Abstract
Background
The objective of this study was to summarize clinical features and PRRT2 mutations of paediatric paroxysmal kinesigenic dyskinesia (PKD) patients and observe the tolerability and effects of morning draughts of oxcarbazepine.
Methods
Twenty patients diagnosed with PKD at Children’s Hospital of Fudan University between January 2011 and December 2015 were enrolled. These patients’ medical records were reviewed. Peripheral venous blood was obtained from all enrolled patients, and polymerase chain reaction (PCR) and Sanger sequencing were used to sequence proline-rich transmembrane protein 2 (PRRT2) gene mutations. Clinical features of PKD patients with and without PRRT2 mutations were compared. All enrolled patients were treated with morning draughts of oxcarbazepine (OXC). The starting dose was 5 mg/kg·d, and the dose was increased by 5 mg/kg·d each week until attacks stopped. Effective doses and adverse effects were recorded.
Results
For all enrolled patients, dyskinesia was triggered by sudden movement. Dyskinetic movement usually involved the limbs and was bilateral; the majority of enrolled patients exhibited both dystonia and choreoathetosis. We identified PRRT2 mutations in 5 patients, including 4 familial patients and 1 sporadic patient. All 20 patients took low doses of OXC (5–20 mg/kg·d) as draughts in the morning, and dyskinesia attacks stopped in 19 patients.
Conclusions
Paediatric PKD patients have various phenotypes. PRRT2 mutations are common in familial cases. OXC taken as morning draughts can be a treatment option for paediatric PKD patients.
Keywords: Clinical features, OXC, PKD, PRRT2, Treatment
Introduction
Paroxysmal kinesigenic dyskinesia (PKD) (OMIM 128200) is the most common form of paroxysmal dyskinesia. The main clinical feature of PKD is brief, unilateral or bilateral attacks of dystonia and choreoathetosis triggered by sudden movements [1]. The prevalence of PKD is ~ 1/150000, certain patients have a family history of PKD, which is typically inherited in an autosomal dominant pattern [2]. The onset age for PKD is typically in childhood or adolescence, and symptoms usually become self-limiting with age [3]. Recently, two Chinese groups had identified mutations in the gene encoding proline-rich transmembrane protein 2 (PRRT2) (OMIM 614386) as a cause of PKD, the most common mutation in PRRT2 was c.649dupC(p.R217Pfs*8) [4, 5].
The pathogenesis and mechanism of PKD have not been completely elucidated. Recently, researchers have found abnormal excitability in the cortex and basal ganglia in certain PKD patients and concluded that channelopathy is an underlying mechanism in PKD [6]. Most PKD patients exhibit a favourable response to carbamazepine (CBZ), which modulates different types of calcium channels, supporting the hypotheses that channelopathy is an underlying mechanism in PKD [7]. However, allergies are present in a subset of PKD patients who use CBZ; thus, a safer and efficient alternative drug must be identified. Oxcarbazepine (OXC), a derivative of CBZ, has been reported to be effective in certain cases of PKD [8].
Few available reports address treatment for paediatric PKD patients. This research sought to investigate clinical manifestations and genetic characteristics of PRRT2 mutations and the correlation between PKD phenotype and the presence of mutations in the PRRT2; in addition, the effects of morning draughts of OXC on paediatric PKD patients were observed.
Methods
Subjects
Twenty Chinese-Han patients with PKD at Children’s Hospital of Fudan University were enrolled between January 2011 and December 2015. All subjects satisfied the following diagnostic criteria for PKD: an identified trigger for attacks (sudden movements), short attack durations (< 1 min), a lack of loss of consciousness or pain during attacks, antiepileptic drug responsiveness, the exclusion of other organic diseases, and age at onset of 1 to 20 years. Disease histories, clinical manifestations, results from physical, neurological, and biochemical examinations, and electroencephalography (EEG) and neuroimaging findings were investigated and analysed.
Genetic analysis
Genomic DNA was extracted from patients’ peripheral blood leukocytes. Polymerase chain reaction (PCR) and Sanger sequencing were performed to identify PRRT2 mutations, and no attempt was made to screen other relevant genes implicated in dystonia like MECR, SLC2A1, SGCE, THAP1, EKD2, PNKD2, DYT7, CNVs were not assessed. Two coding exons (2 and 3) were amplified by PCR (Exon 2AF 5′-CTCCTCCTCTTCCAGGGTTT-3′, Exon 2AR 5′-TTTTTGAGGGTGGTGAGTGA-3′, Exon 2BF 5′-TCTGAGAGTGTAGGGGAAAAGC-3′, Exon 2BR 5′-CTAGGGAGAGGCAAACAAAGG-3′, Exon 3F 5′-TCCACCTGATCCCTTCTGG-3′ and Exon 3R 5′-CAGGCTCCCTTGGTCCTTAG-3′). We used touch down PCR, denature last 3 min at 94 °C, the first thermal cycling was 16 cycles of 94 °C for 30 s, 65 °C for 30 s and 72 °C for 40 s, the second thermal cycling was 30 cycles of 94 °C for 30 s, 60 °C for 30 s and 72 °C for 40 s. GRCh37 was utilized as reference genome and NM_145239.2 was utilized for mutation screening. Clinical features of PKD patients with and without PRRT2 mutations were compared. Differences between two groups were compared using unpaired Student’s t-tests and Fisher’s exact test for quantitative and categorical variables, respectively. The threshold for statistical significance was p < 0.05.
Treatment
OXC, which was taken as a draught in the morning, was used to treat all enrolled patients. The starting dose was 5 mg/kg·d. The frequency of attacks and adverse events were recorded by at least two caregivers of each patient. The dose was increased by 5 mg/kg·d each week until both two caregivers recorded an at least 75% reduction in attacks frequency or reached the maximum dose in the drug instruction. Only when the attack frequency decreased more than 75% last for 1 month, the dose would be recorded as effective dose.
Results
Clinical manifestations and PRRT2 mutations of enrolled PKD patients
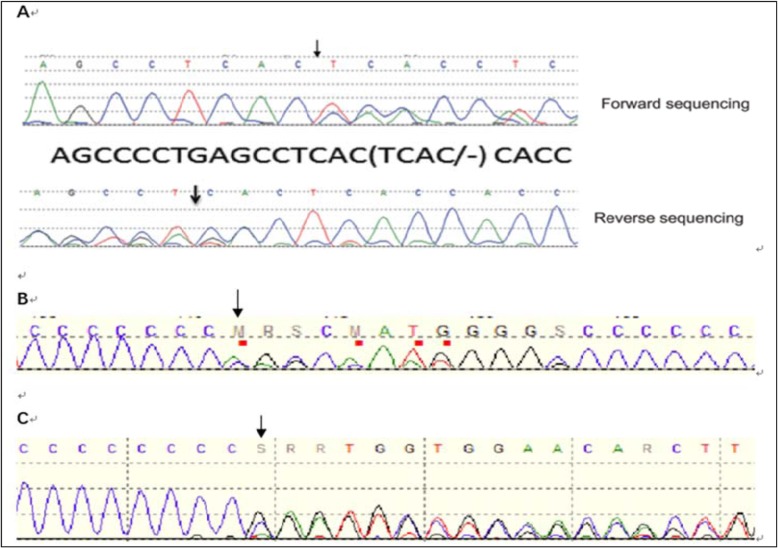
Five familial PKD patients from 4 families (including two patients from one family whose cases have been described in a previously published report [9]) and 15 sporadic PKD patients were enrolled in our study (17 males and 3 females) (Table 1). The age of dyskinesia onset ranged from 2.5 to 13 years, and the mean and median ages were 8.1 and 8 years, respectively. All patients had normal results on physical, neurological, and biochemical examinations and normal EEG and neuroimaging findings. Paroxysmal dyskinesia was triggered by sudden movement in all enrolled patients. Dyskinetic attacks involved the limbs for all enrolled patients, two of them had focal onset in one limb; one patient had facial involvement. Eighteen patients had bilateral dyskinesia, and the remaining patients exhibited unilateral dyskinesia. The phenomenology of attacks was primarily dystonia in 10 patients, primarily choreoathetosis in 4 patients, and both dystonia and choreoathetosis in the remaining 6 patients. The frequency of attacks ranged from several times per day to several times per week. Infantile convulsions with paroxysmal choreoathetosis were observed in 3 familial PKD patients from 2 families. One sporadic case involved partial epilepsy, and the remaining cases involved no comorbidities. PRRT2 mutations were identified in 4 of the 5 familial PKD patients, only point mutations or small indels were tested, in patient 1 and 2 from the same family we found c.604-607delTCAC(chr16:29824979–29,824,982, p.S202Hfs*25, the allele frequency was none), c.629dupC(chr16:29825004, p.Ala211Serfs*14, the allele frequency was 0.0001 in ExAC) and c.649dupC(chr16:29825024, p.Arg217Profs*8, the allele frequency was 0.0000 in ExAC) were found in patient 3 from family 2 and patient 5 from family 4, we also found c.649dupC(chr16:29825024, p.Arg217Profs*8, the allele frequency was 0.0000 in ExAC) in one sporadic PKD patients (Fig. 1).
Table 1.
Patients clinical features
| Patients | Age at onset (years) | Family | Phenomenolo-gy of attack | Localisation | PRRT2 mutations | Frequency of attack (per day) | Comorbidity |
|---|---|---|---|---|---|---|---|
| 1 | 2.7 | fam1 | D + C | Upper and lower limbs |
c.604-607delTCAC p.S202Hfs*25 |
< 5 | ICCA |
| 2 | 7.6 | fam1 | C | Lower limbs |
c.604-607delTCAC p.S202Hfs*25 |
< 5 | ICCA |
| 3 | 7.8 | fam2 | C | Lower limbs |
c.629dupC p.Ala211Serfs*14 |
5 to 10 | ICCA |
| 4 | 2.5 | fam3 | D | Lower limbs | – | > 10 | |
| 5 | 10 | fam4 | D | Upper and lower limbs |
c.649dupC p.Arg217Profs*8 |
5 to< 10 | |
| 6 | 6.7 | S | D | Lower limbs | – | < 5 | |
| 7 | 9.8 | S | D | Right limbs | – | 5 to< 10 | |
| 8 | 13 | S | D + C | Upper and lower limbs | – | 5 to< 10 | |
| 9 | 5.2 | S | D | Left lower limb | – | < 5 | |
| 10 | 5 | S | D | Lower limbs | – | < 5 | |
| 11 | 13 | S | D | Right upper limb | – | < 5 | |
| 12 | 4.7 | S | D + C | Upper and lower limbs facial | – | > 10 | |
| 13 | 13 | S | D | Upper and lower limbs | – | 5to < 10 | |
| 14 | 12.5 | S | D | Lower limbs | – | < 5 | |
| 15 | 9.6 | S | D + C | Lower limbs | – | > 10 | |
| 16 | 10.1 | S | D | Right limbs | – | 5 to< 10 | |
| 17 | 3 | S | C | Upper limbs | – | < 5 | Partial epilepsy |
| 18 | 7.6 | S | C | Upper limbs | – | 5 to< 10 | |
| 19 | 8.2 | S | D + C | Upper and lower limbs |
c.649dupC p.Arg217Profs*8 |
5 to< 10 | |
| 20 | 10 | S | D + C | Upper and lower limbs | – | 5 to< 10 |
M Male, F Female, S Sporadic, D Dystonia, C Choreoathetosis, ICCA Infantile convulsions with paroxysmal choreoathetosis
Fig. 1.
Chromatograms of the detected variants. a Sequence traces of familial PRRT2 mutation with forward and reverse sequences reveal the deletion of TCAC at position 604–607, b Sequence traces of PRRT2 mutation reveal the duplication of C at position 629, c Sequence traces of PRRT2 mutation reveal the duplication of C at position 649
Treatment effects
All enrolled patients took morning draughts of OXC, which stopped attacks in 19 patients. One sporadic patient was treated for 3 weeks but still had a < 75% reduction in attacks frequency after took the dose of 15 mg/kg·d for 1 week since the dose was increased by two times and refused further treatment. All the last 19 patients had a > 75% reduction in attacks frequency last more than 1 month, the effective dose was 5 mg/kg·d in 2 patients, 10 mg/kg·d in 13 patients, 15 mg/kg·d in 3 patients and 20 mg/kg·d in one patient. The median effective dose was 10 mg/kg·d. One patient experienced a slight rash that was alleviated with antiallergic medicines and none had serious idiosyncratic adverse effects.
Discussion
Clinical manifestations and genetic characteristics of PRRT2 mutations
The PRRT2, which encodes proline-rich transmembrane protein 2, is composed of four exons; this protein consists of 340 amino acids and contains two predicted transmembrane domains [10]. The PRRT2 is expressed primarily in the brain, particularly in the cerebral cortex and basal ganglia; this expression pattern may explain why abnormal excitability in the cortex and basal ganglia is detected in a subset of PKD patients [6]. However, the exact function of the PRRT2 remains unknown. Reports have indicated that this gene interacts with synaptosomal-associated protein 25 kDa (SNAP25) [11]. SNAP25 is a presynaptic plasma-membrane-bound protein involved in the synaptic vesicle membrane docking and fusion pathway and plays a key role in calcium-triggered neuronal exocytosis [12]. Its binding partner PRRT2 may also play a role in this process [13]. The absence or low expression of PRRT2 due to mutations in the PRRT2 may result from the loss of a transmembrane domain, which renders PRRT2 unable to anchor to membranes; such changes in PRRT2 may lead to hyperexcitability and trigger dyskinesias [13]. However, further investigation is needed to elucidate how PRRT2 mutations cause PKD.
PRRT2 mutations are present in most familial PKD patients; the most common such mutation is c.649dupC [10]. Among sporadic patients, the rate of PRRT2 mutations ranges from 20 to 45%, with c.649delC and c.649dupC as commonly observed mutations [14]. In addition to PKD patients, PRRT2 mutations have also been identified in patients with infantile convulsions with paroxysmal choreoathetosis, benign familial infantile epilepsy [15], migraine or episodic ataxia [16]. This phenomenon could explain why certain PKD patients have comorbidities such as migraine or seizures [17]. Researchers have determined that among PKD patients, younger age at symptom onset, good response to CBZ and predisposition to non-dyskinetic symptoms are significantly correlated with PRRT2 mutations [18, 19].
We enrolled a total of 20 patients. PRRT2 mutations were detected in 5 patients but not the remaining 15 patients. Four of the 5 patients positive for PRRT2 mutations had familial PKD. Differences in PRRT2 mutations between familial PKD patients and sporadic PKD patients were evaluated using unpaired Student’s t-tests or Fisher’s exact test (Table 2). We found a significantly higher positive rate of PRRT2 mutations among familial PKD patients than among sporadic PKD patients (p < 0.05); similarly, prior studies revealed that PRRT2 mutations were related to PKD, especially familial PKD [10]. PKD patients with PRRT2 mutations had more comorbidities (p < 0.05). Gender distribution and the clinical phenotypes of PKD did not differ between PKD patients with PRRT2 mutations and PKD patients without such mutations. Although many studies have reported that PKD patients with PRRT2 mutations are younger at disease onset than other PKD patients, in our study, there were no differences between these two patient groups. This finding may be attributable to the small sample sizes in our study or to differences among different populations.
Table 2.
Comparison of clinical features between the PKD patients with and without PRRT2 mutations
| patients with PRRT2 mutations | patients without PRRT2 mutations | p | |
|---|---|---|---|
| No. of subjects | 5 | 15 | |
| Male(%) | 4(80%) | 13(86.7%) | 1.000 |
| Age at onset (years) | 0.502 | ||
| Mean (SD) | 7.1(3) | 8.4(3.7) | |
| Median | 7 | 9 | |
| Main phenotype, n | 0.338 | ||
| Choreoathetosis | 2 | 2 | |
| Dystonia | 1 | 9 | |
| Mixed | 2 | 4 | |
| Laterality of dyskinesia | 0.530 | ||
| Unilateral | 0 | 4 | |
| Biateral | 5 | 11 | |
| Involved limb | 0.805 | ||
| Upper limbs | 0 | 3 | |
| Lower limbs | 2 | 6 | |
| Both | 3 | 6 | |
| Frequency of attack/day, n | 0.805 | ||
| < 5 | 2 | 6 | |
| 5–10 | 3 | 6 | |
| > 10 | 0 | 3 | |
| Comorbidity | 3 | 1 | 0.032 |
P* < 0.05
Treatment for PKD
The pathogenesis of PKD has not yet been elucidated; however, recent evidence of abnormal excitability in the cortex and basal ganglia in PKD patients supports the hypothesis that channelopathy is an underlying mechanism of PKD [20]. Moreover, certain studies report that PKD patients usually exhibit good response to antiepileptic drugs, including lamotrigine, phenytoin, valproic acid, CBZ, and OXC, all of which achieve treatment objectives through the mechanism of modulating ion channels [21].
Prior studies have suggested that a low dosage of CBZ (75–300 mg/d) can significantly improve paroxysmal dyskinesia for certain PKD patients during the first week of treatment; however, attacks will recur once the medication is withdrawn or missed [22]. Although CBZ benefits certain PKD patients, the adverse effects, which include serious idiosyncratic adverse effects, cannot be ignored. Toxic epidermal necrolysis and Stevens-Johnson syndrome are serious dermatological reactions to CBZ. The incidence of these reactions is 1 in 60,000 among Caucasians, but the risk is tenfold higher in certain Asian countries due to HLA-B1502 [23]. As a result, the use of CBZ is limited in various Asian countries, including China. As a structural derivative of CBZ, OXC mainly blocks voltage-sensitive sodium currents [24]. Unlike CBZ, OXC is not metabolized by the hepatic cytochrome-P450 enzyme system, and OXC has a lower plasma protein binding rate than CBZ; thus, OXC has fewer side effects and drug interactions [25]. OXC is rapidly and extensively reduced by cytosolic hepatic enzymes to its monohydroxylated derivative (MHD), which represents the antiepileptic agent and the active metabolite of OXC [26]. Half-lives in a healthy person are 1–5 h for OXC and 7–20 h for MHD [24]. A retrospective study addressing the use of CBZ or OXC monotherapy for PKD from 2005 to 2011 found that both CBZ and OXC had similar efficacies and tolerability. Patients experienced significant improvement with low doses of OXC (75–300 mg/d) or CBZ (50–300 mg/d), but 3 patients exhibited better tolerance after conversion from CBZ to OXC [8].
Because attacks of dystonia and choreoathetosis are triggered by sudden movements and patients may engage in more movements during the day, attacks are more likely to occur during the day than at night. Given this characteristic of PKD and the half-lives of OXC and MHD, OXC taken as a morning draught may have good efficacy and improve quality of life. This study observed the efficacy of low doses of OXC taken as a draught in the treatment of paediatric PKD patients. Prior reports have already showed that low doses of OXC are effective for PKD patients. Moreover, because attacks associated with PKD were mainly triggered by movement during the day, to decrease the frequency of drug administration and improve therapy compliance, all 20 enrolled patients took OXC as morning draughts. All but 1 of the 20 patients exhibited considerable improvement in dystonia or choreoathetosis with low doses of OXC (5–20 mg/kg·d).
Differential diagnosis and misdiagnosis of PKD patients
PKD should be distinguished from the other paroxysmal dyskineias such as paroxysmal non-kinesigenic dyskinesia (PNKD) (OMIM 118800) and paroxysmal exertion-induced dyskinesia (PED) (OMIM 612126) as the similar movement disorder could present in all of them [1]. PED need physical exercise for more long time than PKD to trigger and last time varies from 5 to 30 min [7].Unlike PKD and PED, the cause of PNKD has nothing to do with voluntary movement or exercise, attack could be triggered by caffeine, alcohol, excitement and fatigue, the symptom duration minutes to 4 h.
As a paroxysmal disease, PKD can also be misdiagnosed as epilepsy, especially partial epilepsy, given that PKD patients are conscious during dyskinesia attacks. After treatment with antiepileptic drugs, certain PKD patients may not experience attacks, which may lead doctors to mistakenly believe that epilepsy is a reliable diagnosis for these patients. Moreover, PKD patients may have seizures as a comorbidity, contributing to misdiagnoses of PKD.
Two-thirds of the patients in our group had been misdiagnosed with epilepsy; therefore, it is necessary for doctors to distinguish between PKD and epilepsy to improve diagnostic accuracy. Attacks of dyskinesia in PKD patients are triggered by sudden movements, which may help distinguish PKD from epilepsy. Video-Electroencephalogram (VEEG), which can reveal whether epileptic discharge is present during an attack, could be a major approach for the diagnosis and differential diagnosis of PKD. It is also important to identify a syndrome when PKD patients experience seizure attacks, such as infantile convulsions with paroxysmal choreoathetosis (ICCA) (OMIM 602066) or benign familial infantile epilepsy (OMIM 605751).
Conclusion
This study focuses on the clinical features and treatment of paediatric PKD patients. As a rare and paroxysmal disease, PKD can be misdiagnosed; therefore, it is necessary to enhance doctors’ knowledge of PKD and reduce the rate of erroneous diagnosis. Paediatric PKD patients have various phenotypes. PRRT2 mutations are common in familial cases, whereas additional study of the genetic mechanisms of PKD in sporadic cases is required. Attacks in paediatric PKD patients can be improved by OXC taken as morning draughts.
Acknowledgements
Not applicable.
Abbreviations
- CBZ
Carbamazepine
- ICCA
Infantile convulsions with paroxysmal choreoathetosis
- MHD
Monohydroxylated derivative
- OXC
Oxcarbazepine
- PCR
Polymerase chain reaction
- PED
Paroxysmal exertion-induced dyskinesia
- PKD
Paroxysmal kinesigenic dyskinesia
- PNKD
Paroxysmal non-kinesigenic dyskinesia
- PRRT2
Proline-rich transmembrane protein 2
- SNAP25
Synaptosomal-associated protein 25 kDa
- VEEG
Video-Electroencephalogram
Authors’ contributions
ZSZ designed the study. PG and ZLM collect data and materials. PG wrote the manuscript. All authors read and approved the final manuscript.
Authors’ information
Gang Pan is a neuropediatrician in the Children’s hospital of Fudan university.
Linmeizhang is a neuropediatrician in the Children’s hospital of Fudan university. She is also Associate Professor in the Department of pediatrics at Fudan university.
Shuizhen Zhou works as a neuropediatrician and the Director of the department of neurology at Children’s hospital of Fudan university. She is also Full Professor in the Department of pediatrics at Fudan university.
Funding
No funding.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of Children’s Hospital of Fudan University, No. 2017 (15). Written consent to participate was obtained from all participants. Consent was obtained from a parent or guardian on behalf of any participants under the age of 16.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Gang Pan, Email: greghouse@live.cn.
Linmei Zhang, Email: Linmeizhang@outlook.com.
Shuizhen Zhou, Phone: +86-021-64932107, Email: szzhou@shmu.edu.cn.
References
- 1.Jankovic J, Demirkiran M. Classification of paroxysmal dyskinesias and ataxias. Adv Neurol. 2002;89:387–400. [PubMed] [Google Scholar]
- 2.Bennett LB, Roach ES, Bowcock AM. A locus for paroxysmal kinesigenic dyskinesia maps to human chromosome 16. Neurology. 2000;54(1):125–130. doi: 10.1212/wnl.54.1.125. [DOI] [PubMed] [Google Scholar]
- 3.Bruno MK, Hallett M, Gwinn-Hardy K, Sorensen B, Considine E, Tucker S, et al. Clinical evaluation of idiopathic paroxysmal kinesigenic dyskinesia: new diagnostic criteria. Neurology. 2004;63(12):2280–2287. doi: 10.1212/01.wnl.0000147298.05983.50. [DOI] [PubMed] [Google Scholar]
- 4.Chen WJ, Lin Y, Xiong ZQ, Wei W, Ni W, Tan GH, et al. Exome sequencing identifies truncating mutations in PRRT2 that cause paroxysmal kinesigenic dyskinesia. Nat Genet. 2011;43(12):1252–1255. doi: 10.1038/ng.1008. [DOI] [PubMed] [Google Scholar]
- 5.Li J, Zhu X, Wang X, Sun W, Feng B, Du T, et al. Targeted genomic sequencing identifies PRRT2 mutations as a cause of paroxysmal kinesigenic choreoathetosis. J Med Genet. 2012;49(2):76–78. doi: 10.1136/jmedgenet-2011-100635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mir P, Huang YZ, Gilio F, Edwards MJ, Berardelli A, Rothwell JC, et al. Abnormal cortical and spinal inhibition in paroxysmal kinesigenic dyskinesia. Brain. 2005;128:291–299. doi: 10.1093/brain/awh342. [DOI] [PubMed] [Google Scholar]
- 7.Bhatia KP. Paroxysmal dyskinesias. Mov Disord. 2011;26(6):1157–1165. doi: 10.1002/mds.23765. [DOI] [PubMed] [Google Scholar]
- 8.Yang Y, Su Y, Guo Y, Ding Y, Xu S, Jiang Y, et al. Oxcarbazepine versus carbamazepine in the treatment of paroxysmal kinesigenic dyskinesia. Int J Neurosci. 2012;122(12):719–722. doi: 10.3109/00207454.2012.715109. [DOI] [PubMed] [Google Scholar]
- 9.Zhang LM, An Y, Pan G, Ding YF, Zhou YF, Yao YH, et al. Reduced penetrance of PRRT2 mutation in a Chinese family with infantile convulsion and Choreoathetosis syndrome. J Child Neurol. 2015;30(10):1263–1269. doi: 10.1177/0883073814556887. [DOI] [PubMed] [Google Scholar]
- 10.Liu XR, Wu M, He N, Meng H, Wen L, Wang JL, et al. Novel PRRT2 mutations in paroxysmal dyskinesia patients with variant inheritance and phenotypes. Genes Brain Behav. 2013;12(2):234–240. doi: 10.1111/gbb.12008. [DOI] [PubMed] [Google Scholar]
- 11.Zhao N, Hashida H, Takahashi N, Sakaki Y. Cloning and sequence analysis of the human SNAP25 cDNA. Gene. 1994;145(2):313–314. doi: 10.1016/0378-1119(94)90027-2. [DOI] [PubMed] [Google Scholar]
- 12.Jarvis SE, Zamponi GW. Masters or slaves? Vesicle release machinery and the regulation of presynaptic calcium channels. Cell Calcium. 2005;37(5):483–488. doi: 10.1016/j.ceca.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 13.Lamperti C, Invernizzi F, Solazzi R, Freri E, Carella F, Zeviani M, et al. Clinical and genetic features of paroxysmal kinesigenic dyskinesia in Italian patients. Eur J Paediatr Neurol. 2016;20(1):152–157. doi: 10.1016/j.ejpn.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Groffen AJ, Klapwijk T, van Rootselaar AF, Groen JL, Tijssen MA. Genetic and phenotypic heterogeneity in sporadic and familial forms of paroxysmal dyskinesia. J Neurol. 2013;260(1):93–99. doi: 10.1007/s00415-012-6592-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heron SE, Grinton BE, Kivity S, Afawi Z, Zuberi SM, Hughes JN, et al. PRRT2 mutations cause benign familial infantile epilepsy and infantile convulsions with choreoathetosis syndrome. Am J Hum Genet. 2012;90(1):152–160. doi: 10.1016/j.ajhg.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gardiner AR, Bhatia KP, Stamelou M, Dale RC, Kurian MA, Schneider SA, et al. PRRT2 gene mutations: from paroxysmal dyskinesia to episodic ataxia and hemiplegic migraine. Neurology. 2012;79(21):2115–2121. doi: 10.1212/WNL.0b013e3182752c5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gardiner Alice R., Jaffer Fatima, Dale Russell C., Labrum Robyn, Erro Roberto, Meyer Esther, Xiromerisiou Georgia, Stamelou Maria, Walker Matthew, Kullmann Dimitri, Warner Tom, Jarman Paul, Hanna Mike, Kurian Manju A., Bhatia Kailash P., Houlden Henry. The clinical and genetic heterogeneity of paroxysmal dyskinesias. Brain. 2015;138(12):3567–3580. doi: 10.1093/brain/awv310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan LC, Methawasin K, Teng EW, Ng AR, Seah SH, Au WL, et al. Clinico-genetic comparisons of paroxysmal kinesigenic dyskinesia patients with and without PRRT2 mutations. Eur J Neurol. 2014;21(4):674–678. doi: 10.1111/ene.12142. [DOI] [PubMed] [Google Scholar]
- 19.Youn J, Kim JS, Lee M, Lee J, Roh H, Ki CS, et al. Clinical manifestations in paroxysmal kinesigenic dyskinesia patients with proline-rich transmembrane protein 2 gene mutation. J Clin Neurol. 2014;10(1):50–54. doi: 10.3988/jcn.2014.10.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Margari L, Presicci A, Ventura P, Margari F, Perniola T. Channelopathy: hypothesis of a common pathophysiologic mechanism in different forms of paroxysmal dyskinesia. Pediatr Neurol. 2005;32(4):229–235. doi: 10.1016/j.pediatrneurol.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 21.Mink JW. Treatment of paroxysmal dyskinesias in children. Curr Treat Options Neurol. 2015;17(6):350. doi: 10.1007/s11940-015-0350-9. [DOI] [PubMed] [Google Scholar]
- 22.Chillag KL, Deroos ST. Oxcarbazepine use in paroxysmal kinesigenic dyskinesia: report on four patients. Pediatr Neurol. 2009;40(4):295–297. doi: 10.1016/j.pediatrneurol.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 23.Gierbolini J, Giarratano M, Benbadis SR. Carbamazepine-related antiepileptic drugs for the treatment of epilepsy - a comparative review. Expert Opin Pharmacother. 2016;17(7):885–888. doi: 10.1517/14656566.2016.1168399. [DOI] [PubMed] [Google Scholar]
- 24.Bang LM, Goa KL. Spotlight on oxcarbazepine in epilepsy. CNS Drugs. 2004;18(1):57–61. doi: 10.2165/00023210-200418010-00006. [DOI] [PubMed] [Google Scholar]
- 25.Schmidt D, Elger CE. What is the evidence that oxcarbazepine and carbamazepine are distinctly different antiepileptic drugs? Epilepsy Behav. 2004;5(5):627–635. doi: 10.1016/j.yebeh.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 26.Flesch G. Overview of the clinical pharmacokinetics of oxcarbazepine. Clin Drug Investig. 2004;24(4):185–203. doi: 10.2165/00044011-200424040-00001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.