Abstract
Objective:
Families with limited English proficiency (LEP) experience communication barriers and are at risk for adverse events after discharge from the pediatric emergency department (ED). We sought to describe the characteristics of ED discharge communication for LEP families and to assess whether the use of a professional interpreter was associated with provider communication quality during ED discharge.
Methods:
Transcripts of video-recorded ED visits for Spanish-speaking LEP families were obtained from a larger study comparing professional interpretation modalities in a free-standing children’s hospital. Caregiver-provider communication interactions that included discharge education were analyzed for content and for the techniques that providers used to assess caregiver comprehension. Regression analysis was used to assess for an association between professional interpreter use and discharge education content or assessment of caregiver comprehension.
Results:
We analyzed 101 discharge communication interactions from 47 LEP patient visits; 31% of communications did not use professional interpretation. Although most patients (70%) received complete discharge education content, only 65% received instructions on medication dosing, and only 55% were given return precautions. Thirteen percent of the patient visits included an open-ended question to assess caregiver comprehension, and none included teach-back. Professional interpreter use was associated with greater odds of complete discharge education content (odds ratio [OR], 7.1; 95% confidence interval [CI], 1.4–37.0) and high-quality provider assessment of caregiver comprehension (OR, 6.1; 95% CI, 2.3–15.9).
Conclusions:
Professional interpreter use is associated with superior provider discharge communication behaviors. This study identifies clear areas for improving discharge communication, which may improve safety and outcomes for LEP children discharged from the ED.
Keywords: discharge instructions, interpreter use, limited English proficiency, pediatric emergency medicine, patient-centered communication
Individuals with limited English proficiency (LEP) make up a large, growing population in the United States and have high rates of emergency department (ED) utilization.1,2 There are well-documented disparities in health care delivery for this population. LEP individuals face higher costs of care and increased risk for adverse health outcomes, including serious medical errors and physical harm.3–6 Professional interpretation is associated with improved quality of care.4,7 However, although Title VI the Civil Rights Act of 1964 mandates that federally funded programs provide language access to LEP individuals, this requirement is unfunded, and only 10% to 30% of LEP patients receive professional interpretation,4,8–10 giving these patients fewer opportunities to engage in effective communication with providers.
Although clear communication is essential across health care settings, pediatric ED discharge is a critical time for patient education. Communication in the ED is unique, because providers rarely have a previous relationship with the patient and are balancing the care of multiple patients with varying acuity. Studies have repeatedly shown poor comprehension and recall of discharge instructions after an ED visit.11–13 Although best practices for ED discharge instructions include provision of thorough patient education and assessment of comprehension,14,15 few studies have directly examined provider discharge communication practices.
Given the increased risk for adverse outcomes and the high-risk setting of the ED, we sought to characterize provider communication with LEP families during ED discharge. Through analysis of transcripts of video-recorded ED visits, the objectives of this study were to 1) describe provider discharge communication behaviors with LEP families in a pediatric ED, including the content of education, provider strategies for assessing caregiver understanding, and professional interpreter use, and 2) assess the association between professional interpreter use and provider discharge communication behaviors.
Methods
Design, Setting, and Participants
This study analyzes transcripts of video-recorded pediatric ED visits obtained as part of a randomized clinical trial (RCT) comparing telephone and video interpretation.16 The RCT enrolled Spanish-speaking LEP caregivers who presented with their child to the ED of an academic children’s hospital. Randomization to a remote interpreter modality (telephone or video) occurred by day. Providers were encouraged to use the randomly assigned interpreter modality. However, ED visits involve multiple discrete communication interactions between the family and different providers (eg, nurse, resident, attending physician), each of which requires a provider decision regarding use of an interpreter. As such, providers had final discretion on how they communicated during each interaction throughout the ED visit. Enrollment in the video-recording substudy, described here, was offered to all families enrolled in the main study if sufficient time remained in the visit to allow for video setup (Fig. 1). Any provider interactions that occurred before enrollment were not video recorded. This study was approved by the Seattle Children’s Hospital Institutional Review Board.
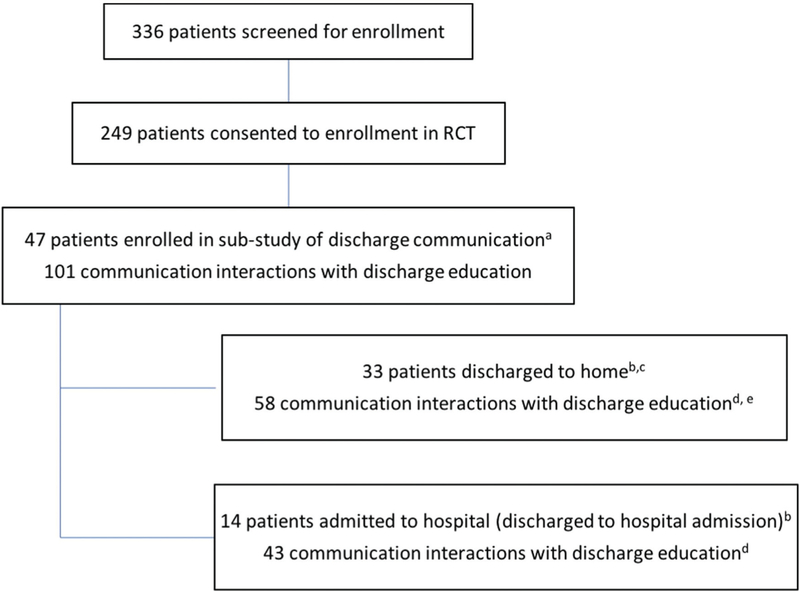
Figure 1.
Study enrollment and levels of analysis. aIncludes patients from main RCT who consented to have the ED visit video-recorded. Does not include 6 patients for whom partial video-recording was completed but no discharge communication was captured. bIncluded in analysis by patient visit of provider assessment of caregiver comprehension. cIncluded in analysis by patient visit of discharge education content. dIncluded in analysis by communication interaction of professional interpreter use and provider assessment of caregiver comprehension. eIncluded in analysis by communication interaction of discharge education content.
Data Collection
Patient characteristics (age, sex, and medical complexity) were obtained from electronic medical records. The Patient Medical Complexity Algorithm,17 which classifies children as having no chronic illness, noncomplex chronic illness, or complex chronic illness, was used to determine medical complexity. Patient Emergency Severity Index (ESI) triage acuity level, which ranges from 1 (life-threatening emergency) to 5 (anticipated need for limited intervention), was captured at enrollment; patients with an ESI of 1 were not eligible. The National Emergency Department Overcrowding Score, in which higher scores (range, 0–200) indicate greater acuity and volume relative to ED resources, was also captured at enrollment. The patient’s ED length of stay was obtained through hospital utilization data. Patient discharge disposition from the ED was either discharge to either home or the hospital (ie, a hospital admission).
Caregiver characteristics (ie, years in the United States, level of English proficiency, highest education level, and family income) were obtained from a follow-up phone survey at 1 to 7 days after discharge. English proficiency was defined using US Census Bureau categories of speaking English not at all, not well, well, or very well.
All video recordings were reviewed (by J.G., J.S., and K. C.L.) and transcribed (by J.G.), and each transcript was subdivided into distinct caregiver-provider communication interactions. Distinct communication interactions were defined by a change in the provider communicating with the caregiver. For example, a distinct caregiver-provider communication interaction might involve a resident discussing test results with the caregiver. If an attending physician entered during this ongoing communication, a new interaction began when the attending joined the conversation.
In initial coding, the video recordings were reviewed to identify characteristics of each communication interaction, including provider type, primary language of communication, and primary mode of interpretation. Providers were identified as attending physicians, nurse practitioners or residents, consulting providers, and nurses. The primary language of communication was either English or Spanish. Interpretation modalities included no interpretation, use of family members or friends to interpret (ad hoc interpretation), or professional interpretation in-person or by telephone or video. Bilingual providers were identified as those who had passed an institutionally required certification exam.
Transcript Coding
Two authors (C.K.G. and L.C.) reviewed the transcripts using a predetermined coding scheme to identify elements of discharge communication (Fig. 2). A subset of transcripts was reviewed by both coders; disagreements were resolved by discussion among 3 authors (C.K.G., L.C., and K.C.L.). Following a training period, the weighted κ statistic for interrater reliability in all areas was >0.7, indicating good agreement. All communication interactions were coded for discharge content. Communication interactions that did not include discharge education were dropped from the analysis.
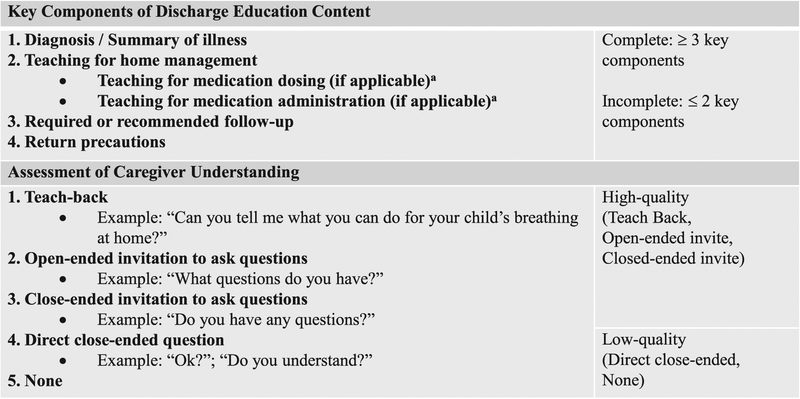
Figure 2.
Provider discharge communication behaviors. aApplicable if home management teaching was given and included specific instructions regarding medication use.
Communication Interaction Coding: Discharge Education Content
Each communication interaction was evaluated for 4 key components of discharge education (Fig. 2), which were identified as essential to safely care for the child after discharge. Because discharge education was defined by the content of the communication, it could occur at any point and was not limited by the timing of the communication within the patient visit. These 4 components of discharge education were developed for this study and reflect the Agency for Healthcare Research and Quality’s best practices for high-quality ED discharge.18 These were 1) a summary of the child’s illness, including the diagnosis if available, or a review of the pertinent presenting signs and symptoms; 2) instructions for home management of the illness; 3) required or recommended follow-up appointments; and 4) return precautions, including signs of worsening illness or when to seek reevaluation. If the home management education included medication use, we further identified 2 aspects of medication education: 1) if the caregiver received education on medication dosing, such as the amount of medication to give or the frequency with which to give it, and 2) if the caregiver received education on medication administration, including instructions or demonstrations of how to measure the appropriate volume or how to deliver the medication to the child. Discharge education was considered complete if 3 or 4 of the key components were provided. Although all 4 components are necessary for complete discharge education for many patients, we chose a cutoff of 3, because a follow-up visit was not universally applicable. Complete discharge education was not necessarily applicable to patients admitted to the hospital, so these patients were excluded from discharge education content analysis.
Communication Interaction Coding: Assessment of Caregiver Comprehension
In each communication interaction, the strategies providers used to assess caregiver comprehension were identified (Fig. 2 presents examples). Teach-back, a technique in which providers ask patients to explain their understanding of what was discussed, is the gold standard for assessing comprehension and was considered the highest-quality assessment method.19 Following this was any invitation for the caregiver to ask questions, with open-ended invitations considered of higher quality than closed-ended invitations, because open-ended questions are more likely to elicit caregiver concerns.20 Provider use of a direct closed-ended question to confirm receipt of information was considered a low-quality assessment method. We also captured whether no assessment occurred. A communication interaction was considered to include high-quality assessment of caregiver understanding if the provider used teach-back or gave any invitation (open- or closed ended) for the caregiver to ask questions. This cutoff for classifying an assessment as high quality was chosen because so few communication interactions involved open-ended questions or teach-back.
Patient-Level Summary
Each patient visit included multiple individual communication interactions. The discharge process often took place over many discrete interactions with multiple providers, and even if all aspects of discharge education were not present in a single communication interaction, a patient might have received complete discharge education over the course of the entire patient visit. As such, discharge education content was summarized for the entire visit. Each key component of discharge education was considered present in the patient visit if it was included in at least one communication interaction for that patient. The strategies used by providers to assess caregiver understanding were also summarized by patient. For each patient visit, the highest-quality strategy used in any communication interaction was identified and coded for if it was used at least once during the patient’s ED visit.
Data Analysis
For each communication interaction, descriptive statistics were used to summarize provider and professional interpretation characteristics and provider discharge communication behaviors. For each patient visit, descriptive statistics were used to summarize patient demographics, caregiver survey responses, and ED characteristics, as well as summary discharge education content and strategies to assess caregiver understanding.
Within communication interactions, regression analysis was used to assess for an association between professional interpreter use and discharge education content or provider strategies to assess caregiver understanding. Given the limited sample size, we aimed to be judicious in including only potential confounders in our model. Thus, we tested for associations between covariables identified a priori (ie, insurance type, caregiver maximum education, caregiver English proficiency, family income, medical complexity, and ESI) and professional interpreter use. ESI (dichotomized into higher acuity [levels 2 and 3] and lower acuity [levels 4 and 5] categories) was the sole covariable with a statistically significant association with professional interpreter use, and thus was included in the adjusted model.
Results
In the RCT, 336 Spanish-speaking families were screened for eligibility and 249 were enrolled (Fig. 1). Fifty-three families consented to video recording; 6 of those families had no discharge education captured on video (ie, recording started too late in the visit to capture discharge education, or discharge education was not provided in the available recording) and so were not eligible for this study, leaving 47 visits that were included. The transcripts from the 47 included visits were composed of 451 caregiver-provider communication interactions, 101 (22%) of which contained discharge education. Thirty-three of 47 patients (70%) with video-recorded visits were discharged to home, and those visits included 58 communication interactions that involved discharge education.
Patient Characteristics
Table 1 presents the demographic characteristics of patients with discharge-containing video-recorded ED visits and includes information collected from those care-givers who completed the follow-up phone survey. Care-givers reported a low level of English proficiency, with 84% reporting speaking English “not well” or “not at all.” Nearly one half (48%) of caregivers enrolled in the sub-study reported their highest educational attainment as grade 8 or less.
Table 1.
Patient, Caregiver, and ED Characteristics
| Patient Characteristics | Admitted (n = 14)* | Discharged (n = 33) | Total (n = 47) |
|---|---|---|---|
| Age, y, mean (SD) | 4.5 (4.3) | 5.9 (4.7) | 5.4 (4.6) |
| Male sex, % | 79 | 61 | 66 |
| Medical complexity, %† | |||
| No chronic conditions | 43‡ | 82 | 70 |
| Noncomplex chronic | 29‡ | 15 | 19 |
| Complex chronic | 29‡ | 3 | 11 |
| Triage acuity level, %§ | |||
| High | |||
| Level 2 | 14 | 3 | 6 |
| Level 3 | 86 | 33 | 49 |
| Low | |||
| Level 4 | 0 | 61 | 43 |
| Level 5 | 0 | 3 | 2 |
| ED characteristics | |||
| Crowding score‖, mean (SD) | 56 (15) | 59 (23) | 58 (21) |
| Length of stay, min, mean (SD) | 347 (120) | 172 (103) | 224 (134) |
| Caregiver characteristics¶ | n = 13 | n = 29 | n = 42 |
| Years in United States, mean (SD) | 10.9 (6.4) | 11.1 (4.2) | 11.1 (4.9) |
| English proficiency, % | |||
| Not at all | 38 | 28 | 31 |
| Not well | 46 | 55 | 53 |
| Well | 8 | 17 | 14 |
| Did not respond | 8 | 0 | 2 |
| Highest education, % | |||
| ≥8th grade | 31 | 55 | 48 |
| Some high school | 23 | 17 | 19 |
| High school graduate or GED | 38 | 17 | 24 |
| Some college or more | 8 | 11 | 9 |
| Did not respond | 0 | 0 | 0 |
| Annual family income, % | |||
| <$15,000 | 15 | 21 | 19 |
| $15,000–30,000 | 54 | 62 | 60 |
| $30,000–50,000 | 8 | 7 | 7 |
| >$50,000 | 8 | 3 | 5 |
| Did not respond | 15 | 7 | 9 |
SD indicates standard deviation; ED, emergency department; and GED, general equivalency diploma.
Includes 1 patient admitted to magnetic resonance imaging and subsequently discharged from there; included in the admitted category because final discharge education occurred outside of the ED and was not captured in video recording.
Patient Medical Complexity Algorithm.18
Sum >100% owing to rounding errors.
Emergency Severity Index, range 1–5; level 1 patients (highest acuity) were not eligible for inclusion in the randomized controlled trial.
National Emergency Department Overcrowding Score (range 0 to 200); level 2 (range 20–60) indicates a busy ED, level 3 (60–100) indicates an extremely busy ED.
Obtained from follow-up telephone survey.
Analysis of Communication Interactions
In almost one half (47%) of discharge communication interactions, the provider speaking with the caregiver and patient was a resident or nurse practitioner. Attending ED physicians and consultants each provided discharge education in 21% of communication interactions, and nurses provided discharge education in 11%. A professional interpreter was used in 66% of discharge communication interactions, and a bilingual provider in 3%. Thirty-one percent of the communication interactions that included discharge education occurred without professional interpretation (Table 2).
Table 2.
Professional Interpretation and Provider Discharge Communication Behaviors
| Parameter | Value |
|---|---|
| Communication interaction analysis | |
| Interpretation modality in individual communication interactions (n = 101), %* | |
| Professional interpretation | 66 |
| In-person | 2 |
| Phone | 39 |
| Video | 26 |
| No professional interpretation | 31 |
| Spoke in English | 20 |
| Spoke in Spanish | 7 |
| Use of ad hoc interpreter† | 4 |
| Bilingual provider‡ | 3 |
| Patient visit analysis | |
| Content of discharge education covered in each patient visit (n = 33§), % | |
| Summary of illness/diagnosis | 100 |
| Teaching for home management | 85 |
| Instructions on medication use‖ | 82 |
| Teaching on medication dosing¶ | 65 |
| Teaching on medication administration¶ | 0 |
| Required or recommended follow-up | 48 |
| Return precautions | 55 |
| Highest-quality strategy to assess comprehension in each patient visit (n = 47#), % | |
| Teach-back | 0 |
| Open-ended invitation to ask questions | 13 |
| Close-ended invitation to ask questions | 64 |
| Direct closed question | 15 |
| None | 9 |
Includes all communication interactions containing discharge education.
Use of a family member, friend, or other untrained individual for interpretation.
Providers who had passed a certification exam and were permitted to provide care bilingually.
Includes only patient visits in which the patient was discharged to home from the emergency department.
Applicable if provider gave teaching for home management (n = 28).
Applicable if provider gave instructions on medication use (n = 23).
Includes all patient visits.
Analysis of Patient Visits
All caregivers of children who were discharged to home from the ED were given a summary of their child’s illness, and 70% received complete discharge education. Of the caregivers given instructions regarding medication use, 65% were given instructions on medication dosing, but none were taught how to administer the medication (Table 2). More than one half of discharged patients (55%) were given information on return precautions.
Three quarters (77%) of patient visits included an invitation to ask questions as a way to assess caregiver understanding (Table 2). Providers used an open-ended invitation for caregivers to ask questions in 13% of visits and a closed-ended invitation to ask questions in 64% of visits. In 15% of patient visits, the provider used a direct closed-ended question to confirm caregiver receipt of information but did not invite the caregiver to ask questions or demonstrate comprehension. There was no provider assessment of caregiver understanding in 9% of patient visits. Teach-back was not used in any discharge communications.
Regression Analysis
Results of the adjusted regression analysis are shown in Table 3. Within a communication interaction, the use of professional interpretation compared with none was associated with 7.1-fold increased odds of containing complete discharge education content (95% confidence interval, 1.4–37). Similarly, the use of professional interpretation compared with none was associated with a 6.1-fold increased odds of a high-quality assessment of care-giver understanding (95% confidence interval, 2.3–15.9).
Table 3.
Professional Interpreter Use and Provider Discharge Communication Behaviors
| Communication Interaction Analysis | ||
|---|---|---|
| Provider Discharge Communication Behavior (Outcome) | Professional Interpreter Use (Predictor) | Adjusted Odds Ratio* (95% Confidence Interval) |
| Complete discharge education† | ||
| None | Reference | |
| Professional interpreter | 7.1 (1.4–37.0) | |
| Bilingual provider | 2.7 (0.2–46.5) | |
| High-quality assessment‡ | ||
| None | Reference | |
| Professional interpreter | 6.1 (2.3–15.9) | |
| Bilingual provider | § | |
Adjusted for Emergency Severity Index triage acuity (high vs low) on presentation to the emergency department.
Discharge education considered complete if ≥3 key components of discharge education content were present in the communication interaction; n = 58 communication interactions containing discharge education for patients discharged to home.
Assessment of caregiver understanding was considered high quality if the communication interaction included teach-back or an invitation for the caregiver to ask questions; n = 101 communication interactions containing discharge education for all patients.
Dropped from model owing to small sample size (n = 3).
Discussion
In this study of video-recorded ED visits for LEP families, we found suboptimal approaches by providers regarding essential discharge education. Discharge instructions often missed essential information, such as return precautions, follow-up instructions, and medication dosing and administration education. Assessment of care-giver comprehension was often of low quality. These findings were associated with interpreter use; providers who used professional interpretation were more likely to give complete discharge education and to invite the patient and caregiver to ask questions. The quality of provider discharge communication with LEP families was higher when done with professional interpretation.
Our analysis was embedded in an RCT that evaluated types of professional interpretation in which providers were aware of the study and of video recording; despite this, professional interpreters were not used in one third of discharge education communication interactions. Professional interpreter use is known to be underused by health care providers.8 Our results confirm this underuse and emphasize the importance of professional interpretation when communicating with LEP families, given the potential for professional interpreter use to improve communication quality and, subsequently, patient outcomes.
Providers in this study had final discretion regarding if and when to use interpretation. This mirrors real-world conditions, in which complex decision making influences the provider’s decision to “get by” without an interpreter for each interaction with an LEP family, because each interaction requires time to access either an in-person or remote interpreter.21,22 By analyzing each individual interaction, we found a clear association between professional interpreter use and provider communication behaviors that are associated with better engagement and outcomes. This makes sense for several reasons. First, without interpretation, 2-way communication is limited, which may discourage providers from asking open-ended questions for which they do not expect to understand the answers. Second, providers may provide less information when they are aware of a language barrier but are not using interpretation, in an effort to keep vocabulary and concepts simple. Finally, there is excellent research suggesting that much of the variability in how providers communicate, including how much information they provide and how supportive they are, is owing to how patients and families communicate, including how many questions they ask and what concerns they express.23–26 Thus, it is unsurprising that in the absence of interpretation, members of an LEP family may be unable to express themselves in a way that prompts high-quality communication from a provider.
We looked at the patient visits in their entirety, and our findings are similar to other studies involving observation of provider discharge communication in adult ED settings.27,28 In this limited existing literature, analysis of audio recordings has shown that discharge education is often incomplete, and that providers rarely create opportunities to assess patient comprehension. Although this study did not include a comparison of communication with English-speaking families in the same setting, our results highlight areas for improvement that are of particular importance for LEP families, who are at higher risk for low health literacy and adverse patient outcomes.
Although most patients received complete or nearly complete discharge education, the most frequently missing topics were in areas in which LEP families are known to be at high risk: medication dosing education, return precautions, and follow-up. One third of caregivers who were instructed to use medications were not taught dosing information, and none were taught how to administer medications. Caregivers of LEP children are at high risk for making medication dosing errors,29,30 and dosing errors decrease when caregivers receive education on medication administration.31 Although physicians often rely on multidisciplinary involvement from pharmacists for medication education, professional interpreter use at pharmacies is low,32,33 and pharmacy-based education might not be a realistic expectation for LEP families. This leaves LEP families at high risk for safety issues related to medication administration errors.
In this study, 45% of the patients discharged to home were not given return precautions, and 52% were not given instructions regarding follow-up. Many parents of children with return ED visits report having previously received incomplete discharge instructions.34 LEP patients are more likely to have a return visit35 and to subsequently require hospital admission.36 Although the reasons for this are multifactorial, providing LEP patients with clear instructions on when to return to the ED and recommendations for primary care follow-up may prompt more timely and appropriate utilization patterns.
The strategies that providers used to assess caregiver understanding were suboptimal. Most visits included an opportunity for the caregiver to ask questions, although this was most often done with a closed-ended invitation to do so. Furthermore, there was little or no assessment of caregiver understanding in nearly one quarter of visits. This is an area in which patient-centered communication with LEP families clearly can be improved, with an emphasis on increasing caregiver engagement to ensure transfer of essential information. The opportunity for bidirectional communication through a professional interpreter may explain the finding that higher-quality, open-ended strategies to assess caregiver understanding were used more often when a professional interpreter was present. Notably, teach-back, in which patients are asked to demonstrate their understanding and providers can clarify and correct, was not used at all. Opening the door to patient questions may be viewed as time-consuming; moreover, providers often perceive professional interpretation as adding time delays, although this is not supported in the literature.8 Although patient-centered care is a priority in institutional and national quality improvement efforts, neither time spent in communication nor professional interpreter use is directly reimbursed, which may serve as a barrier to providers working with LEP families. However, teach-back has been found to be well received by ED patients when done without judgment,37 has been demonstrated to improve comprehension in patients with low health literacy after ED discharge,38 and has been associated with improved patient outcomes.19 Given the high proportion of LEP patients with low health literacy,39 the use of teach-back to assess and promote caregiver comprehension may be a particularly important strategy for providers working with LEP families.
This study is subject to limitations. The data were collected at a single academic children’s hospital with ready availability of in-person and remote interpreters and might not be reflective of interpreter access elsewhere. The hospital is a referral center with high patient acuity and medical complexity, which may impact communication patterns and practices. The analysis is limited by the small sample size; only a small proportion of families from the original RCT consented to video recording, which may have resulted in selection bias. The small sample limited the number of covariables that could be included in the multivariate model, although there are a number of additional potential confounders known to affect provider communication with LEP families. There is the potential for having missed relevant communication, because video recording only began after patient consent, which sometimes occurred after the initial provider evaluation. However, because any missing communications occurred at the beginning of the visit, it is unlikely that this contained significant discharge education. Providers in this study were aware that they were being video recorded for an interpretation-related study, so our findings may overestimate the frequency of desirable communication behaviors and interpreter use. This also may account for the low use of ad hoc interpreters, a practice that is actively discouraged at our institution. This study included Spanish-speaking LEP patients and might not be applicable to LEP patients who speak languages other than Spanish. Similarly, we could not assess the quality of discharge communication used with English-proficient patients. This study was limited to verbal discharge education and did not evaluate any concurrent written discharge instructions. Written discharge instructions are an essential adjunct to the discharge process; however, they may be less effective for LEP families.15 Finally, the association between interpreter use and higher-quality discharge communication behaviors may reflect that providers who intend to provide more comprehensive education and assessment choose to use an interpreter to do so, rather than interpreter use itself promoting better communication behaviors.
Conclusions
The use of professional interpretation during discharge communication with LEP families is associated with higher-quality provider communication. Our study highlights areas in which ED discharge communication with LEP families can be improved, specifically in the use of professional interpretation for discharge education, teaching regarding medication use and return precautions, and provider assessment of patient and caregiver comprehension. These findings have spurred ongoing quality improvement interventions and planned research evaluations at our institution aimed at increasing professional interpreter use and improving the discharge education process for all ED patients. Addressing these areas has the potential to improve safety and outcomes for LEP children discharged from the ED.
What’s New.
Discharge communication is inadequate for most limited English proficiency (LEP) patients in a pediatric emergency department (ED). Professional interpretation is associated with superior discharge education and assessment of caregiver comprehension. Improving ED discharge communication may improve outcomes for LEP patients.
Acknowledgments
We thank the Seattle Children’s Hospital Department of Interpreter Services and the Seattle Children’s Hospital ED Research Team for their contributions to this project, and thank the ED staff and patients for their participation.
Financial disclosure: This work was funded by the Seattle Children’s Research Institute Center for Child Health, Behavior and Development and the Seattle Children’s Hospital Center for Diversity and Health Equity. K.C.L. was supported by National Institute of Child Health and Human Development Grant K23 HD078507 (PI, K. C. Lion). Data collection through REDCap at the University of Washington’s Institute of Translational Health Sciences was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1 TR002319.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Ryan C. Language Use in the United States: 2011. Washington, DC: US Census Bureau; 2013. [Google Scholar]
- 2.Njeru JW, St Sauver JL, Jacobson DJ, et al. Emergency department and inpatient health care utilization among patients who require interpreter services. BMC Health Serv Res. 2015;15:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fiscella K, Franks P, Doescher MP, et al. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care. 2002;40:52–59. [DOI] [PubMed] [Google Scholar]
- 4.Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62:255–299. [DOI] [PubMed] [Google Scholar]
- 5.Lion KC, Rafton SA, Shafii J, et al. Association between language, serious adverse events, and length of stay among hospitalized children. Hosp Pediatr. 2013;3:219–225. [DOI] [PubMed] [Google Scholar]
- 6.Cohen AL, Rivara F, Marcuse EK, et al. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. 2005;116:575–579. [DOI] [PubMed] [Google Scholar]
- 7.Karliner LS, Jacobs EA, Chen AH, et al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42:727–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. J Health Care Poor Underserved. 2008;19:352–362. [DOI] [PubMed] [Google Scholar]
- 9.Kuo DZ, O’Connor KG, Flores G, et al. Pediatricians’ use of language services for families with limited English proficiency. Pediatrics. 2007;119:e920–e927. [DOI] [PubMed] [Google Scholar]
- 10.Lee KC, Winickoff JP, Kim MK, et al. Resident physicians’ use of professional and nonprofessional interpreters: a national survey. JAMA. 2006;296:1050–1053. [DOI] [PubMed] [Google Scholar]
- 11.Engel KG, Heisler M, Smith DM, et al. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;53: 454–461. e415. [DOI] [PubMed] [Google Scholar]
- 12.Musso MW, Perret JN, Sanders T, et al. Patients’ comprehension of their emergency department encounter: a pilot study using physician observers. Ann Emerg Med. 2015;65:151–155.e154. [DOI] [PubMed] [Google Scholar]
- 13.Glick AF, Farkas JS, Nicholson J, et al. Parental management of discharge instructions: a systematic review. Pediatrics. 2017;140:e20164165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Limpahan LP, Baier RR, Gravenstein S, et al. Closing the loop: best practices for cross-setting communication at ED discharge. Am J Emerg Med. 2013;31:1297–1301. [DOI] [PubMed] [Google Scholar]
- 15.Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the emergency department. Ann Emerg Med. 2012;60:152–159. [DOI] [PubMed] [Google Scholar]
- 16.Lion KC, Brown JC, Ebel BE, et al. Effect of telephone vs video interpretation on parent comprehension, communication, and utilization in the pediatric emergency department: a randomized clinical trial. JAMA Pediatr. 2015;169:1117–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simon TD, Cawthon ML, Stanford S, et al. Pediatric medical complexity algorithm: a new method to stratify children by medical complexity. Pediatrics. 2014;133:e1647–e1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boonyasai RT, Ijagbemi OM, Pham JC, et al. Improving the Emergency Department Discharge Process. AHRQ Publication No. 14 (15)-0067-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [Google Scholar]
- 19.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. [DOI] [PubMed] [Google Scholar]
- 20.Branch WT, Malik TK. Using windows of opportunities in brief interviews to understand patients concerns. JAMA. 1993;269: 1667–1668. [PubMed] [Google Scholar]
- 21.Diamond LC, Schenker Y, Curry L, et al. Getting by: underuse of interpreters by resident physicians. J Gen Intern Med. 2009;24: 256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lion KC, Thompson DA, Cowden JD, et al. Clinical Spanish use and language proficiency testing among pediatric residents. Acad Med. 2013;88:1478–1484. [DOI] [PubMed] [Google Scholar]
- 23.Street RL. Communicative styles and adaptations in physician-parent consultations. Soc Sci Med. 1992;34:1155–1163. [DOI] [PubMed] [Google Scholar]
- 24.Cegala DJ, Street RL Jr, Clinch CR. The impact of patient participation on physicians’ information provision during a primary care medical interview. Health Commun. 2007;21:177–185. [DOI] [PubMed] [Google Scholar]
- 25.Tran AN, Haidet P, Street RL Jr, et al. Empowering communication: a community-based intervention for patients. Patient Educ Couns. 2004;52:113–121. [DOI] [PubMed] [Google Scholar]
- 26.Ashton CM, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med 2003;18:146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rhodes KV, Vieth T, He T, et al. Resuscitating the physician-patient relationship: emergency department communication in an academic medical center. Ann Emerg Med. 2004;44: 262–267. [DOI] [PubMed] [Google Scholar]
- 28.Vashi A, Rhodes KV. “Sign right here and you’re good to go”: a content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2011;57:315–322.e311. [DOI] [PubMed] [Google Scholar]
- 29.Samuels-Kalow ME, Stack AM, Porter SC. Parental language and dosing errors after discharge from the pediatric emergency department. Pediatr Emerg Care. 2013;29:982–987. [DOI] [PubMed] [Google Scholar]
- 30.Harris LM, Dreyer BP, Mendelsohn AL, et al. Liquid medication dosing errors by Hispanic parents: role of health literacy and English proficiency. Acad Pediatr. 2017;17:403–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McMahon SR, Rimsza ME, Bay RC. Parents can dose liquid medication accurately. Pediatrics. 1997;100(3 Pt 1):330–333. [DOI] [PubMed] [Google Scholar]
- 32.Bradshaw M, Tomany-Korman S, Flores G. Language barriers to prescriptions for patients with limited English proficiency: a survey of pharmacies. Pediatrics. 2007;120:e225–e235. [DOI] [PubMed] [Google Scholar]
- 33.Feichtl MM, Clauson KA, Alkhateeb FM, et al. Community pharmacists’ use of language-access services in the United States. J Am Pharm Assoc. 2011;51:368–372. [DOI] [PubMed] [Google Scholar]
- 34.Navanandan N, Schmidt SK, Cabrera N, et al. The caregiver perspective on unscheduled 72-hour return visits to pediatric acute care sites: a focus on discharge processes. Acad Pediatr. 2017;17:755–s761. [DOI] [PubMed] [Google Scholar]
- 35.Samuels-Kalow ME, Stack AM, Amico K, et al. Parental language and return visits to the emergency department after discharge. Pediatr Emerg Care. 2017;33:402–404. [DOI] [PubMed] [Google Scholar]
- 36.Gallagher RA, Porter S, Monuteaux MC, et al. Unscheduled return visits to the emergency department: the impact of language. Pediatr Emerg Care. 2013;29:579–583. [DOI] [PubMed] [Google Scholar]
- 37.Samuels-Kalow M, Hardy E, Rhodes K, et al. “Like a dialogue”: teach-back in the emergency department. Patient Educ Couns. 2016;99:549–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Griffey RT, Shin N, Jones S, et al. The impact of teach-back on comprehension of discharge instructions and satisfaction among emergency patients with limited health literacy: a randomized, controlled study. J Commun Healthc. 2015;8:10–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sentell T, Braun KL. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J Health Commun. 2012;17 (Suppl 3):82–99. [DOI] [PMC free article] [PubMed] [Google Scholar]