Abstract
Introduction
Due to the increase in people who use opioids in the US, there has been a steady increase in injection drug use. Without access to safe syringe disposal locations, people who inject drugs (PWID) have few options other than improper disposal, including in public places. In 2016, Florida’s first legal Syringe Services Program (SSP) was established in Miami. This study aims to compare syringe disposal practices among PWID before and after the implementation of an SSP.
Methods
Visual inspection walkthroughs of randomly selected census blocks in the neighborhoods in the top quartile of narcotics-related arrests were conducted to assess improperly discarded syringes. Syringe location was geocoded in ArcGIS. Adult PWID pre-SSP (n=448) and post-SSP (n=482) implementation were recruited for a survey using respondent driven sampling in Miami. A Poisson regression model was used to determine the adjusted relative risk (aRR) of improper syringe disposal pre and post-SSP.
Results
A total of 191 syringes/1,000 blocks were found post-implementation versus 371/1,000 blocks pre-implementation, representing a 49% decrease after SSP implementation. In the surveys, 70% reported any improper syringe disposal post-SSP implementation versus 97% pre-SSP implementation. PWID in the post-implementation survey had 39% lower adjusted relative risk (aRR= 0.613; 95% CI=0.546, 0.689) of improper syringe disposal as compared to pre-implementation.
Conclusions
There was a significant decrease in the number of improperly discarded syringes in public in Miami after the implementation of an SSP. Providing PWID with proper disposal venues such as an SSP could decrease public disposal in other communities.
Keywords: HIV, opioids, PWID, Syringe Services Programs, Syringe Disposal
1. Introduction
In 2017, there were 38,739 people diagnosed with HIV in the United States (U.S.) (CDC, 2018). Over nine percent of those diagnoses were accounted for by people who inject drugs (PWID) (CDC, 2018). Furthermore, injection drug use is the most common transmission route of hepatitis C virus (HCV) transmission in the U.S. (CDC, 2018). From 2004 to 2014, the increasing incidence of acute HCV correlated to the corresponding rise in injection drug use during this time-period (Zibbell et al., 2018). It is well established that needle sharing among PWID is a major risk factor for contracting both HIV and HCV (CDC, 2018; CDC, 2018). However, needle-sticks from improperly disposed needles in public spaces rarely pose a viral transmission risk to community members. The annual incidence of community-acquired needle-stick injuries in the U.S. is estimated to be 2,000 per year with an annual cost of $9.8 million to the healthcare system (Jason et al, 2013; Papenburg et al., 2008; Slinger et al., 2000; Thompson et al., 2003) and unnecessary exposure of affected individuals to post-exposure prophylaxis. Despite this burden, there have been very few studies conducted detailing the role of various public health syringe disposal interventions in reducing the prevalence of improperly discarded syringes (Tookes et al, 2012; Wenger et al, 2011; Quinn et al, 2014).
Many public health interventions have been implemented in an effort to decrease the incidence of improper syringe disposal. These interventions include establishing Syringe Services Programs (SSPs) and overdose prevention sites, passing state legislation designating pharmacies as permissible sites for PWID to access and properly dispose of syringes, designating community syringe disposal sites (Riley et al., 1998), and providing PWID with sharps containers and education (Cleland et al., 2006; Gosden et al., 1975; Kinnard et al., 2014).
The current literature suggests SSPs are effective at reducing needle sharing among PWID and decreasing the risk of HIV and HCV infection (Abdul-Quader et al., 2013; Wodak and Cooney, 2006). Nationally, hospitalizations related to injection drug use have increased in recent years causing significant morbidity from life-threatening infectious diseases (e.g. endocarditis) and resulting in surging healthcare expenditures (Herzig et al, 2016; Feeishauer et al, 2017). Skin and soft tissue infections are common among PWID, especially those without adequate access to harm reduction supplies and education, and have also been increasing with the nationwide epidemic (Dahlman et al, 2015; Ciccarone et al, 2016); Dahlman et al, 2017; Smith et al, 2015). High risk injection practices are associated with increased risk of these preventable infections, emphasizing the need for programs that promote safe injection practices through education and provision of clean equipment (Dahlman et al, 2008; Philips et al, 2017).
By design, SSPs provide PWID access to clean syringes and proper syringe disposal. In one study, a city without an SSP (Miami, FL) was shown to have 8 times more improperly disposed needles than a city with multiple long-established SSPs (San Francisco, CA)(Tookes et al., 2012; Wenger et al., 2011). Furthermore, a recent study conducted in Los Angeles, CA, demonstrated that SSP utilization in the past 30 days was associated with decreased risk of improper syringe disposal whereas access to syringes from a pharmacy in the past 6 months was correlated with increased risk of improper syringe disposal (Quinn et al., 2014). In New York, NY, implementation of pharmacy sales of syringes was not associated with an increased number of improperly discarded syringes in public (Fuller et al, 2002).
Miami-Dade County, Florida, continues to have the highest incidence of new HIV infections nationwide (2018). In response to reports of improperly discarded syringes in Miami, high healthcare expenditures related to injection drug use at the county safety-net hospital, increasing incidence of HIV, and surging number of opioid-caused deaths, the Florida Legislature passed the Infectious Disease Elimination Act, authorizing Florida’s first legal SSP in July of 2016 (Tookes et al., 2015; Tookes et al., 2012).
Prior to this investigation, to our knowledge, there have been few studies in a major U.S. city analyzing the changes in syringe disposal among PWID before and after the implementation of an SSP (Bluthenthal et al., 2007; Broadhead and Heckathorn, 1999; Doherty et al., 1997; Doherty et al., 2000; Quinn et al., 2014). This study compares the prevalence of improperly disposed syringes in public spaces and self-reported syringe disposal among PWID in Miami, before (2009) and after (2018) the implementation of an SSP.
2. Materials and Methods
We conducted a serial cross-sectional study, replicating the methods from Tookes et al 2012, to assess the differences between Miami in 2009 (pre-SSP) and Miami in 2018 (post-SSP). Visual inspection walkthroughs of Miami were conducted alongside structured interviews of PWID as part of the Center for Disease Control’s National HIV Behavioral Surveillance (NHBS). Data were collected June to December of 2018 and compared to the previously published results of Miami in 200914.
2.1. Visual Inspection Walkthroughs
Following the same methodological approach as Tookes et al 2012, visual inspection walkthroughs were conducted among the census block groups with the highest quartile number of narcotics-related arrests. Data provided by the Miami Police Department was mapped using ArcGIS Software (version 10.2; Redlands, CA). From the top quartile of census block groups, we randomly selected 775 census blocks for visual inspection walkthroughs. All four sides of each census block were inspected for improperly discarded syringes. Visual inspections were conducted in all publicly accessible areas, including sidewalks, alleys, parks and parking lots. All syringes that were found during the walkthroughs were photographed and geocoded via mobile phone in ArcGIS. Walkthroughs occurred from July to December of 2009 and August to December of 2018.
2.2. Quantitative Surveys of PWID
To examine the differences in syringe disposal practices among PWID, we conducted surveys of PWID in Miami at two time points pre and post SSP implementation (N=448 in 2009 and N=482 in 2018). As part of NHBS, respondent-driven sampling (RDS) was used to recruit participants. RDS has been shown to be an effective strategy for the recruitment of hidden populations involved in illegal behaviors (Lansky et al., 2007; Magnani et al., 2005; Malekinejad et al., 2008; Malekinejad et al., 2011). Eligibility criteria included: (1) age 18 years or older; (2) injection of illicit drugs within the previous 12 months; and (3) informed consent. All data were collected via face-to-face interview and recorded electronically on a handheld assisted personal interviewing tablet computer. The interview application was developed using Questionnaire Development System software (QDS™ Version 2.6.1, NOVA Research Company, Bethesda, Maryland).
2.3. Ethics Statement
The visual inspection walkthroughs were exempt from human subjects research. The quantitative surveys were approved by the Institutional Review Boards at the University of Miami (IRB#20170527) and the Florida Department of Health (IRB#2017-20-FDOH).
2.4. Measures
To compare results pre and post SSP implementation, we used the same syringe disposal measures that had been developed in Miami in 2009 (Tookes et al 2012). This included asking how many syringes in the past 30 days had been disposed of (a) in a public place, (b) by selling or giving away, (c) in the trash, (d) at an SSP, (e) at a hospital/clinic, (f) at a pharmacy, (g) in a sharps container, or (h) other place. The main outcome variable was improper syringe disposal, which is defined as having disposed of a syringe in a public place, by selling them or giving them away, by putting them in the trash at home or another’s home, in the sewer, or by flushing.
The outcome variable combined the counts of the improper methods of syringe disposal by summing them. Then that variable was dichotomized into no improper syringe disposal (no improper disposal methods) and improper disposal (>1 improper disposal method reported).
2.5. Statistical Analyses
2.5.1. Visual Inspection Walkthroughs
The number of syringes found in Miami in 2018 was standardized per 1,000 census blocks in the sample. We also standardized the number of syringes per 1,000 people living in the census blocks inspected.
2.5.2. Quantitative Survey of PWID
We compared demographic and individual syringe disposal location variables by pre and post-SSP implementation samples using chi-squared tests. Because the two samples were 9 years apart, it is not possible to use RDS-specific statistical methods (RDSAT). As such, the samples were not weighted to adjust for interdependence of study participants. A multivariable Poisson regression model with robust standard errors was used to assess the difference in self-reported improper disposal of syringes in 2009 and 2018, both unadjusted and adjusting for gender, race/ethnicity, ever HIV-positive, and currently homeless. Analyses were performed using SAS statistical software (Version 9.4; SAS Institute, Cary, NC). All tests were performed at a significance level of 0.05, and unadjusted (RR), adjusted relative risk ratios (aRR) and 95% confidence intervals (CI) were reported.
3. Results
3.1. Visual Inspection Walkthroughs and Syringe Density
There were a total of 149 syringes (191 per 1,000 census blocks) found in Miami in 2018 compared to 328 syringes (371 per 1,000 census blocks) found in Miami in 2009. This represents a 49% decrease in syringes found in public areas after the implementation of an SSP. The number of syringes found per 1,000 people decreased from 4.9 in 2009 to 1.2 in 2018, representing a 75% decrease post-SSP. The locations of the syringes that were found in Miami in 2009 and 2018 are presented in Figure 1. Each dot represents the location of an encountered syringe and can represent many syringes found within the census block.
Figure 1. Locations of Publicly Discarded Syringes.
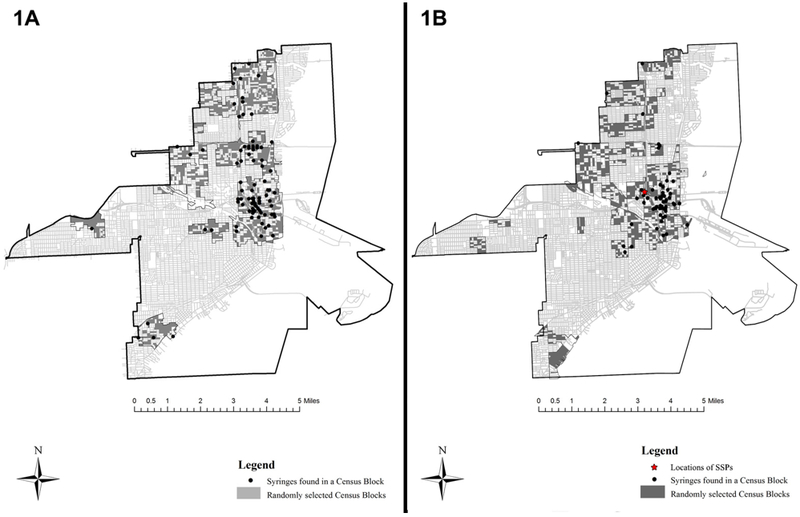
1A. Locations of found syringes in Miami, FL Pre-SSP (2009)
1B. Locations of found syringes in Miami, FL Post-SSP (2018)
3.2. Quantitative Surveys
The demographic and syringe disposal practices in 2009 and 2018 are presented in Table 1. The sample in 2018 was significantly more likely to be non-Hispanic White (29% vs. 23%, p=0.004), younger (49% younger than 40 vs. 28%, p<0.001) and to report current homelessness (84% vs. 50%, p<0.001).
Table 1.
Demographic Characteristics of People Who Inject Drugs in Miami 2009 and 2018 and Self-reported Syringe Disposal Locations in the Past 30 days
| Variable | Miami 2009 (n=448) |
Miami 2018 (n=482) |
p-value |
|---|---|---|---|
| Biological Sex | 0.766 | ||
| Male | 79% | 77% | |
| Female | 21% | 23% | |
| Intersex | 0% | 0% | |
| Race/ethnicity | 0.004 | ||
| White (Non-Hispanic) | 23% | 29% | |
| Black (Non-Hispanic) | 36% | 29% | |
| Hispanic | 40% | 39% | |
| Native American | 1% | 2% | |
| Asian or Pacific Islander | 1% | 1% | |
| Multiple Races/Other | 0% | 1% | |
| Age (years) | <0.001 | ||
| 18–29 | 8% | 17% | |
| 30–39 | 20% | 32% | |
| 40–49 | 31% | 25% | |
| 50+ | 41% | 26% | |
| Currently homeless | 50% | 84% | <0.001 |
| HIV-positive (self- report) | 10% | 11% | 0.788 |
| Syringe Disposal Locations | |||
| Public place | 68.7% | 49.1% | <0.001 |
| Selling/giving away | 12.6% | 23.3% | <0.001 |
| Trash | 66.2% | 31.3% | <0.001 |
| SSP | 0% | 38.6% | <0.001 |
| Hospital or clinic | 1.6% | 1.9% | 0.802 |
| Pharmacy | 0% | 0% | - |
| Sharps container | 3.8% | 15.4% | <0.001 |
| Other Location | 6.5% | 8.3% | 0.293 |
| Any improper disposal | 96.6% | 69.5% | <0.001 |
In bivariate analysis, PWID in 2018 were significantly less likely to report disposal of syringes in a public place (49.1% vs. 68.7%, p<0.001) and in the trash (31.3% vs. 66.2%, p<0.001) compared to PWID in 2009. After the establishment of the SSP, 38.6% PWID surveyed in 2018 reported syringe disposal at the SSP. Additionally, in 2018, PWID were significantly more likely to dispose of syringes in a sharps container (15.4% vs. 3.8%, p<0.001) and sell/give away syringes (23.3% vs. 12.6%, p<0.001) than in 2009. Overall, PWID in 2018 were significantly less likely to report any improper disposal of syringes (69.5% vs. 96.6%, p<0.001) than in 2009.
Of the total reported syringes disposed in the past 30 days, in 2018, 25.3% (7,960 of 31,412) were improperly disposed of compared to 94.9% (9,845 of 10,379) in 2009. In 2018, 17,914 (57%) and 5,029 (16%) syringes were disposed of in a SSP or sharps container, respectively, compared to 0 (0%) and 334 (3.2%) in 2009 (Table 2).
Table 2.
Number of Syringes Disposed in the Past 30 days as reported by People Who Inject Drugs in Miami Pre (2008) and Post (2018) implementation of SSP
| Disposal Location | Pre-SSP (%) | Post-SSP (%) |
|---|---|---|
| Public Place | 4,689 (45.2) | 4,095 (13.0) |
| Selling/giving away | 675 (6.5) | 1,301 (4.1) |
| Trash | 4,004 (38.6) | 2,356 (7.5) |
| Syringe Service Program | 0 (0.0) | 17,914 (57.0) |
| Hospital or clinic | 200 (1.9) | 128 (0.4) |
| Pharmacy | 0 (0.0) | 8 (0.03) |
| Sharps container | 334 (3.2) | 5,029 (16.0) |
| Sewer/manhole | 234 (2.2) | 0 (0) |
| Flush down the toilet | 163 (1.6) | 208 (0.7) |
| Other | 80 (0.8) | 373 (1.2) |
| Total syringes improperly disposed | 9,845 (94.9) | 7,960 (25.3) |
| Total syringes disposed | 10,379 | 31,412 |
In the multivariable Poisson regression (Table 3), after adjusting for gender, age, race/ethnicity, homelessness, and HIV-positive status, PWID in the post-implementation survey had 29.5% lower non-adjusted (RR= 0.705; 95% confidence interval [CI]=0.659, 0.755), and 39% lower adjusted (aRR= 0.613; 95% CI=0.546, 0.689) relative risk of improper syringe disposal as compared to PWID in the pre-implementation survey. The regression model also revealed that those reporting current homelessness had increased adjusted relative risk of improper syringe disposal (aRR=1.589, 95% CI: 1.400, 1.803).
Table 3.
Self-reported Improper Disposal of Syringes by People Who Inject Drugs in Miami (N=930)
| Variable | RR | 95% CI | aRR | 95% CI |
|---|---|---|---|---|
| Miami Pre vs Post-SSP | 0.705* | (0.66 – 0.755) | 0.61* | (0.545 – 0.69) |
| Male (vs Female) | 1.03 | (0.95 – 1.11) | 1.15 | (0.985 - 1.34) |
| Age (years) | 1.00 | (1.00 – 1.01) | 0.995 | (0.99 - 1.00) |
| Race/Ethnicity | ||||
| White (vs Black) | 0.88* | (0.81 – 0.96) | 0.89 | (0.76 - 1.05) |
| Other (vs Black) | 0.78 | (0.60 – 1.01) | 0.83 | (0.55 - 1.25) |
| Hispanic (vs Black) | 0.95 | (0.89 – 1.02) | 1.03 | (0.90 - 1.17) |
| Homeless | 1.04 | (0.975 – 1.11) | 1.59* | (1.40-1.80) |
| HIV Positive | 0.91 | (0.815 – 1.02) | 0.935 | (0.78 - 1.125) |
significant at p < 0.05
4. Discussion
This study provides comparative data assessing syringe disposal in a city before and after the implementation of an SSP both through visual inspection walkthroughs and a quantitative survey. There were almost half of the number of syringes found discarded publicly in Miami after SSP implementation, at a time when there is a national Public Health Emergency due to the opioid overdose crisis. Importantly, the quantitative survey corroborated these findings, with PWID in 2018 significantly less likely to report that they improperly disposed of syringes. Public awareness of the nationwide opioid overdose crisis and acceptance of opioid use disorder as a disease could have contributed to better syringe disposal practices, but the decrease in improperly discarded syringes in public despite increased opioid use suggests the importance of the SSP in providing a venue for proper syringe disposal.
While only 38.6% of respondents in 2018 reported having used the SSP, 57% of syringes disposed by all respondents in the prior 30 days were disposed at the SSP. This suggests that the SSP provides safe disposal for not just the PWID who use the program. PWID who go to SSPs often exchange syringes for PWID who do not go to SSPs, thus broadening the reach of SSPs (Lorvick et al., 2006). Additionally, the increase in syringe disposal in sharps containers is likely the result of widespread distribution of sharps containers at the SSP, suggesting that up to 73% percent of syringes were properly disposed in 2018 as a result of the SSP. Increasing the reach of the SSP through concerted mobile outreach in the areas identified with publicly discarded syringes should be prioritized in order to increase the number of syringes in circulation and simultaneously provide a venue for proper disposal (Iyengar et al., 2019; Kaplan and Heimer, 1994). This increased access to syringes has been shown to decrease syringe sharing and HIV infection among PWID (Bluthenthal et al., 2007). Importantly, visual inspection of blocks in Miami showed that there were 49% fewer improperly disposed syringes in public post-SSP implementation, despite the SSP’s distribution of 149,989 syringes in 2018. These results support the findings of Tookes et al (2012) that SSPs are a significant means of collecting of used syringes and do not increase the number of publicly discarded syringes.
Several potential limitations should be noted when interpreting the results of this study. First, the visual inspection study may have undercounted the number of publicly discarded syringes in 2018 because there may have been an increase in public works cleanup due to gentrification of parts of Miami. However, the visual inspection walkthroughs were not conducted in the same blocks during 2009 and 2018, but in the areas most affected by drug use at each point in time as reflected in Miami Police Department data. Furthermore, the survey data of PWID corroborated our visual inspection findings. Second, these findings may not generalize to all areas of the city or to other cities. Third, the results of the quantitative survey may have been impacted by social desirability or recall bias. However, it is important to note that these surveys were conducted as part of a Florida Department of Health and Centers for Disease Control surveillance, independent of the SSP or its staff. We conducted both quantitative surveys and walkthrough inspections in order to address the limitations of each individual study design.
5. Conclusion
There was a significant decrease in the number of improperly discarded syringes encountered through visual inspection of in Miami after the implementation of the SSP, a finding that was corroborated by quantitative surveys of PWID. Providing PWID proper disposal venues such as an SSP could decrease public syringe disposal in other communities where they are implemented, while also reducing syringe sharing and its attendant risks for HIV and viral hepatitis transmission.
6. Acknowledgements
This study was financially supported, in whole or in part, by the Florida Department of Health’s CDC National HIV Behavioral Surveillance (Grant# NU62PS005082-01-02) and the Consejo Nacional de Ciencia y Tecnología (CVU810654). We thank the following individuals for their contributions to this study: Raul Rodriguez, Donald Washington, Johann Amirali, Juan Carlos Díaz, Monica Faraldo, Abraham Parrish, Emelina Martinez, Edward Suárez Jr., Carlos Padrón, Jacqueline Wright, Leslie Molit, Sandy St. Hilaire, Carlos Dos Santos, Valerie Francillion, Paula Da Silva, Nobuyo Nakamura, Nicole Martuscelli, Kelly Ann Conley, Hardik Patel, Kasha Bornstein, Austin Coye, Margaret Ginoza, Megan Nocita, Catherine Johnson, Alexander Moskowitz, Daniel Beckerman, Samantha Grutzner, Shannon Wagner, Lily Ostrer, Abraham Parrish, Jorge Quintanela.
Funding: This study was supported by the Florida Department of Health’s CDC National HIV Behavioral Surveillance (Grant# NU62PS005082-01-02) and the Consejo Nacional de Ciencia y Tecnología (CVU810654).
References
- Centers for Disease Control and Prevention. HIV Surveillance Report, 2017; vol. 29 http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2018. [Google Scholar]
- Centers for Disease Control and Prevention. Viral Hepatitis Surveillance Report, 2016. https://www.cdc.gov/hepatitis/statistics/2016surveillance/index.htm Published November 2018.
- Abdul-Quader AS, Feelemyer J, Modi S, Stein ES, Briceno A, Semaan S, Horvath T, Kennedy GE, Des Jarlais DC, 2013. Effectiveness of structural-level needle/syringe programs to reduce HCV and HIV infection among people who inject drugs: a systematic review. AIDS Behav. 17, 2878–2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Anderson R, Flynn NM, Kral AH, 2007. Higher syringe coverage is associated with lower odds of HIV risk and does not increase unsafe syringe disposal among syringe exchange program clients. Drug Alcohol. Depend 89, 214–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadhead RS, Heckathorn DD, 1999. Termination of an Established Needle-Exchange: A Study of Claims and Their Impact. Social Problems 46, 48–66. [Google Scholar]
- Cleland CM, Deren S, Fuller CM, Blaney S, McMahon JM, Tortu S, Des Jarlais DC, Vlahov D, 2006. Syringe Disposal Among Injection Drug Users in Harlem and the Bronx During the New York State Expanded Syringe Access Demonstration Program. Health Educ. and Behav 34, 390–403. [DOI] [PubMed] [Google Scholar]
- Doherty MC, Garfein RS, Vlahov D, Junge B, Rathouz PJ, Galai N, Anthony JC, Beilenson P, 1997. Discarded Needles Do Not Increase Soon After the Opening of a Needle Exchange Program. Am. J. Epidemiol 145, 730–737. [DOI] [PubMed] [Google Scholar]
- Doherty MC, Junge B, Rathouz P, Garfein RS, Riley E, Vlahov D, 2000. The effect of a needle exchange program on numbers of discarded needles: a 2-year follow-up. Am J Public Health 90, 936–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosden JR, Mitchell AR, Buckland RA, Clayton RP, Evans HJ, 1975. The location of four human satellite DNAs on human chromosomes. Exp. Cell Res 92, 148–158. [DOI] [PubMed] [Google Scholar]
- Iyengar S, Kravietz A, Bartholomew TS, Forrest D, Tookes HE, 2019. Baseline differences in characteristics and risk behaviors among people who inject drugs by syringe exchange program modality: an analysis of the Miami IDEA syringe exchange. Harm Reduct. J 16, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason J, 2013. Community-acquired, non-occupational needlestick injuries treated in US Emergency Departments. J. Public Health 35, 422–430. [DOI] [PubMed] [Google Scholar]
- Kaplan EH, Heimer R, 1994. A circulation theory of needle exchange. AIDS 8, 567–574. [DOI] [PubMed] [Google Scholar]
- Kinnard EN, Howe CJ, Kerr T, Skjodt Hass V, Marshall BD, 2014. Self-reported changes in drug use behaviors and syringe disposal methods following the opening of a supervised injecting facility in Copenhagen, Denmark. Harm Reduct. J 11, 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansky A, Abdul-Quader AS, Cribbin M, Hall T, Finlayson TJ, Garfein RS, Lin LS, Sullivan PS, 2007. Developing an HIV behavioral surveillance system for injecting drug users: the National HIV Behavioral Surveillance System. Public Health Rep 122 Suppl 1, 48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorvick J, Bluthenthal RN, Scott A, Lou Gilbert M, Riehman KS, Anderson RL, Flynn NM, Kral AH, 2006. Secondary syringe exchange among users of 23 California syringe exchange programs. Subst. Use Misuse 41, 865–882. [DOI] [PubMed] [Google Scholar]
- Magnani R, Sabin K, Saidel T, Heckathorn D, 2005. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS 19 Suppl 2, S67–72. [DOI] [PubMed] [Google Scholar]
- Malekinejad M, Johnston LG, Kendall C, Kerr LRFS, Rifkin MR, Rutherford GW, 2008. Using respondent-driven sampling methodology for HIV biological and behavioral surveillance in international settings: a systematic review. AIDS Behav. 12, 105–130. [DOI] [PubMed] [Google Scholar]
- Malekinejad M, McFarland W, Vaudrey J, Raymond HF, 2011. Accessing a diverse sample of injection drug users in San Francisco through respondent-driven sampling. Drug Alcohol Depend. 118, 83–91. [DOI] [PubMed] [Google Scholar]
- Papenburg J, Blais D, Moore D, Al-Hosni M, Laferriere C, Tapiero B, Quach C, 2008. Pediatric injuries from needles discarded in the community: epidemiology and risk of seroconversion. Pediatrics 122, e487–492. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2018. Viral hepatitis surveillance United States, 2016, in: National Center for Hiv/Aids, V.H.S.T.D., Hepatitis, T.B.P.D.o.V, National Notifiable Diseases Surveillance, S; Atlanta, GA. [Google Scholar]
- Quinn B, Chu D, Wenger L, Bluthenthal RN, Kral AH, 2014. Syringe disposal among people who inject drugs in Los Angeles: the role of sterile syringe source. Int. J. Drug Policy 25, 905–910. [DOI] [PubMed] [Google Scholar]
- Riley E, Beilenson P, Vlahov D, Smith L, Koenig M, Jones TS, Doherty M, 1998. Operation Red Box: a pilot project of needle and syringe drop boxes for injection drug users in East Baltimore. Jaids. and Hr 18 Suppl 1, S120–125. [DOI] [PubMed] [Google Scholar]
- Slinger R, Mackenzie SG, Tepper M, 2000. Community-acquired needle stick injuries in Canadian children: Review of Canadian Hospitals Injury Reporting and Prevention Program data from 1991 to 1996. Paediatr. Child Health 5, 324–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson SC, Boughton CR, Dore GJ, 2003. Blood-borne viruses and their survival in the environment: is public concern about community needlestick exposures justified? Aust. N. Z. J. Public Health 27, 602–607. [DOI] [PubMed] [Google Scholar]
- Tookes H, Diaz C, Li H, Khalid R, Doblecki-Lewis S, 2015. A Cost Analysis of Hospitalizations for Infections Related to Injection Drug Use at a County Safety-Net Hospital in Miami, Florida. PLoS One 10, e0129360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tookes HE, Kral AH, Wenger LD, Cardenas GA, Martinez AN, Sherman RL, Pereyra M, Forrest DW, LaLota M, Metsch LR, 2012. A comparison of syringe disposal practices among injection drug users in a city with versus a city without needle and syringe programs. Drug Alcohol Depend. 123, 255–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenger LD, Martinez AN, Carpenter L, Geckeler D, Colfax G, Kral AH, 2011. Syringe disposal among injection drug users in San Francisco. Am. J. Public Health 101, 484–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wodak A, Cooney A, 2006. Do needle syringe programs reduce HIV infection among injecting drug users: a comprehensive review of the international evidence. Subst. Use Misuse 41, 777–813. [DOI] [PubMed] [Google Scholar]
- Zibbell JE, Asher AK, Patel RC, Kupronis B, Iqbal K, Ward JW, Holtzman D, 2018. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am. J. Public Health 108, 175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]


