Abstract
BACKGROUND AND OBJECTIVE:
Patients with limited English proficiency (LEP) experience worse health care outcomes compared to English proficient (EP) patients, and professional interpretation is underutilized in clinical settings. The objectives of this study were to describe patterns of interpreter use in a pediatric emergency department (ED), to determine factors associated with its use, and to examine differences in outcomes between EP families and those with LEP.
METHODS:
ED encounters for LEP and EP patients were reviewed in a retrospective cohort study design over a 15 month period. Generalized estimating equations were used to compare patient encounters and factors associated with interpreter use.
RESULTS:
Interpreter use for families who preferred a non-English language was 45.4%. Use of interpretation was less likely during busier times of day (odds ratio [OR] 0.85, confidence interval [CI] 0.78–0.93), with a lower triage acuity (OR 0.66, CI 0.62–0.70), and with each increasing year of patient age (OR 0.97, CI 0.96–0.98). LEP patients who did not receive interpretation were less likely to be admitted than EP patients (OR 0.69, 0.62–0.78). Patients of LEP families, with or without interpretation, were more likely to be transferred to the ICU within 24 hours of admission than patients of EP families (OR 1.76, 1.07–2.90; 1.85, 1.08–3.18) suggesting that an aspect of clinical severity may have been missed in the ED.
CONCLUSIONS:
Professional interpretation is currently underutilized in this ED for patients with LEP, and important differences in outcomes exist between LEP and EP patients. Factors associated with interpreter use will inform ongoing improvement efforts.
Keywords: health equity, interpreter use, quality of care, emergency department, pediatrics
AN ESTIMATED 26 MILLION individuals in the United States have limited English proficiency (LEP) as defined by speaking English less than “very well” when asked during a census. This represents 8.6% of the US population; the most common spoken language is Spanish.1
Disparities in medical care provided for families with LEP have been well described in the literature. LEP is an independent risk factor for poor health outcomes among children with chronic health care needs; children with LEP are more likely to be uninsured, have no usual source of care or medical home, and are less likely to be satisfied with their care.2 Higher overall health care utilization and use of urgent care services have been reported for these families, perhaps as a result of difficulty in accessing primary care.3
In the Emergency Department (ED) setting, differences have been observed in tests ordered by providers, disposition, triage levels, and treatment interventions for patients with LEP.4,5 Families with LEP are at higher risk for having a return visit to the ED within 72 hours,6 and they are more likely to experience complications such as a perforated appendix.7 Spanish-speaking families with LEP report difficulty with access to care, health information, and education.8 Families with LEP have also reported lower trust of their physicians.9
Spanish-speaking patients with LEP are more likely to be involved in serious adverse events when hospitalized.10 Compared to those who are English proficient, documentation of informed consent,11 and postoperative pain assessments and treatment are less likely to occur for patients with LEP.12
Interpretation for patients with LEP can reduce or eliminate disparities in care.13,14 Professional interpretation can occur with in-person interpreters, dual handset phones, or video units. When compared to each other, differences in length of stay (LOS), comprehension of discharge diagnosis and reported lapses in communication have been shown depending on the type of interpretation used.15–17 However, any professional interpretation improves outcomes and is superior to no interpretation or ad hoc interpretation by staff, family or friends.13
Bilingual providers are another resource that can help to improve communication with families who prefer a non-English language. However, it has been shown that a provider’s willingness to use another language in a clinical setting does not equate with his or her language ability18 and it is therefore important that providers demonstrate proficiency prior to using another language with patients and families.19
Although pediatrician use of professional interpretation is increasing, significant gaps still exist. In the ED and office settings, approximately half of patients with LEP receive professional language interpretation.20,21
The objective of this study was to describe patterns of interpreter use in an academic pediatric ED and determine factors associated with use of an interpreter as well as differences in patient outcomes between LEP and English proficient (EP) populations.
METHODS
This was a retrospective cohort study of patients seen in the Seattle Children’s Hospital ED from October 2015 to December 2016. All patient records from this time frame were extracted from the electronic health record and included in the study. This academic pediatric ED in a freestanding children’s hospital is staffed by residents, fellows, and nurse practitioners with supervision provided by faculty trained in pediatric emergency medicine. When a patient is registered in the ED, the following question is asked to screen for LEP: “What is your preferred language for care?” The answer to this screening question is recorded in the patient electronic medical record at each encounter. Registration can occur at any time during an ED visit, but usually occurs near the beginning of the visit. All ED rooms are equipped with dual handset telephones with 1-touch dialing to a vendor who provides interpretation in a large variety of languages. Four mobile touch screen devices are available for video interpretation through a third party vendor that offers real time in-person remote interpretation for 28 languages 24 hours a day, and one in person Spanish interpreter is available and dedicated to the ED during peak hours (2 pm–12 am). Hospital policy permits bilingual providers to conduct care in a foreign language only if they have passed the Clinician Cultural and Linguistic Assessment, a telephonic language certification test for medical providers.22 There are very few ED providers who have this certification: one ED attending, one ED nurse, and approximately 20 of the 129 pediatric residents who rotate through the ED.
Patients who reported preferring a language other than English were designated as having LEP. Vendor billing data for video and phone interpretation time and duration were matched to patient encounter information. In-person interpreter use was determined by electronic orders, so timing and duration for these were not available. For encounters that used phone and video, interpretation within the first 60 minutes of the visit was considered as having been used for the initial assessment, within the last 30 minutes was considered as being used for discharge, and any other timing as mid-visit. The visit was considered to be during a “high volume” time if it occurred between 2 pm and 2 am based on ED visit history.
Demographic information and data related to interpretation encounters, modalities, and timing were evaluated by language. Patient Emergency Severity Index (ESI) triage acuity level, which ranges from 1 (life-threatening emergency) to 5 (anticipated need for limited to no intervention) was captured. The Patient Medical Complexity Algorithm23 (PMCA) category, which classifies children as having no chronic illness, noncomplex chronic illness, or complex chronic illness, was used to determine medical complexity. Patient characteristics were summarized using means, standard deviations, medians, and interquartile ranges for continuous variables, and frequencies and percentages for categorical variables. A sensitivity analysis was performed excluding Spanish speakers, given that a small subset of these patients may receive care from certified bilingual ED providers that we were unable to quantify (Supplementary Table 1).
The cohorts were defined as EP and LEP; the latter was divided into those with record of any interpretation during the visit (phone, video, or in person) and those without. Unadjusted differences in ESI levels between LEP and EP subjects were assessed using a Cochran-Armitage Trend Test, which tests for a linear trend in a cross-tabulation. A linear-mixed effect model with a compound symmetry covariance structure, which assumes correlated measures within subjects assumed to be the same for each set of measures, was used to assess differences in the length of ED stay between LEP patients with and without interpreters and EP patients. Mean LOS was estimated from the model.
Generalized estimating equations (GEE) were used to assess differences in admission, readmission to the ED within 72 hours, and transfer to the ICU within 24 hours of admission to a non-ICU unit between LEP patients with an interpreter, LEP patients without an interpreter, and EP patients. The GEE models accounted for correlation within subject measures. Another GEE analysis was used to assess predictors of interpreter use among LEP patients exclusively.
Significance testing was completed at α = 0.05 level. All analyses were carried out using SAS statistical software version 9.4 (SAS Institute Inc., Cary, NC).
RESULTS
A total of 51,826 patient encounters were evaluated from October 1, 2015 through December 15, 2016. Demographic data, the assigned ESI level, the PMCA categories, and disposition are summarized in Table 1. A total of 19.8% of patients were admitted, and 79.8% of patients were discharged. ICU admissions occurred in 2% of encounters. The overall proportion of patients with a repeat ED visit within 72 hours was 3.3%.
Table 1.
Patient Characteristics and Outcomes
| LEP (N = 5670) N (%) |
EP (N = 31,321) N (%) |
All Patients (N = 36,992)* N (%) |
|
|---|---|---|---|
| Age, median (IQR) | 5.9 (8.5) | 5.7 (9.8) | 5.8 (9.6) |
| Sex | |||
| Male | 3014 (53.2) | 16,710 (53.4) | 19,725 (53.3) |
| Female | 2656 (46.8) | 14,611 (46.7) | 17,267 (46.7) |
| Race and ethnicity | |||
| Non-Hispanic White | 190 (3.4) | 15,767 (50.4) | 15,957 (43.1) |
| Hispanic | 3444 (60.7) | 4238 (13.5) | 7682 (20.8) |
| Black or African American | 790 (13.9) | 3071 (9.8) | 3861 (10.4) |
| Asian | 790 (13.9) | 2461 (7.9) | 3251 (8.8) |
| Native Hawaiian or Other Pacific Islander | 14 (0.3) | 387 (1.2) | 401 (1.1) |
| American indian and Alaska native | 5 (0.1) | 266 (0.9) | 271 (0.7) |
| 2 or more | 59 (1.0) | 1940 (6.2) | 1999 (5.4) |
| Other | 249 (4.4) | 1610 (5.1) | 1859 (5.0) |
| Patient refused | 129 (7.6) | 1576 (5.0) | 1705 (4.6) |
| Readmission within 72 hours | 208 (3.7) | 1289 (4.1) | 1497 (4.1) |
| ICU transfer within 24 hours | 33 (0.6) | 126 (0.4) | 159 (0.4) |
| Length of stay in minutes, mean (SD) | 170.2 (122.8) | 192.7 (128.9) | 189.3 (128.3) |
The total number of encounters was 51,826; the number of distinct patients was 36,992.
The most common ethnicities reported were non-Hispanic White (41.2%), Hispanic (22.2%), African American (11.4%), and Asian (8.4%). A total of 16.2% reported a language preference other than English. The most common languages requested were Spanish (63%), Somali (8.9%), Cantonese or Mandarin (5.4%), Vietnamese (4.9%), Amharic (3.1%), Arabic (2.2%), Oromo (1.8%), Tigrinya (1.6%), and Russian (1.4%).
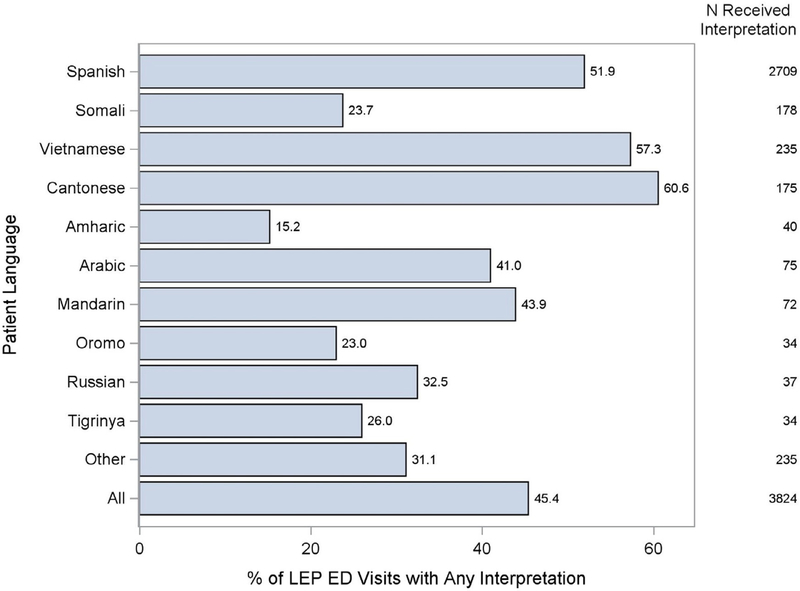
A total of 45.4% of patient encounters where families preferred care in a non-English language had evidence of having received any interpretation during their ED visit (Figure). Of those who received interpretation, 51.6% of the time it was by video, 15.3% in person, and 9.7% by phone; 23.4% received multiple modalities of interpretation. For those who received remote (video or phone) interpretation, 64.8% had interpretation for their initial assessment, 41.2% had interpretation at the time of discharge, and 34.8% had any interpretation during the middle of their visit. When using remote interpretation, a median of 13.3% of the LOS was interpreted.
Figure.
Interpreter use by language.
Factors associated with interpreter use are summarized in Table 2. Interpretation was less likely to be utilized during high volume times of the day (OR 0.85, 95% CI 0.78–0.93) and with each lower level of acuity by ESI (OR 0.66, 95% CI 0.62–0.70). The majority (65.9%) of ESI level 1 patients received interpretation; patients with ESI levels 2–5 had interpretation 60.3%, 48.3%, 40.5%, and 32.7% of the time respectively. The odds of receiving interpretation also decreased by 3% (OR 0.97, 95% CI 0.96–0.98) with each increasing year of patient age.
Table 2.
Predictors for Interpreter Use Among LEP Patients
| Odds Ratio (95% CI) | P Value | |
|---|---|---|
| PMCA | ||
| Non-chronic | Reference | Reference |
| Non-complex chronic | 0.95 (0.82–1.11) | .53 |
| Complex chronic | 1.16 (0.98–1.38) | .09 |
| Age* | 0.97 (0.96–0.98) | <.01 |
| Timing of visit† | ||
| Lower volume time | Reference | Reference |
| Higher volume time | 0.85 (0.78–0.93) | <.01 |
| ESI level‡ | 0.66 (0.62–0.70) | <.01 |
| Repeated encounters§ | 0.92 (0.89–0.95) | <.01 |
| Language | ||
| Spanish | Reference | Reference |
| Amharic | 0.15 (0.10–0.22) | <.01 |
| Arabic | 0.58 (0.41–0.84) | <.01 |
| Cantonese | 1.40 (1.05–1.87) | .02 |
| Mandarin | 0.66 (0.46–0.93) | .02 |
| Oromo | 0.27 (0.17–0.43) | <.01 |
| Other | 0.35 (0.29–0.43) | <.01 |
| Russian | 0.42 (0.27–0.64) | <.01 |
| Somali | 0.26 (0.22–0.32) | <.01 |
| Tigrinya | 0.34 (0.22–0.52) | <.01 |
| Vietnamese | 1.12 (0.88–1.41) | .35 |
Each year of increasing age.
Lower volume: visit between 2 am and 2 pm, higher volume: visit between 2 pm and 2 am.
Average difference between each ESI level from 1 to 5.
Repeated visits for the same patient.
There were differences in the odds that an interpreter would be used during a visit based on language type. Using Spanish as a reference, families speaking African languages were least likely to receive interpretation during their ED encounters: Tigrinya (OR 0.34, 0.22–0.52), Somali (OR 0.26, 0.22–0.32), and Amharic (OR 0.15, 0.10–0.22). Russian and Arabic-speaking families were also less likely to receive interpretation compared to Spanish speakers (Russian OR 0.42, 95% CI 0.27–0.64; Arabic OR 0.58, 95% CI 0.41–0.84). Interpretation for Cantonese was more likely than for Spanish (OR 1.40, 1.05–1.87).
Patient outcomes were compared between LEP and EP patients overall and between LEP with interpretation, LEP without interpretation, and EP (Table 3). In a comparison of LEP and EP patients overall, those with LEP were more likely to be assigned a lower acuity ESI level of 4 or 5 (P < .001). When controlling for ESI and PMCA category, LEP patients who did not receive interpretation were less likely to be admitted than EP patients (OR 0.69, 0.62–0.78); however, when LEP patients received interpretation, their odds of admission were slightly higher than EP patients (OR 1.12, 1.01–1.25). LEP patients, with or without interpretation, were more likely to be transferred from an inpatient unit to the ICU within 24 hours of admission compared to EP patients (LEP with interpretation vs EP: OR 1.76, 1.07–2.90; LEP without interpretation vs. EP: 1.85, 1.08–3.18). There was no difference in the proportion of patients with return visits to this ED when comparing EP to LEP with or without interpretation; information about return visits to other facilities was not available.
Table 3.
Comparison of Health Outcomes Among LEP Patients Who Received Interpretation, LEP Patients Without Interpretation, and EP Patients Who Visited the Emergency Department
| Outcome | Odds Ratio (95% CI) | P Value | |
|---|---|---|---|
| Readmission within 72 hours* | EP | Reference | Reference |
| LEP with interpretation | 0.92 (0.44–1.90) | .82 | |
| LEP without interpretation | 0.38 (0.09–1.51) | .17 | |
| Admission† | EP | Reference | Reference |
| LEP with interpretation | 1.12(1.01–1.25) | .03 | |
| LEP without Interpretation | 0.69 (0.62–0.78) | <.01 | |
| ICU within 24 hours‡ | EP | Reference | Reference |
| LEP with interpretation | 1.76(1.07–2.90) | .03 | |
| LEP without interpretation | 1.85(1.08–3.18) | .02 | |
| Model based mean (SE), in minutes | P value | ||
| Length of stay§ | EP | 196.72 (11.13) | Reference |
| LEP with interpretation | 210.45(11.29) | <.01 | |
| LEP without interpretation | 186.18(11.22) | <.01 | |
Controlling for PMCA Category, timing of visit, age, repeated encounters, and ESI.
Controlling for PMCA Category, ESI, age, repeated encounters, and timing of visit. Model excludes patients who transferred to another facility or expired.
Controlling for PMCA Category, ESI, repeated encounters, timing of visit, and age. (Patients sent to floor and then transferred to ICU).
Controlling for timing of visit, ESI, repeated encounters, and patient age.
The ED LOS was shortest for LEP without interpretation (186.18 minutes) and longest for LEP with interpretation (210.45 minutes) and both were significantly different than the LOS for EP patients (196.72 minutes) (P < .01). The mean LOS for the ED encounters overall during this timeframe was 193.3 minutes.
DISCUSSION
Professional interpretation for families who preferred a non-English language was underutilized in this academic pediatric ED; factors such as lower assigned acuity, increasing patient age, and ED visit during a high volume time of day were associated with a lower likelihood of interpreter use. There were also significant differences for LEP families when compared to EP families in ESI level, ED LOS, and likelihood of admission. For all LEP patients, there was a higher risk of unexpected transfer to the ICU within 24 hours of admission to the inpatient unit.
Interpretation was provided in the ED for less than half (45.4%) of patients who preferred a language other than English for their care. This is despite the National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care guidelines from the Department of Health and Human Services that state patients should have access to linguistically appropriate care in a medical setting.24
Although professional interpretation is not reimbursed in Washington State, our hospital has a relatively well-resourced department for interpreter services and multiple options for providers to access interpretation for clinical encounters. Despite this, we still found that interpretation was underutilized. There were several factors which affected the likelihood of receiving interpretation. The lower odds during times of high ED volumes likely reflect the challenges of using interpretation given the clinical demands on providers. The association between the age of the patient and use of interpretation has not previously been reported and is likely related to the older patient’s ability to communicate independently. There was a lower odds of interpreter use for each year of increasing age. The standard for family centered care is to obtain a history and form a plan in a language that the entire family can understand. In cases where the child is bilingual and EP, it still may be difficult or inappropriate for them to adequately relay information to their family members regarding a diagnosis and care recommendations. In a study of video recording data also collected in this ED, patients of LEP parents who spoke English routinely translated the conversation which had occurred to their parents once a provider left the room.25
Interpretation was less likely to occur for lower acuity patients with an ESI level of 4 or 5, and this may reflect a provider bias about the importance of communication. Previous studies have found that providers’ base decision-making around interpreter use on the anticipated complexity of the discussion, but this does not take into account the family’s needs or goals for care.26 Given that families with LEP have poorer access to primary care and are less likely to have a medical home,2 they may have questions in the ED setting that will not be addressed by another provider in a timely manner. We also found that LEP patients are more likely to be triaged as a level 4 or 5 when compared to EP patients. It may be that these families are using the ED for lower acuity complaints or that they are not given the opportunity to fully explain the details of their child’s symptoms. Under-triage of LEP patients has also been described elsewhere27 and the combination of under-triage and subsequent lower use of interpretation by triage level compounds the risk of missing important information during their visit.
Patients of families who preferred a non-English language had significant differences related to hospital admission when compared to EP patients. When controlling for acuity and medical complexity, patients of families with LEP were less likely be admitted overall; however, patients of families with LEP who received interpretation were slightly more likely to be admitted than the EP patients. Both ESI and PMCA were controlled in our analysis of admission, therefore differences in acuity do not explain the admission differences seen with interpretation. Since ESI is also associated with a lower triage level for LEP patients, any bias introduced in using ESI as a covariate for admission would be in the direction of lower acuity. This might explain the lower proportion of admissions overall, but does not explain why admissions for patients with LEP who received interpretation were actually higher than for EP patients.
The LEP population in this study was more likely to be transferred to the ICU from an inpatient unit within 24 hours of admission than the EP population regardless of interpretation use, suggesting that signs of severity or impending deterioration may have been missed in the ED. This is a crucially important safety measure and introduces the possibility that there is a component of language barrier to the clinical assessment in the ED that might affect appropriate disposition. Interestingly, interpretation use did not make a difference among LEP patients for this outcome, which could be due to the small sample, incomplete or ineffective interpretation for some patients, incomplete or ineffective communication from providers (due to perceived difficulty of using an interpreter), cultural barriers, or implicit bias. Additional investigation will be needed to understand the reasons behind this finding.
When compared to Spanish, patients who spoke languages such as Amharic, Oromo, Somali, and Russian were less likely to receive interpretation. Although in person Spanish interpretation is available during high volume hours of the day, availability of remote (video or phone) interpretation, which is our most commonly used modality, does not differ among these languages. There may be differences in language ability within a family, where 2 parents have a discordant ability to speak and understand English. Some families also present with relatives who are fluent in English to help with communication. More research is needed to determine the different factors involved in use of interpretation and its association with language type.
Defining which families with LEP will benefit from interpretation can also be challenging. The question that we use in our setting, “What language do you prefer for care?” does not necessarily correspond perfectly with language comprehension28 and there is likely a subset of patients who may not have benefited from interpretation or did not actually want it. Some families state they prefer another language for care when asked, but then either refuse interpretation during the visit or prefer to “get by” without it. Further research is needed to determine exactly when interpretation is desired and additive to the patient experience and overall comprehension.
Finally, the LOS for LEP families receiving interpretation was estimated to be 14 minutes longer than EP patients, representing a 7% difference. Among the LEP patients, the difference for those receiving interpretation was 24 minutes longer than for LEP families not receiving interpretation. The shortest LOS among the three groups (EP, LEP with and without interpretation) was for the LEP patients who did not receive interpretation, but does not take into account what may have been missed during the visit. The shorter LOS for that group suggests they may have received less communication than the EP group. Interpretation does take some time, but it is a small proportion of the overall visit and overall LOS is similar to that of EP patients. There are financial and logistical implications of providing interpretation that were not addressed in this study given the resources available at our institution, but they cannot be ignored when addressing barriers to interpretation use in the ED (and outpatient) setting. This difference in LOS may be a helpful consideration for other institutions in this regard.
There were several limitations to this study. Results of this single center study may not be generalizable to other settings. Because of the retrospective design, our data are limited by any omissions or errors that occurred in the medical record. Documentation of interpreter use by a provider order or by matching vendor billing data to the medical record is a challenge because we do not know how much of any particular visit was interpreted. However, monthly audits of overall interpreter use for families with a language preference other than English were not significantly different than the numbers in our dataset. Defining exactly which patients want and would benefit from interpretation beyond the “preferred language” question is another ongoing challenge and opportunity for future work. In some cases, families may decline interpretation for a number of reasons while others who are EP may prefer to speak in another language in a highly stressful or complex situation. Therefore, there may be misclassification of our denominator of families who request another language. We hope to focus future work on empowering families to access interpretation when they wish to have it. We also did not have a way to track interactions with bilingual providers and, with an increasingly diverse work force, it will be important to consider the role of providers who speak the patient’s preferred language directly.
CONCLUSION
In this retrospective cohort study of over 51,000 encounters in an academic pediatric ED, we found that fewer than half of patient encounters for families who preferred a language other than English had evidence of receiving any interpretation during their visit. The following factors were significantly associated with a lower odds of interpreter use: visit occurring during a high volume time of day, lower triage acuity by ESI, and each year of increasing child age. There were also significant differences in patient outcomes for LEP families in comparison to EP families. LEP patients were more likely overall to be assigned a lower triage acuity level than EP patients. When controlling for acuity and complexity, LEP children who did not receive interpretation were less likely to be admitted than EP patients; those who did receive interpretation were slightly more likely to be admitted than EP patients. LEP patients, with or without interpretation, were more likely to be transferred to the ICU within 24 hours of admission than EP patients, raising concerns for underestimating the child’s illness severity due to language barriers. The findings suggest that interventions should emphasize provider decision making around interpreter use and the associated clinical outcomes. Current interventions include education for providers and nurses, increasing availability and ease of use of remote interpretation units, and tracking when interpretation is used during a visit to encourage its use multiple times including for updates and discharge. Process changes are needed to identify LEP patients earlier in their visit and to make their preference more visible to the ED care team. Future work should include a multisite collaboration to look at trends of interpretation use and its impact on the quality of care in different regions of the United States with different patient populations, reimbursement policies, and access to interpretation modalities.
Supplementary Material
Footnotes
SUPPLEMENTARY DATA
Supplementary data related to this article can be found online at https://doi.org/10.1016Zj.acap.2019.07.006.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.U.S. Census Bureau 2016. American Community Survey 1-Year Estimates. Language Spoken at Home. American Fact Finder. https://factfinder.census.gov Published 2016 Accessed April 2, 2018. [Google Scholar]
- 2.Eneriz-Wiemer M, Sanders LM, Barr DA, et al. Parental limited English proficiency and health outcomes for children with special health care needs: a systematic review. Acad Pediatr. 2014;14:128–136. 10.1016/j.acap.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Sanders LM, Thompson VT, Wilkinson JD. Caregiver health literacy and the use of child health services. Pediatrics. 2007;119:e86–e92. 10.1542/peds.2005-1738. [DOI] [PubMed] [Google Scholar]
- 4.Hampers LC, Mcnulty JE. Professional interpreters and bilingual physicians in a pediatric emergency department. Arch Pediatr Adolesc Med. 2002;156:1108 10.1001/archpedi.156.11.1108. [DOI] [PubMed] [Google Scholar]
- 5.Rogers AJ. The effect of limited English proficiency on admission rates from a pediatric emergency department: stratification by acuity. Acad Emerg Med. 2003;10:435 10.1197/aemj.10.5.435. [DOI] [PubMed] [Google Scholar]
- 6.Gallagher RA, Porter S, Monuteaux MC, et al. Unscheduled return visits to the emergency department. Pediatr Emerg Care. 2013; 29:579–583. 10.1097/pec.0b013e31828e62f4. [DOI] [PubMed] [Google Scholar]
- 7.Levas MN, Dayan PS, Mittal MK, et al. Effect of Hispanic ethnicity and language barriers on appendiceal perforation rates and imaging in children. J Pediatr. 2014;164:1286–1291. 10.1016/j.jpeds.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Arthur KC, Mangione-Smith R, Meischke H, et al. Impact of English proficiency on care experiences in a pediatric emergency department. Acad Pediatr. 2015;15:218–224. 10.1016/j.acap.2014.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Fields A, Abraham M, Gaughan J, et al. Language matters. Pediatr Emerg Care. 2016;32:222–226. 10.1097/pec.0000000000000453. [DOI] [PubMed] [Google Scholar]
- 10.Cohen AL. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. 2005;116:575–579. 10.1542/peds.2005-0521. [DOI] [PubMed] [Google Scholar]
- 11.Schenker Y, Wang F, Selig SJ, et al. The impact of language barriers on documentation of informed consent at a hospital with on-site interpreter services. J Gen Intern Med. 2007;22:294–299. 10.1007/s11606-007-0359-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jimenez N, Jackson DL, Zhou C, et al. Postoperative pain management in children, parental English proficiency, and access to interpretation. Hosp Pediatr. 2014;4:23–30. 10.1542/hpeds.2013-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flores G, Abreu M, Barone CP, et al. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann Emerg Med. 2012;60:545–553. 10.1016/j.annemergmed.2012.01.025. [DOI] [PubMed] [Google Scholar]
- 14.Jimenez N, Jackson DL, Zhou C, et al. Postoperative pain management in children, parental English proficiency, and access to interpretation. Hosp Pediatr. 2014;4:23–30. 10.1542/hpeds.2013-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lion KC, Brown JC, Ebel BE, et al. Effect of telephone vs video interpretation on parent comprehension, communication, and utilization in the pediatric emergency department. JAMA Pediatr. 2015;169:1117–1125. 10.1001/jamapediatrics.2015.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crossman KL, Wiener E, Roosevelt G, et al. Interpreters: telephonic, in-person interpretation and bilingual providers. Pediatrics. 2010;125: e631–e638. 10.1542/peds.2009-0769. [DOI] [PubMed] [Google Scholar]
- 17.Grover A, Deakyne S, Bajaj L, et al. Comparison of throughput times for limited English proficiency patient visits in the emergency department between different interpreter modalities. J Immigr Minor Health. 2011;14:602–607. 10.1007/s10903-011-9532-z. [DOI] [PubMed] [Google Scholar]
- 18.Lion KCL, Thompson DA, Cowden JD, et al. Clinical Spanish use and language proficiency testing among pediatric residents. Acad Med. 2013;88:1478–1484. 10.1097/ACM.0-b013e3182a2e30d. [DOI] [PubMed] [Google Scholar]
- 19.Lion KCL, Thompson DA, Cowden JD, et al. Impact of language proficiency testing on provider use of Spanish for clinical care. Pediatrics. 2012;130:e80–e87. 10.1542/peds.2011-2794. [DOI] [PubMed] [Google Scholar]
- 20.Wallbrecht J, Hodes-Villamar L, Weiss SJ, et al. No difference in emergency department length of stay for patients with limited proficiency in English. South Med J. 2014;107:1–5. 10.1097/smj.0000000000000037. [DOI] [PubMed] [Google Scholar]
- 21.DeCamp LR, Kuo DZ, Flores G, et al. Changes in language services use by US pediatricians. Pediatrics. 2013;132:e396–e406. 10.1542/peds.2012-2909d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clinician Cultural and Linguistic Assessment | Kaiser CCLA. ALTA Language Services. http://www.altalang.com/language-testing/ccla/Accessed April 2, 2018.
- 23.Simon TD, Cawthon ML, Stanford S, et al. Pediatric medical complexity algorithm: a new method to stratify children by medical complexity. Pediatrics. 2014;133:e1647-e1654 10.1542/peds.2013-3875d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Department of Health and Human Services. National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care. https://www.federalregister.gov/documents/2013/09/24/2013-23164/national-standards-for-culturally-and-linguistically-appropriate-services-clas-in-health-and-health Published September 24, 2013. Accessed September 17, 2018.
- 25.Lion KC, Brown JC, Ebel BE, et al. “Patterns and predictors of professional interpreter use in the pediatric emergency department” Presented at the Pediatric Academic Societies Annual Meeting; San Diego, CA: April 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Diamond L, Schenker Y, Bradley EH, et al. Getting by: underuse of interpreters by resident physicians. J Gen Intern Med. 2009;24:256–262. 10.1007/s11606-008-0875-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grigg A, Shetgiri R, Michel E, et al. Factors associated with nonurgent use of pediatric emergency care among Latino families. J Natl Med Assoc. 2013;105:77–84. 10.1016/s0027-9684(15)30088-2. [DOI] [PubMed] [Google Scholar]
- 28.Okrainec K, Miller M, Holcroft C, et al. Assessing the need for a medical interpreter: are all questions created equal? J Immigr Minor Health. 2014;16:756–760. 10.1007/s10903-013-9821-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.