117 (100) |
| Choose lowest | 34 (41) | 29 (83) | 63 (54) |
| Quality assessment using predefined criteria | 31 (38) | 4 (11) | 35 (30) |
| Case-by-case quality assessment of scientific basis | 27 (33) | 2 (6) | 29 (25) |
| Other | 10 (12) | 7 (20) | 17 (15) |
| Perceived issues with step III OELs b | |||
| Sum respondents | 66 (100) | 27 (100) | 93 (100) |
| Hazardbanding concentration ranges too conservative | 23 (35) | 9 (33) | 32 (34) |
| Lack of data | 24 (36) | 7 (26) | 31 (33) |
| Methodology for OEL derivation | 20 (30) | 7 (26) | 27 (29) |
| Lack of expertise | 11 (17) | 1 (4) | 12 (13) |
| Labour- and cost intensive | 9 (14) | 3 (11) | 12 (13) |
| Uncertain results | 4 (6) | 1 (4) | 5 (5) |
| Other | 7 (11) | 6 (22) | 13 (14) |
| Proposed solutions to the identified issues with step III OELs b | |||
| Sum respondents | 56 (100) | 19 (100) | 75 (100) |
| OEL derivation protocol | 20 (36) | 7 (37) | 27 (36) |
| Toxicological expertise/training | 8 (14) | 6 (32) | 14 (19) |
| Information sharing/curated database of step III OELs | 9 (16) | 2 (11) | 11 (15) |
| Improve knowledgebase | 7 (13) | 4 (21) | 11 (15) |
| Access to tox data | 6 (11) | 0 (0) | 6 (8) |
| Other | 11 (20) | 1 (5) | 12 (16) |
aPercentages may not sum to 100 due to rounding off or due to more than one answer possible (labelled b).
bThese are categorized free-text answers, more than one answer per respondent possible, no statistical tests performed.
cThese respondents do not fully correspond to the ones stating to derive private OELs; 4 occupational hygienists and 7 Safety Engineers stated to derive private OELs but did not respond to the questions on step II OELs.
Step II OELs (e.g. adopt an OEL derived in another country or derived by producer)
Step II private OELs are generally adapted from other countries. The respondents reported to use a variety of sources, mainly consisting of publicly available or commercially available curated databases or, to a lesser extent, specifically named lists of OELs they preferred to use (Table 1). Safety engineers to a larger extent (29%) than occupational hygienists (10%) stated to use the information provided by the producer (for example, by means of the SDS) as a source of step II OELs. Occupational hygienists more frequently referred to ECHA, REACH, or DNELs than to producers and/or SDSs.
The most common principle, or rule of thumb, for selecting a suitable step II private OEL was to use the lowest OEL if several were available (Table 1). We see a clear difference between occupational hygienists and safety engineers in that among the latter group selecting the lowest OEL was the dominating principle (Table 1), whereas among occupational hygienists two other groups of principles or rules of thumbs were almost equally frequently stated as that of selecting the lowest OEL. The first of these two included various descriptions of predefined personal quality criteria, such as giving preference to OELs from a particular country or to choosing the most recently derived OEL. The second principle was stating to review the scientific basis of the OELs in order to find the most robust OEL.
In response to an open-ended question about difficulties of applying step II OELs relatively few respondents (occupational hygienists n = 39, safety engineers n = 13) offered any comments. Among the more common issues raised were problems with finding suitable OELs, how to choose between several conflicting OELs and difficulties in assessing the scientific and/or policy basis of potential step II OELs. A handful of respondents also raised the issue that it is unclear how DNELs relate to private OELs.
Step III OELs (de novo derivation of OEL)
The derivation of step III private OELs poses a number of challenges to occupational health and safety professionals (Table 1). Because of the small number of safety engineers, it is not possible to see any significant differences between the two professional groups regarding the issues raised with step III OELs. The most frequently found issue in our investigation was that available step III approaches such as target airborne concentration ranges of hazard banding (e.g. COSHH Essentials or DOHSBase kick-off values) may lead to low private OELs, often perceived as overly conservative by our respondents. Also commonly pointed out was lack of data on toxicological and/or physicochemical properties of the substances, hampering de novo derivation of OELs and leading to uncertain results. The third most commonly recurring theme was that of lacking a validated and generally approved methodology for derivation of step III private OELs, the lack of which leads to highly variable outcomes between approaches and communicative difficulties with end users and customers. A few respondents also pointed towards the derivation of step III private OELs being a resource and labour intensive undertaking (Table 1).
The respondents were also asked to specify what support they needed for resolving the issues with step III OELs, to which 75 commented (occupational hygienists n = 56, safety engineers n = 19). The most frequent response to this question was the need for a harmonized protocol for derivation of OELs. With regard to the derivation of step III OELs, respondents stated that the toxicological knowledge base needs improvement for data-poor substances. Furthermore, respondents mentioned that they need better access to available toxicological data as well as to develop of their own toxicological expertise. It was also suggested that companies need to be incentivized to commission step III OELs for the data-rich substances as these are time consuming, and thus expensive to derive. Another suggestion raised by several respondents was to build a database of private OELs, where companies can share their step III OELs.
Position of REACH DNELs in the Dutch dual system of OELs
To the question ‘Do you see a role for REACH worker DNELs as private OELs?’, approximately two-thirds of the safety engineers and two-fifths of the occupational hygienists stated that they were not familiar with DNELs or left the question unanswered (Table 2). Compared to the occupational hygienists, safety engineers to a larger extent stated to not know about these kinds of worker DNELs. The difference between the professional groups was statistically significant for both Registrant’s (χ 2 = 47.83, df = 2, P < 0.0001, excluding non-responders) and ECHA RAC’s worker DNELs (χ 2 = 51.74, df = 2, P < 0.0001, excluding non-responders). Roughly half of the occupational hygienists saw a role for worker DNELs from Registrants or ECHA RAC as private OELs (51% and 60%, respectively) and about one-fifth of safety engineers saw such a role (20% and 21%, respectively; Table 2). Comparing within each occupational group, there was no statistically significant difference between seeing a role or not for Registrants’ compared to ECHA RAC’s worker DNELs; neither for occupational hygienists (χ 2 = 0.58, df = 1, P = 0.45) nor for safety engineers (χ 2 = 1.46, df = 1, P = 0.23). In free-text comments to this question, several respondents mentioned that the potential role of worker DNELs depends on the quality of their derivation.
Table 2.
Role of worker DNELs as private OELsa
| Occupational hygienists | Safety engineers | |||
|---|---|---|---|---|
| Worker DNELs from: | Registrants count (%) | ECHA RAC count (%) | Registrants count (%) | ECHA RAC count (%) |
| Do you see a role for worker DNELs as private OELs? | ||||
| Yes, possibly | 27 (19) | 36 (26) | 23 (12) | 18 (9) |
| Yes, has already used | 44 (32) | 47 (34) | 16 (8) | 23 (12) |
| Combined Yes | 71 (51) | 83 (60) | 39 (20) | 41 (21) |
| No | 10 (7) | 8 (6) | 27 (14) | 18 (9) |
| Not familiar with these | 23 (17) | 17 (12) | 89 (45) | 74 (37) |
| Did not answer | 35 (25) | 31 (22) | 43 (22) | 65 (33) |
| If yes, worker DNELs would correspond to | ||||
| Step 0 | 3 (4) | 3 (4) | 5 (13) | 5 (12) |
| Step I | 5 (7) | 22 (26) | 14 (36) | 13 (32) |
| Step I or IIb | 2 (3) | 5 (6) | 0 (0) | 0 (0) |
| Step II | 31 (44) | 29 (35) | 10 (26) | 15 (37) |
| Step II or IIIb | 5 (7) | 4 (5) | 1 (3) | 0 (0) |
| Step III | 17 (24) | 12 (15) | 5 (13) | 6 (15) |
| Did not answer | 8 (11) | 8 (10) | 4 (10) | 2 (5) |
aPercentages may not sum to 100 due to rounding off.
bRespondents filled in two options.
Among those seeing a potential role of worker DNELs, opinions varied on where in the OEL-hierarchy (i.e. step 0–III in Figure 1) DNELs from Registrants or ECHA RAC would fit (Table 2). Answers ranged from step 0, i.e. DNELs equating or outweighing public OELs, to step III, i.e. DNELs equating target airborne concentration ranges of hazard banding. Hygienists were more likely to place ECHA RAC worker DNELs higher in the hierarchy (i.e. lower step number) than Registrant’s worker DNELs (Fishers’ exact test P = 0.008, excluding combination answers ‘Step I or II’ and ‘Step II or III’ and non-responders). This tendency was not seen among safety engineers, who also displayed a more even spread between the different steps in the hierarchy (χ 2 = 0.79, df = 3, P = 0.85, excluding combination answer ‘Step II or III’ and non-responders). In free-text comments, the most frequent reasons given for placing DNELs at a high position in the OEL hierarchy (e.g. step 0 or step I) connected to DNELs being health-based and derived following a harmonized protocol. On the other hand, for other respondents, concerns about the method and transparency of DNEL derivation were reasons to place them on a lower level (step II or step III OELs).
Discussion
The Dutch dual system is rather unique in that public, regulatory OELs are only provided for a limited number of substances, and companies are legally obliged to derive their own private OELs for all other chemical substances they use. This system was adopted in 2007, just before REACH entered into force, and DNELs were not available yet. Now, after one decade of operation of both systems, our study aimed to investigate the experience of Dutch occupational professionals with the use of private OELs and how they perceive REACH DNELs for workers’ inhalation exposure in relation to private OELs. A limitation of this study is the low response rate, in particular the 7% of safety engineers. Such a low response rate, however, may not be unexpected given that these professionals often may be focussed on other issues in occupational health and safety than chemical risk management (e.g. noise, physical health risks, psychological factors, accident prevention, also discussed in Schenk and Palmen (2013)). The difference in response rates (27% versus 7%) likely reflects the difference in the degree to which these professions work with chemical risk management. In addition, safety engineers being members of both organizations were asked to only fill in the occupational hygienist version of the questionnaire. Nevertheless, we do see that both professional groups are relevant to target with information and/or further education about OELs and chemicals risk management.
A recurring topic in the comments regarding private OELs was the lack of consistency, i.e. that different workplaces may apply different OELs for the same substance. Reliability of OELs may differ between sources, for various reasons (e.g. Deveau et al., 2015), and only one-third of occupational hygienists and very few safety engineers stated to review the background information of an OEL when selecting one out of several potential OELs in step II. There is a demand for a curated database of suitable values and the corresponding background documents. There are several databases overviewing OELs, both freely and commercially available, which are being used by the respondents, for instance, the GESTIS International Limit Values (available at: https://limitvalue.ifa.dguv.de/, Accessed 24 May 2019). Another example of a freely available database is the one hosted by the Dutch Socio-Economic Council (SER). Given the national context this is an important resource for our respondents and keeping it up to date and developing its user-friendliness would be a valuable asset for occupational health and safety professionals. At the time of writing, the SER is working on an update of their online database of OELs (available at: https://www.ser.nl/nl/thema/arbeidsomstandigheden/Grenswaarden-gevaarlijke-stoffen/Grenswaarden, under development, 24 May 2019).
With respect to step III OELs, these are required in case there are no step II OELs available, an issue often correlating to lack of toxicological information about the substances. A clear derivation methodology, possibly combined with a clearer incentive for companies to allow for the time and resources required, may help with issues such as consistency and communication for data-rich substances. However, the situation of uncertainty will remain unresolved until more knowledge is available for the data-poor substances. A precautionary approach seems reasonable, however, many of the respondents seem to find current available approaches based on hazard banding to be unreasonably conservative. Vaughan and Rajan-Sithamparanadarajah (2017) showed that the exposure concentration ranges of COSHH Essentials corresponded to the 10th percentile of OELs for substances in that hazard band. Assuming the subset of substances with OELs is representative for the subset without OELs, this implies a relatively high degree of protection. However, arguments could be made for aiming for the 5th or even 1st percentile as well. We note that defining over-conservatism is a complex issue and that what constitutes over-protection in the absence of substance-specific data is an issue for further policy discussion.
Regarding the role of REACH worker DNELs as private OELs, it was striking that a considerable proportion of the respondents replied that they were not familiar with DNELs or did not answer the question at all. Indeed, the questionnaire was distributed the same month as the third and final REACH registration deadline, a circumstance we expected to increase awareness of, and interest in, DNELs. It should be noted that some of our respondents commented that this question was unclear to them (hygienists n = 12 engineers n = 5); however, this does not explain the full extent of non-responders. The high number of respondents being unfamiliar with, or undecided about, DNELs in 2018 indicates a need for education of occupational professionals regarding the role of REACH worker DNELs and their possibilities as well as limitations for use as private OELs. Of those respondents who were familiar with DNELs, 34% of the occupational hygienists and 12% of the safety engineers claimed to have used worker DNELs from ECHA’s Risk Assessment Committee (RAC). RAC has derived worker DNELs for a very limited set of substances (RAC opinions are available at: https://echa.europa.eu/en/about-us/who-we-are/committee-for-risk-assessment, Accessed 18 April 2019). In comparison, worker DNELs from REACH Registrants cover around 5000 substances (GESTIS, 2018). These had been used by 32% and 8% of the occupational hygienists and safety engineers, respectively. Although the answers to the follow-up question indicate that most occupational hygienists are aware of the difference between DNELs derived by RAC or by Registrants, as they rank them differently, we did not see such a distinction among safety engineers. A possible interpretation is that these respondents were not fully aware of there being different sources of worker DNELs, and thus not how to label the RAC DNELs in relation to the Registrant worker DNELs, which we presume are the kind of worker DNELs mainly accessed. Again, this indicates an important need for education, especially since in the Netherlands safety engineers often are the first person of contact regarding chemical risk management, in particular in smaller companies.
The broad range of responses on which step of private OELs a worker DNEL would correspond to, if at all suitable, could to some part reflect lack of guidance regarding under which conditions these may be approved or disapproved as private OELs. This needs to be discussed in relation to the system of private OELs in the Netherlands. In addition, several respondents in the comments throughout the questionnaire expressed doubts about the quality of registrant’s DNELs. Lack of transparency is an issue for third-party evaluation of the reliability of DNELs, and there are also reports of unreliable DNELs, for instance, some DNELs were based on route-to-route extrapolation while the available toxicological data pointed towards local effects in the respiratory tract (Schenk et al., 2015; Schenk and Johanson, 2019).
However, neither the label ‘OEL’ nor the label ‘DNEL’ is a guarantee for a reliable health-based limit. All exposure guidance values are subject to epistemological limitations (Hansson, 1998; Fairhurst, 2003). Issues with reliability, consistency, and/or transparency of (specific) OELs have been pointed out repeatedly (Fairhurst, 1995; Hansson, 1998; Borak and Brosseau, 2015). A recent example is the scrutiny of the safety margins applied by SCOEL by Schenk and Johanson (2018). Reliability of an exposure standard is a key issue for occupational health and safety professionals in all OEL systems, especially in the dual-system of OELs applied in the Netherlands where companies are required to select (or derive) well-founded private OELs. This study offers some insight into issues encountered by occupational hygienists and safety engineers in the application of the dual system of OEL setting in the Netherlands, especially the application and derivation of private OELs.
It must be noted that the SER scheme of the hierarchy of OELs, as depicted in Figure 1, is currently being revised (at the time of conducting the survey, this revision had not been announced yet). The revised scheme will include DNELs and will hopefully provide more guidance on how to use and derive step II and step III OELs. The results of this survey may provide some directions regarding the information needs to be addressed in the revision of the scheme.
Conclusions
We saw differences between the two professional groups of occupational hygienists and safety engineers regarding application and derivation of private OELs according to the Dutch dual system of OELs. As expected, occupational hygienists were more active in deriving private OELs themselves than safety engineers. Nevertheless, both groups would benefit from more guidance how different sources of OELs qualify as step II private OELs and how to approach the issue of step III private OELs. In addition, there is lack of clarity whether worker DNELs may qualify as private OELs, and where they would fit in the hierarchy of private OELs. The opinions on this issue were very disparate.
The current situation results in varying approaches and the possibility of widely variable private OELs co-existing for the same substance. Harmonized guidance for the application of step II OELs and the derivation of step III OELs could decrease these inconsistencies. This would aid in achieving consistent levels of protection for employees as well as levelling the playing field regarding costs for risk management measures.
Acknowledgements
The authors are grateful to the NVvA and NVVK for assistance with questionnaire distribution and to the members of NVvA and NVVK who kindly shared their experience and expertise through answering to our questionnaire. The authors thank Cindy Bekker for assistance with the questionnaire development, distribution and comments on a previous version of the manuscript. Thanks also to Renske Beestra for comments on a previous version of the manuscript.
Funding
Linda Schenk’s participation was funded by the AFA Insurance Foundation (project no 160032). The authors designed and executed the study and have sole responsibility for the writing and content of the manuscript.
Disclaimer
The authors declare no conflict of interest relating to the material presented in this article.
References
- Borak J, Brosseau LM (2015) The past and future of occupational exposure limits. J Occup Environ Hyg; 12 Suppl 1: S1–3. doi: 10.1080/15459624.2015.1091263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consortium TNO, Bureau KLB and Royal Haskoning (2008) Beslisschema grenswaarde keuze. Notitie aan de Beleidingscommissie Leidraad. January 8th 2008. Reference: 9S2119.01/N0009D/Nijm, Sociaal-Economische Raad.
- Deveau M, Chen CP, Johanson G et al. (2015) The global landscape of occupational exposure limits–implementation of harmonization principles to guide limit selection. J Occup Environ Hyg; 12 Suppl 1: S127–44. doi: 10.1080/15459624.2015.1060327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECHA – European Chemicals Agency (2012) Guidance on information requirements and chemical safety assessment Chapter R.8: Characterisation of dose [concentration]-response for human health. November 2012. Version 2.1. Helsinki: ECHA. [Google Scholar]
- Fairhurst S. (1995) The uncertainty factor in the setting of occupational exposure standards. Ann Occup Hyg 39:375–85. doi: 10.1016/0003-4878(95)00007-2. [DOI] [Google Scholar]
- Fairhurst S. (2003) Hazard and risk assessment of industrial chemicals in the occupational context in Europe: some current issues. Food Chem Toxicol 41:1453–62, doi: 10.1016/S0278-6915(03)00193-5. [DOI] [PubMed] [Google Scholar]
- GESTIS (2018) GESTIS DNEL-list Available at: https://www.dguv.de/ifa/gestis/gestis-dnel-liste/index-2.jsp, version accessed: June 2018.
- Hansson SO. (1998) Setting the limit: Occupational health standards and the limits of science. New York: Oxford University Press; ISBN: 0195121600. [Google Scholar]
- NVvA (2018) Samenvatting workshop grenswaarden [Summary workshop occupational exposure limits.] NVvA symposium 12 April 2018, Session S 14:30. Available at: https://www.arbeidshygiene.nl/symposium/vorige-symposia/symposium-2018/, Accessed 24 May 2019.
- Schenk L, Antonsson AB (2015) Implementation of the chemicals regulation REACH - Exploring the impact on occupational health and safety management among Swedish downstream users. Saf Sci 80:233–42. doi: 10.1016/j.ssci.2015.08.001. [DOI] [Google Scholar]
- Schenk L, Johanson G (2011) A quantitative comparison of the safety margins in the European indicative occupational exposure limits and the derived no-effect levels for workers under REACH. Toxicol Sci; 121: 408–16. doi: 10.1093/toxsci/kfr056 [DOI] [PubMed] [Google Scholar]
- Schenk L, Johanson G (2018) Use of uncertainty factors by the European Commission Scientific Committee of Occupational Exposure Limits: A follow up. Crit Rev Toxicol; 48: 513–521. doi:10.1080/10408444.2018.1483891 [DOI] [PubMed] [Google Scholar]
- Schenk L, Johanson G (2019) Will worker DNELs derived under the European REACH regulation extend the landscape of occupational exposure guidance values? Arch Toxicol; 93: 1187–1200. doi: 10.1007/s00204-019-02439-0 [DOI] [PubMed] [Google Scholar]
- Schenk L, Deng U, Johanson G (2015) Derived no-effect levels (DNELs) under the European chemicals regulation REACH–an analysis of long-term inhalation worker-DNELs presented by industry. Ann Occup Hyg; 59: 416–38. doi: 10.1093/annhyg/meu103 [DOI] [PubMed] [Google Scholar]
- Schenk L, Palmen NG (2013) Throwing the baby out with the bath water? Occupational hygienists’ views on the revised Dutch system for occupational exposure limits. Ann Occup Hyg; 57: 581–92. doi: 10.1093/annhyg/mes095 [DOI] [PubMed] [Google Scholar]
- Terwoert J. (2017) Veilige werkwijzen voor stoffen—waaraan moeten deze voldoen? [Safe working methods for substances—what should they fulfil?] J Appl Occup Sci 30: 29–35. In Dutch. Available at: https://www.arbeidshygiene.nl/-uploads/files/insite/tta-2017-02-opinierend-terwoert.pdf, Accessed 1 May 2019. [Google Scholar]
- Vaughan NP, Rajan-Sithamparanadarajah R (2017) An assessment of the robustness of the COSHH-Essentials (C-E) target airborne concentration ranges 15 years on, and their usefulness for determining control measures. Ann Work Expo Health; 61: 270–83. doi: 10.1093/annweh/wxx002 [DOI] [PubMed] [Google Scholar]