Abstract
The aim of the present study is to report the demographic and clinical characteristics of all jaw cysts diagnosed in a single Oral Pathology Department. 5294 cases of jaw cysts diagnosed during a 38-year period were retrospectively collected and classified according to the latest classification of Head and Neck Tumors of the World Health Organization. The patients’ gender and age, as well as the main clinical features of the cysts were retrieved from biopsy report forms. Jaw cysts were more common in male patients, with a male to female ratio of 1.6:1. Most patients were in the 4th–6th decade of life, with a mean age of 42.3 ± 16.1 years. There was no jaw predilection and the majority of lesions were more commonly encountered in the anterior region of the maxilla, followed by the molar region of the mandible. The most common jaw cyst was radicular cyst followed by dentigerous cyst, residual cyst and odontogenic keratocyst. The majority of jaw cysts are of inflammatory origin and represent a sequale of pulp necrosis. However, other type of jaw cysts may also be found.
Keywords: Jaw cysts, Odontogenic cysts, Jaw cysts epidemiology
Introduction
Jaw cysts are considered uncommon in clinical practice [1], although they constitute a large percentage of specimens in oral and maxillofacial pathology practice [2]. Jaw cysts are classified as true cysts or pseudocysts, depending on the presence or absence of lining epithelium; as inflammatory or developmental based on their pathogenesis and odontogenic or non-odontogenic according to the tissue of origin [3]. The recent World Health Organization (WHO) classification of Head and Neck Tumors 2017 [4] included jaw cysts and classified them as follows:
-
Odontogenic cysts of inflammatory origin
- Radicular cyst (RC)
- Inflammatory Collateral Cysts (ICC)
-
Odontogenic and non- odontogenic developmental cysts
- Dentigerous cyst (DC)
- Odontogenic Keratocyst (OKC)
- Lateral periodontal cyst (LPC) and botryoid odontogenic cyst (BOC)
- Gingival cyst (GC)
- Glandular odontogenic cyst (GOC)
- Calcifying odontogenic cyst (COC)
- Orthokeratinized odontogenic cyst (OOC)
- Nasopalatine duct cyst (NDC)
-
Bone cysts
- Aneurysmal bone cyst (ABC)
- Simple bone cyst (SBC)
The most significant changes in the new classification compared to the previous one [5], refer to the replacement of keratocystic odontogenic tumor and calcifying cystic odontogenic tumor by OKC and COC respectively. The re-instatement of these entities in the cyst group is in accordance with two previous WHO classifications [6, 7]. In addition, ABC and SBC are classified as “bone cysts” [4] instead of “bone related lesions” [5]; OOC is considered a distinct entity [4], whereas in previous classifications it was either not mentioned [5], or was reported as a variant of odontogenic keratocyst [7]; buccal bifurcation cyst (BBC) and paradental cyst (PDC) are included under the collective term “inflammatory collateral cysts” [4]; new diagnostic histopathological criteria are proposed for the GOC [4]; finally, NDC is the only non-odontogenic cyst which is included in the new classification [4], whereas nasolabial cyst, is omitted as a soft tissue cyst [8].
To the best of our knowledge, the latest WHO classification has been applied only in one study of jaw cysts, considering pediatric patients [9]. The aim of the present study is to report the demographic and clinical features of jaw cysts of a single center classified according to the latest WHO classification of Head and Neck Tumors [4].
Materials and Methods
This is a retrospective study on pathology material. All cases of jaw cysts diagnosed from 1980 to 2017 were retrieved from the files of the Department of Oral Medicine and Pathology and diagnoses were confirmed by studying representative 5 μm thick hematoxylin and eosin stained tissue sections, following the latest WHO classification of Head and Neck Tumors [4]. The age and gender of the patients, as well as the location of the lesions were collected from the biopsy request forms and were tabulated using Microsoft Excel® 2016. Concerning location, each jaw was divided into six regions named anterior (area of anterior teeth), premolar (area of premolars), molar (area of molars and distal of them) and combinations of the aforementioned regions to encompass lesions which extended to more than one area (anterior-premolar, anterior-molar, premolar-molar). The study was approved by the Ethics and Research Committee of the Department of Dentistry, School of Health Sciences, National and Kapodistrian University of Athens, Greece (Ref.367/22.06.208).
Results
Out of 32.701 biopsies retrieved during a 38-year study period, 5294 cases of jaw cysts were detected, representing approximately 16.2% of the total number of cases. The diagnosis was modified in the following cases:
Out of 57 cases diagnosed as GOC, 19 fulfilled the new diagnostic criteria [4], whereas the remaining were re-classified as RC (22 cases), DC (10 cases), residual cysts (RDC) (5 cases) and NDC (1 case).
One case initially diagnosed as OKC was re-classified as OOC, as the lining epithelium was orthokeratinized.
Six cases diagnosed as globulomaxillary cysts were re-classified as RC (5 cases) and DC (1 case).
All diagnoses are tabulated in Table 1. RC was the most common jaw cyst representing 57.3% of the total sample size. RC reached an even higher percentage of 71.4% with the addition of RDC, which is a “radicular cyst that remains in the jaws after extraction of the affected tooth” [4]. The second most common jaw cyst was DC (14.5% or 14.6% with the inclusion of eruption cyst (EC) which is “a variant of dentigerous cyst found in the soft tissues overlying an erupting tooth” [4]) followed by OKC (8.2%).
Table 1.
Number of cases of each jaw cyst
| Cyst | Number of cases (%) | % of male patients | % of female patients | Male: female ratio |
|---|---|---|---|---|
| All cysts | 5294 (100) | 61.9 | 38.1 | 1.6:1 |
| RC | 3035 (57.3) | 59 | 41 | 1.4:1 |
| DC | 766 (14.5) | 65.3 | 34.7 | 1.8:1 |
| RDC | 749 (14.1) | 74.2 | 25.8 | 2.9:1 |
| OKC | 436 (8.2) | 56.7 | 43.3 | 1.3:1 |
| NDC | 129 (2.4) | 66.7 | 33.3 | 2:1 |
| PDC | 53 (1) | 52.8 | 47.2 | 1.1:1 |
| LPC | 31 (0.6) | 51.6 | 48.4 | 1.1:1 |
| COC | 19 (0.4) | 42.1 | 57.9 | 0.7:1 |
| GOC | 19 (0.4) | 68.4 | 31.6 | 2.2:1 |
| OOC | 15 (0.3) | 92.9 | 7.1 | 13:1 |
| GC | 13 (0.2) | 38.5 | 61.5 | 0.6:1 |
| ABC | 11 (0.2) | 36.4 | 63.6 | 0.6:1 |
| SBC | 9 (0.2) | 22.2 | 77.8 | 0.3:1 |
| EC | 5 (0.1) | 60 | 40 | 1.5:1 |
| BBC | 4 (0.1) | 75 | 25 | 3:1 |
A minority of patients presented with more than one cyst: 47 patients had two, 3 patients three and 1 patient four RCs; 7 patients had two and 1 patient three RDCs; 20 patients presented with two and 1 patient with four DCs; 15 patients had two, 8 patients three and 3 patients four OKCs; Finally, 1 patient developed two OOCs. Concerning OKC, according to the information provided by the biopsy request forms, nine patients were already diagnosed with Basal Cell Nevus Syndrome (BCNS) (OMIM #109400). Of those patients, 2 had one OKCs, 4 had two and 3 patients four OKCs.
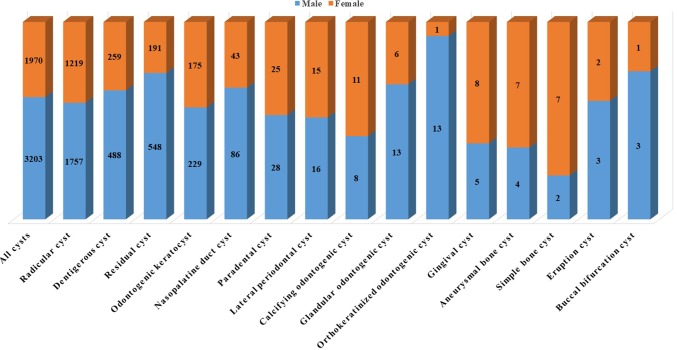
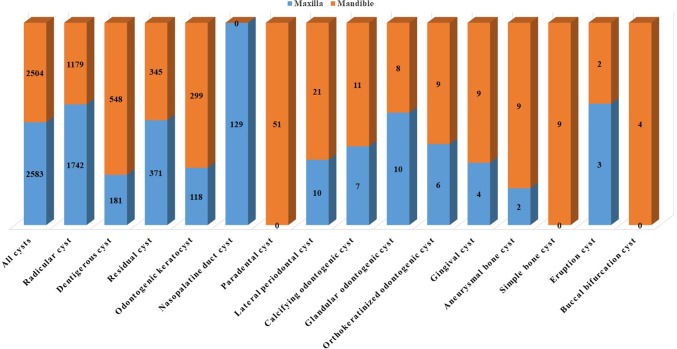
As a whole, jaw cysts were more common in males (61.9%) compared to females (38.1%) (Fig. 1; Table 1). Most patients were in the 4th -6th decade of life with a mean age of 42.3 ± 16.1 years (median age 42 years) (Tables 2, 3). The difference in the mean age between males (43.2 ± 16 years, median age 43 years) and females (40.8 ± 16.2 years, median age 40 years), was not statistically significant. There was no predilection for either jaw (Fig. 2). Most cases appeared in the anterior region of the maxilla and the molar region of the mandible (Table 4).
Fig. 1.
Number of male and female patients for each jaw cyst
Table 2.
Age of patients in years
| Cyst | Mean age of all patients (age range) (median age) | Mean age of male patients (age range) (median age) | Mean age of female patients (age range) (median age) |
|---|---|---|---|
| All cysts | 42.3 ± 16.1 (0.5–93) (42) | 43.2 ± 16 (0.5–92) (43) | 40.8 ± 16.2 (1–93) (40) |
| RC | 41.2 ± 14.4 (2–93) (40) | 41.4 ± 14 (2–86) (40) | 40.8 ± 15.1 (7–93) (40) |
| DC | 38.7 ± 18.4 (0.5–86) (40) | 39.8 ± 18.6 (0.5–86) (42) | 36.6 ± 17.8 (1–77) (36) |
| RDC | 50.5 ± 14.6 (11–93) (50) | 51.7 ± 14.3 (11–92) (51) | 46.8 ± 15.2 (12–93) (46) |
| OKC | 42.5 ± 19.4 (5–84) (42.5) | 43.5 ± 19.2 (7–84) (44) | 41.3 ± 19.6 (5–80) (40) |
| NDC | 46.6 ± 16.3 (9–85) (45) | 47.3 ± 17.4 (9–85) (46.5) | 45 ± 14.7 (16–80) (45) |
| PDC | 29.3 ± 7.2 (18–56) (28) | 28.8 ± 8.3 (18–56) (26.5) | 29.7 ± 6 (21–44) (28.5) |
| LPC | 51.1 ± 15.6 (12–81) (52) | 46.5 ± 16.5 (12–72) (46) | 55.8 ± 13.6 (24–81) (58) |
| COC | 44.3 ± 22 (14–92) (37.5) | 47.8 ± 20.6 (28–92) (42) | 41.6 ± 23.7 (14–82) (32) |
| GOC | 51.1 ± 14.4 (30–84) (50.5) | 49.5 ± 16.1 (30–84) (50) | 55.4 ± 8.3 (43–64) (55) |
| OOC | 48 ± 19.5 (20–81) (45) | 50.1 ± 18.5 (28–81) (45) | 20 (20) (20) |
| GC | 52.5 ± 10.4 (35–65) (57) | 58.2 ± 3.7 (54–63) (59) | 48.9 ± 11.8 (35–65) (49) |
| ABC | 24.8 ± 16.4 (8–55) (16) | 21.3 ± 15.9 (12–45) (14) | 26.9 ± 17.6 (8–55) (23) |
| SBC | 21.8 ± 12.3 (14–51) (16) | 33.5 ± 24.7 (16–51) (33.5) | 18.6 ± 6.5 (14–32) (15) |
| EC | 8.2 ± 4 (2–13) (9) | 6.3 ± 3.8 (2–9) (8) | 11 ± 2.8 (9–13) (11) |
| BBC | 8.4 ± 2.6 (6–12) (7.75) | 7.2 ± 1.3 (6–8.5) (7) | 12 (12) (12) |
Table 3.
Age of patients by decade in years
| Cyst | 1st decade (Male/Female) | 2nd decade (Male/Female) | 3rd decade (Male/Female) | 4th decade (Male/Female) | 5th decade (Male/Female) | 6th decade (Male/Female) | 7th decade (Male/Female) | 8th decade (Male/Female) | 9th decade (Male/Female) | 10th decade (Male/Female) |
|---|---|---|---|---|---|---|---|---|---|---|
| All cysts | 59 (38/21) | 328 (184/144) | 716 (382/334) | 1059 (682/377) | 1066 (683/383) | 903 (583/320) | 549 (351/198) | 201 (143/58) | 42 (29/13) | 4 (2/2) |
| RC | 9 (6/3) | 147 (74/73) | 476 (258/218) | 698 (449/249) | 660 (408/252) | 485 (281/404) | 272 (159/113) | 64 (39/25) | 14 (7/7) | 1 (0/1) |
| DC | 37 (23/14) | 99 (66/33) | 92 (51/41) | 127 (77/50) | 126 (84/42) | 134 (97/37) | 64 (45/19) | 28 (19/9) | 4 (4/0) | 0 |
| RDC | 0 | 8 (5/3) | 43 (21/22) | 119 (86/33) | 166 (126/40) | 178 (136/42) | 121 (97/24) | 69 (57/12) | 11 (10/1) | 2 (1/1) |
| OKC | 4 (2/2) | 53 (29/24) | 56 (28/28) | 62 (38/24) | 57 (32/25) | 58 (38/20) | 54 (27/27) | 31 (20/11) | 5 (3/2) | 0 |
| NDC | 1 (1/0) | 6 (4/2) | 9 (5/4) | 22 (16/6) | 31 (17/14) | 20 (14/6) | 24 (18/6) | 5 (5/0) | 3 (2/1) | 0 |
| PDC | 0 | 1 (1/0) | 27 (14/13) | 17 (8/9) | 4 (2/2) | 1 (1/0) | 0 | 0 | 0 | 0 |
| LPC | 0 | 1 (1/0) | 3 (2/1) | 0 | 9 (6/3) | 7 (2/5) | 8 (3/5) | 1 (1/0) | 1 (0/1) | 0 |
| COC | 0 | 1 (0/1) | 4 (1/3) | 4 (2/2) | 3 (2/1) | 2 (2/0) | 1 (0/1) | 1 (0/1) | 1 (0/1) | 1 (1/0) |
| GOC | 0 | 0 | 0 | 3 (3/0) | 4 (3/1) | 7 (5/2) | 2 (0/2) | 1 (1/0) | 1 (1/0) | 0 |
| OOC | 0 | 0 | 3 (2/1) | 3 (3/0) | 2 (2/0) | 3 (3/0) | 0 | 1 (1/0) | 2 (2/0) | 0 |
| GC | 0 | 0 | 0 | 2 (0/2) | 2 (0/2) | 6 (3/3) | 3 (2/1) | 0 | 0 | 0 |
| ABC | 1 (0/1) | 5 (3/2) | 1 (0/1) | 1 (0/1) | 2 (1/1) | 1 (0/1) | 0 | 0 | 0 | 0 |
| SBC | 0 | 5 (1/4) | 2 (0/2) | 1 (0/1) | 0 | 1 (1/0) | 0 | 0 | 0 | 0 |
| EC | 4 (3/1) | 1 (0/1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| BBC | 3 (3/0) | 1 (0/1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Fig. 2.
Jaw distribution for each jaw cyst
Table 4.
Site of all cysts
| Cyst | AnMax (M/F) | PrMax (M/F) | MlMax (M/F) | AnPrMax (M/F) | AnMlMax (M/F) | PrMlMax (M/F) | AnMnd (M/F) | PrMnd (M/F) | MlMnd (M/F) | AnPrMnd (M/F) | AnMlMnd (M/F) | PrMlMnd (M/F) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All cysts | 1350 (785/564) | 391 (246/145) | 438 (248/189) | 138 (97/41) | 104 (82/22) | 96 (69/27) | 364 (190/174) | 484 (311/173) | 1334 (841/493) | 69 (53/16) | 82 (65/17) | 110 (81/29) |
| RC | 975 (532/442) | 284 (175/109) | 257 (142/114) | 80 (52/28) | 53 (42/11) | 49 (36/13) | 252 (130/122) | 287 (178/109) | 520 (321/199) | 39 (29/10) | 17 (14/3) | 42 (28/14) |
| DC | 72 (51/21) | 9 (5/4) | 62 (38/24) | 17 (12/5) | 8 (6/2) | 6 (3/3) | 26 (16/10) | 41 (21/20) | 439 (292/147) | 3 (3/0) | 7 (7/0) | 17 (13/4) |
| RDC | 134 (92/42) | 78 (57/21) | 61 (42/19) | 28 (24/4) | 31 (26/5) | 33 (26/7) | 32 (19/13) | 108 (86/22) | 101 (70/31) | 20 (16/4) | 35 (29/6) | 34 (28/6) |
| OKC | 25 (15/10) | 13 (8/5) | 53 (22/31) | 6 (4/2) | 7 (4/3) | 6 (3/3) | 29 (19/10) | 30 (15/15) | 193 (108/85) | 5 (5/0) | 21 (13/8) | 14 (11/3) |
| NDC | 128 (85/43) | 0 | 0 | 1 (1/0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| PDC | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 (1/0) | 50 (26/24) | 0 | 0 | 0 |
| LPC | 4 (3/1) | 4 (1/3) | 1 (1/0) | 0 | 1 (0/1) | 0 | 6 (1/5) | 12 (7/5) | 2 (2/0) | 0 | 0 | 1 (1/0) |
| COC | 2 (0/2) | 2 (0/2) | 1 (1/0) | 0 | 1 (1/0) | 1 (1/0) | 3 (1/2) | 2 (0/2) | 3 (2/1) | 1 (0/1) | 1 (1/0) | 0 |
| GOC | 4 (2/2) | 1 (0/1) | 0 | 3 (3/0) | 2 (2/0) | 0 | 1 (1/0) | 0 | 6 (4/2) | 0 | 0 | 0 |
| OOC | 1 (1/0) | 0 | 1 (1/0) | 1 (1/0) | 1 (1/0) | 1 (0/1) | 1 (1/0) | 1 (1/0) | 6 (6/0) | 0 | 1 (1/0) | 0 |
| GC | 3 (2/1) | 0 | 1 (1/0) | 0 | 0 | 0 | 7 (1/6) | 1 (1/0) | 0 | 1 (0/1) | 0 | 0 |
| ABC | 0 | 0 | 1 (0/1) | 1 (0/1) | 0 | 0 | 2 (0/2) | 0 | 5 (4/1) | 0 | 0 | 2 (0/2) |
| SBC | 0 | 0 | 0 | 0 | 0 | 0 | 5 (1/4) | 1 (0/1) | 3 (1/2) | 0 | 0 | 0 |
| EC | 2 (2/0) | 0 | 0 | 1 (0/1) | 0 | 0 | 0 | 0 | 2 (1/1) | 0 | 0 | 0 |
| BBC | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 (3/1) | 0 | 0 | 0 |
M/F male/female, AnMax anterior maxilla, PrMax premolar maxilla, MlMax molar maxilla, AnPrMax anterior-premolar maxilla, AnMlMax anterior-molar maxilla, PrMlMax premolar-molar maxilla, AnMnd anterior mandible, PrMnd premolar mandible, MlMnd molar mandible, AnPrMnd anterior-premolar mandible, AnMlMnd anterior-molar mandible, PrMlMnd premolar-molar mandible
COC, GC, ABC and SBC were more common in female patients and ABC, SBC, EC and BBC occurred in younger patients. DC, OKC, LPC, GC and ABC more commonly developed in the mandible. PDC, SBC and BBC occurred exclusively in the mandible, whereas NDC exclusively in the maxilla.
Discussion
In this retrospective study based on pathology material, the demographic and clinical features of 5294 jaw cysts are described. In Table 5, the results of the present study are compared to those of previous ones with a sample of at least 1000 patients [2, 10–17]. It should be noted that the sample size of the present study is the 3rd largest in the literature following Daley’s et al. [17] and Jones’ and Franklin‘s [2] investigations. Four out of ten studies included in Table 5 [11, 12, 14, 16] included only odontogenic cysts, whereas two studies [2, 10] provided details on the majority of jaw cysts.
Table 5.
Studies including more than 1000 patients reporting the frequency of each jaw cyst
| Cyst | Present Study (2017 [4] WHO classification) | Lo Muzio et al. [10] (2005 [5] WHO classification) | Jaeger et al. [11] (1992 [7] and 2005 [5] WHO classification) | Khosravi et al. [12] (2005 [5] WHO classification) | Tekkesin et al. [13] (1992 [7] WHO classification) | Sharifian and Khalili [14] (1992 [7] WHO classification) | Grossmann et al. [15] (1992 [7] WHO classification) | Ochsenius et al. [16] (1992 [7] WHO classification) | Jones and Franklin [2] (1992 [7] WHO classification) | Daley et al. [17] (No referral to any WHO classification) |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of cases (%) | Number of cases (%) | Number of cases (%) | Number of cases (%) | Number of cases (%) | Number of cases (%) | Number of cases (%) | Number of cases (%) | Number of cases (%) | Number of cases (%) | |
| All cysts | 5294 (100) | 2018 (100) | 5157 (100) | 1603 (100) | 5003 (100) | 1151 (100) | 2876 (100) | 2944 (100) | 6164 (100) | 6996 (100) |
| RC | 3035 (57.3) | 865 (42.9) | 3240 (62.8) | 563 (35.1) | 2802 (56) | 465 (40.4) | 1772 (61.6) | 1494 (50.7) | 3229 (52.4) | 4468 (63.9) |
| DC | 766 (14.5) | 806 (39.9) | 1248 (24.2) | 413 (25.8) | 529 (10.6) | 303 (26.3) | 735 (25.6) | 546 (18.5) | 1081 (17.5) | 1662 (23.8) |
| RDC | 749 (14.1) | 218 (10.8) | – | 208 (13) | 482 (9.6) | 99 (8.6) | – | 328 (11.1) | 564 (9.1) | Included in RC |
| OKC | 436 (8.2) | – | 475 (9.2) | 362 (22.6) | 1048 (20.9) | 239 (20.8) | 208 (7.2) | 421 (14.3) | 591 (9.6) | 335 (4.8) |
| NDC | 129 (2.4) | 38 (1.9) | – | – | 66 (1.3) | – | 64 (2.2) | – | 237 (3.8) | 295 (4.2) |
| PDC | 53 (1) | 20 (1) | 63 (1.2) | 10 (0.6) | 11 (0.2) | 23 (2) | 19 (0.7) | 113 (3.8) | 367 (6) | 33 (0.5) |
| LPC | 31 (0.6) | 14 (0.7) | 21 (0.4) | 13 (0.8) | 6 (0.1) | 7 (0.6) | 7 (0.2) | 17 (0.6) | 25 (0.4) | 106 (1.5) |
| COC | 19 (0.4) | – | 30 (0.6) | 21 (1.3) | 33 (0.7) | – | 30 (1) | – | 16 (0.3) | 18 (0.3) |
| GOC | 19 (0.4) | 14 (0.7) | 3 (0.1) | 7 (0.4) | 23 (0.5) | 4 (0.3) | 2 (0.1) | 1 (0.03) | 10 (0.2) | 6 (0.1) |
| OOC | 15 (0.3) | 9 (0.4) | 18 (0.3) | 4 (0.2) | – | – | 9 (0.3) | – | – | – |
| GC | 13 (0.2) | 12 (0.6) | 9 (0.2) | 1 (0.1) | – | 4 (0.3) | 1 (0.03) | 10 (0.3) | 15 (0.2) | 33 (0.5) |
| ABC | 11 (0.2) | 6 (0.3) | – | – | – | – | – | 7 (0.1) | – | |
| SBC | 9 (0.2) | 4 (0.2) | – | – | – | – | – | – | 17 (0.3) | – |
| EC | 5 (0.1) | 12 (0.6) | 50 (1) | 1 (0.1) | 1 (0.02) | 7 (0.6) | 26 (0.9) | 11 (0.4) | 5 (0.1) | 40 (0.6) |
| BBC | 4 (0.1) | – | – | – | – | – | – | – | – | - |
| BOC | – | – | – | – | 2 (0.04) | – | 2 (0.1) | – | – | – |
| GCI | – | – | – | – | – | – | 1 (0.03) | 3 (0.1) | – | – |
GCI gingival cyst of infants
Jaw cysts in our study represented approximately 16.2% of all biopsies accessioned during a 38 year period. Jones and Franklin [2] reported 6164 cysts among 44,007 (14%) biopsies during a 30-year period. Tekkesin et al. [13], 5003 cases in a total of 42,296 biopsies (11.8%) during a 40-year period and Daley et al. [17] 6996 cysts among 40,000 cases (17.5%) during a 27-year period. The results of the three aforementioned studies and the present study, confirm that jaw cysts are not a rarity in an oral and maxillofacial pathology department.
Odontogenic cysts in the present study accounted for 97.2% of the sample size, which is comparable to 97.6% and 95.8% reported by Lo Muzio et al. [10] and Jones and Franklin [2], respectively. In the majority of the studies included in Table 5 [2, 11, 12, 14–17] RC was reported as the most common jaw cyst followed by DC, OKC and RDC. In the present study, RDC was more common than OKC, whereas in the study of Tekkesin et al. [13], OKC was the second most common jaw cyst, after RC, followed by DC and RDC, while in the study of Lo Muzio et al. [10] OKC was not included in the sample and as such after RC, the most common jaw cysts were DC and RDC.
Differences in the origin of the study material, as well as the classification adopted [10, 17] may account for minor differences among the studies. The demographic and clinical characteristics of RC, DC, RDC, PDC, GOC, LPC, GC and EC in the present study are in accordance with those reported in the excellent review presented by Lo Muzio et al. [10]. However, as there are more recent systematic reviews on LPC, GC [18] and GOC [19], those cysts, as well as OKC, OOC, COC, NDC, ABC, SBC and BBC will be further analyzed.
In a recent systematic review [20], OKC showed a male predominance with a male to female ratio of 1.5:1. The majority of patients were in the 2nd-4th decade of life with a mean age of 37.81 ± 6.33 years and most lesions developed in the posterior part of the mandible. In the present study, OKC had a slight predilection for males and for the molar region of the mandible, but the majority of the patients were in the 4th–6th decade of life with a mean age of 42.5 ± 19.4 years. Differences in the mean age of patients may be attributed to the variability in the clinical and demographic characteristics of OKC among ethnic groups [20]. In the present study patients diagnosed with BCNS represented approximately 2.2% of all OKC patients, in contrast to the 7% reported previously [20]. It is possible that more patients in our study, especially younger ones [21] or those with multiple lesions [22] could have been diagnosed with BSNS. However, as we relied solely on the information provided in the biopsy request forms, no such conclusions could be drawn, as the diagnosis of the syndrome is based on specific diagnostic criteria [21]. This limitation also holds for the recurrence rate which in our study was only 5.2% compared to the 16.5% reported in a recent systematic review [23].
In a systematic review by MacDonald-Jankowski [24], OOC showed a male to female ratio of approximately 2:1; most patients were in the 2nd-4th decade of life with a mean age of 34.89 ± 5.28 years; and the posterior mandible was most frequently involved. In contrast, in our study, only 1 out of 15 cases presented in a female patient and the majority of the patients were in the 3rd, 4th and 6th decade of life with a mean age of 48 ± 19.5 years. A predilection for the molar region of the mandible was also found.
de Arruda et al. [25] carried out a systematic review of the literature on ghost cell odontogenic lesions of the jaws. In their study [25] COCs exhibited no gender predilection, as 51.8% of the patients were males and 48.2% females and the majority of the patients were in the 2nd decade of life with a mean age of 30.7 ± 21 years. Furthermore, no predilection for either jaw was noted with 51.7% cases affecting the mandible and 48.3% the maxilla [25]. In addition, no predilection for a specific anatomical region of jaws was noted with 47.5% of cases developing in the anterior region, 43.9% in the posterior region, while 8.6% extended from the posterior to the anterior region [25]. Among the 19 COCs of our sample, females comprised 57.9%, most patients were in the 3rd-5th decade of life with a mean age of 44.3 ± 22 years, and 61.1% of the lesions involved the mandible, without predilection for any specific region.
Considering LPC, a recent systematic review [18] reported that 52.6% of the cases occurred in males; most patients were in the 4th-6th decade of life with a mean age of 46.8 ± 12.5 years; 69.8% of LPC involved the mandible, while the more common regions were in descending order the mandibular premolar region (25.9%), the maxillary anterior region (23.6%) and the mandibular anterior-premolar region (18.4%). Those findings are comparable to those of the 31 LPC cases of the present study, where 51.6% of the patients were males, most patients were in the 5th-7th decade of life with a mean age of 51.1 ± 15.6 years, while 67.7% of the lesions affected the mandible, in particular the premolar (38.7%) and anterior (19.4%) regions.
In the systematic review of Chrcanovic and Gomes [18], 58.4% of GC manifested in females, the majority of the patients were in the 6th decade of life with a mean age of 48.6 ± 12.9 years, and 76.5% of lesions occurred in the mandible, specifically in the anterior-premolar (35.7%) and anterior region (27.7%). This data is in agreement with our findings as 61.5% of GC cases appeared in females, mostly in the 6th decade of life with a mean age of 52.5 ± 10.4 years, and 69.2% of lesions developed in the mandible and specifically in the anterior region (53.8%).
The aforementioned authors, performed a systematic review on GOC [19] applying diagnostic criteria comparable but not identical to those of WHO 2017 [4]. According to their investigation [19], 53.6% of the patients were males; the majority of the patients were in the 5th and 6th decade of life with a mean age of 48.1 ± 13.1 years and 73.2% of the lesions occurred in the mandible and specifically in the anterior-premolar (20.5%), anterior-molar (15.9%) and the anterior (14.8%) regions. A recurrence rate of 21.6% was also reported [19]. Based on the criteria of the recent WHO classification [4], of the 57 cases with a diagnosis of GOC in our material, only 19 were considered consistent with GOC. The majority of patients (68.4%) were males, mostly in the 5th and 6th decade of life with a mean age of 51.1 ± 14.4 years. 55.6% of cases involved the maxilla while the most common locations were the mandibular molar region (35.3%) and the anterior region of the maxilla (23.5%).
The data of three large epidemiological studies on NDC [26–28] showed that in 102 cases of NDC, males were affected in 66.7% of the cases and the mean age of the patients was 42.7 ± 18.54 years [26], 37.4 years [27] and 46.8 years [28] respectively. Jones and Franklin [2], who have reported the largest number of NDCs to date along with its demographic characteristics, also showed that this type of cyst is more common in male patients (66.2%) and the mean age of the patients is 48.3 ± 15.4 years. The results of the present study, are in accordance with the aforementioned data of the literature as the majority of patients (66.7%) were males, mostly in the 4th-7th decade of life and a mean age of 46.6 ± 16.3 years.
According to the largest study on ABC in the maxillofacial area [29], male patients constituted 57.5% of the cases, the majority of the patients were in the 2nd decade of life with a mean age of 20.7 ± 2.5 years, and 71.8% of lesions involved the mandible, with the posterior regions being more commonly affected in both jaws. In our sample of 11 ABCs 63.6% affected female patients, mostly in the 2nd decade of life with a mean age of 24.8 ± 16.4 years and 81.8% of the lesions involved the mandible, while the most common location was the mandibular molar region (45.5%).
SBC and BBC were uncommon in our material with only 9 and 4 cases respectively. SBC has a female predominance (77.8%), the majority of patients were in the 2nd decade of life with a mean age of 21.8 ± 12.3 years, and all lesions involved the mandible. Combining the demographic characteristics of the three large case series regarding SBCs [30–32], it can be assumed that this lesion has no gender predominance with 59 cases (48.4%) occurring in males and 63 (51.6%) in females. Peacock et al. [32] reported that the mean age of patients of their study was 30 years while Perdigão et al. [30] and Chadwick et al. [31] provided separately the median and mean age respectively for females (18 [30] and 18.8 [31] years) and males (16 [31] and 18.2 [30] years). In two studies [31, 32] in which the location was reported, 95.5% of SBC cases were located in the mandible, particularly in the posterior areas. BBC in the present study occurred in three males and one female patient, all in the buccal aspect of the first molar with the mean age being 8.4 ± 2.6 years. Our findings are comparable to those of the largest study on BCC [33] but no bilateral case was detected in contrast to 23.6% of bilateral occurrence which has been reported in the aforementioned study.
Conclusion
Jaw cysts are common in oral and maxillofacial pathology practice. Most are of odontogenic origin, mainly radicular cysts, although other types may also be found, most commonly dentigerous cysts and odontogenic keratocysts. The clinical and demographic characteristics of jaw cysts in the present study, are in accordance with other large retrospective studies or systematic reviews. However, this study is the only large retrospective study based on the 2017 WHO classification of Head and Neck Tumors [4]. More studies using this classification will help to determine the exact incidence and specific clinicopathological features of jaw cysts.
Compliance with Ethical Standards
Conflict of interest
All authors declare that the have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Johnson NR, Savage NW, Kazoullis S, Batstone MD. A prospective epidemiological study for odontogenic and non-odontogenic lesions of the maxilla and mandible in Queensland. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:515–522. doi: 10.1016/j.oooo.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 2.Jones AV, Franklin CD. An analysis of oral and maxillofacial pathology found in adults over a 30-year period. J Oral Pathol Med. 2006;35:392–401. doi: 10.1111/j.1600-0714.2006.00451.x. [DOI] [PubMed] [Google Scholar]
- 3.Shear M, Speight P. Cysts of the Oral and Maxillofacial Regions. Ames: Wiley-Blackwell; 2007. pp. 1–2. [Google Scholar]
- 4.El-Naggar AK, Chan JKC, Grandis JR, Takata T, Sootweg P. World Health Organization classification of head and neck tumours. 4. Lyon: IARC; 2017. pp. 232–240. [Google Scholar]
- 5.Barnes L, Eveson JW, Reichart P, Sidransky D, editors. WHO classification of tumors. Pathology and genetics of head and neck tumours. Lyon: IARC Press; 2005. pp. 284–327. [Google Scholar]
- 6.Pindborg J, Kramer I. WHO international histological classification of tumours. Histological typing of odontogenic tumours, jaw cysts and allied lesions. Geneva: WHO; 1971. [Google Scholar]
- 7.Kramer I, Pindborg J, Shear M. WHO international histological classification of tumours. Histological typing of odontogenic tumours. 2. Berlin: Springer-Verlag; 1992. [Google Scholar]
- 8.Martin LHC, Speight PM. Odontogenic cysts: an update. Diagn Histopathol. 2017;23:260–265. doi: 10.1016/j.mpdhp.2017.04.006. [DOI] [Google Scholar]
- 9.da Silva LP, Gonzaga AK, Severo ML, et al. Epidemiologic study of odontogenic and non-odontogenic cysts in children and adolescents of a Brazilian population. Med Oral Patol Oral Cir Bucal. 2018;23:e49–e53. doi: 10.4317/medoral.22138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lo Muzio L, Mascitti M, Santarelli A, et al. Cystic lesions of the jaws: a retrospective clinicopathologic study of 2030 cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;124:128–138. doi: 10.1016/j.oooo.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Jaeger F, de Noronha MS, Silva ML, et al. Prevalence profile of odontogenic cysts and tumors on Brazilian sample after the reclassification of odontogenic keratocyst. J Craniomaxillofac Surg. 2017;45:267–270. doi: 10.1016/j.jcms.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 12.Khosravi N, Razavi SM, Kowkabi M, Navabi AA. Demographic distribution of odontogenic cysts in Isfahan (Iran) over a 23-year period (1988–2010) Dent Res J (Isfahan) 2013;10:162–167. doi: 10.4103/1735-3327.113325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tekkesin MS, Olgac V, Aksakalli N, Alatli C. Odontogenic and nonodontogenic cysts in Istanbul: analysis of 5088 cases. Head Neck. 2012;34:852–855. doi: 10.1002/hed.21820. [DOI] [PubMed] [Google Scholar]
- 14.Sharifian MJ, Khalili M. Odontogenic cysts: a retrospective study of 1227 cases in an Iranian population from 1987 to 2007. J Oral Sci. 2011;53:361–367. doi: 10.2334/josnusd.53.361. [DOI] [PubMed] [Google Scholar]
- 15.Grossmann SM, Machado VC, Xavier GM, et al. Demographic profile of odontogenic and selected nonodontogenic cysts in a Brazilian population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e35–e41. doi: 10.1016/j.tripleo.2007.05.028. [DOI] [PubMed] [Google Scholar]
- 16.Ochsenius G, Escobar E, Godoy L, Peñafiel C. Odontogenic cysts: analysis of 2944 cases in Chile. Med Oral Patol Oral Cir Bucal. 2007;12:E85–E91. [PubMed] [Google Scholar]
- 17.Daley TD, Wysocki GP, Pringle GA. Relative incidence of odontogenic tumors and oral and jaw cysts in a Canadian population. Oral Surg Oral Med Oral Pathol. 1994;77:276–280. doi: 10.1016/0030-4220(94)90299-2. [DOI] [PubMed] [Google Scholar]
- 18.Chrcanovic BR, Gomez RS. Gingival cyst of the adult, lateral periodontal cyst, and botryoid odontogenic cyst: an updated systematic review. Oral Dis. 2017 doi: 10.1111/odi.12808. [DOI] [PubMed] [Google Scholar]
- 19.Chrcanovic BR, Gomez RS. Glandular odontogenic cyst: an updated analysis of 169 cases reported in the literature. Oral Dis. 2018;24:717–724. doi: 10.1111/odi.12719. [DOI] [PubMed] [Google Scholar]
- 20.MacDonald-Jankowski DS. Keratocystic odontogenic tumour: systematic review. Dentomaxillofac Radiol. 2011;40:1–23. doi: 10.1259/dmfr/29949053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bree AF, Shah MR, BCNS Colloquium Group Consensus statement from the first international colloquium on basal cell nevus syndrome (BCNS) Am J Med Genet A. 2011;155A:2091–2097. doi: 10.1002/ajmg.a.34128. [DOI] [PubMed] [Google Scholar]
- 22.Pastorino L, Pollio A, Pellacani G, et al. Novel PTCH1 mutations in patients with keratocystic odontogenic tumors screened for nevoid basal cell carcinoma (NBCC) syndrome. PLoS ONE. 2012;7:e43827. doi: 10.1371/journal.pone.0043827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Moraissi EA, Dahan AA, Alwadeai MS, et al. What surgical treatment has the lowest recurrence rate following the management of keratocystic odontogenic tumor?: a large systematic review and meta-analysis. J Craniomaxillofac Surg. 2017;45:131–144. doi: 10.1016/j.jcms.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 24.Macdonald-Jankowski DS. Orthokeratinized odontogenic cyst: a systematic review. Dentomaxillofac Radiol. 2010;39:455–467. doi: 10.1259/dmfr/19728573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Arruda JAA, Monteiro JLGC, Abreu LG, et al. Calcifying odontogenic cyst, dentinogenic ghost cell tumor, and ghost cell odontogenic carcinoma: a systematic review. J Oral Pathol Med. 2018 doi: 10.1111/jop.12727. [DOI] [PubMed] [Google Scholar]
- 26.Barros CCDS, Santos HBP, Cavalcante IL, et al. Clinical and histopathological features of nasopalatine duct cyst: a 47-year retrospective study and review of current concepts. J Craniomaxillofac Surg. 2018;46:264–268. doi: 10.1016/j.jcms.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 27.Vasconcelos R, de Aguiar MF, Castro W, de Araújo VC, Mesquita R. Retrospective analysis of 31 cases of nasopalatine duct cyst. Oral Dis. 1999;5:325–328. doi: 10.1111/j.1601-0825.1999.tb00098.x. [DOI] [PubMed] [Google Scholar]
- 28.Tsuneki M, Maruyama S, Yamazaki M, et al. Inflammatory histopathogenesis of nasopalatine duct cyst: a clinicopathological study of 41 cases. Oral Dis. 2013;19:415–424. doi: 10.1111/odi.12022. [DOI] [PubMed] [Google Scholar]
- 29.Motamedi MH, Behroozian A, Azizi T, et al. Assessment of 120 maxillofacial aneurysmal bone cysts: a nationwide quest to understand this enigma. J Oral Maxillofac Surg. 2014;72:1523–1530. doi: 10.1016/j.joms.2013.12.032. [DOI] [PubMed] [Google Scholar]
- 30.Perdigão PF, Silva EC, Sakurai E, et al. Idiopathic bone cavity: a clinical, radiographic, and histological study. Br J Oral Maxillofac Surg. 2003;41:407–409. doi: 10.1016/S0266-4356(03)00145-1. [DOI] [PubMed] [Google Scholar]
- 31.Chadwick JW, Alsufyani NA, Lam EW. Clinical and radiographic features of solitary and cemento-osseous dysplasia-associated simple bone cysts. Dentomaxillofac Radiol. 2011;40:230–235. doi: 10.1259/dmfr/16355120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peacock ME, Krishna R, Gustin JW, et al. Retrospective study on idiopathic bone cavity and its association with cementoosseous dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:e246-51. doi: 10.1016/j.oooo.2014.09.032. [DOI] [PubMed] [Google Scholar]
- 33.Philipsen HP, Reichart PA, Ogawa I, Suei Y, Takata T. The inflammatory paradental cyst: a critical review of 342 cases from a literature survey, including 17 new cases from the author’s files. J Oral Pathol Med. 2004;33:147–155. doi: 10.1111/j.0904-2512.2004.00139.x. [DOI] [PubMed] [Google Scholar]