Abstract
Background
The rapid decrease in international funding for HIV/AIDS has been challenging for many nations to effectively mobilize and allocate their limited resources for HIV/AIDS programs. Economic evaluations can help inform decisions and strategic planning. This study aims to examine the trends and patterns in economic evaluation studies in the field of HIV/AIDS and determine their research landscapes.
Methods
Using the Web of Science databases, we synthesized the number of papers and citations on HIV/AIDS and economic evaluation from 1990 to 2017. Collaborations between authors and countries, networks of keywords and research topics were visualized using frequency of co-occurrence and Jaccards’ similarity index. A Latent Dirichlet Allocation (LDA) analysis to categorize papers into different topics/themes.
Results
A total of 372 economic evaluation papers were selected, including 351 cost-effectiveness analyses (CEA), 11 cost-utility analyses (CUA), 12 cost-benefit analyses (CBA). The growth of publications, their citations and usages have increased remarkably over the years. Major research topics in economic evaluation studies consisted of antiretroviral therapy (ART) initiation and treatment; drug use prevention interventions and prevention of mother-to-child transmission interventions. Moreover, lack of contextualized evidence was found in specific settings with high burden HIV epidemics, as well as emerging most-at-risk populations such as trans-genders or migrants.
Conclusion
This study highlights the knowledge and geographical discrepancies in HIV/AIDS economic evaluation literature. Future research directions are also informed for advancing economic evaluation in HIV/AIDS research.
Keywords: HIV/AIDS, Health economics, Economic evaluation, Bibliometric, Content analysis
Background
Global efforts to put an end of the HIV/AIDS epidemic in 2030 require extraordinary amounts of investments in both international and national levels [1]. The latest global statistics in 2019 reported that in 2018, more than 37.9 million people are currently living with HIV/AIDS, and 770 thousand people died due to AIDS-related diseases [2]. African countries continue to have the highest number of people living with HIV (PLWH) with 27.8 million, following Asian and the Pacific region with 5.9 million [2]. It has been estimated that from 2000 to 2015, worldwide expenditures on HIV/AIDS totaled US$ 562.6 billion, of which national expenditure accounted for 57.6% [1]. The Joint United Nations Programme on HIV/AIDS (UNAIDS) estimates that by 2020, total resources needed for HIV/AIDS responses in low and middle-income countries (LMICs) will be a sum of US$ 26.2 billion, which is US$ 4.9 billion higher than the investment in 2017 (US$ 21.3 billion) [3]. Filling this financial resource gap in these countries becomes a significant challenge as they are shifting to self-sustain financing HIV/AIDS programs due to a rapid decrease of foreign aids [3–5]. With limited available resources, selecting optimal allocation strategies are vital to achieving the highest benefits with the lowest costs, or in other words, focus on the right population, in the right place, and at the right time [6–8].
Economic evaluations can support this decision-making process by systematically quantifying and comparing the costs and outcomes of different interventions or health programs. Economic evaluation has been defined as “the comparative analysis of alternative courses of action in terms of both their costs and consequences” [9]. There are three primary forms of economic evaluation: cost-effectiveness analysis (CEA), cost-benefit analysis (CBA) and cost-utility analysis (CUA) [9]. They are distinguished by the measure of outcomes. The first form measures natural units of effects (e.g., new HIV infection averted or prevented), while the second form evaluates the outcomes in monetary terms, and the third form assesses the effectiveness in terms of Disability-adjusted life years (DALYs) or Quality-adjusted life years (QALYs) [9–11]. In the literature, economic evaluation is proposed as a powerful tool to assist in prioritization and scarce resources allocation [8, 12, 13]. In the field of HIV/AIDS, the number of economic evaluation studies significantly increase in recent years with a wide range of topics from prevention (e.g., behavior risk reduction, HIV testing and screening, pre-prophylaxis exposure, or prevention of mother-to-child HIV transmission) [8, 14–18] to treatment and care (e.g., ART alone, ART with other medications, or adherence support) [19–22]. The rapid development of economic evaluation studies in this field requires a further assessment to understand the knowledge gap and propose future research directions.
Importantly, one question that should be raised is about the applicability and transferability of the economic evaluation studies from one setting to others, considering both technical and contextualization aspects. Ramos et al. indicated that scientific production on HIV was dominated by the United States of America (USA) and Western Europe (accounted for 83% of total publications in 2003), while little empirical evidence was available in the most severe HIV-affected regions such as Sub-Sahara Africa or South East Asia [23]. This finding was also confirmed by other narrative and systematic reviews on economic evaluation in HIV/AIDS [7, 8, 17, 24–26]. A prior analysis in some low- and middle-income countries (LMICs) found that human capacity was a major limiting attributed to the unmet need of health economic evidence for decision-making process [27]. Indeed, countries with lower human capacity may be beneficial if they can adapt and apply the economic evaluation evidence created from neighboring nations in the same region, or with the similar socioeconomic, health system, and decision-making processes [28, 29]. Thus, examining collaboration networks among countries is helpful on the transferability of economic evaluation evidence and the enhancement of the countries’ capacities to build economic evaluation programs in the field of HIV/AIDS.
Bibliometric analysis is a useful tool to explore the research gaps and collaboration networks in a particular research field [30, 31]. This method informs objective data about scientific publications in both quantity and quality perspectives [32]. Bibliometric studies show the development of scientific publications over time, including the number of publications; the emergence of new scientific terms and journals; topics, subject areas and contents of research; and the impact of research via citations and co-citations. Moreover, this approach enables scholars to understand the collaboration patterns by identifying the geographic distribution and co-authorships among institutions and countries [30, 31]. Analyzing these characteristics would help to figure out the current state and further agenda for economic evaluation in HIV/AIDS research, which can be eventually used to advance these research areas.
Previously, several papers attempted to provide the health economic research patterns in HIV/AIDS. For example, Youle et al. searched five databased and extracted 79 economic studies (including cost analysis and economic evaluations) published from 1985 to 1998 [33]. Other two studies were conducted by Beck et al. to review publications about cost of HIV/AIDS treatment and care [34, 35]. However, to date, little is known about the patterns of research development and scopes in scientific publications, as well as collaborations in economic evaluation studies of HIV/AIDS interventions and programs. This study aims to examine the trends and patterns in economic evaluation studies in the field of HIV/AIDS and determine their research landscapes.
Methods
Search strategy
The Web of Science (WoS) was employed to collect research articles regarding economic evaluations in HIV/AIDS. We preferred WoS instead of other databases namely Scopus or MEDLINE due to its useful in examining research disciplines, which could not be performed in other databases. In addition, the WoS database encompassed high quality scientific journals, while other databases consisted of journals with varied quality [23–25]. The WoS also allowed us to conduct advanced search as well as filter the result according to specific criteria in order to assess the research productivity in different subgroups. In this study, we concentrated on publications regarding economic evaluations in HIV/AIDS published until December 31st, 2017 in the WoS journals. We did not include 1) non-English literature; 2) grey literature, conference proceedings, or books/book chapters. We also excluded narrative reviews or systematic reviews or meta-analysis. The search strategy was performed in three steps:
First, we combined the following terms to extract publications about HIV/AIDS using option “Topic”: HIV; human-immunodeficiency-virus; AIDS; Acquired-Immune-Deficiency-Syndrome
Second, used search term: “cost-effectiveness”, “cost effectiveness”, “cost-benefit”, “cost benefit”, “cost utility” or “cost-utility” in the Title or Abstract to extract publications about economic evaluation.
Final, we screened the titles and abstracts of these publications according to eligible and exclusion criteria in order to extract only those meeting our inclusion criteria.
Data extraction
Publication data were downloaded from the WoS comprising all necessary information about authors’ names, title of papers, journal names, keywords, institutional affiliations, the frequency of citation, subject category, usage (number of downloads) and abstracts. All data were collected and synthesized using Microsoft Excel to check for errors before further analysis. Standardized procedures were developed and performed by two researchers to check for any discrepancies in author names and affiliations, then make necessary changes to make the search results consistent. Disagreements between the two researchers were resolved by discussing with a senior researcher. After having correct data, we screened the titles and abstracts, and excluded publications which were: 1) not original articles and reviews; 2) not published in English; 3) not about HIV/AIDS. Figure 1 shows the results of the searching process. The final dataset was transferred to a data file to be further analyzed using STATA version 14.0 (STATACorp., Texas, the USA).
Fig. 1.
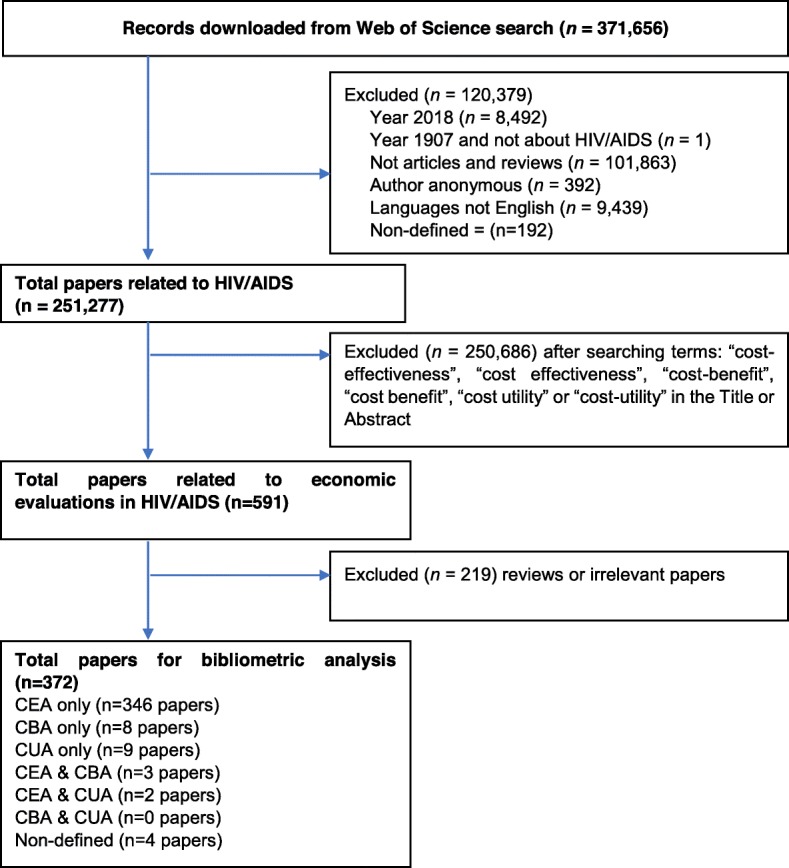
Selection of papers
Data analysis
We described some fundamental characteristics of publications, which consisted of years of publication, the number of papers per country/per year, total citations up to 2017, mean citation rate per year, total usage in the last 6 months/5 years, and mean use rate the last 6 months/5 years. We used Circos platform to draw network graphs to figure the collaboration networks among countries using co-authorships data [27]. This tool was originally used to figure the variations of genome [27]. We used the VOSviewer (version 1.6.8, Center for Science and Technology, Leiden University, the Netherlands) to illustrated networks of co-occurrence keywords. By using STATA version 14, we conducted a Latent Dirichlet Allocation (LDA) analysis to categorize papers into different topics/themes [36–40]. Two researchers reviewed all titles and abstracts of papers in each topic/theme and identify the content of the ten topics. Disagreements were resolved by involving opinions from a senior researcher. Jaccard’s similarity index was used to determine research topics or terms that most frequently co-occur with each other.
Results
Figure 1 reveals the searching and selection processes. Among 250,270 papers about HIV/AIDS, 372 papers are about economic evaluations in HIV/AIDS.
Table 1 outlines some basic characteristics of the selected publications. Overall, the number of articles studying economic or finance perspective in the field of HIV/AIDS, as well as the total citations and mean cite rate per year increased significantly from period 1991–1997 to 1998–2001 albeit a decrease in the period 2002–2005. Notably, the total usage (total number of downloads) and the mean use rate in the last 5 years of papers published in 2013 were the highest compared with other years.
Table 1.
General characteristics of publications
| Year published | Total number of papers | Total citations | Mean cite rate per year | Total usage last 6 montha | Total usage last 5 yearsa | Mean use rate last 6 monthb | Mean use rate per year in last 5 yearb |
|---|---|---|---|---|---|---|---|
| 2017 | 23 | 25 | 1.09 | 36 | 82 | 1.57 | 0.71 |
| 2016 | 26 | 99 | 1.90 | 13 | 138 | 0.50 | 1.06 |
| 2015 | 23 | 144 | 2.09 | 9 | 143 | 0.39 | 1.24 |
| 2014 | 25 | 224 | 2.24 | 8 | 170 | 0.32 | 1.36 |
| 2013 | 28 | 369 | 2.64 | 10 | 285 | 0.36 | 2.04 |
| 2012 | 26 | 494 | 3.17 | 3 | 211 | 0.12 | 1.62 |
| 2011 | 26 | 396 | 2.18 | 6 | 177 | 0.23 | 1.36 |
| 2010 | 16 | 498 | 3.89 | 1 | 105 | 0.06 | 1.31 |
| 2009 | 10 | 119 | 1.32 | 1 | 23 | 0.10 | 0.46 |
| 2008 | 14 | 487 | 3.48 | 1 | 66 | 0.07 | 0.94 |
| 2007 | 11 | 171 | 1.41 | 0 | 34 | 0.00 | 0.62 |
| 2006 | 21 | 527 | 2.09 | 10 | 107 | 0.48 | 1.02 |
| 2005 | 10 | 765 | 5.88 | 2 | 43 | 0.20 | 0.86 |
| 2004 | 13 | 362 | 1.99 | 4 | 45 | 0.31 | 0.69 |
| 2003 | 8 | 438 | 3.65 | 3 | 32 | 0.38 | 0.80 |
| 2002 | 3 | 60 | 1.25 | 1 | 16 | 0.33 | 1.07 |
| 2001 | 17 | 1023 | 3.54 | 1 | 68 | 0.06 | 0.80 |
| 2000 | 17 | 880 | 2.88 | 2 | 67 | 0.12 | 0.79 |
| 1999 | 15 | 626 | 2.20 | 1 | 39 | 0.07 | 0.52 |
| 1998 | 14 | 519 | 1.85 | 1 | 24 | 0.07 | 0.34 |
| 1997 | 7 | 507 | 3.45 | 2 | 40 | 0.29 | 1.14 |
| 1996 | 7 | 250 | 1.62 | 0 | 10 | 0.00 | 0.29 |
| 1995 | 3 | 69 | 1.00 | 0 | 2 | 0.00 | 0.13 |
| 1994 | 5 | 87 | 0.73 | 2 | 4 | 0.40 | 0.16 |
| 1993 | 2 | 27 | 0.54 | 0 | 0 | 0.00 | 0.00 |
| 1992 | 1 | 10 | 0.38 | 0 | 0 | 0.00 | 0.00 |
| 1991 | 1 | 109 | 4.04 | 0 | 0 | 0.00 | 0.00 |
aTotal usage: Total number of downloads
bUse rate: Total number of downloads/Total number of papers
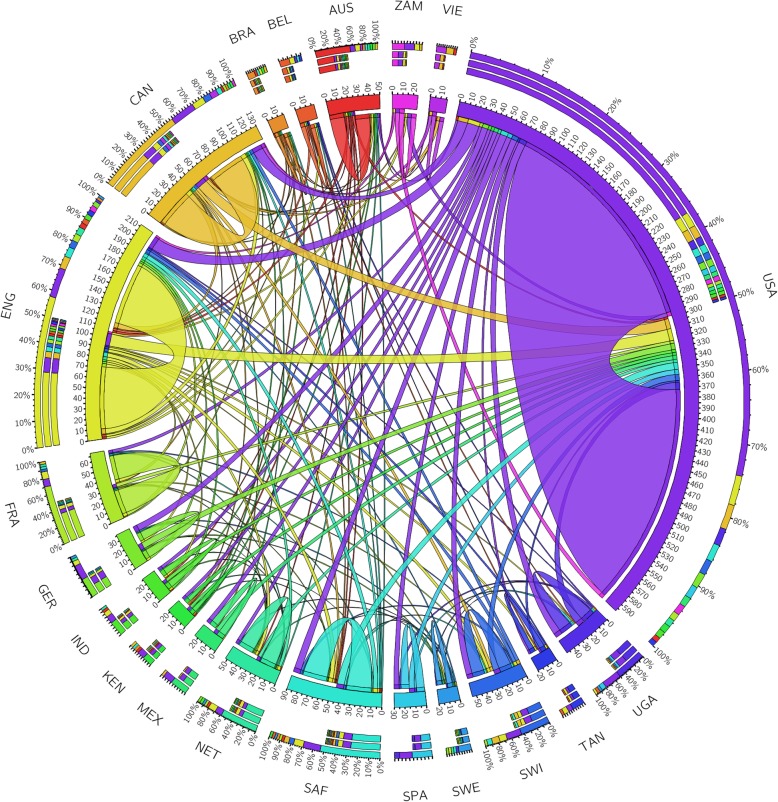
Figure 2 reveals the collaboration networks between the top 20 contributing countries. Overall, 46 countries contributed to at least one article in the final dataset with 372 papers, of which the United States of America (USA) and England had the highest number of publications (306 and 118 papers, respectively), following by Canada (66 papers), South Africa (45 papers), and France (35 papers). In top 10 countries with the highest number of publications, only South Africa and Uganda had hyperendemic and generalized HIV/AIDS epidemic, respectively, while others had concentrated (such as the USA or England) or low-level epidemic (such as France). Meanwhile, among the top 20 country, only South Africa, Uganda, Zambia, Kenya and Tanzania had hyperendemic or generalized epidemic. England and the USA had the highest volume of collaborations with 27 and 22 countries, respectively. These were followed by Canada (13 countries), South Africa (11 countries) and Australia (11 countries).
Fig. 2.
Collaboration network between the top 20 countries by the number of publications. The outer rim reflects the volume of collaborations between one country with other countries in the top 20, showing collaboration among countries. Abbreviation: USA, the United States of America; ENG, England; GER, Germany; AUS, Australia; NET, Netherlands; CAN, Canada; SAF, South Africa; FRA, France; SWI, Switzerland; UGA, Uganda; SPA, Spain; MEX, Mexico; IND, India; ZAM, Zambia, KEN, Kenya, TAN, Tanzania; BEL, Belgium; SWE, Sweden; BRA, Brazil; VIE, Vietnam
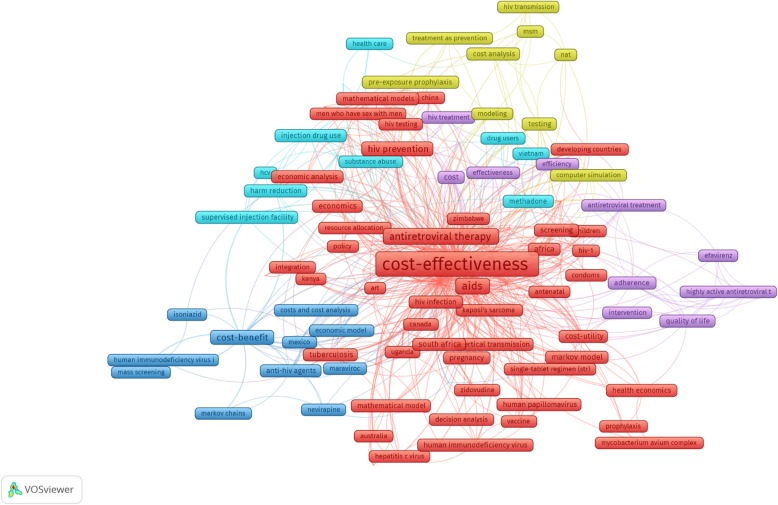
To illustrate the scopes of studies and development of research landscapes, we performed abstracts and keywords analysis. Figure 3 reveals five major clusters from 121 most frequent keywords co-occurrence. Each keyword had to appear at least 2 times. Of which, there were five greatest clusters of keywords: 1) the red cluster indicated topics of cost-effectiveness studies such as HIV and Sexually Transmitted Infections (STIs) prevention or HIV treatment in developing countries; 2) the yellow cluster indicated interventions using ART as prevention (such as pre-exposure prophylaxis or treatment as prevention approach), especially in men who have sex with men; 3) the blue cluster referred to the economic evaluation studies on injection drug use; 4) the navy blue cluster referred to topics of cost-benefit studies, focusing on HIV screening and treatment; 5) the purple cluster covered the interventions to improve adherence and quality of life in HIV patients.
Fig. 3.
Co-occurrence of most frequent author’s keywords. Note: the colors refer to different clusters; the nodes size reflects keywords’ occurrences; lines’ thickness was visualized according to the strength of the relationship between two keywords
Table 2 lists the top 10 research topics as well as the 20 most frequent keywords in each topic that emerged from the LDA for contents of titles/abstracts. The top three topics with highest number of publications were 1) Economic evaluations for ART interventions; 2) Economic evaluations for Drug use prevention interventions (such as harm reduction or methadone maintenance treatment); and 3) Economic evaluation for Prevention of mother-to-child transmission interventions.
Table 2.
Ten research topics emerged classified by LDA for titles and abstracts’ contents
| No | Topic | Most frequent terms | N | Percent |
|---|---|---|---|---|
| 1 | ART intervention | cost-effectiveness; antiretroviral; therapy; patients; analysis, clinical; effectiveness; treatment; objective; infection, highly; regimens; study; HIV-infected; combination, trial; active; HAART; HIV-1; adults | 45 | 13.2% |
| 2 | Drug use prevention intervention | cost-effectiveness; treatment; methadone; maintenance; injection, users; health; programs; study; intervention, supervised; drugs; prevention; reduction; background, opioid; analysis; substance; abuse; injecting | 41 | 12.0% |
| 3 | Prevention of mother-to-child transmission intervention | cost-effectiveness; transmission; Africa; objective; model; south; women; prevent; methods; effectiveness; sub-Saharan; mother-to-child; prevention; strategies; analysis; design; reduce; health; interventions; estimate | 37 | 10.8% |
| 4 | Cancer screening and testing intervention in HIV/AIDS patients | Human; virus; immunodeficiency; cost-effectiveness; screening; Hepatitis; testing; blood; infection; study; compared; antibody; cancer; background; tests; cervical; donations; purpose; papillomavirus; determine | 36 | 10.5% |
| 5 | ART intervention in resource-limited settings | antiretroviral; therapy; cost-effectiveness; settings; background, treatment; monitoring; health; Africa; resource-limited, clinical; sub-Saharan; guidelines; viral; resistance, world; different; first-line; organization; countries | 35 | 10.2% |
| 6 | HIV counseling and testing intervention | testing; screening; cost-effectiveness; united; states, analysis; objective; voluntary; counseling; design, effectiveness; disease; routine; impact; evaluate, infection; patients; expanded; benefits; objectives | 33 | 9.6% |
| 7 | Condom distribution intervention | cost-effectiveness; analysis; transmitted; workers; sexually, infections; female; background; south; condom, program; impact; Africa; cost-benefit; cost-utility, India; health; evidence; diseases; intervention | 32 | 9.4% |
| 8 | HIV-related respiratory diseases treatment and prevention | Effectiveness; tuberculosis; background; HIV-infected; patients; strategies; infection; efficacy; diagnosis; mortality; Individuals; rapid; diagnostic; study; persons; early; preventive; infected; isoniazid; Uganda | 28 | 8.2% |
| 9 | Pre and post-exposure prophylaxis interventions | cost-effectiveness; prophylaxis; economic; impact; evaluation, prevention; sexual; background; pre-exposure; intervention, program; potential; objective; post-exposure; exposure, Zambia; couples; following; service; methods | 28 | 8.2% |
| 10 | HIV/AIDS vaccination intervention | costs; prevention; HIV/aids; cost-effectiveness; effectiveness, interventions; disease; economic; treatment; estimates, study; comparing; important; medical; policy; using; healthcare; integrated; incremental; vaccine | 27 | 7.9% |
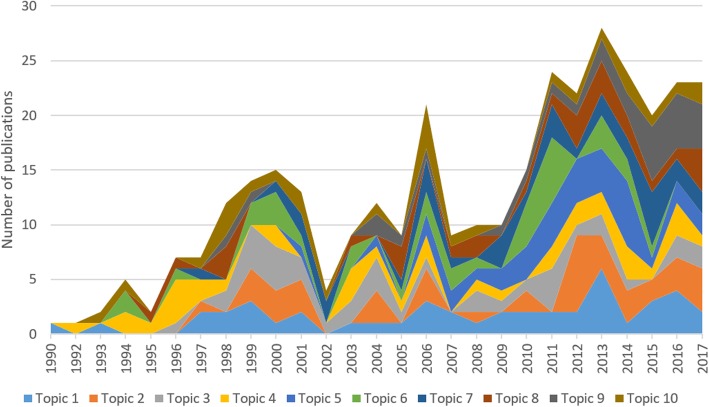
Figure 4 showed the trend of research topics in the whole period. The first paper published in 1990 is belonged to Topic 1, following by a publication in 1992 about Topic 3. Since then, Topic 1 and Topic 2 were still paid the highest attention. However, in the last 3 years, publications in the Topic 9 “Pre and post-exposure prophylaxis interventions”, following by Topic 1, Topic 2 and Topic 5, have been raised significantly compared to other topics.
Fig. 4.
Changes in research topics development
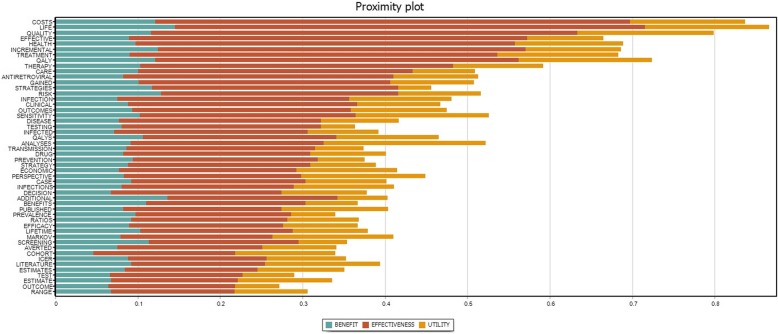
Figure 5 describes the most frequent terms co-occurring with “cost-effectiveness analysis” (CEA), “cost-utility analysis” (CUA), “cost-benefit analysis” (CBA) terms in the content analysis of all abstracts. CBA has been identified that frequently co-occurred with strategies for risk reduction and screening and testing services. This method was more likely to be treated as an additional method along with CEA as the terms “life,” “quality,” “QALYs” were frequently presented. The Markov model seems to be a more common method in CBA compared to the Decision Tree. Meanwhile, in terms of CEA, HIV treatment and care were perhaps the most common topic, following by risk reduction strategies (especially drug use), and HIV screening and testing. QALY gained was the most common outcome, followed by infectious cases averted. Decision Tree and Markov Model were the two most common methods with similar shares in total publications.
Fig. 5.
Proximity Plot of “cost-effectiveness analysis” (CEA), “cost-utility analysis” (CUA), “cost-benefit analysis” (CBA) terms with top 50 most frequent concurrence terms in 372 Economic Evaluation Studies’ abstracts. The x-axis shows the Jaccard coefficient which reflect similarities amning certain sample sets. It refers to the range of the intersection divided by the range of the union of the sample sets
Similar to CEA, treatment was the most common topic in CUA, following by risk reduction and care service. The Markov model was more frequently co-occurring with CUA compared to the Decision tree. Published papers and cohort studies were more likely to be the most common sources of data for all three forms of economic evaluation.
Top 20 most cited papers on economic evaluation in HIV populations are presented in Table 3. These studies primarily focused on medications for HIV treatment and care, behavior risk reduction (drug use), and HIV/Cancer screening and testing. Moreover, some studies concentrated on evaluating interventions to address co-infections such as Hepatitis C, Tuberculosis and other sexually transmitted infections and opportunistic infections. Other studies focused on different sub-populations such as breastfeeding women and men who have sex with men.
Table 3.
Top 20 most cited papers among economic evaluation publications
| # | Title | Journal | Citations | Years | Cite rate per year |
|---|---|---|---|---|---|
| 1 | Expanded screening for HIV in the United States - An analysis of cost-effectiveness [41] | New England Journal Of Medicine | 369 | 2005 | 28.38 |
| 2 | The cost effectiveness of combination antiretroviral therapy for HIV disease [42] | New England Journal Of Medicine | 349 | 2001 | 20.53 |
| 3 | Cost-effectiveness of voluntary HIV-1 counselling and testing in reducing sexual transmission of HIV-1 in Kenya and Tanzania [43] | Lancet | 250 | 2000 | 13.89 |
| 4 | Cost effectiveness of single-dose nevirapine regimen for mothers and babies to decrease vertical HIV-1 transmission in sub-Saharan Africa [44] | Lancet | 196 | 1999 | 10.32 |
| 5 | The cost-effectiveness of NAT for HIV, HCV, and HBV in whole-blood donations [45] | Transfusion | 184 | 2003 | 12.27 |
| 6 | Use of genotypic resistance testing to guide HIV therapy: Clinical impact and cost-effectiveness [46] | Annals Of Internal Medicine | 169 | 2001 | 9.94 |
| 7 | Updates of cost of illness and quality of life estimates for use in economic evaluations of HIV prevention programs [47] | Journal Of Acquired Immune Deficiency Syndromes And Human Retrovirology | 167 | 1997 | 7.95 |
| 8 | The cost-effectiveness of preventing AIDS-related opportunistic infections [48] | JAMA-Journal Of The American Medical Association | 163 | 1998 | 8.15 |
| 9 | HIV transmission and the cost-effectiveness of methadone maintenance [49] | American Journal Of Public Health | 134 | 2000 | 7.44 |
| 10 | Cost-Effectiveness of Serum Cryptococcal Antigen Screening to Prevent Deaths among HIV-Infected Persons with a CD4(+) Cell Count <= 100 Cells/mL Who Start HIV Therapy in Resource-Limited Settings [50] | Clinical Infectious Diseases | 130 | 2010 | 16.25 |
| 11 | Should resistance testing be performed for treatment-naive HIV-infected patients? A cost-effectiveness analysis [51] | Clinical Infectious Diseases | 125 | 2005 | 9.62 |
| 12 | Cost-effectiveness of improved treatment services for sexually transmitted diseases in preventing HIV-1 infection in Mwanza Region, Tanzania [52] | Lancet | 124 | 1997 | 5.90 |
| 13 | Cost-effectiveness of screening for anal squamous intraepithelial lesions and anal cancer in human immunodeficiency virus-negative homosexual and bisexual men | American Journal Of Medicine | 121 | 2000 | 6.72 |
| 14 | Positive and negative life events after counselling and testing: the Voluntary HIV-1 Counselling and Testing Efficacy Study [53] | AIDS | 112 | 2001 | 6.59 |
| 15 | Modeling the impact of HIV chemoprophylaxis strategies among men who have sex with men in the United States: HIV infections prevented and cost-effectiveness [54] | AIDS | 110 | 2008 | 11.00 |
| 16 | Cost-Effectiveness Of Low-Dose Zidovudine Therapy For Asymptomatic Patients With Human-Immunodeficiency-Virus (HIV) Infection [55] | Annals Of Internal Medicine | 109 | 1991 | 4.04 |
| 17 | Cost-effectiveness of expanded human immunodeficiency virus-testing protocols for donated blood [56] | Transfusion | 105 | 1997 | 5.00 |
| 18 | The cost-effectiveness of buprenorphine maintenance therapy for opiate addiction in the United States [57] | Addiction | 98 | 2001 | 5.76 |
| 19 | The cost-effectiveness of HLA-B*5701 genetic screening to guide initial antiretroviral therapy for HIV [58] | AIDS | 89 | 2008 | 8.90 |
| 20 | Is antenatal syphilis screening still cost effective in sub-Saharan Africa [59] | Sexually Transmitted Infections | 85 | 2003 | 5.67 |
Discussion
This study mapped the trends and patterns of economic evaluation publications in the field of HIV/AIDS, and hence it enriches the previous bibliometric studies regarding health economics in HIV/AIDS research [33–35]. Our study captured the growth of these publications as well as their usage in the last 5 years, suggesting the critical role of this topic in HIV/AIDS research. We also observed the overwhelming majority of CEA compared to CUA and CBA; and the predominance of the USA in performing economic evaluation studies in HIV/AIDS. Moreover, we applied an advanced method to understand thoroughly the content of keywords and abstracts, indicating the development of research domains as well as landscapes in this field and exploring the research gaps. The findings would be used to recommend further directions in order to advance this research area.
By analyzing the contents of abstracts, we could identify the most common economic evaluation research topics in the field of HIV/AIDS. Economic evaluation had been applied in various topics, including prevention (such as harm reduction, condom use or pre and post-exposure prophylaxis); HIV-related clinical services (testing and counselling services; ART, or vaccine); or co-infections (tuberculosis, hepatitis C, or HPV). Nonetheless, these results also imply some research gaps that have not been fully investigated. For instance, little economic evaluation evidence was found for transgender or migrant people, who are at very high risk of HIV infection [60, 61]. Also, there was a lack of economic evaluation evidence in structural interventions such as policy experiments or integrated/decentralized HIV-related service models, especially for stigmatized populations such as men who have sex with men [8, 62]. As infecting HIV requires lifelong treatment, evaluations in effectiveness and cost-effectiveness of interventions reducing the burden of aging and non-communicable diseases in HIV patients are also necessary [63–65]. Furthermore, our results showed a lack of economic evaluation evidence on the intervention using theory-driven eHealth approach, which is increasingly performed to prevent HIV risk behaviors, promote HIV testing and support HIV treatment [66, 67]. Last, but not least, the studies on the affordability were lacking. Policymakers with short-term constrained resources may not be able to invest in the high-cost interventions despite their superior health benefits [68]. Therefore, information about the affordability, feasibility and acceptability of the interventions should be incorporated into the economic evaluation studies. This information will support policymakers optimally allocating the available resource.
In this study, we found that CEA was the most common analytical method for economic evaluation, which is in line with other studies investigating the patterns of economic evaluations in general [69] and in pediatric research [70]. CEA uses disease-specific clinical, biomedical indicators or non-compound measures of survival as outcomes, for example, cost per infection averted/prevented or cost per life year saved; hence, contextualized features are not fully reflected [12]. Meanwhile, CUA is the gold standard for economic evaluation, since it uses utility-based units as outcomes (such as cost per QALYs gained or DALYs averted), which enables the comparison of various type of interventions and disease conditions. A previous review indicated that QALYs were more popular in high income countries, while low and low-middle income countries mostly used DALYs averted [71]. A key benefit of the utility-based units CUA uses is that they consider both the patients’ quality of life/health and the effects of interventions on mortality, which are more important than purely clinical outcomes often used in CEA. However, in practice, many studies in the field of HIV/AIDS reported both clinical outcomes and QALYs/DALYs outcomes; and they used the term “cost-effectiveness analysis” instead of “cost-utility analysis” [7, 8, 17, 24–26]. In CBA it is necessary to quantify the monetary value of the outcomes of healthcare interventions. This is complex and some consider it to be unethical to place a monetary value on human life. These disadvantages hinder the use of CBA and CEA/CUA studies have become the dominant method.
Our findings also revealed a discrepancy in the geographical distribution of economic evaluation studies. The current results illustrate a high fragmentation of economic evaluation studies, which were mostly performed by authors in a few countries such as the USA (concentrated epidemic), England (concentrated epidemic), Canada (concentrated epidemic) and South Africa (Hyperendemic). Among top 20 countries as study settings having the highest number of economic evaluation publications, only five countries had severe HIV epidemic including South Africa (hyperendemic), Uganda (generalized), Kenya (generalized), Tanzania (generalized), and Zambia (generalized). Indeed, the application of economic evaluation studies for HIV responses highly depends on socioeconomic, epidemiological and health system characteristics in each nation. Jacobsen et al. argued that most of the economic evaluation models examining HIV/AIDS interventions were heterogeneous due to variations of methodologies and settings [68]. Insufficient local cost and effectiveness data were one of the major reasons that obstructed the utilization of economic evaluation research in policy-making process, leading to incorrect decisions in selecting priorities [72]. This lost benefit might even be greater in LMICs than that in high-income countries [69]. The Second Panel on Cost-effectiveness in Health and Medicine in 2016 suggested that interventions’ impacts on both health and non-health outcomes (such as work productivity, education, or environment) should be measured to reflect fully the societal perspectives of interventions in specific settings [73]. Therefore, increasing the presence of contextualized data and strategies are vital to promoting the quality and applicability of economic evaluation studies in HIV/AIDS research.
The partnership network analysis in our study shows clearly that countries in similar geographical regions tended to collaborate in performing economic evaluation research. This result implies that building strong regional and sub-regional partnership networks between leading countries and other countries in similar regions or with similar contexts may be beneficial. For example, countries such as South Africa, India, China, Brazil and the United Kingdom could play a center role in bringing together available resources from other countries in the same regions to conduct multi-country economic evaluation studies. Such a regional initiative could substantially increase the quality of evidence as well as the research capacity of each country members in the network. Previous bibliometric analyses had agreements in the critically important role of international and local collaboration networks in enhancing research capacity and evidence transfer [29, 74].
Our study contains several limitations. First, our searching process restricted in using only the WoS albeit its advantages compared to other databases. The limited databases might restrict our ability to cover all possible health economic and economic evaluation studies in HIV/AIDS field. The misuse of keyword such as CEA instead of CUA could result in the underestimation in the volume of publications for each economic evaluation form. Second, we only included peer-reviewed publications in the English language; therefore, potential grey documents reporting health economic studies and economic evaluation were not considered. Furthermore, we could only analyze abstracts and keywords instead of full-text of publications, which might not capture the main themes of selected publications. Fourth, our analysis was not able to examine the transferability of each research, which referred to the application of economic evaluation evidence in one country to another country. Further research should evaluate the transferability and applicability of economic evaluation in the decision-making process in each country.
Conclusion
In conclusion, this study highlighted the methodological and geographical discrepancies in health economic and economic evaluations in the field of HIV/AIDS. Developing regional collaboration networks and performing studies that incorporate affordability, feasibility and acceptability of the interventions would potentially improve the research capacity and study quality in economic evaluation research.
Acknowledgements
Not applicable
Abbreviations
- ART
Antiretroviral therapy
- CBA
Cost-benefit analysis
- CEA
Cost-effectiveness analysis
- CUA
Cost-utility analysis
- DALY
Disability-adjusted life years
- LDA
Latent Dirichlet Allocation
- LMICs
Low- and middle-income countries
- PLWH
People living with HIV
- QALY
Quality-adjusted life years
- STIs
Sexually Transmitted Infections
- UNAIDS
Joint United Nations Programme on HIV/AIDS
- USA
United States of America
- WoS
Web of Science
Authors’ contributions
BXT, LHN, HCT, SN, GTV, CTN, CAL, CSHH, RCMH conceived of the study, and participated in its design and implementation and wrote the manuscript. BXT, LHN analyzed the data. All authors read and approved the final manuscript.
Funding
This study did not receive any funding.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional file.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests. Bach Tran is a member of the editorial board of BMC Health Services Research. HCT is supported by the Wellcome Trust [089276/B/09/7].
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bach Xuan Tran, Phone: +84-982228662, Email: bach.jhu@gmail.com.
Long Hoang Nguyen, Email: longnh.ph@gmail.com.
Hugo C. Turner, Email: hturner@oucru.org
Son Nghiem, Email: s.nghiem@griffith.edu.au.
Giang Thu Vu, Email: giang.coentt@gmail.com.
Cuong Tat Nguyen, Email: cuong.ighi@gmail.com.
Carl A. Latkin, Email: carl.latkin@jhu.edu
Cyrus S. H. Ho, Email: cyrushosh@gmail.com
Roger C. M. Ho, Email: pcmrhcm@nus.edu.sg
References
- 1.Dieleman JL, Haakenstad A, Micah A, Moses M, Abbafati C, Acharya P, Adhikari TB, Adou AK, Ahmad Kiadaliri A, Alam K, et al. Spending on health and HIV/AIDS: domestic health spending and development assistance in 188 countries, 1995–2015. Lancet. 2018;391(10132):1799–1829. doi: 10.1016/S0140-6736(18)30698-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global HIV & AIDS statistics — 2019 fact sheet. https://www.unaids.org/en/resources/fact-sheet. Accessed 3 Sept 2019.
- 3.Snapshot - HIV investment. http://www.unaids.org/sites/default/files/media_asset/HIV_investments_Snapshot_en.pdf. Accessed 3 Sept 2019.
- 4.Schwartländer B, Stover J, Hallett T, Atun R, Avila C, Gouws E, Bartos M, Ghys PD, Opuni M, Barr D, et al. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet. 2011;377(9782):2031–2041. doi: 10.1016/S0140-6736(11)60702-2. [DOI] [PubMed] [Google Scholar]
- 5.Olakunde BO, Ndukwe CD. Improved domestic funding enhances the sustainability of HIV/AIDS response in Nigeria. Ann Glob Health. 2015;81(5):684–688. doi: 10.1016/j.aogh.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Resources and Financing. http://www.unaids.org/en/topic/resources. Accessed 3 Sept 2019.
- 7.Holtgrave DR, Qualls NL, Graham JD. Economic evaluation of HIV prevention programs. Annu Rev Public Health. 1996;17:467–488. doi: 10.1146/annurev.pu.17.050196.002343. [DOI] [PubMed] [Google Scholar]
- 8.Galarraga O, Colchero MA, Wamai RG, Bertozzi SM. HIV prevention cost-effectiveness: a systematic review. BMC Public Health. 2009;9(Suppl 1):S5. doi: 10.1186/1471-2458-9-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drummond MF, Aguiar-Ibanez R, Nixon J. Economic evaluation. Singap Med J. 2006;47(6):456–461. [PubMed] [Google Scholar]
- 10.Blumenschein K, Johannesson M. Economic evaluation in healthcare. A brief history and future directions. PharmacoEconomics. 1996;10(2):114–122. doi: 10.2165/00019053-199610020-00003. [DOI] [PubMed] [Google Scholar]
- 11.Drummond M, Jonsson B, Rutten F. The role of economic evaluation in the pricing and reimbursement of medicines. Health Policy. 1997;40(3):199–215. doi: 10.1016/S0168-8510(97)00901-9. [DOI] [PubMed] [Google Scholar]
- 12.Rudmik L, Drummond M. Health economic evaluation: important principles and methodology. Laryngoscope. 2013;123(6):1341–1347. doi: 10.1002/lary.23943. [DOI] [PubMed] [Google Scholar]
- 13.Tarride JE, Blackhouse G, Bischof M, McCarron EC, Lim M, Ferrusi IL, Xie F, Goeree R. Approaches for economic evaluations of health care technologies. J Am Coll Radiol. 2009;6(5):307–316. doi: 10.1016/j.jacr.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 14.Cambiano V, Miners A, Dunn D, McCormack S, Ong KJ, Gill ON, Nardone A, Desai M, Field N, Hart G, et al. Cost-effectiveness of pre-exposure prophylaxis for HIV prevention in men who have sex with men in the UK: a modelling study and health economic evaluation. Lancet Infect Dis. 2018;18(1):85–94. doi: 10.1016/S1473-3099(17)30540-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pinkerton SD, Holtgrave DR, Jemmott JB., 3rd Economic evaluation of HIV risk reduction intervention in African-American male adolescents. J Acquir Immune Defic Syndr. 2000;25(2):164–172. doi: 10.1097/00126334-200010010-00011. [DOI] [PubMed] [Google Scholar]
- 16.Huang YL, Lasry A, Hutchinson AB, Sansom SL. A systematic review on cost effectiveness of HIV prevention interventions in the United States. Appl Health Econ Health Policy. 2015;13(2):149–156. doi: 10.1007/s40258-014-0142-5. [DOI] [PubMed] [Google Scholar]
- 17.Dibosa-Osadolor O, Roberts T. Economic evaluation, human immunodeficiency virus infection and screening: a review and critical appraisal of economic studies. Int J Technol Assess Health Care. 2010;26(3):301–308. doi: 10.1017/S0266462310000292. [DOI] [PubMed] [Google Scholar]
- 18.Werayingyong P, Phanuphak N, Chokephaibulkit K, Tantivess S, Kullert N, Tosanguan K, Butchon R, Voramongkol N, Boonsuk S, Pilasant S, et al. Economic evaluation of 3-drug antiretroviral regimens for the prevention of mother-to-child HIV transmission in Thailand. Asia Pac J Public Health. 2015;27(2):Np866–Np876. doi: 10.1177/1010539513489134. [DOI] [PubMed] [Google Scholar]
- 19.Tse WF, Yang W, Huang W. A narrative review of cost-effectiveness analysis of people living with HIV treated with HAART: from interventions to outcomes. Clinicoecon Outcomes Res. 2015;7:431–439. doi: 10.2147/CEOR.S85535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Colombo GL, Di Matteo S, Antinori A, Medaglia M, Murachelli S, Rizzardini G. Economic evaluation of initial antiretroviral therapy for HIV-infected patients: an update of Italian guidelines. Clinicoecon Outcomes Res. 2013;5:489–496. doi: 10.2147/CEOR.S48246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Merito M, Bonaccorsi A, Pammolli F, Riccaboni M, Baio G, Arici C, Monforte AD, Pezzotti P, Corsini D, Tramarin A, et al. Economic evaluation of HIV treatments: the I.CO.N.A. cohort study. Health Policy. 2005;74(3):304–313. doi: 10.1016/j.healthpol.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 22.Patel AR, Kessler J, Braithwaite RS, Nucifora KA, Thirumurthy H, Zhou Q, Lester RT, Marra CA. Economic evaluation of mobile phone text message interventions to improve adherence to HIV therapy in Kenya. Medicine (Baltimore) 2017;96(7):e6078. doi: 10.1097/MD.0000000000006078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramos JM, Gutierrez F, Padilla S, Masia M, Martin-Hidalgo A. Geography of medical publications. An overview of HIV/AIDS research in 2003. AIDS. 2005;19(2):219–220. doi: 10.1097/00002030-200501280-00020. [DOI] [PubMed] [Google Scholar]
- 24.Ruger JP, Lazar CM. Economic evaluation of drug abuse treatment and HIV prevention programs in pregnant women: a systematic review. Addict Behav. 2012;37(1):1–10. doi: 10.1016/j.addbeh.2011.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nosyk B, Krebs E, Eyawo O, Min JE, Barrios R, Montaner JS. Cost-effectiveness analysis along the continuum of HIV care: how can we optimize the effect of HIV treatment as prevention programs? Curr HIV/AIDS Rep. 2014;11(4):468–478. doi: 10.1007/s11904-014-0227-7. [DOI] [PubMed] [Google Scholar]
- 26.Mauskopf J, Annemans L, Hill AM, Smets E. A review of economic evaluations of darunavir boosted by low-dose ritonavir in treatment-experienced persons living with HIV infection. PharmacoEconomics. 2010;28(Suppl 1):1–16. doi: 10.2165/11587410-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 27.Li R, Hernandez-Villafuerte K, Towse A, Vlad I, Chalkidou K. Mapping priority setting in health in 17 countries across Asia, Latin America, and sub-Saharan Africa. Health Syst Reform. 2016;2(1):71–83. doi: 10.1080/23288604.2015.1123338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jenniskens F, Tiendrebeogo G, Coolen A, Blok L, Kouanda S, Sataru F, Ralisimalala A, Mwapasa V, Kiyombo M, Plummer D. How countries cope with competing demands and expectations: perspectives of different stakeholders on priority setting and resource allocation for health in the era of HIV and AIDS. BMC Public Health. 2012;12:1071. doi: 10.1186/1471-2458-12-1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hernandez-Villafuerte K, Li R, Hofman KJ. Bibliometric trends of health economic evaluation in sub-Saharan Africa. Glob Health. 2016;12(1):50. doi: 10.1186/s12992-016-0188-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ellegaard O, Wallin JA. The bibliometric analysis of scholarly production: how great is the impact? Scientometrics. 2015;105(3):1809–1831. doi: 10.1007/s11192-015-1645-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Durieux V, Gevenois PA. Bibliometric indicators: quality measurements of scientific publication. Radiology. 2010;255(2):342–351. doi: 10.1148/radiol.09090626. [DOI] [PubMed] [Google Scholar]
- 32.Rosas SR, Kagan JM, Schouten JT, Slack PA, Trochim WM. Evaluating research and impact: a bibliometric analysis of research by the NIH/NIAID HIV/AIDS clinical trials networks. PLoS One. 2011;6(3):e17428. doi: 10.1371/journal.pone.0017428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Youle M, Trueman P, Simpson KJP. Health economics in HIV disease. Pharmacoeconomics. 1999;15(1):1–12. doi: 10.2165/00019053-199915001-00001. [DOI] [PubMed] [Google Scholar]
- 34.Beck EJ, Miners AH, Tolley KJP. The cost of HIV treatment and care. Pharmacoeconomics. 2001;19(1):13–39. doi: 10.2165/00019053-200119010-00002. [DOI] [PubMed] [Google Scholar]
- 35.Beck EJ, Harling G, Gerbase S, DeLay P. The cost of treatment and care for people living with HIV infection: implications of published studies, 1999–2008. Curr Opin HIV AIDS. 2010;5(3):215–224. doi: 10.1097/COH.0b013e32833860e9. [DOI] [PubMed] [Google Scholar]
- 36.Massey CN, Feig EH, Duque-Serrano L, Wexler D, Moskowitz JT, Huffman JC. Well-being interventions for individuals with diabetes: a systematic review. Diabetes Res Clin Pract. 2019;147:118–133. doi: 10.1016/j.diabres.2018.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Valle D, Albuquerque P, Zhao Q, Barberan A, Fletcher RJ., Jr Extending the latent Dirichlet allocation model to presence/absence data: a case study on north American breeding birds and biogeographical shifts expected from climate change. Glob Chang Biol. 2018;24(11):5560–5572. doi: 10.1111/gcb.14412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen C, Zare A, Trinh HN, Omotara GO, Cobb JT, Lagaunne TA. Partial membership latent Dirichlet allocation for soft image segmentation. IEEE Trans Image Process. 2017;26(12):5590–5602. doi: 10.1109/TIP.2017.2736419. [DOI] [PubMed] [Google Scholar]
- 39.Lu HM, Wei CP, Hsiao FY. Modeling healthcare data using multiple-channel latent Dirichlet allocation. J Biomed Inform. 2016;60:210–223. doi: 10.1016/j.jbi.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 40.Gross A, Murthy D. Modeling virtual organizations with latent Dirichlet allocation: a case for natural language processing. Neural Netw. 2014;58:38–49. doi: 10.1016/j.neunet.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 41.Paltiel AD, Weinstein MC, Kimmel AD, Seage GR, 3rd, Losina E, Zhang H, Freedberg KA, Walensky RP. Expanded screening for HIV in the United States--an analysis of cost-effectiveness. N Engl J Med. 2005;352(6):586–595. doi: 10.1056/NEJMsa042088. [DOI] [PubMed] [Google Scholar]
- 42.Freedberg KA, Losina E, Weinstein MC, Paltiel AD, Cohen CJ, Seage GR, Craven DE, Zhang H, Kimmel AD, Goldie SJ. The cost effectiveness of combination antiretroviral therapy for HIV disease. N Engl J Med. 2001;344(11):824–831. doi: 10.1056/NEJM200103153441108. [DOI] [PubMed] [Google Scholar]
- 43.Sweat M, Gregorich S, Sangiwa G, Furlonge C, Balmer D, Kamenga C, Grinstead O, Coates T. Cost-effectiveness of voluntary HIV-1 counselling and testing in reducing sexual transmission of HIV-1 in Kenya and Tanzania. Lancet. 2000;356(9224):113–121. doi: 10.1016/S0140-6736(00)02447-8. [DOI] [PubMed] [Google Scholar]
- 44.Marseille E, Kahn JG, Mmiro F, Guay L, Musoke P, Fowler MG, Jackson JB. Cost effectiveness of single-dose nevirapine regimen for mothers and babies to decrease vertical HIV-1 transmission in sub-Saharan Africa. Lancet. 1999;354(9181):803–809. doi: 10.1016/S0140-6736(99)80009-9. [DOI] [PubMed] [Google Scholar]
- 45.Jackson BR, Busch MP, Stramer SL, AuBuchon JP. The cost-effectiveness of NAT for HIV, HCV, and HBV in whole-blood donations. Transfusion. 2003;43(6):721–729. doi: 10.1046/j.1537-2995.2003.00392.x. [DOI] [PubMed] [Google Scholar]
- 46.Weinstein MC, Goldie SJ, Losina E, Cohen CJ, Baxter JD, Zhang H, Kimmel AD, Freedberg KA. Use of genotypic resistance testing to guide hiv therapy: clinical impact and cost-effectiveness. Ann Intern Med. 2001;134(6):440–450. doi: 10.7326/0003-4819-134-6-200103200-00008. [DOI] [PubMed] [Google Scholar]
- 47.Holtgrave DR, Pinkerton SD. Updates of cost of illness and quality of life estimates for use in economic evaluations of HIV prevention programs. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;16(1):54–62. doi: 10.1097/00042560-199709010-00009. [DOI] [PubMed] [Google Scholar]
- 48.Freedberg KA, Scharfstein JA, Seage GR, 3rd, Losina E, Weinstein MC, Craven DE, Paltiel AD. The cost-effectiveness of preventing AIDS-related opportunistic infections. Jama. 1998;279(2):130–136. doi: 10.1001/jama.279.2.130. [DOI] [PubMed] [Google Scholar]
- 49.Zaric GS, Barnett PG, Brandeau ML. HIV transmission and the cost-effectiveness of methadone maintenance. Am J Public Health. 2000;90(7):1100–1111. doi: 10.2105/AJPH.90.7.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meya DB, Manabe YC, Castelnuovo B, Cook BA, Elbireer AM, Kambugu A, Kamya MR, Bohjanen PR, Boulware DR. Cost-effectiveness of serum cryptococcal antigen screening to prevent deaths among HIV-infected persons with a CD4+ cell count < or = 100 cells/microL who start HIV therapy in resource-limited settings. Clin Infect Dis. 2010;51(4):448–455. doi: 10.1086/655143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sax PE, Islam R, Walensky RP, Losina E, Weinstein MC, Goldie SJ, Sadownik SN, Freedberg KA. Should resistance testing be performed for treatment-naive HIV-infected patients? A cost-effectiveness analysis. Clin Infect Dis. 2005;41(9):1316–1323. doi: 10.1086/496984. [DOI] [PubMed] [Google Scholar]
- 52.Gilson L, Mkanje R, Grosskurth H, Mosha F, Picard J, Gavyole A, Todd J, Mayaud P, Swai R, Fransen L, et al. Cost-effectiveness of improved treatment services for sexually transmitted diseases in preventing HIV-1 infection in Mwanza Region, Tanzania. Lancet. 1997;350(9094):1805–1809. doi: 10.1016/S0140-6736(97)08222-6. [DOI] [PubMed] [Google Scholar]
- 53.Goldie SJ, Kuntz KM, Weinstein MC, Freedberg KA, Palefsky JM. Cost-effectiveness of screening for anal squamous intraepithelial lesions and anal cancer in human immunodeficiency virus-negative homosexual and bisexual men. Am J Med. 2000;108(8):634–641. doi: 10.1016/S0002-9343(00)00349-1. [DOI] [PubMed] [Google Scholar]
- 54.Grinstead OA, Gregorich SE, Choi KH, Coates T. Positive and negative life events after counselling and testing: the voluntary HIV-1 counselling and testing efficacy study. AIDS. 2001;15(8):1045–1052. doi: 10.1097/00002030-200105250-00013. [DOI] [PubMed] [Google Scholar]
- 55.Desai K, Sansom SL, Ackers ML, Stewart SR, Hall HI, Hu DJ, Sanders R, Scotton CR, Soorapanth S, Boily MC, et al. Modeling the impact of HIV chemoprophylaxis strategies among men who have sex with men in the United States: HIV infections prevented and cost-effectiveness. AIDS. 2008;22(14):1829–1839. doi: 10.1097/QAD.0b013e32830e00f5. [DOI] [PubMed] [Google Scholar]
- 56.Schulman KA, Lynn LA, Glick HA, Eisenberg JM. Cost effectiveness of low-dose zidovudine therapy for asymptomatic patients with human immunodeficiency virus (HIV) infection. Ann Intern Med. 1991;114(9):798–802. doi: 10.7326/0003-4819-114-9-798. [DOI] [PubMed] [Google Scholar]
- 57.Barnett PG, Zaric GS, Brandeau ML. The cost-effectiveness of buprenorphine maintenance therapy for opiate addiction in the United States. Addiction. 2001;96(9):1267–1278. doi: 10.1046/j.1360-0443.2001.96912676.x. [DOI] [PubMed] [Google Scholar]
- 58.Schackman BR, Scott CA, Walensky RP, Losina E, Freedberg KA, Sax PE. The cost-effectiveness of HLA-B*5701 genetic screening to guide initial antiretroviral therapy for HIV. AIDS. 2008;22(15):2025–2033. doi: 10.1097/QAD.0b013e3283103ce6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Terris-Prestholt F, Watson-Jones D, Mugeye K, Kumaranayake L, Ndeki L, Weiss H, Changalucha J, Todd J, Lisekie F, Gumodoka B, et al. Is antenatal syphilis screening still cost effective in sub-Saharan Africa. Sex Transm Infect. 2003;79(5):375–381. doi: 10.1136/sti.79.5.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–222. doi: 10.1016/S1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- 61.Coffee M, Lurie MN, Garnett GP. Modelling the impact of migration on the HIV epidemic in South Africa. AIDS. 2007;21(3):343–350. doi: 10.1097/QAD.0b013e328011dac9. [DOI] [PubMed] [Google Scholar]
- 62.Iskarpatyoti BS, Lebov J, Hart L, Thomas J, Mandal M. Evaluations of structural interventions for HIV prevention: a review of approaches and methods. AIDS Behav. 2018;22(4):1253–1264. doi: 10.1007/s10461-017-1997-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kemp CG, Weiner BJ, Sherr KH, Kupfer LE, Cherutich PK, Wilson D, Geng EH, Wasserheit JN. Implementation science for integration of HIV and non-communicable disease services in sub-Saharan Africa: a systematic review. AIDS. 2018;32:S93–S105. doi: 10.1097/QAD.0000000000001897. [DOI] [PubMed] [Google Scholar]
- 64.Patel P, Rose CE, Collins PY, Nuche-Berenguer B, Sahasrabuddhe VV, Peprah E, Vorkoper S, Pastakia SD, Rausch D, Levitt NS. Noncommunicable diseases among HIV-infected persons in low-income and middle-income countries: a systematic review and meta-analysis. AIDS. 2018;32(Suppl 1):S5–s20. doi: 10.1097/QAD.0000000000001888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brent RJ, Brennan M, Karpiak SE. Economic evaluations of HIV prevention in rich countries and the need to focus on the aging of the HIV-positive population. Curr Opin HIV AIDS. 2010;5(3):255–260. doi: 10.1097/COH.0b013e3283384a88. [DOI] [PubMed] [Google Scholar]
- 66.Henny KD, Wilkes AL, McDonald CM, Denson DJ, Neumann MS. A rapid review of eHealth interventions addressing the continuum of HIV care (2007-2017) AIDS Behav. 2018;22(1):43–63. doi: 10.1007/s10461-017-1923-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kemp CG, Velloza J. Implementation of eHealth interventions across the HIV care cascade: a review of recent research. Curr HIV/AIDS Rep. 2018;15(6):403–413. doi: 10.1007/s11904-018-0415-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jacobsen MM, Walensky RP. Modeling and cost-effectiveness in HIV prevention. Curr HIV/AIDS Rep. 2016;13(1):64–75. doi: 10.1007/s11904-016-0303-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pitt C, Goodman C, Hanson K. Economic evaluation in global perspective: a bibliometric analysis of the recent literature. Health Econ. 2016;25(Suppl 1):9–28. doi: 10.1002/hec.3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wendy JU. Paediatric health economic evaluations: a world view. World Health Popul. 2006;8(4):89–101. doi: 10.12927/whp.2006.18475. [DOI] [Google Scholar]
- 71.Neumann PJ, Anderson JE, Panzer AD, Pope EF, D'Cruz BN, Kim DD, Cohen JT. Comparing the cost-per-QALYs gained and cost-per-DALYs averted literatures. Gates Open Res. 2018;2:5. doi: 10.12688/gatesopenres.12786.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Taleski SJ, Ahmed K, Whiteside A. The relationship between economic evaluations and HIV and AIDS treatment policies. Curr Opin HIV AIDS. 2010;5(3):204–209. doi: 10.1097/COH.0b013e3283384b58. [DOI] [PubMed] [Google Scholar]
- 73.Neumann PJ, Kim DD, Trikalinos TA, Sculpher MJ, Salomon JA, Prosser LA, Owens DK, Meltzer DO, Kuntz KM, Krahn M, et al. Future directions for cost-effectiveness analyses in health and medicine. Med Decis Mak. 2018;38(7):767–777. doi: 10.1177/0272989X18798833. [DOI] [PubMed] [Google Scholar]
- 74.McIntyre D, Wayling S. Strengthening health-economics capability in Africa: summary and outcomes of a regional consultation of experts and policy-makers. Geneva: World Health Organization/Special Programme for Research & Training in Tropical Diseases; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article and its additional file.