Abstract
β-myosin heavy chain (MHC) 7 (MYH7) is the dominant pathogenic gene that harbors mutations in 20–30% of cases of familial hypertrophic cardiomyopathy (HCM). The aim of this study was to elucidate the distribution and type of genetic variations among Chinese HCM families. From 2013 to 2017, the clinical data of 387 HCM probands and their families were collected. Targeted exome-sequencing technology was used in all probands, and the selected mutations were subsequently verified by Sanger sequencing in the probands, family members and 300 healthy ethnic-matched volunteers. Three-dimensional models were created using Swiss-PdbViewer 4.1, and further genetic analyses were performed to determine sequence conservation and frequency of the mutations. Among the 5 probands with double MYH7 mutations, 4 carried compound heterozygous mutations, and 1 carried monoallelic double mutations (A934V and E1387K). Four family members of the proband with monoallelic double mutations had the same mutation as the proband. Echocardiography and 12-lead electrocardiography revealed abnormalities in the proband and 3 of the 4 carriers. The probands with compound heterozygous mutation had a higher left ventricular mass as revealed by echocardiography and higher QRS, SV1 and RV5+SV1 amplitudes than those with monoallelic double mutations (P<0.05). Simulation of the 3D structure of mutated proteins showed that the replacement of alanine by valine affected the flexibility of the MHC neck domain in case of the A934V mutation, whereas reactivity of the MHC rod domain was affected in the case of the E1387K mutation. In conclusion, we identified several novel HCM-causing MYH7 mutations. More importantly, this is the first study to report a rare HCM family with monoallelic double mutations.
Keywords: hypertrophic cardiomyopathy, genetic analysis, double mutation, sudden cardiac death, MYH7 mutation
Introduction
Hypertrophic cardiomyopathy (HCM) is the most common inherited cardiovascular disease, with a prevalence of 1 in 500 in the population (1,2). A recent study reported that the prevalence is most likely to be 1 in 200 (3). HCM is a common cause of sudden death in adolescents and the leading cause of sudden death in young athletes (4,5). Approximately 50% of HCM cases are inherited, and this variant is referred to as familial HCM (FHCM) (6). The underlying pathogenesis in HCM is primarily attributed to cardiac sarcomere protein mutations, with over 1,400 HCM mutations being reported in at least 20 genes (7,8). FHCM is also known as a sarcomere disease. Moreover, FHCM is morphologically diverse, substantially heterogeneous within families and shows considerable genetic variability (9). HCM follows a single-gene dominant inheritance, with approximately 7% of cases having polygenic or compound mutations. Compared with patients with single-gene mutations, those with polygenic or compound mutations have a greater incidence of disease, with more severe clinical manifestations and worse prognosis (10–12). Although polygenic or compound mutations are mainly sarcomere protein mutations, a recent study showed that the occurrence of HCM is closely associated with calcium channel gene mutations (13).
Approximately 20–30% of all HCM cases are FHCM ones with β-myosin heavy chain (MHC) 7 (MYH7) as the dominant pathogenic gene (14). Patients carrying compound heterozygous mutations of two alleles in the MYH7 gene may have a more severe clinical phenotype. However, the clinical phenotypes of monoallelic double mutations in MYH7 or their severity has not yet been studied. The aim of the present study was to determine the clinical phenotypes caused by compound heterozygous and monoallelic double mutations of MYH7 using next-generation sequencing.
Materials and methods
Subjects
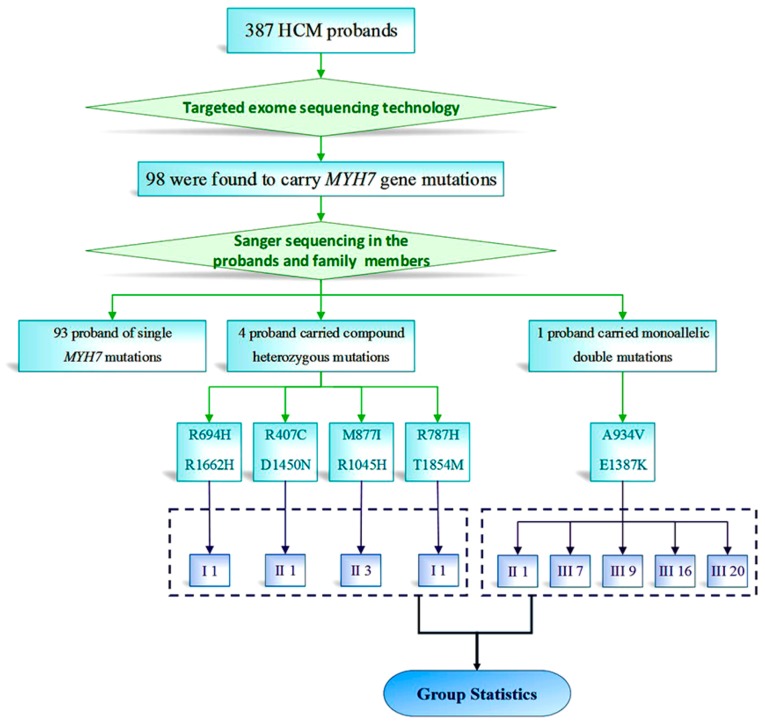
This study conformed to the principles of the Helsinki Declaration and was approved by the Ethics Committee of Xijing Hospital, Fourth Military Medical University, China. The subjects were 387 HCM probands, with clinical data of medical history, 12-lead electrocardiograms and echocardiograms. The probands sought medical care in Xijing Hospital of the Fourth Military Medical University (Fig. 1). We recalled the 4 patients with compound heterozygote mutations and all family members carrying monoallelic double mutations after confirming the mutation, and then acquired ultrasound images and electrocardiographic data. Other patients were not called back for data collection.
Figure 1.
Schematic representation of the filtering process of targeted capture and sequencing data from 387 HCM patients. Among the 387 HCM probands included in the study, 98 were found to carry MYH7 mutations. Among 5 probands with double MYH7 mutations, 4 probands carried compound heterozygous mutations and 1 proband carried monoallelic double mutations. MYH7, β-myosin heavy chain (MHC) 7; HCM, hypertrophic cardiomyopathy.
The diagnostic criteria were based on the 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy and the 2014 ESC Guidelines on Diagnosis and Management of Hypertrophic cardiomyopathy (8,9). In adults, HCM diagnosis requires a wall thickness ≥15 mm in one or more left ventricular (LV) myocardial segments, measured by any imaging technique including echocardiography, cardiac magnetic resonance imaging or computed tomography. In children, HCM diagnosis requires LV wall thickness to be ≥ predicted mean ± standard deviation (z-score >2). On the other hand, among first-degree relatives of patients with unequivocal disease, HCM is defined as an unexplained increase in LV wall thickness ≥13 mm in one or more LV myocardial segments, measured using any cardiac imaging technique. The exclusion criteria for diagnosis are ventricular wall hypertrophy resulting from hypertension, coronary heart disease, coarctation of the aorta, valvular heart disease, congenital heart disease or metabolic disorders and cardiac hypertrophy in athletes.
Genomic DNA extraction and high-throughput sequencing
The RelaxGene Blood DNA System (cat. no. DP319; Tiangen Biotech Co., Ltd., Beijing, China) was used to extract the genomes from white blood cells isolated from 10 ml of peripheral vein blood of the proband, family members and healthy controls. Using targeted exome-sequencing technology, the proband underwent exon amplification and high-throughput sequencing for 96 genes (15) (Table SI) related to FHCM. After synonymous mutations were filtered, mutation loci >0.1% were excluded through several databases including the 1000 Genomes Project (http://browser.1000genomes.org), Exome Variant Server (http://evs.gs.washington.edu/EVS) and ExAC browser (http://exac.broadinstitute.org/terms). The associated variants were subsequently verified by Sanger sequencing in blood relatives of the proband. Meanwhile, 300 healthy individuals of the same ethnic group as the probands (Han ethnic group) were checked for the presence of the same variants.
Imaging studies
For echocardiography, the subjects were examined in the left lateral decubitus position and with quiet breathing, with simultaneous electrocardiogram recording. First, an S5-1 probe was used to perform routine echocardiography, with two-dimensional measurements being made for interventricular septal end-diastolic dimension and LV end-diastolic wall thickness in a 16-segment model. Simpson's rule was used to measure LV volume, LV end-diastolic volume and LV end-systolic volume. Pulsed wave Doppler (PWD) was used to measure the peak velocity flow in early diastole (E) and late diastole (A) so as to calculate the E/A ratio. Tissue Doppler imaging and PWD were used in combination to measure peak velocity of early and late diastolic mitral annulus (Ea and Aa, respectively), followed by the calculation of Ea/Aa and E/Ea. Further, LV mass, LV mass index, stroke volume, LV volume index and LV ejection fraction were determined.
Prediction of mutant protein function
Using Swiss-PdbViewer 4.1 (16) (http://swissmodel.expasy.org/), three-dimensional (3D) models of MYH7-associated proteins were created, and conservation of sequence across species was analyzed.
Statistical analysis
Continuous variables are expressed as means ± standard errors. Differences were analyzed using Student's t-tests. P-values of <0.05 were considered to indicate statistical significance.
Results
Gene mutation analyses
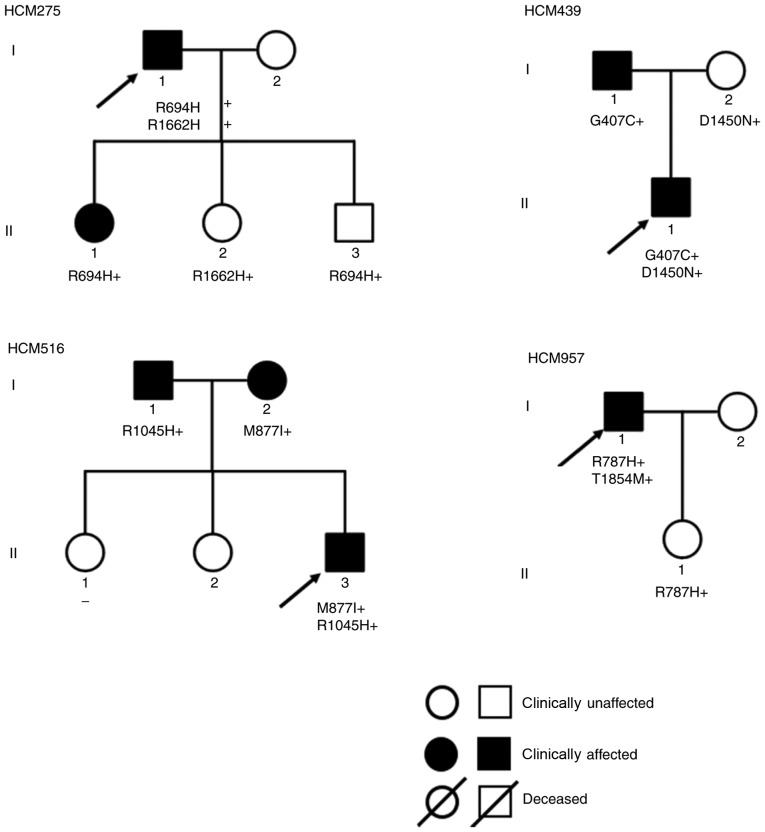
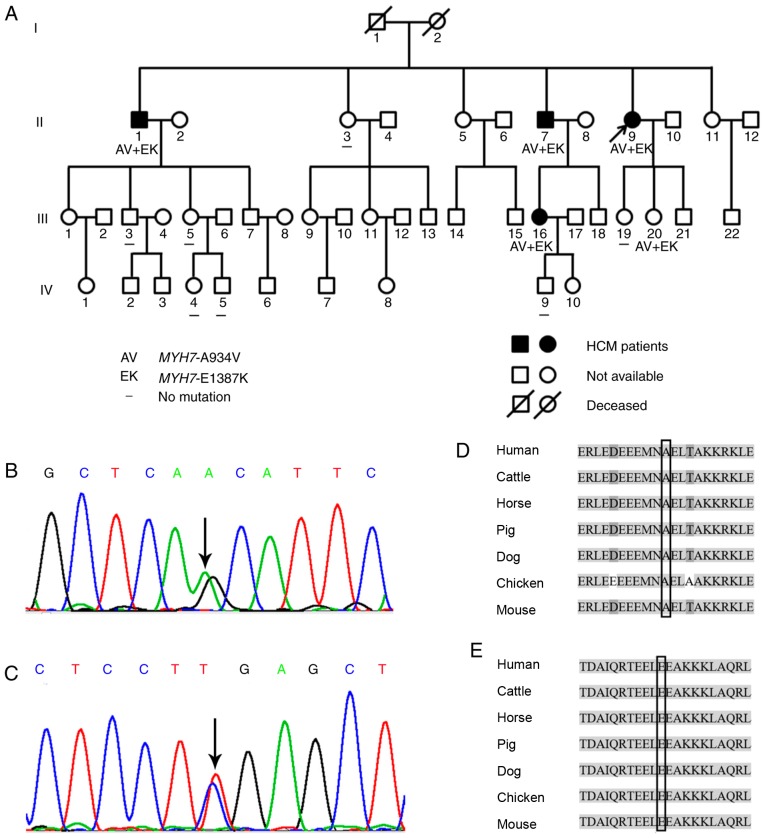
Among the 387 HCM probands included in the study, 98 were found to carry MYH7 mutations. Among 5 probands with double MYH7 mutations, 4 carried compound heterozygous mutations (Fig. 2) and 1 carried monoallelic double mutations. Targeted exon sequencing was performed in 387 HCM probands. These included 98 probands carrying MYH7 mutations (25.3% of all probands) and 5 probands carrying double MYH7 mutations (5.1% of all carrying MYH7 probands) after other sarcomere gene mutations were excluded. Among the 98 probands with MYH7 mutations, 4 (4.1%) had compound heterozygous double mutations and 1 (1%) had monoallelic double mutations. In the family of the proband with monoallelic double mutations, 3 patients were aged <30 years at the time of initial diagnosis, 2 patients had LV outflow tract obstruction, 2 had reduced diastolic function and 3 had syncope (Table I). The variants confirmed in this family were MYH7-A934V and MYH7-E1387K (Fig. 3A). MYH7-A934V is a mutant caused by a C>T substitution in base 2801 of MYH7 exon 23, which results in a change from alanine (amino acid 934, Fig. 3B) to valine. MYH7-E1387K is a mutant caused by a G>A substitution in base 4159 of MYH7 exon 30, which results in a change from glutamic acid (amino acid 1387) to lysine (Fig. 3C).
Figure 2.
Pedigree of the family with phenotypic and genotypic information. Male and female family members are indicated by squares and circles, respectively. Solid symbols represent individuals diagnosed with hypertrophic cardiomyopathy (HCM), and unavailable individuals are represented by open symbols. In addition, the proband is marked with a black arrow. The genotype for each individual is noted below the symbol, where available. Absence of mutations is indicated by a ‘−’ sign.
Table I.
Clinical and genetic characteristics of the probands carrying compound heterozygous MYH7 mutations in the studied HCM cohort.
| Echocardiography | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient ID | Gender/age (years) | Symptoms | Mutation 1 | Mutation 2 | ECG | MLVWT (mm) | LVEF (%) | E/A ratio | LVOT-PG (mmHg) |
| HCM275 | M/59 | Syncope (4) | R694H | R1662H | Inverted T-waves, ST-segment depression | 28 | 65 | 1.30 | 68 |
| HCM439 | M/15 | − | G407C | D1450N | Inverted T-waves, ST-segment depression | 22 | 64 | 1.21 | 14 |
| HCM516 | M/23 | Chest tightness, syncope (1) | M877I | R1045H | Inverted T-waves, ST-segment depression | 28 | 67 | 0.64 | 44 |
| HCM957 | M/30 | Syncope (many times) | R787H | T1854M | Inverted T-waves, ST-segment depression, left anterior branch block | 28 | 58 | 1.25 | 7 |
MLVWT, maximal left ventricular wall thickness; LVEF, left ventricular ejection fraction; E/A ratio, ratio of early to late mitral inflow velocities; LVOT-PG, left ventricular outflow tract pressure gradient. MYH7, β-myosin heavy chain (MHC) 7; HCM, hypertrophic cardiomyopathy.
Figure 3.
(A) Pedigree of the family with phenotypic and genotypic information. Male and female family members are indicated by squares and circles, respectively. Solid symbols represent individuals diagnosed with HCM, and unavailable individuals are represented by open symbols. In addition, the proband is marked with a black arrow. The genotype for each individual is noted below the symbol, where available. Absence of mutations is indicated by a ‘−’ sign. AV, MYH7-A934V; EK, MYH7-E1387K. (B) MYH7-A934V and (C) MYH7-E1387K mutations. Conservation of the mutated site of (D) MYH7-A934 and (E) E1387. Both sites are highly conserved among different species. MYH7, β-myosin heavy chain (MHC) 7; HCM, hypertrophic cardiomyopathy.
Polymerase chain reaction primers were designed to perform Sanger sequencing of MYH7-A934V and MYH7-E1387K for the proband with monoallelic double mutations and her blood relatives. Five family members, including the proband (II9, II1, II7, III16 and III20), were revealed to be carriers of MYH7-A934V and MYH7-E1387K, which were not detected in other family members.
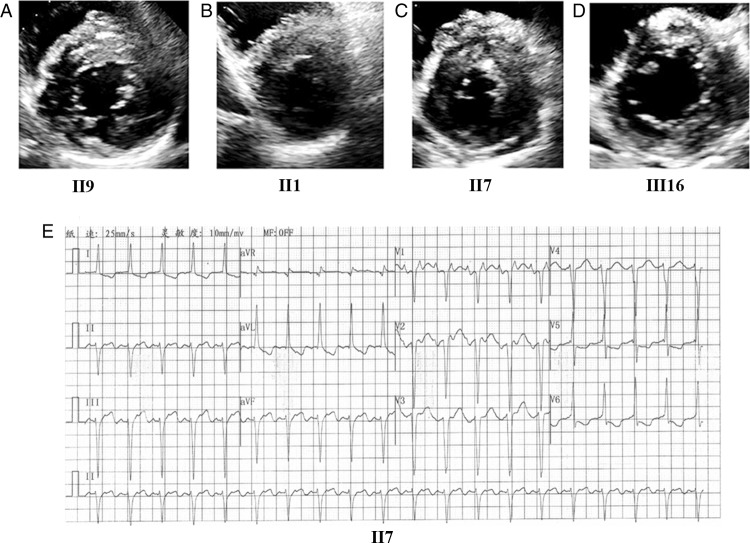
Clinical features
Table II summarizes the clinical features and genotype characteristics. The same 2 mutations were carried by II9, II1, II7, III16 and III20. The proband (II9) was a 46-year-old female who presented with palpitation, breathlessness and chest discomfort. Echocardiography revealed the following: Maximum LV wall thickness, 22 mm (Fig. 4A); left atrium (LA) dimension, 44 mm; E/A, 1.29 and Ea/Aa, 0.74. Electrocardiography showed TI and aVL (flattened and inverted) as well as left axis deviation (−48°). II1 was a 59-year-old male without marked symptoms, for whom echocardiography revealed the following: Maximum LV wall thickness, 15 mm, (Fig. 4B); E/A, 0.4 and Ea/Aa, 0.5. Electrocardiography indicated clockwise rotation. The elder brother of the proband, II7, a 55-year-old male, presented with clear symptoms and the following echocardiography findings: Maximum LV wall thickness, 28 mm (Fig. 4C) and LA dimension, 59 mm. Electrocardiography showed atrial tachycardia, left axis deviation, LV fascicular block, inverted T-waves and ST-segment depression (Fig. 4E). The proband's asymptomatic niece (III16), a 26-year-old female, had borderline LV wall thickening (Fig. 4D). Another carrier was the proband's 14-year-old daughter (III20), who was asymptomatic and had unremarkable physical examination findings. Among the family members without the 2 mutations, none showed abnormal findings.
Table II.
Clinical and genetic characteristics of the index family with single allele double MYH7 mutations in the studied HCM cohort.
| Echocardiography | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient ID | Gender/age (years) | Symptoms | MYH7- A934V | MYH7- E1387K | ECG | MLVWT (mm) | LVEF (%) | E/A ratio | LVOT-PG (mmHg) |
| II-1 | M/59 | − | + | + | Indicated clockwise rotation. | 15 | 60 | 0.40 | 5 |
| II-3 | F/57 | − | − | − | Normal | 10 | 63 | 1.31 | 1 |
| II-7 | M/55 | Chest tightness | + | + | LV fascicular block inverted T-waves, ST-segment depression | 28 | 56 | atrial tachycardia | 4 |
| II-9 | F/46 | Chest tightness, palpitation | + | + | T flattened and inverted, and left axis deviation (−48°). | 22 | 63 | 1.29 | 4 |
| III-3 | M/32 | − | − | − | Normal | 12 | 52 | 0.69 | 2 |
| III −5 | F/31 | − | − | − | Nearly normal | 9 | 63 | 1.33 | 3 |
| III-16 | F/26 | − | + | + | Flat T waves in leads I, aVL and V | 13 | 58 | 1.13 | 2 |
| III-19 | F/19 | − | − | − | Normal | 9 | 57 | 1.6 | 3 |
| III-20 | F/14 | − | + | + | Normal | 6 | 67 | 1.32 | 1 |
| IV-4 | F/6 | − | − | − | Normal | 4 | 61 | 1.54 | 2 |
| IV-5 | M/4 | − | − | − | Normal | 3 | 65 | 2.96 | 1 |
| IV-9 | M/4 | − | − | − | Normal | 4 | 62 | 1.3 | 2 |
E/A ratio, ratio of early to late mitral inflow velocities; LVEF, left ventricular ejection fraction; MLVWT, maximal left ventricular wall thickness. LVOT-PG, left ventricular outflow tract pressure gradient MYH7, β-myosin heavy chain (MHC) 7; HCM, hypertrophic cardiomyopathy; M, male; F, female.
Figure 4.
Echocardiographic images of the left ventricle by the short-axis view and electrocardiography findings in genetically affected family members with HCM. (A, B, C and D) Echocardiography with parasternal short-axis view, (E) electrocardiography of II-7. HCM, hypertrophic cardiomyopathy.
Comparisons of compound heterozygous and monoallelic double mutations
Statistical analysis of clinical ultrasound data showed that the compound heterozygous mutation carriers had higher LV mass (LVM) than those with monoallelic double mutations (P=0.03). The compound heterozygous mutation carriers also showed higher amplitudes in QRS, SV1 and RV5+SV1. On the other hand, there were no significant differences in LV wall thickness, LA dimension or other parameters (Table III).
Table III.
Comparisons of the echocardiographic parameters between the subgroups.
| Variables | Compound heterozygous mutations (n=4) | Monoallelic double mutations (n=5) | P-valuea |
|---|---|---|---|
| Age (years) | 32±19 | 40±19 | 0.543 |
| LVOT-PG (mmHg) | 33±28 | 3±2 | 0.123 |
| MLVWT (mm) | 27±3 | 17±8 | 0.068 |
| LA diameter (mm) | 41±6 | 39±11 | 0.079 |
| LVMI (g/m2) | 114±24 | 86±33 | 0.191 |
| LVM (g) | 222±32 | 135±57 | 0.03a |
| LVEF | 64±4 | 61±4 | 0.363 |
| E/A | 1.1±0.3 | 1.0±0.4 | 0.815 |
| E/e′ | 16.57±9.52 | 15.28±10.72 | 0.864 |
| HR (bpm) | 69±12 | 88±21 | 0.157 |
| QRS (msec) | 111±7 | 95±8 | 0.015a |
| PR (msec) | 161±26 | 172±32 | 0.578 |
| QT (msec) | 415±41 | 358±46 | 0.094 |
| QTC (msec) | 440±30 | 424±29 | 0.459 |
| RV5, mV | 1.64±0.67 | 1.00±0.23 | 0.149 |
| SV1, mV | 3.19±1.11 | 1.11±0.38 | 0.028a |
| RV5+SV1, mV | 4.84±1.74 | 2.11±0.56 | 0.047a |
LVOT-PG, left ventricular outflow tract pressure gradient; MLVWT, maximal left ventricular wall thickness; LA, left atrial; LVMI, left ventricular mass index; LVM, left ventricular mass; LVEF, left ventricular ejection fraction; E/A ratio, ratio of early to late mitral inflow velocities; E/e′ ratio, ratio of early diastolic mitral inflow velocity to septal early diastolic mitral annular velocity; HR, heart rate.
P<0.05, statistically significant result.
Prediction analysis of mutant protein function
Prediction for sequence conservation
In the blocks shown (Fig. 3D and E), the sequences marked in light grey, where sequence conservation is usually observed, were identical. In addition, the mutation sites, i.e., MYH7-A934 (Fig. 3D) and MYH7-E1387 (Fig. 3E), which are highly conserved among species, were located in the block, whereas sequences indicated in light grey were exactly the same. Genetic backgrounds of both novel MYH7 mutations identified in the cohort are described in Table IV.
Table IV.
Genetical background of 2 novel MYH7 mutations identified in the study.
| Prediction | Frequency | |||||
|---|---|---|---|---|---|---|
| Mutation | SIFT | PolyPhen-2 | 1000 Genomes | ExAC_EAS | ESP | Conservation GERP++ |
| MYH7-A934V | 0.001 (D) | 0.647 (P) | 0 | 0 | 0 | 5.33 |
| MYH7-E1387K | 0 (D) | 1 (D) | 0 | 0 | 0 | 4.83 |
If the SIFT-score is <0.05 (rank score >0.395), then the corresponding nsSNV is predicted as D (Damaging); otherwise it is predicted as T (tolerated). Polyphen2 prediction based on HumDiv: D (probably damaging), HDIV score in [0.957, 1]; P (possibly damaging), HDIV score in [0.453, 0.956] and B (benign), HDIV score in [0, 0.452]. GERP++ RS score: The larger the score, the more conserved the site. Scores range from −12.3 to 6.17. ESP: Frequencies in the database of European and African-American normal.
Protein structure and pathogenicity prediction
Three-dimensional structure of amino acid 934 based on the published MYH7 structure (PDB code, 2FXM) viewed with the Swiss-PdbViewer 4.1 software showed that the replacement of alanine by valine at codon 934 (Fig. 5A) led to a change in the side chains of the amino acid but did not have a significant impact on the local intermolecular hydrogen bonds or surface charge distribution. The structural changes on the side chains may result in pathogenesis by affecting the flexibility of the MHC neck domain (Fig. 5B). On the other hand, the simulated structure of amino acid 1387 based on the published MYH7 structure 4XA3 showed that the replacement of the acidic glutamic acid by an alkaline lysine at codon 1387 (Fig. 5C) led to a significant impact on surface charge distribution, resulting in a change in the molecular surface, but had no effect on local intermolecular hydrogen bonds. This mutation might change the local structure and potential molecular interactions, contributing to pathogenesis by affecting the reactivity of the MHC rod domain (Fig. 5D).
Figure 5.
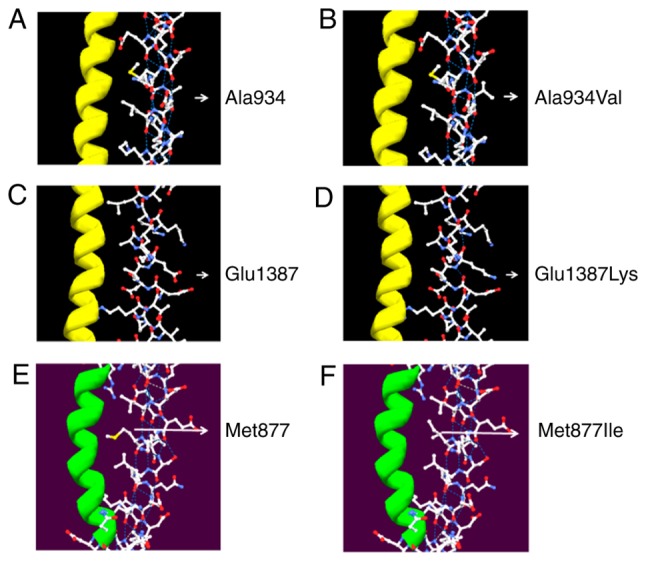
Three-dimensional structural modification of protein-bearing mutations of (A and B) MYH7-A934V vs. wild-type MHY7, (C and D) MYH7-E1387K vs. wild-type MHY7, (E and F) MYH7-E877I vs. wild-type MHY7. MYH7, β-myosin heavy chain (MHC) 7.
For amino acid 877, the simulation based on the MYH7 structure (2FXM) showed that the replacement of methionine by isoleucine at codon 877 (Fig. 5E) led to a change in the side chains of the amino acid but had no significant impact on the local intermolecular hydrogen bonds or surface charge distribution. These structural changes on the side chains might result in pathogenesis by affecting the flexibility of the MHC neck domain (Fig. 5F).
In accordance with the variant classification criteria stated in the American College of Medical Genetics and Genomics (ACMG) guidelines (17), MYH7-A934V is considered in line with 1 type of PM (PM2) and 3 types of PP (PP1, PP3 and PP4) variants, and was therefore identified as having uncertain significance; MYH7-E1387K, considered in line with 1 type of PM (PM2) and 4 types of PP (PP1, PP3, PP4 and PP5) variants, and was therefore identified as likely pathogenic. Since the 2 variants existed in the same allele, carrier status for both variants should be classified as likely pathogenic; however, sufficient evidence to support this classification is currently unavailable.
Discussion
In the present study cohort, there were a total of 5 hypertrophic cardiomyopathy (HCM) probands carrying double MYH7 mutations. Among these, MYH7-V934A, MYH7-E1387K and MYH7-M877I were identified as novel MYH7 mutations causing HCM. We were unable to find these mutations in the normal control population in searches of the ESP database (http://evs.gs.washington.edu/EVS), the 1000 Genomes and the ExAC browser. Predictive analyses using SIFT (http://sift.jcvi.org), PolyPhen-2 (http://genetics.bwh.harvard.edu/pph2) and GERP++ (http://mendel.stanford.edu/sidowlab/downloads/gerp/index.html) revealed that MYH7-M877I, MYH7-E1387K and MYH7-M877I were all pathogenic mutations. More importantly, our findings demonstrated a rare HCM family with monoallelic double mutations in MYH7 that has not been reported previously. Finally, statistical analysis revealed that the clinical phenotype was less severe in the carriers with monoallelic double mutations than in those with diallelic double mutations in MYH7.
Based on the published MYH7 structure 2FXM, the 3D structure of the amino acids 934 and 877 simulated with the Swiss-PdbViewer 4.1 showed that V934A and M877I could cause changes in the side chains of the amino acids. These changes may contribute to HCM pathogenesis by affecting the flexibility of the MHC neck domain. Similarly, based on the published MYH7 structure 4XA3, the simulated structure of the amino acid 1387 showed that E1387K could result in a significant impact on surface charge distribution, resulting in a change in the molecular surface, but would otherwise have no effect on the local intermolecular hydrogen bonds. This mutation would change the local structure and potential molecular interactions, potentially contributing to the pathogenesis by changing the reactivity of the MHC rod domain.
Molecular genetic studies have demonstrated that 40–60% of the pathogenic genes in patients with HCM are attributable to mutations in sarcomere proteins and associated proteins (9,18). MYH7 is the predominant pathogenic gene in HCM (30–50% of all cases). The common symptoms associated with the mutation are observed in malignant HCM phenotypes and include early onset, high penetrance, high degree of hypertrophy and high incidence of sudden death (18,19). MYH7 is located between 14q11 and 14q12 and contains 40 exons, among which 38 participate in encoding 1935 amino acids. It encodes β-MHC, which is the principal constituent of the thick myofilament and is composed of globular head, neck and rod domains (20).
The head is the location for the adenosine triphosphatase activity locus as well as the binding sites for actin and the essential light chain. This region thus serves a vital function and mutations in this region often result in more severe clinical phenotypes than those in the rod domain (21). The 2018 ACMG guidelines for the Pathogenicity Analysis of MYH7 provide moderate pathogenic evidence for the region comprising the amino acids 181–937 (22). However, these definitions are for single-gene mutation sites, and currently there are no guidelines for carriers with ≥2 MYH7 mutations, including those with monoallelic double mutations.
The main pathogenic event in HCM cases with MYH7 as the mutant gene is a single point mutation. No studies have reported the proportion of compound heterozygous MYH7 mutations in HCM families. Second-generation analysis of 387 HCM families in the current study showed that the proportion of compound heterozygous MYH7 mutations was 5.1%. Furthermore, no study in China or elsewhere has elucidated monoallelic double mutations in MYH7; the present study is the first to provide data on the proportion of compound heterozygous MYH7 mutations in Chinese families with HCM, which should aid in the genetic counselling of HCM patients.
Regarding the pathogenesis associated with these mutations, it is possible that the presence of the monoallelic double mutations might be functionally compensated by the normal allele; this might explain the normal clinical presentation of some of the carriers in the present study. In probands with multiple MYH7 gene mutations, using a familial cosegregation test to identify specific infringement alleles will have a significant impact on risk assessment and clinical intervention strategies in carriers. The pathogenicity of single-gene MYH7 mutations can be determined using the 2018 ACMG Guidelines for the Pathogenicity Analysis of MYH7 (22). However, these guidelines do not address the potential influence of carrying multiple genes on disease severity. It is controversial whether the double mutations or compound heterozygosity in MYH7 may affect HCM severity. Viswanathan et al provided evidence that compound mutations may not increase the severity of the HCM phenotype compared with single mutations, but it may substantially increase the risk of developing HCM (23). Wang et al enrolled 529 Chinese HCM patients, and found that the HCM patients with multiple rare sarcomere mutations had earlier age of onset, more severe left ventricular hypertrophy and enlarged left atrium, as well as higher risk of sudden cardiac death, as compared to those with single rare mutation (11). The 2017 Guideline for Hypertrophic Cardiomyopathy in China showed that approximately 7% patients have complex mutations regardless of their genetic inheritance status (10–12,24). HCM onset in these patients is earlier than those with single-gene mutations, and the clinical manifestations are more severe. In the present study, such patients carried previously unreported monoallelic double mutations. Carriers with compound heterozygous mutations had significantly higher LVM by echocardiography and higher amplitudes in QRS, SV1 and RV5+SV1 than those with monoallelic double mutations.
Upon electrocardiography, QRS, RV5, RV5+SV1 were positively correlated with LV voltage. Furthermore, LV voltage was positively correlated with LV wall thickness, and higher LV voltages were associated with more severe LV hypertrophy. The degree of hypertrophy of the ventricular wall has been positively correlated with the risk of sudden death in patients with HCM (25,26). Therefore, this study suggests that if patients undergoing clinical genetic analyses are detected with 2 mutations of the pathogenic gene, the proband will either carry monoallelic double mutations or compound heterozygous double mutations. The prognosis of mutation carriers among blood relatives has a certain guiding significance and should have an important impact on the clinical management of patients and those at risk. However, our study lacks clinical indicators of the prognosis to stratify the arrhythmic risks in both control and mutant groups, such as Holter and stress test. This has been realized by us, and relevant data will be collected in future studies.
Limitations to the present study must be addressed. In the present study, we found differences between the two groups of compound heterozygote mutations and monoallelic double mutations. Yet, a statistically significant impact of the mutations on clinical phenotypes in a single family with monoallelic double mutations is not representative of all patients or families carrying this type of variation. Whether our preliminary results can be amplified into the population still requires verification by large populations that will be carried out in future investigation.
In conclusion, we identified several novel MYH7 mutations that are potentially pathogenic in HCM. Moreover, we reported the findings of a rare HCM family carrying monoallelic MYH7 double mutations, which have not been previously reported. Our findings suggest that the clinical presentation of carriers with these monoallelic double mutations may be less severe than that of those with diallelic double mutations.
Supplementary Material
Acknowledgements
The authors would like to thanks Professor Yuan-Ming Wu, Fourth Military Medical University, Xi'an, Shaanxi, China, for his genetic data analysis.
Funding
This research was supported by the International Science and Technology Cooperation Program of China (2014DFA31980), the Natural Science Foundation of China (81671693, 81601498 and 81670304), Shaanxi Provincial Key Project (2017ZDXM-SF-058) and Xijing Funded Project for New Technologies and Services (417432A).
Availability of data and materials
The datasets used during the present study are available from the corresponding author upon reasonable request.
Authors' contributions
LWL and DH conceived and designed the study. BW, LFW, YH and QLY collected and analyzed genetic data. JW, FY, LX and LZ collected and analyzed UCG data. WXL and HS collected and analyzed ECG data. BW and JW wrote the paper. LFW reviewed and edited the manuscript. All authors read and approved the manuscript and agree to be accountable for all aspects of the research in ensuring that the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval and consent to participate
This study conformed to the principles of the Helsinki Declaration and was approved by the Ethics Committee of Xijing Hospital, Fourth Military Medical University, China.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Maron BJ, Gardin JM, Flack JM, Gidding SS, Kurosaki TT, Bild DE. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA study. Coronary artery risk development in (young) adults. Circulation. 1995;92:785–789. doi: 10.1161/01.CIR.92.4.785. [DOI] [PubMed] [Google Scholar]
- 2.Maron BJ, Maron MS. Hypertrophic cardiomyopathy. Lancet. 2013;381:242–255. doi: 10.1016/S0140-6736(13)60922-8. [DOI] [PubMed] [Google Scholar]
- 3.Semsarian C, Ingles J, Maron MS, Maron BJ. New perspectives on the prevalence of hypertrophic cardiomyopathy. J Am Coll Cardiol. 2015;65:1249–1254. doi: 10.1016/j.jacc.2015.01.019. [DOI] [PubMed] [Google Scholar]
- 4.Maron BJ. Contemporary insights and strategies for risk stratification and prevention of sudden death in hypertrophic cardiomyopathy. Circulation. 2010;121:445–456. doi: 10.1161/CIRCULATIONAHA.109.878579. [DOI] [PubMed] [Google Scholar]
- 5.Maron BJ, Thompson PD, Ackerman MJ, Balady G, Berger S, Cohen D, Dimeff R, Douglas PS, Glover DW, Hutter AM, Jr, et al. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: A scientific statement from the American heart association council on nutrition, physical activity, and metabolism: Endorsed by the American college of cardiology foundation. Circulation. 2007;115:1643–1655. doi: 10.1161/CIRCULATIONAHA.107.181423. [DOI] [PubMed] [Google Scholar]
- 6.Ahmad F, Seidman JG, Seidman CE. The genetic basis for cardiac remodeling. Annu Rev Genomics Hum Genet. 2005;6:185–216. doi: 10.1146/annurev.genom.6.080604.162132. [DOI] [PubMed] [Google Scholar]
- 7.Waldmüller S, Sakthivel S, Saadi AV, Selignow C, Rakesh PG, Golubenko M, Joseph PK, Padmakumar R, Richard P, Schwartz K, et al. Novel deletions in MYH7 and MYBPC3 identified in Indian families with familial hypertrophic cardiomyopathy. J Mol Cell Cardiol. 2003;35:623–636. doi: 10.1016/S0022-2828(03)00050-6. [DOI] [PubMed] [Google Scholar]
- 8.Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, Nishimura RA, Ommen SR, Rakowski H, et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:2761–2796. doi: 10.1161/CIR.0b013e318223e230. [DOI] [PubMed] [Google Scholar]
- 9.Authors/Task Force members. Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli G, et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: The task force for the diagnosis and management of hypertrophic cardiomyopathy of the European society of cardiology (ESC) Eur Heart J. 2014;35:2733–2779. doi: 10.1093/eurheartj/ehu284. [DOI] [PubMed] [Google Scholar]
- 10.Maron BJ, Maron MS, Semsarian C. Double or compound sarcomere mutations in hypertrophic cardiomyopathy: A potential link to sudden death in the absence of conventional risk factors. Heart Rhythm. 2012;9:57–63. doi: 10.1016/j.hrthm.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Wang J, Wang Y, Zou Y, Sun K, Wang Z, Ding H, Yuan J, Wei W, Hou Q, Wang H, et al. Malignant effects of multiple rare variants in sarcomere genes on the prognosis of patients with hypertrophic cardiomyopathy. Eur J Heart Fail. 2014;16:950–957. doi: 10.1002/ejhf.144. [DOI] [PubMed] [Google Scholar]
- 12.Zou Y, Wang J, Liu X, Wang Y, Chen Y, Sun K, Gao S, Zhang C, Wang Z, Zhang Y, et al. Multiple gene mutations, not the type of mutation, are the modifier of left ventricle hypertrophy in patients with hypertrophic cardiomyopathy. Mol Biol Rep. 2013;40:3969–3976. doi: 10.1007/s11033-012-2474-2. [DOI] [PubMed] [Google Scholar]
- 13.Helms AS, Alvarado FJ, Yob J, Tang VT, Pagani F, Russell MW, Valdivia HH, Day SM. Genotype-dependent and -independent calcium signaling dysregulation in human hypertrophic cardiomyopathy. Circulation. 2016;134:1738–1748. doi: 10.1161/CIRCULATIONAHA.115.020086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cam FS, Güray M. Hypertrophic cardiomyopathy: Pathological features and molecular pathogenesis. Anadolu Kardiyol Derg. 2004;4:327–330. [PubMed] [Google Scholar]
- 15.Wang L, Zuo L, Hu J, Shao H, Lei C, Qi W, Liu Y, Miao Y, Ma X, Huang CL, et al. Dual LQT1 and HCM phenotypes associated with tetrad heterozygous mutations in KCNQ1, MYH7, MYLK2, and TMEM70 genes in a three-generation Chinese family. Europace. 2016;18:602–609. doi: 10.1093/europace/euv043. [DOI] [PubMed] [Google Scholar]
- 16.Guex N, Peitsch MC. SWISS-MODEL and the Swiss-PdbViewer: An environment for comparative protein modeling. Electrophoresis. 1997;18:2714–2723. doi: 10.1002/elps.1150181505. [DOI] [PubMed] [Google Scholar]
- 17.Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American college of medical genetics and genomics and the association for molecular pathology. Genet Med. 2015;17:405–424. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lopes LR, Zekavati A, Syrris P, Hubank M, Giambartolomei C, Dalageorgou C, Jenkins S, McKenna W, Uk10k Consortium, Plagnol V, Elliott PM. Genetic complexity in hypertrophic cardiomyopathy revealed by high-throughput sequencing. J Med Genet. 2013;50:228–239. doi: 10.1136/jmedgenet-2012-101270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang S, Zou Y, Fu C, Xu X, Wang J, Song L, Wang H, Chen J, Wang J, Huan T, Hui R. Worse prognosis with gene mutations of beta-myosin heavy chain than myosin-binding protein C in Chinese patients with hypertrophic cardiomyopathy. Clin Cardiol. 2008;31:114–118. doi: 10.1002/clc.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woo A, Rakowski H, Liew JC, Zhao MS, Liew CC, Parker TG, Zeller M, Wigle ED, Sole MJ. Mutations of the beta myosin heavy chain gene in hypertrophic cardiomyopathy: Critical functional sites determine prognosis. Heart. 2003;89:1179–1185. doi: 10.1136/heart.89.10.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walsh R, Rutland C, Thomas R, Loughna S. Cardiomyopathy: A systematic review of disease-causing mutations in myosin heavy chain 7 and their phenotypic manifestations. Cardiology. 2010;115:49–60. doi: 10.1159/000252808. [DOI] [PubMed] [Google Scholar]
- 22.Kelly MA, Caleshu C, Morales A, Buchan J, Wolf Z, Harrison SM, Cook S, Dillon MW, Garcia J, Haverfield E, et al. Adaptation and validation of the ACMG/AMP variant classification framework for MYH7-associated inherited cardiomyopathies: Recommendations by ClinGen's inherited cardiomyopathy expert panel. Genet Med. 2018;20:351–359. doi: 10.1038/gim.2017.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Viswanathan SK, Sanders HK, McNamara JW, Jagadeesan A, Jahangir A, Tajik AJ, Sadayappan S. Hypertrophic cardiomyopathy clinical phenotype is independent of gene mutation and mutation dosage. PLoS One. 2017;12:e0187948. doi: 10.1371/journal.pone.0187948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guidelines for the diagnosis and treatment for Chinese adult patients with hypertrophic cardiomyopathy. Zhonghua Xin Xue Guan Bing Za Zhi. 2017;45:1015–1032. doi: 10.3760/cma.j.issn.0253-3758.2017.12.005. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 25.Elliott PM, Gimeno JR, Tomé MT, Shah J, Ward D, Thaman R, Mogensen J, McKenna WJ. Left ventricular outflow tract obstruction and sudden death risk in patients with hypertrophic cardiomyopathy. Eur Heart J. 2006;27:1933–1941. doi: 10.1093/eurheartj/ehl041. [DOI] [PubMed] [Google Scholar]
- 26.Maron MS, Olivotto I, Betocchi S, Casey SA, Lesser JR, Losi MA, Cecchi F, Maron BJ. Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy. N Engl J Med. 2003;348:295–303. doi: 10.1056/NEJMoa021332. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used during the present study are available from the corresponding author upon reasonable request.