Abstract
Dental implants have become an increasingly popular treatment choice for replacing missing teeth. Yet, little is known about the prevalence and sociodemographic distribution of dental implant use in the United States. To address this knowledge gap, we analyzed data from 7 National Health and Nutrition Examination Surveys from 1999 to 2016. We estimated dental implant prevalence among adults missing any teeth for each survey period overall as stratified by sociodemographic characteristics. We calculated absolute and relative differences from 1999–2000 to 2015–2016 and fit logistic regression models to estimate changes over time. We also used multivariable logistic regression to estimate independent associations of sociodemographic covariates with the presence of any implant. We projected the proportion of patients treated with dental implants into the year 2026 under varying assumptions of how the temporal trend would continue. There has been a large increase in the prevalence of dental implants, from 0.7% in 1999 to 2000 to 5.7% in 2015 to 2016. The largest absolute increase in prevalence (12.9%) was among individuals 65 to 74 y old, whereas the largest relative increase was ~1,000% among those 55 to 64 y old. There was an average covariate-adjusted increase in dental implant prevalence of 14% per year (95% CI, 11% to 18%). Having private insurance (vs. none or public insurance) or more than a high school education (vs. high school or less) was each associated with a 2-fold increase in prevalence, with an almost 13-fold (95% CI, 8 to21) increase for older adults. Dental implant prevalence projected to 2026 ranged from 5.7% in the most conservative scenario to 23% in the least. This study demonstrates that dental implant prevalence among US adults with missing teeth has substantially increased since 1999. Yet access overall is still very low, and prevalence was consistently higher among more advantaged groups.
Keywords: endosseous dental implantation, prevalence, National Health and Nutrition Examination Survey, projection, cross-sectional studies, dental care
Introduction
The concept of osseointegration was introduced nearly 50 y ago (Brånemark et al. 1969). Since then, implant dentistry has developed from an experimental invention to a successful and predictable treatment modality for replacing missing teeth (Buser et al. 2017). Dental implants have gained popularity because, in contrast to other treatment modalities, they preserve adjacent tooth structure and bone (Jivraj and Chee 2006; Battle-Siatita et al. 2009). Moreover, implant rehabilitation for patients who are edentulous and partially edentulous reportedly enhances masticatory function and quality of life (Tang et al. 1999; Jofre et al. 2013; Hartlev et al. 2014). Therefore, dental implants have become an important treatment option for replacing missing teeth (Tarnow 2014; Buser et al. 2017).
Little is known about the prevalence of dental implant use among the US population (Alkan et al. 2018). There is a general impression that use of implants has been increasing, and market research indicates that the overall number of implants used has been increasing. What has not been documented is the temporal trend in the proportion of patients receiving implants when they are missing teeth. Evaluating current and future trends in the prevalence of implants is important for understanding potential health disparities in access to this treatment and could also assist in the allocation of health care resources. Therefore, the primary objective of this study was to describe trends in the prevalence of dental implants among adults in the United States from 1999 to 2016 and in the sociodemographic characteristics of implant recipients over time. The secondary objective was to project implant prevalence to the years 2021 and 2026 under several simple, realistic scenarios.
Materials and Methods
We analyzed data from the National Health and Nutrition Examination Survey (NHANES), conducted by the National Center for Health Statistics (Centers for Disease Control and Prevention 2017). NHANES is a cross-sectional stratified multistage probability-sampled survey of the civilian noninstitutionalized population of the United States, conducted annually beginning in 1999. NHANES surveys include information about participants’ racial/ethnic background, socioeconomic position, and health conditions. Participants also undergo clinical examination, including a detailed oral examination of tooth condition, tooth count, periodontal status, occlusion, dental treatment needs, and overall oral health status.
We used data from 7 NHANES surveys conducted between 1999 and 2016, excluding participants <18 y old and those without a dental examination (Centers for Disease Control and Prevention 2017). Regarding implant prevalence, all individuals missing ≥1 permanent teeth were eligible for analyses (N = 32,758).
The study outcome was the proportion of individuals receiving at least 1 dental implant—a whole-mouth binary outcome (any implant present or absent) derived from 32 tooth-level indicators of condition. We use the term implant prevalence in this study to indicate the number of individuals who have at least 1 dental implant among all of those with at least 1 missing tooth. We also created 2 indicators of implant location: by dental arch (maxilla or mandible) and by the position in the arch (anterior or posterior).
For sociodemographic variables, we categorized education into high school degree or less versus greater than a high school education and race into White versus non-White. Because NHANES assessed educational attainment only for adults aged ≥20 y, this was a further age restriction for analyses that included education. For comparability across surveys, we collapsed health insurance variables into 3 categories: private, public, and no insurance.
Statistical Analysis
We estimated the survey-weighted proportion of individuals receiving at least 1 implant for each survey period overall and stratified by sex, age, education, race, and insurance status, with 95% CIs. Additionally, we stratified implant prevalence by dental arch, location in the arch, and tooth position. We estimated changes in prevalence over time by calculating absolute and relative differences from 1999–2000 to 2015–2016. We also estimated the independent associations of each characteristic with the presence of any implant, in a survey-weighted multivariable logistic regression model that included NHANES year and participants’ age, sex, education level, race, and insurance type. We evaluated whether the temporal trend in implant prevalence was different according to these same characteristics by adding multiplicative interaction terms in separate models (e.g., sex × year or education × year).
Before projecting the proportion of people treated with implants 5 and 10 y out from the last NHANES data set, we compared the average annual change in log odds of having an implant between the unadjusted and covariate-adjusted models, and the difference was negligible. Because there was little evidence of confounding by sociodemographic factors, including age, we used unadjusted logistic regression models to regress presence of any implant versus year. After fitting the model, we added new observations for the years 2021 and 2026 and derived predicted values (and corresponding 95% prediction interval; StataCorp 2013; Inlow 2018) for all years. To vary assumptions about how the temporal trend would be predicted to continue into the years 2021 and 2026, we proposed 4 simple scenarios. Specifically, we assumed that the increase in implant prevalence would 1) stop, 2) slow, 3) continue at the same pace, or 4) continue at an increased pace. We operationalized these assumptions by varying which years were included in the model fitting. For all 4 scenarios, we used logistic regression to regress the presence of any implant versus year. For the first scenario, we assumed that the proportion of eligible patients with any implant would remain the same as the fitted value (i.e., average probability estimated by the regression line for all years) in 2015 to 2016. For the other 3 scenarios, we predicted the future prevalence based on the slope of the regression line, using all years from 2000 to 2016 for scenario 2, excluding 2015 to 2016 in scenario 3 (in case it was aberrantly high), and excluding 1999 to 2000 and 2001 to 2002 in scenario 4 (because the proportion with implants did not really start taking off until 2003 to 2004 or later). We plotted all observed percentages, fitted percentages, and projected percentages over time (in years). Because we did not adjust these models for covariates, the projected populations are assumed to have similar population distributions by age, insurance type, and so on. We know that this assumption may not be true. However, we picked several otherwise realistic scenarios that provide a range of rough estimates for implant use through 2026. The least realistic scenario is also the most conservative, predicting that the increase in prevalence of implants might abruptly stop.
We used survey weights to account for the complex survey design in making population inferences. We analyzed the data with STATA 13 (StataCorp 2013). This study was reviewed by the institutional review board of the Harvard T.H. Chan School of Public Health and determined to be “not-human subjects research” since the data are publicly available and de-identified.
Results
Among US adults aged ⩾18 y in this study, 32,758 had at least 1 missing tooth, and 618 had at least 1 implant (Table 1). The majority of that sample were women (56%) and had received greater than a high school education (77%). Twenty-eight percent were in the age category of 65 to 77 y; most were White (80%); and around 54% had private health insurance. Compared with these distributions, adults with missing teeth but without implants had a slightly lower proportion of women and a much lower proportion of those who had greater than a high school education (59%), were White (70%), and had health insurance (public + private: 83% vs. 95%).
Table 1.
Demographic Characteristics of Adults with Missing Teeth: National Health and Nutrition Examination Survey (1999 to 2016).
| Population-Weighted Proportions (95% CI) |
||
|---|---|---|
| Variable | With Implants (n = 618) | Without Implants (n = 32,140) |
| Sex | ||
| Male | 44.1 (39.3 to 49.0) | 47.7 (47.1 to 48.2) |
| Female | 55.9 (51.0 to 60.7) | 52.3 (51.8 to 52.9) |
| Age, y | ||
| 18 to 34 | 6.4 (4.4 to 9.3) | 28.2 (27.0 to 29.4) |
| 35 to 44 | 9.1 (6.6,12.5) | 19.5 (18.6 to 20.4) |
| 45 to 54 | 21.2 (16.7 to 26.5) | 19.5 (18.7 to 20.3) |
| 55 to 64 | 23.8 (19.6 to 28.6) | 15.1 (14.4,15.8) |
| 65 to 74 | 28.1 (23.9 to 32.6) | 10.2 (9.8,10.7) |
| ≥75 | 11.4 (9.1 to 14.1) | 7.6 (7.1 to 8.1) |
| Educationa | ||
| High school or less | 23.5 (19.3 to 28.4) | 40.9 (39.3 to 42.6) |
| More than high school | 76.5 (71.6 to 80.7) | 59.1 (57.4 to 60.7) |
| Race | ||
| White | 79.6 (75.3 to 83.3) | 69.6 (67.1 to 72.0) |
| Non-White | 20.4 (16.7 to 24.7) | 30.4 (28.0 to 32.9) |
| Health insurance | ||
| No insurance | 5.2 (3.6 to 7.6) | 17.5 (16.6 to 18.5) |
| Private insurance | 53.9 (48.2 to 59.5) | 56.2 (54.8 to 57.6) |
| Public insurance | 40.8 (35.5 to 46.3) | 26.3 (25.3 to 27.3) |
All estimates are based on individuals aged ≥18 y except for education, which is based on those aged ≥20 y.
There has been a substantial increase in the proportion of individuals receiving implants in the United States. From 1999 to 2000, the prevalence of implants among adults missing at least 1 tooth was 0.7% (95% CI = 0.4% to 1.2%). A pronounced increase in prevalence was not seen until 2009 to 2010 (1.9%, 95% CI = 1.4% to 2.5%), and the prevalence was 5.7% (95% CI = 4.1% to 7.7%) from 2015 to 2016. A similar increasing trend did occur across all sociodemographic variables examined, including sex, age, education, race, and health insurance (Table 2). Since 1999, the largest absolute increase (12.9%) in implant prevalence was among those 65 to 74 y old, while the largest relative increase was 1,034% among those 55 to 64 y old.
Table 2.
Prevalence of Implants among Adults Who Have at Least 1 Missing Tooth: National Health and Nutrition Examination Survey (1999 to 2016).
| Population-Weighted Proportions (95% CI) |
Trenda |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total (N = 32,758) | 1999 to 2000 (n = 4,312) | 2001 to 2002 (n = 4,802) | 2003 to 2004 (n = 4,483) | 2009 to 2010 (n = 4,153) | 2011 to 2012 (n = 4,790) | 2013 to 2014 (n = 5,142) | 2015 to 2016 (n = 5,076) | Absolute | Relative | |
| Total sample | 2.4 (2.0 to 2.8) | 0.7 (0.4 to 1.2) | 0.9 (0.5 to 1.5) | 0.9 (0.5 to 1.5) | 1.9 (1.4 to 2.5) | 2.3 (1.5 to 3.5) | 3.3 (2.5 to 4.5) | 5.7 (4.1 to 7.7) | 5.0 | 738.2 |
| Sex | ||||||||||
| Male | 2.2 (1.8 to 2.7) | 0.7 (0.3 to 1.5) | 0.8 (0.5 to 1.6) | 0.8 (0.4 to 1.7) | 2.1 (1.5 to 2.9) | 2.0 (1.1 to 3.3) | 2.6 (1.9 to 3.7) | 5.5 (3.7 to 8.2) | 4.8 | 733.3 |
| Female | 2.5 (2.1 to 3.0) | 0.7 (0.3 to 1.6) | 0.9 (0.4 to 1.8) | 1.0 (0.4 to 2.1) | 1.7 (0.9 to 2.9) | 2.6 (1.6 to 4.2) | 4.0 (2.8 to 5.6) | 5.8 (4.2 to 7.9) | 5.1 | 728.6 |
| Age, y | ||||||||||
| 18 to 34 | 0.5 (0.4 to 0.8) | 0.2 (0.0 to 1.3) | 0.3 (0.1 to 1.6) | 0.4 (0.1 to 1.6) | 0.8 (0.2 to 3.9) | 0.4 (0.1 to 1.2) | 0.6 (0.2 to 1.8) | 1.3 (0.7 to 2.3) | 1.1 | 712.5 |
| 35 to 44 | 1.1 (0.8 to 1.6) | 0.8 (0.2 to 3.2) | 0.4 (0.1 to 1.8) | 0.7 (0.2 to 2.1) | 0.9 (0.4 to 2.0) | 0.6 (0.2 to 1.3) | 1.3 (0.6 to 2.9) | 3.3 (1.8 to 6.1) | 2.5 | 297.6 |
| 45 to 54 | 2.6 (1.9 to 3.5) | 0.8 (0.2 to 2.8) | 1.2 (0.5 to 3.1) | 1.0 (0.3 to 3.4) | 2.8 (1.6 to 4.9) | 2.7 (1.5 to 4.8) | 2.9 (1.3 to 6.5) | 6.1 (3.1 to 11.7) | 5.3 | 643.9 |
| 55 to 64 | 3.7 (2.9 to 4.7) | 0.7 (0.1 to 3.1) | 1.7 (0.8 to 3.4) | 1.2 (0.4 to 3.2) | 1.8 (0.8 to 4.1) | 3.5 (1.7 to 7.1) | 5.9 (3.8 to 9.0) | 7.6 (5.0 to 11.2) | 6.9 | 1,034.3 |
| 65 to 74 | 6.2 (5.0 to 7.7) | 1.3 (0.5 to 3.3) | 1.0 (0.3 to 3.2) | 2.5 (1.1 to 5.4) | 2.9 (1.5 to 5.8) | 5.7 (2.8 to 11.2) | 9.3 (7.2 to 12.1) | 14.2 (10.1 to 19.7) | 12.9 | 967.7 |
| ≥75 | 3.5 (2.8 to 4.4) | 1.5 (0.6 to 3.6) | 1.8 (0.8 to 4.4) | 0.8 (0.3 to 2.4) | 2.4 (1.3 to 4.4) | 5.0 (2.7 to 8.9) | 4.6 (2.6 to 7.8) | 6.6 (4.3 to 10.0) | 5.1 | 352.1 |
| Education b | ||||||||||
| ≤High school | 1.4 (1.1 to 1.8) | 0.8 (0.3 to 1.8) | 0.5 (0.2 to 1.3) | 0.9 (0.5 to 1.6) | 1.3 (0.9 to 1.7) | 1.6 (0.9 to 2.8) | 1.6 (0.8 to 3.1) | 3.4 (2.0 to 5.8) | 2.6 | 347.4 |
| >High school | 3.1 (2.6 to 3.7) | 0.7 (0.4 to 1.1) | 1.2 (0.6 to 2.1) | 1.0 (0.5 to 2.1) | 2.4 (1.6 to 3.7) | 2.8 (1.8 to 4.5) | 4.5 (3.5 to 5.8) | 7.0 (5.2 to 9.3) | 6.4 | 976.9 |
| Race | ||||||||||
| White | 2.7 (2.2 to 3.2) | 0.8 (0.4 to 1.4) | 1.0 (0.5 to 1.8) | 1.1 (0.7 to 1.9) | 1.9 (1.3 to 2.9) | 2.6 (1.6 to 4.3) | 4.1 (3.0 to 5.6) | 6.7 (4.7 to 9.4) | 6.0 | 793.3 |
| Non-White | 1.6 (1.3 to 2.0) | 0.5 (0.1 to 2.0) | 0.6 (0.2 to 1.5) | 0.2 (0.0 to 1.0) | 1.7 (1.3 to 2.3) | 1.6 (1.2 to 2.1) | 1.6 (1.1 to 2.6) | 3.8 (2.5 to 5.7) | 3.3 | 660.0 |
| Health insurance | ||||||||||
| No insurance | 0.7 (0.5 to 1.1) | 0.5 (0.1 to 2.2) | 0.5 (0.1 to 1.7) | 0 | 1.2 (0.5 to 2.6) | 0.5 (0.2 to 1.2) | 1.1 (0.4 to 2.9) | 1.3 (0.5 to 3.2) | 0.8 | 160.0 |
| Private | 2.3 (1.9 to 2.7) | 0.7 (0.2 to 1.7) | 1.0 (0.5 to 1.8) | 1.1 (0.6 to 2.0) | 2.0 (1.3 to 3.1) | 2.2 (1.4 to 3.5) | 3.4 (2.3 to 5.0) | 5.2 (3.5 to 7.7) | 4.5 | 642.9 |
| Public | 3.6 (3.0 to 4.4) | 0.8 (0.3 to 2.0) | 0.8 (0.3 to 2.1) | 1.1 (0.6 to 2.0) | 2.2 (1.6 to 3.2) | 3.9 (2.1 to 7.0) | 4.8 (3.7 to 6.1) | 8.5 (6.1 to 11.7) | 7.7 | 962.5 |
Absolute and relative increase in the prevalence of implants between 1999 to 2000 and 2015 to 2016.
All estimates are based on individuals aged ≥18 y except for education, which is based on those aged ≥20 y.
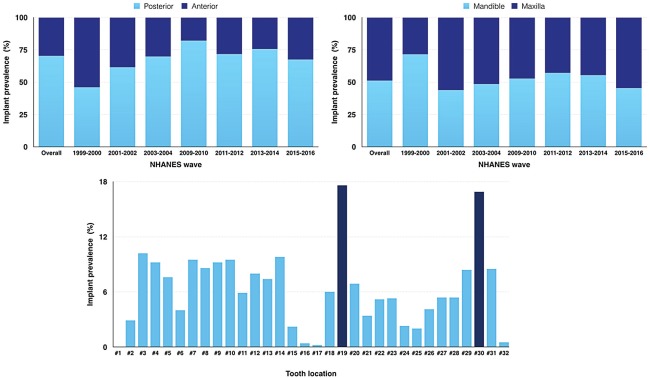
Roughly half the implants were placed in the mandible (51%, 95% CI = 45% to 57%) and half in the maxilla (49%, 95% CI = 43% to 55%), although the percentage placed in the mandible was at times slightly higher or lower than 50% depending on the survey year (Fig. 1). Additionally, most implants were placed in posterior sites, except for 1999 to 2000, when nearly 54% (95% CI = 32% to 75%) were placed in anterior sites. When stratified by site, the most common tooth to be replaced by an implant was number 19 (18%, 95% CI = 14% to 22%) or number 30 (17%, 95% CI = 13% to 22%; Appendix).
Figure 1.
Implant distribution among adults with missing teeth and receiving implants per the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2016.
From 1999–2000 to 2015–2016, there was an average covariate-adjusted 14% increase in implant prevalence per year (95% CI = 11% to 18%) (Table 3). Independent of the temporal trend, specific characteristics were associated with greater implant use, including almost a 13-fold increase in implant prevalence for older adults (65 to 74 y) as compared with younger adults (18 to 34 y) (95% CI = 8 to 21). In addition, having private insurance and greater than a high school education was each associated with a 2-fold increase in implant prevalence. No subgroup differences in trend met significance thresholds of P < 0.05 (not shown). Descriptively, among age groups, the temporal trend was much stronger for people 65 to 74 y, and there was a much slower increase in implant prevalence among those with no medical insurance versus those with public or private insurance, as well as among people with a high school education or less versus those having greater than a high school education (Appendix Fig).
Table 3.
Associations of Sociodemographic Variables with Implant Prevalence Among Adults with Missing Teeth: National Health and Nutrition Examination Survey (1999 to 2016).
| Odds Ratio | 95% CI | P Value | |
|---|---|---|---|
| Year | 1.14 | 1.11 to 1.18 | ≤0.005 |
| Sex | |||
| Male | Reference | ||
| Female | 1.1 | 0.9 to 1.4 | 0.439 |
| Age, y | |||
| 18 to 34 | Reference | ||
| 35 to 44 | 2.1 | 1.1 to 3.7 | 0.018 |
| 45 to 54 | 4.5 | 2.8 to 7.3 | ≤0.005 |
| 55 to 64 | 6.0 | 3.7 to 9.7 | ≤0.005 |
| 65 to 74 | 13.4 | 8.4 to 21.4 | ≤0.005 |
| ≥75 | 8.2 | 5.0 to 13.6 | ≤0.005 |
| Education | |||
| ≤High school | Reference | ||
| >High school | 1.9 | 1.5 to 2.6 | ≤0.005 |
| Race | |||
| Non-White | Reference | ||
| White | 1.2 | 0.9 to 1.5 | 0.154 |
| Health insurance | |||
| No insurance | Reference | ||
| Private insurance | 2.0 | 1.3 to 3.1 | 0.002 |
| Public insurance | 1.4 | 0.8 to 2.3 | 0.185 |
Survey-weighted multivariable logistic regression model included survey year and participant’s age, sex, education level, race, and insurance type. Survey waves included 1999 to 2000, 2001 to 2002, 2003 to 2004, 2009 to 2010, 2011 to 2012, 2013 to 2014, and 2015 to 2016.
In only the most conservative scenario would dental implant prevalence projected to the year 2026 be <10% (Fig. 2). If the trend continues at the current pace, a jump from 5.7% to 17% can be expected by 2026 (95% CI = 11% to 27%). If the trend steepens, prevalence could reach 23% (95% CI = 13% to 39%).
Figure 2.
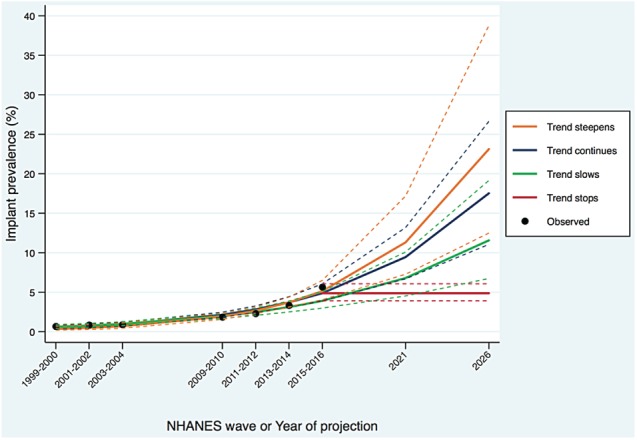
Observed, predicted, and projected implant prevalence among adults with missing teeth in the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2016 and projected to 2021 and 2026. Estimates are from survey-weighted multivariable logistic regression models. For projection scenario 1) trend stops: implant prevalence is estimated to be the same average probability estimated by the regression line in 2015-2016; 2) trend continues at the same pace: the slope of the regression line included all years 2000-2016; 3) trend slows: the slope of the regression line included all years excluding 2015-2016; and 4) trend steepens: the slope of the regression line included all years excluding 1999-2000 and 2001-2002. Solid lines represent the estimated prevalence (for 2016 and earlier) and projected prevalence (after 2016), and dashed lines represent the 95% prediction intervals for those estimates.
Discussion
To our knowledge, this is the first report to describe and project population trends in the prevalence of dental implants in the United States. We used nationally representative data to describe the prevalence of dental implants among adults missing at least 1 tooth, as well as associations with sociodemographic characteristics. There was a large increase in the prevalence of dental implants from 1999 to 2016. Although this trend was generally observed for all sociodemographic indicators in this study, it was most pronounced among older adults and was much slower to change among adults without health insurance or with only a high school education or less.
Across years, adults with higher than a high school education and of White race were more likely to have received dental implants. There was also a wide gap in implant prevalence between adults with and without health insurance. A major barrier for receiving dental implants is the high cost (Zimmer et al. 1992; Christensen 2012). In the United States, public insurance does not cover dental implants, and depending on the dental plan, private insurance may cover only part of the total cost. Additionally, the lack of availability of dentists with sufficient implant training (Christensen 2012) and patients’ knowledge about this treatment option may be contributing to this disparity (Deeb et al. 2017).
These results highlight the increased adoption of dental implants in the current treatment of missing teeth; growth that has been fueled in part by scientific advances in the field of implant dentistry (Buser et al. 2017). Very few studies have been designed to examine trends in the prevalence or use of dental implants. However, there is a growing body of literature regarding specific aspects of dental implant use, such as implant design, material, and clinical behavior, that suggests an increase in implant utilization (Annibali et al. 2012; Papaspyridakos et al. 2012; Pieralli et al. 2017). Marketing research has also indicated that the overall number of implants sold has been increasing and that market share in North America is less than that of other regions of the world—as compared with, for example, Europe, which dominated the market in 2016 (Grand View Research, Inc. 2018). Our analysis complements the market research in that we examined trends in the prevalence of the use of implants among US patients who appear to be eligible to receive them. The results highlight not only a health disparity but also a gap in market penetration.
Although, in general, the risk of losing teeth has decreased over the last few decades (Wu et al. 2014), the US population is aging. These factors will likely combine such that the demand for dental implants will continue to rise in the next decade. If the observed trend continues at an average rate similar to that observed since 2003 to 2004, projection models suggest that among adults missing teeth, the prevalence of dental implant use could reach as high as 23% by the year 2026.
We used a simplified projection approach, and the results must be interpreted accordingly. The goal of the prediction was simply to document the average change in prevalence of implant over time. Thus, we did not adjust these regression models for underlying characteristics of the population that have changed over time and will continue to change (Muller and MacLehose 2014). The most obvious expected demographic trend, as mentioned, is the continued aging of the population, and because the risk of tooth loss increases with age, we may have underestimated implant prevalence projected to 2026. Nevertheless, the covariate-adjusted (including age adjustment) and unadjusted models differed only negligibly in the estimated average rate of change in prevalence per year. This suggests that, though clearly related to implant use, age did not confound the temporal trend, supporting the use and interpretability of the unadjusted regression approach.
In future work, we will build on this preliminary evidence by developing more rigorous cost-benefit analyses under different assumptions about demographic and clinical trends. We will also factor in the number of missing teeth and number of dental implants rather than using a simple prevalence estimate, which serves as an indicator of access. Although one might expect each patient’s probability of any dental implants to increase with the number of missing teeth, the distribution of tooth loss itself is highly sociodemographically skewed.
Another source of possible underestimation of implant prevalence is that we included adults missing any teeth, including third molars. Although third molars are rarely replaced, initial descriptive analyses indicated that close to 1% of all dental implants in this study were placed at the third molar location; thus, we included them in the analysis.
Tooth loss affects about 52% of adults in the United States (Dye et al. 2015). Despite an overall decrease in its prevalence, tooth loss remains a prevalent dental condition that is unequally distributed among the population. Disparities by sociodemographic status have been documented, and adults from disadvantaged groups consistently experience a greater burden of this condition (Cunha-Cruz et al. 2007; Elani et al. 2012; Peres et al. 2015; Elani et al. 2017). Tooth loss negatively affects chewing ability, quality of life, and aesthetics, and the extent of this impact depends on the number of missing teeth and their location (Sheiham and Steele 2001; Gerritsen et al. 2010). Options for dental treatments to replace missing teeth vary depending on the severity of tooth loss, the condition of remaining teeth, alveolar ridge condition, patients’ financial ability, and providers’ expertise. Among the various treatment options, including traditional fixed and removable prostheses, dental implants have become the most desirable treatment due to their functional and aesthetic advantages (Tarnow 2014; Buser et al. 2017). However, our findings document similar persistent disparities for receiving implant treatment. Thus, disadvantaged groups are most vulnerable to having missing teeth and also appear to lack access to this emerging dental treatment option.
According to this study, only 6% of adults benefited from the advantages of tooth replacement with dental implants as recently as 2016. Further efforts should be made to better understand the factors associated with this disparity and to ensure that a larger portion of the population has access to dental implant treatment.
Conclusion
Based on nationally representative data, this study demonstrates that dental implant prevalence among US adults has substantially increased since 1999. This trend was not uniform across sociodemographic indicators examined; implant prevalence was consistently higher among more advantaged groups. A range of reasonable projection estimates suggest that dental implant prevalence could be as high as 23% by 2026. These findings provide valuable information for workforce development and for the implant industry to allocate resources for the anticipated future demand among patients eligible for implant treatment yet not receiving it.
Author Contributions
H.W. Elani, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; J.D. Da Silva, G.O. Gallucci, contributed to conception, design, and data interpretation, critically revised the manuscript; J.R. Starr, contributed to conception, design, data analysis, and interpretation, drafted and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Supplemental Material
Supplemental material, DS_10.1177_0022034518792567 for Trends in Dental Implant Use in the U.S., 1999–2016, and Projections to 2026 by H.W. Elani, J.R. Starr, J.D. Da Silva and G.O. Gallucci in Journal of Dental Research
Footnotes
A supplemental appendix to this article is available online.
This work was conducted with support from Harvard Catalyst, the Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health award UL1 TR001102), and financial contributions from Harvard University and its affiliated academic health care centers.
The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, or the National Institutes of Health.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Alkan EA, Mau LP, Schoolfield J, Guest GF, Cochran DL. 2018. Prevalence of dental implants and evaluation of peri-implant bone levels in patients presenting to a dental school: a radiographic cross-sectional 2-year study. Int J Oral Maxillofac Implants. 33(1):145–151. [DOI] [PubMed] [Google Scholar]
- Annibali S, Cristalli MP, Dell’Aquila D, Bignozzi I, La Monaca G, Pilloni A. 2012. Short dental implants: a systematic review. J Dent Res. 91(1):25–32. [DOI] [PubMed] [Google Scholar]
- Battle-Siatita SO, Bartoloni JA, Hancock RH, Chong CH. 2009. Retrospective analysis of dental implants among United States Air Force basic military trainees. Mil Med. 174(4):437–440. [DOI] [PubMed] [Google Scholar]
- Brånemark PI, Adell R, Breine U, Hansson BO, Lindström J, Ohlsson A. 1969. Intra-osseous anchorage of dental prostheses: I. Experimental studies. Scand J Plast Reconstr Surg. 3(2):81–100. [DOI] [PubMed] [Google Scholar]
- Buser D, Sennerby L, De Bruyn H. 2017. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol 2000. 73(1):7–21. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2017. National Health and Nutrition Examination Survey; [accessed 2017 Jan 1]. https://www.cdc.gov/nchs/nhanes/index.htm.
- Christensen GJ. 2012. Why are dental implants not used more in the United States? J Am Dent Assoc. 143(8):903–905. [DOI] [PubMed] [Google Scholar]
- Cunha-Cruz J, Hujoel PP, Nadanovsky P. 2007. Secular trends in socio-economic disparities in edentulism: USA, 1972–2001. J Dent Res. 86(2):131–136. [DOI] [PubMed] [Google Scholar]
- Deeb G, Wheeler B, Jones M, Carrico C, Laskin D, Deeb JG. 2017. Public and patient knowledge about dental implants. J Oral Maxillofac Surg. 75(7):1387–1391. [DOI] [PubMed] [Google Scholar]
- Dye BA, Thornton-Evans G, Li X, Iafolla TJ. 2015. Dental caries and tooth loss in adults in the United States, 2011–2012. Hyattsville, MD: US Department of Health and Human Services. [Google Scholar]
- Elani HW, Harper S, Allison PJ, Bedos C, Kaufman JS. 2012. Socio-economic inequalities and oral health in Canada and the United States. J Dent Res. 91(9):865–870. [DOI] [PubMed] [Google Scholar]
- Elani HW, Harper S, Thomson WM, Espinoza IL, Mejia GC, Ju X, Jamieson LM, Kawachi I, Kaufman JS. 2017. Social inequalities in tooth loss: a multinational comparison. Community Dent Oral Epidemiol. 45(3):266–274. [DOI] [PubMed] [Google Scholar]
- Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. 2010. Tooth loss and oral health–related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes. 8:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grand View Research, Inc. 2018. Dental implants market size, share and trends analysis report by product (titanium implants, zirconium implants), by region (North America, Europe, Asia Pacific, Latin America, MEA), and segment forecasts, 2018–2024; [accessed 2018 Jul 13]. https://www.grandviewresearch.com/industry-analysis/dental-implants-market
- Hartlev J, Kohberg P, Ahlmann S, Andersen NT, Schou S, Isidor F. 2014. Patient satisfaction and esthetic outcome after immediate placement and provisionalization of single-tooth implants involving a definitive individual abutment. Clin Oral Implants Res. 25(11):1245–1250. [DOI] [PubMed] [Google Scholar]
- Inlow M. 2018. Prediction confidence intervals after logistic regression. StataCorp; [accessed 2018 Jul 13]. https://www.stata.com/support/faqs/statistics/prediction-confidence-intervals/.
- Jivraj S, Chee W. 2006. Rationale for dental implants. Br Dent J. 200(12):661–665. [DOI] [PubMed] [Google Scholar]
- Jofre J, Castiglioni X, Lobos CA. 2013. Influence of minimally invasive implant-retained overdenture on patients’ quality of life: a randomized clinical trial. Clin Oral Implants Res. 24(10):1173–1177. [DOI] [PubMed] [Google Scholar]
- Muller CJ, MacLehose RF. 2014. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 43(3):962–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. 2012. Success criteria in implant dentistry: a systematic review. J Dent Res. 91(3):242–248. [DOI] [PubMed] [Google Scholar]
- Peres MA, Luzzi L, Peres KG, Sabbah W, Antunes JL, Do LG. 2015. Income-related inequalities in inadequate dentition over time in Australia, Brazil and USA adults. Community Dent Oral Epidemiol. 43(3):217–225. [DOI] [PubMed] [Google Scholar]
- Pieralli S, Kohal RJ, Jung RE, Vach K, Spies BC. 2017. Clinical outcomes of zirconia dental implants: a systematic review. J Dent Res. 96(1):38–46. [DOI] [PubMed] [Google Scholar]
- Sheiham A, Steele J. 2001. Does the condition of the mouth and teeth affect the ability to eat certain foods, nutrient and dietary intake and nutritional status amongst older people? Public Health Nutr. 4(3):797–803. [DOI] [PubMed] [Google Scholar]
- StataCorp. 2013. Stata statistical software: release 13. College Station (TX): StataCorp LP. [Google Scholar]
- Tang L, Lund JP, Tache R, Clokie CM, Feine JS. 1999. A within-subject comparison of mandibular long-bar and hybrid implant-supported prostheses: evaluation of masticatory function. J Dent Res. 78(9):1544–1553. [DOI] [PubMed] [Google Scholar]
- Tarnow DP. 2014. Commentary: replacing missing teeth with dental implants. A century of progress. J Periodontol. 85(11):1475–1477. [DOI] [PubMed] [Google Scholar]
- Wu B, Hybels C, Liang J, Landerman L, Plassman B. 2014. Social stratification and tooth loss among middle-aged and older Americans from 1988 to 2004. Community Dent Oral Epidemiol. 42(6):495–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmer CM, Zimmer WM, Williams J, Liesener J. 1992. Public awareness and acceptance of dental implants. Int J Oral Maxillofac Implants. 7(2):228–232. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_0022034518792567 for Trends in Dental Implant Use in the U.S., 1999–2016, and Projections to 2026 by H.W. Elani, J.R. Starr, J.D. Da Silva and G.O. Gallucci in Journal of Dental Research