Supplemental Digital Content is available in the text
Abstract
BACKGROUND
Perception of halitosis in patients during intubation is a common and additional stressor for anaesthesiologists and may lead to potential health risks.
OBJECTIVES
We hypothesised that intubation with videolaryngoscopy could help reduce the anaesthesiologists’ perception of patients’ oral malodor during intubation.
DESIGN
A single-blinded, randomised controlled trial.
SETTING
Single centre general hospital, Guangdong Province, China.
PARTICIPANTS
A total of 440 patients who underwent intubation under general anaesthesia for elective surgery, aged 18 to 60 years old, American Society of Anaesthesiologists class I to III, without upper airway abnormality or airway infection were enrolled.
INTERVENTION
Patients were randomly assigned to receive either UE videolaryngoscopy (UE) or Macintosh's direct laryngoscopy (Macintosh) group. All intubations were performed by one of six very experienced anaesthesiologists.
MAIN OUTCOME MEASURES
The patient's oral odour score was measured prior to induction of anaesthesia. The anaesthesiologists’ perception of the patient's oral malodor during intubation was recorded. The shortest distance from patient's mouth to the anaesthesiologist's nose (MN distance), the exertion rating and discomfort were also measured.
RESULTS
The oral malodor score did not differ in the UE and Macintosh groups prior to the induction of anaesthesia. However, the incidence of the anaesthesiologists’ perception of halitosis during intubation was significantly lower in the UE group compared with the Macintosh group (P < 0.001). Similarly, the MN distance was significantly greater in the UE group compared with the Macintosh group (P < 0.001). The first-attempt success rate was higher in the UE group compared to the Macintosh group (P < 0.001). However, the exertion scores were considerably higher in the Macintosh group. After intubation, anaesthesiologists experienced more waist and shoulder discomfort with the Macintosh than the UE technique of intubation.
CONCLUSION
Compared with direct laryngoscopy, videolaryngoscopy might reduce the anaesthesiologists’ perception of the patients’ oral malodor, help improve first-attempt success rate, as well as alleviate the anaesthesiologists’ waist and shoulder discomfort.
TRIAL REGISTRATION
Clinicaltrials.gov (ChiCTR-IOR-15007038).
Introduction
Chinese anaesthesiologists experience a considerable degree of burnout and low job satisfaction.1 Anaesthesiologists are usually exposed to potential health risks, including occupational hazards, in their day-to-day practice.2,3 The occupational hazards include physical risks (e.g. noise), ergonomic risks (e.g. awkward postures) and mental risks (e.g. stress that may cause work absence or work-related disorders).4,5 Doleman et al.6 found an association between the patient's American Society of Anaesthesiologists (ASA) grade and the anaesthesiologist's risk of increased stress as well as impairment of nontechnical skills during intubation. The administration of general anaesthesia is one of the most frequently conducted procedures in anaesthesiology. The mental and physical workloads can be intense during general anaesthesia, and the awkward posture that anaesthesiologists employ during intubation has been reported as a stressor.7 In addition, the patient's oral malodor would prove to be unpleasant or offensive for the anaesthesiologist during intubation.
Oral malodor, also known as halitosis or bad breath, ranges from 2% to more than 70% in the general population.8–10 At our hospital, our pilot data found that nearly 40% of patients manifest halitosis during intubation, which poses an additional stressor that may be a potential risk to patient safety during anaesthesia. Despite the prevalence of the problem that halitosis poses for anaesthesiologists, objective data on this topic are absent from the literature.
Videolaryngoscopy – compared with Macintosh's direct laryngoscopy – facilitates a more ergonomic posture for anaesthesiologists7,11 and provides an extended distance to the head of the manikin during intubation.12 Moreover, the greater proximity of the patient's mouth to the anaesthesiologist's nose might worsen the discomfort caused by the patient's halitosis and may impair the efficiency with which the anaesthesiologist operates.
The effects of different laryngoscopic techniques on anaesthesiologists’ perception of patients’ halitosis has remained largely unknown, although it is hypothesised that the greater proximity of the patient's mouth to the anaesthesiologist's nose could worsen the malodor-induced discomfort and possibly influence the anaesthesiologist's performance of duties.
The present clinical trial was designed to investigate the anaesthesiologist's perception of patients’ oral malodor during intubation with different laryngoscopic techniques.
Methods
Study population
This randomised, single-blind, prospective, controlled study enrolled patients who were scheduled to undergo intubation under general anaesthesia for elective surgery. The inclusion criteria were age between 18 and 60 years; ASA physical status I/II/III; no upper airway abnormality; no airway infection; and written informed consent for study participation.
Patients were randomly assigned to receive either UE videolaryngoscopy (UE) or Macintosh's direct laryngoscopy (Macintosh) on the basis of a computer-generated randomisation number table that was revealed via a sealed envelope when the enrolled patient was in the operation theatre. This study was conducted in accordance with the principles of the Declaration of Helsinki, and approved by the Institutional Review Board of the Third Affiliated Hospital of Sun Yat-sen University (approval no. [2014]2–117). The study was registered with the Chinese Clinical Trial Registry at www.chictr.org on 8 September 2015 (registration no. ChiCTR-IOR-15007038).
Sample size
Based on the retrospective data from our institution in the same anaesthetic group, the prevalence of oral malodor was quantified to be as much as 30%. We hypothesised UE videolaryngoscopy would halve the incidence of anaesthesiologist's perception of patients’ halitosis. Based on our study parameters, EpiCalc 2000 (downloaded from http://www.brixtonhealth.com/epicalc.html) specified that 156 participants were required in each group, with a power of 90%; a two-tailed P value of less than 0.05 was considered indicative of statistical significance. We factored in a 20% dropout, and estimated that a minimum of 188 participants were required in each group.
Study procedures
The anaesthesiologist asked the patients to exhale to the Halitosis Detector (TANITA, HC-2126-WH, detecting the volatile sulfide compounds in the exhaust gas) to measure the oral odour (score ≤5) prior to induction of anaesthesia. All procedures were performed according to the manufacturer's instructions (as shown in Supplementary Fig. 1). Patients were blinded to the type of laryngoscopy that was carried out.
The standardised anaesthesia protocol consisted of intravenous induction with midazolam (0.1 mg kg−1), fentanyl (2 to 4 μg kg−1), propofol (1 to 2 mg kg−1) and cisatracurium (0.2 mg kg−1). Each tracheal tube was lubricated with a water-based agent before placement. All intubations were carried out by one of six expert anaesthesiologists, who were skilled in different laryngoscopic techniques and had work experience of more than 5 years. The time to successful intubation was measured from the moment of blade insertion into the patients’ mouth to the first capnography upstroke after intubation. An intubation failure was recorded when the tube could not be successfully placed within two attempts. Following intubation, the anaesthesiologists immediately recorded the exertion rating, which was defined as the length in centimetres from 0 (no exertion) to 10 (heavy exertion) on the visual analogue scale (VAS). During the intubation, we recorded the shortest distance from patient's mouth to the anaesthesiologist's nose (mouth to nose distance, MN distance, as shown in Fig. 1) by a laser distance detector (BOSCH, Professional GLM25).
Fig. 1.

Determination of MN distance. MN distance means the shortest distance from patient's mouth to the anaesthesiologist's nose, it was measured by a laser distance detector (BOSCH, Professional GLM25). MN, mouth to nose.
Primary and secondary outcome variables
The primary outcome of our investigation was the incidence of the anaesthesiologists’ perception of the patient's oral malodor. Secondary outcome variables included the MN distance, rate of the first successful intubation, intubation time, and complications.
Statistical analysis
Qualitative/rank data are presented as the percentage/composition ratio; we used the nonparametric test, Pearson's χ2 test, or Fisher's exact probabilities to detect the between-group differences. Continuous variables were expressed as mean ± SD and analysed with the Student t test. Two-tailed P values of less than 0.05 were considered significant. All analyses were conducted on SPSS 19.0 (SPSS Inc., Chicago, Illinois, USA).
Results
We enrolled a total of 440 patients in the current study. We excluded one patient because of intubation failure with UE videolaryngoscopy, and a subsequent successful intubation by fiberbronchoscopy. Three patients in the Macintosh group were intubated by UE videolaryngoscopy, subsequent to intubation failure with Macintosh laryngoscopy. Therefore, data of 436 patients were included in the final analyses. The patient disposition in this study is shown in Fig. 2.
Fig. 2.
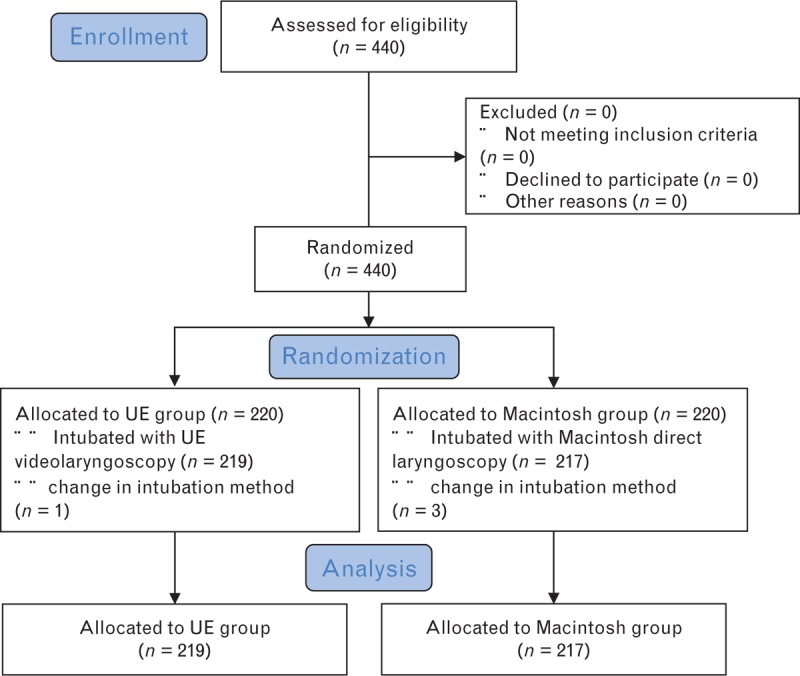
CONSORT flow chart of patient disposition in the study.
Patient characteristics in the UE and Macintosh groups did not differ significantly with regard to sex, age, weight, height, BMI, ASA physical status, pre-existing diseases, Modified Mallampati Score or the thyromental distance (Table 1).
Table 1.
Peri-operative baseline variables
| Variables | Group 1-U, n = 219 | Group 2-M, n = 217 | P value |
| Sex, n (%) | 0.928 | ||
| Male | 117 (53.42) | 115 (53.00) | |
| Female | 102 (46.58) | 102 (47.00) | |
| Age (years) | 45.03 ± 0.96 | 45.69 ± 1.05 | 0.642 |
| Height (cm) | 163.28 ± 0.54 | 163.26 ± 0.551 | 0.980 |
| Weight (kg) | 61.43 ± 0.90 | 60.03 ± 0.65 | 0.212 |
| BMI, n (%) | 0.374 | ||
| <18.5 | 22 (10.05) | 24 (11.06) | |
| 18.5 to 23.9 | 117 (53.42) | 129 (59.45) | |
| 24 to 28 | 66 (30.14) | 56 (25.81) | |
| >28 | 14 (6.39) | 8 (3.69) | |
| ASA, n (%) | 0.207 | ||
| 1 | 75 (34.25) | 92 (42.40) | |
| 2 | 131 (59.82) | 115 (53.00) | |
| 3 | 13 (5.94) | 10 (4.60) | |
| SBP | 123.84 ± 1.39 | 124.06 ± 1.39 | 0.912 |
| DBP | 74.78 ± 1.04 | 75.42 ± 1.06 | 0.837 |
| MBP | 90.61 ± 1.03 | 90.85 ± 0.98 | 0.863 |
| HR | 74.03 ± 0.73 | 74.99 ± 0.68 | 0.671 |
| Modified Mallampati Score, n (%) | 0.311 | ||
| 1 | 97 (44.29) | 90 (41.47) | |
| 2 | 104 (47.49) | 108 (49.77) | |
| 3 | 15 (6.85) | 19 (8.76) | |
| 4 | 3 (0.014) | 0 (0) | |
| Mouth opening <3 fingers, n (%) | 0 (0) | 0 (0) | 1.000 |
| Thyromental distance <6.5 cm, n (%) | 3 (0.014) | 1 (0.005) | 0.622 |
Values are expressed as an absolute number (proportion) or mean ± SD. Group-1-U, UE group; Group-2-M, Macintosh group; HR, heart rate; MBP, mean blood pressure.
The oral malodor score was measured successfully in all patients and did not differ in the UE and Macintosh groups prior to the induction of anaesthesia. However, the incidence of the anaesthesiologists’ perception of halitosis in patients during intubation was significantly lower in the UE group compared with the Macintosh group (P < 0.001; Table 2). Similarly, the MN distance during intubation was significantly greater in the UE group compared with the Macintosh group (P < 0.001; Table 3).
Table 2.
Primary outcome between the two groups
| Variables | Group 1-U, n = 219 | Group 2-M, n = 217 | P value |
| Oral malodor score, n | 0.135 | ||
| 0 | 0 (0) | 0 (0) | |
| 1 | 111 (50.7) | 105 (48.4) | |
| 2 | 87 (39.7) | 82 (37.8) | |
| 3 | 19 (8.7) | 30 (13.8) | |
| 4 | 2 (0.9) | 0 (0) | |
| 5 | 0 (0) | 0 (0) | |
| Oral malodor score, n | 0.169 | ||
| 0 to 2 | 198 (90.4) | 187 (86.2) | |
| 3 to 5 | 21 (9.6) | 30 (13.8) | |
| Perception of patients’ oral malodor during intubation | 5 (2.3) | 72 (33.2) | 0.000 |
Values are expressed as an absolute number (proportion). The oral malodor scores of patients were detected using a halitosis detector before the induction of anaesthesia. The oral odour was stratified into six scores (0 to 5). Group-1-U, UE group; Group-2-M, Macintosh group.
Table 3.
Secondary outcomes between the two groups
| Variables | Group 1-U, n = 219 | Group 2-M, n = 217 | P value |
| MN distance (mm) | 401.11 ± 3.24 | 202.88 ± 3.91 | 0.000 |
| Intubation time (s) | 43.99 ± 0.72 | 26.40 ± 0.53 | 0.000 |
| Glottis exposure score under laryngoscopy, n | 0.000 | ||
| 1 | 177 | 37 | |
| 2 | 40 | 119 | |
| 3 | 2 | 66 | |
| 4 | 0 | 5 | |
| Lifting strength scale | 0.000 | ||
| 1 | 126 | 7 | |
| 2 | 39 | 15 | |
| 3 | 35 | 10 | |
| 4 | 18 | 15 | |
| 5 | 0 | 23 | |
| 6 | 0 | 34 | |
| 7 | 1 | 70 | |
| 8 | 0 | 36 | |
| 9 | 0 | 7 | |
| Lifting strength scale | 0.000 | ||
| 1 to 3 | 200 | 32 | |
| 4 to 6 | 18 | 72 | |
| 7 to 10 | 1 | 113 | |
| First-attempt success rate, n (%) | 205 (93.61) | 191 (88.02) | 0.043 |
| Waist discomfort | 0.000 | ||
| No | 131 (59.82) | 59 (27.19) | |
| Mild | 79 (36.07) | 96 (44.24) | |
| Moderate | 9 (4.11) | 60 (27.65) | |
| Severe | 0 (0) | 2 (0.92) | |
| Shoulder discomfort | 0.000 | ||
| No | 127 (57.99) | 62 (28.57) | |
| Mild | 78 (35.62) | 95 (43.78) | |
| Moderate | 14 (6.39) | 59 (27.19) | |
| Severe | 0 (0) | 1 (0.46) |
Values are expressed as an absolute number (proportion) or mean ± SD. The glottis exposure score under laryngoscopy was graded as: Grade 1, full view of the vocal cords; Grade 2, partial view of the cords including arytenoids; Grade 3, epiglottis only; and Grade 4, others (pharynx, other). The lifting strength scale was assessed by VAS: from 0 (no exertion) to 10 (maximal exertion). Group-1-U, UE group; Group-2-M, Macintosh group; MN, mouth to nose; VAS, visual analogue scale.
The ability to view the vocal cords was graded as: Grade 1, full view of the vocal cords; Grade 2, partial view of the cords including arytenoids; Grade 3, epiglottis only; and Grade 4 others (pharynx, other). Grades 1 and 2 were considered to be good views. As expected, the view grades were much better in the UE group than in the Macintosh group (P < 0.001; Table 3). Accordingly, the first-attempt success rate was higher in the UE group versus the Macintosh group (P < 0.001; Table 3). However, the intubation time was much shorter in the Macintosh group in comparison with that of the UE group.
The exertion [lifting strength, assessed by VAS: from 0 (no exertion) to 10 (maximal exertion)] were considerably higher in the Macintosh group compared with the UE group (P < 0.001; Table 3). Therefore, after intubation, anaesthesiologists experienced more waist and shoulder discomfort with the Macintosh than the UE technique of intubation.
Discussion
As anaesthesiologists, we may begin our day-work with a pleasant endotracheal intubation. Once we smell oral malodor during intubation, we have to endure it until the intubation process is over. Anyway, it's absolutely not a pleasant experience. Improving the anaesthesiologist's perception of the patients during intubation may be beneficial to both – better work efficiency and less occupational stress; however, there has been no research undertaken on this problem until now. In the current study, we compared UE videolaryngoscopy and Macintosh's direct laryngoscopy to investigate the effects of the laryngoscopic technique on the anaesthesiologist's perception of the patient's oral odour. Compared with Macintosh's direct laryngoscopy, UE videolaryngoscopy led to a statistically significant reduction in the anaesthesiologist's perception of patient's oral odour as well as the MN distance. Furthermore, UE videolaryngoscopy improved the ability to view the vocal cords as well as the first-attempt success rate; in addition, it alleviated the waist and shoulder discomfort of anaesthesiologists but extended the intubation time.
These results may not come as a surprise to many anaesthesiologists who have used UE videolaryngoscopy. Previous studies have shown that videolaryngoscopy ensures a more erect operator position, including smaller neck and upper arm deflections, than with the Macintosh blade.7,12 Accordingly, the current study directly measured the MN distance and found that UE videolaryngoscopy extended the distance, compared with the Macintosh blade. As a result, the anaesthesiologist's perception of the patient's oral odour was much lower in the UE group, compared with the Macintosh group.
Oral malodor – a disagreeable odour emanating from the mouth – could be caused by various oral conditions including periodontal disease, improper dental restorations or nonoral aetiological factors (e.g. infections, gastrointestinal ulcerations and metabolic disorders).10,13 The prevalence of oral malodor varies from 2 to 70% in different studies and affects a large population as a cause of embarrassment.14,15 Anaesthesiologists may find the patient's oral malodor discomforting and distracting. Intubation is a critical procedure associated with potentially intense mental and physical workloads.16,17 Particularly, in emergency intubation outside the operation theatre, the operator may be exposed to infectious agents including blood or other secretions of the patient.5 To obtain a good view of the glottis, the operator has to adjust his/her body posture to gain binocular vision while simultaneously completing the optimal lifting and pushing actions that require specific neck and upper arm deflections.18,19 Thus, emergency intubation is associated with a higher risk for the operator as well as difficulty in laryngoscopic intubation.20,21 Previous studies have shown that videolaryngoscopy, compared with direct laryngoscopy, is associated with improved ergonomic postures of the operator and glottic visualisation of the patients.12,22 In the current study, intubation with videolaryngoscopy significantly reduced the operator's perception of the patients’ oral odour, reduced waist and shoulder discomfort and increased the first-attempt success rate.
The Macintosh blade is a device that requires the alignment of the patient's mouth, pharynx and tracheal axes to obtain a direct view of the glottis. In contrast, a videolaryngoscope allows the operator to indirectly achieve better visualisation of the glottis and decreases the requirement for optimisation of certain operator neck and upper arm deflections.23 The erect position would shorten the MN distance and consequently lessen the discomfort caused by the patient's oral malodor, as proved in the current study. The ergonomic posture was probably attributed to lesser peak lifting force on the base of the tongue during laryngoscopy with a videolaryngoscope, compared with that using the Macintosh blade.24 Therefore, the operator's waist and shoulder discomfort would be improved, and the perception of patient's oral malodor would diminish.
The first-attempt success rate was high with the UE videolaryngoscope, compared with that with the Macintosh blade; however, the intubation time was significantly longer with UE, rather than Macintosh laryngoscopy. Although a previous meta-analysis showed that the shorter intubation time with the videolaryngoscope was confined to nonexpert rather than expert – operators,22 all of our patients were intubated by expert operators. Sulser et al.25 demonstrated that visualisation of the vocal cords was improved by using the C-MAC videolaryngoscope compared with direct laryngoscopy, but better visualisation did not improve first-attempt success rate, which in turn was probably based on the high level of experience of the participating anaesthesia consultants. We noticed that the angle of the lens is 15 to 20 degrees for direct laryngoscopes and 30 to 42 degrees for the UE videolaryngoscope (As shown in the Supplementary Fig. 2). Using a direct laryngoscope, the catheter can be inserted more directly and quickly into the trachea, because the three axes of the upper respiratory tract coincide.26 However, the distal end of the tracheal tube should be bent at a larger angle to facilitate its smooth insertion into the trachea when using a UE videolaryngoscope, and this will prolong the intubation time (As shown in the Supplementary Fig. 3).
Furthermore, given that the large angle of the lens can more easily facilitate better visualisation of the glottis, the videolaryngoscope is used most often in patients who have predictors for difficult direct laryngoscopy.27,28 Considering the benefits of Macintosh and UE videolaryngoscope blades together, we suggest that a videolaryngoscope with an adjustable lens not only helps anaesthesiologists intubate their patients smoothly, but also extends the MN distance and reduces the perception of halitosis.
The current study had some limitations. First, the study was a single-centre clinical trial. Therefore, these preliminary results need to be confirmed by a large-scale multicenter study. Second, the parameter used to measure the patients’ oral odour during intubation was subjective. Therefore, the perceptions of different anaesthesiologists with regard to the patients’ oral odour could be subject to individual biases, and the results need to be confirmed by a single anaesthesiologist in future research.
Conclusion
In summary, our results focus on the effect of different laryngoscopic techniques on the anaesthesiologists’ perception of the patients’ oral odour. Compared with Macintosh's direct laryngoscopy, UE videolaryngoscopy might reduce the anaesthesiologists’ perception of the patients’ oral malodor, help improve vocal cord visualisation and first-attempt success rate, as well as alleviate the discomfort in the anaesthesiologists’ waist and shoulder.
Supplementary Material
Acknowledgements relating to this article
Assistance with the study: the authors thank all of the patients who kindly participated in this study.
Financial support and sponsorship: none.
Conflicts of interest: none.
Presentation: none.
Chaojin Chen and Ziqing Hei are co-first authors.
Published online 18 October 2019
References
- 1.Li H, Zuo M, Gelb AW, et al. Chinese anesthesiologists have high burnout and low job satisfaction: a cross-sectional survey. Anesth Analg 2018; 126:1004–1012. [DOI] [PubMed] [Google Scholar]
- 2.Andrade GO, Dantas RA. Work-related mental and behaviour disorders in anesthesiologists. Braz J Anesthesiol 2015; 65:504–510. [DOI] [PubMed] [Google Scholar]
- 3.Santovito A, Cervella P, Delpero M. Evaluation of genomic damage in peripheral lymphocytes from occupationally exposed anesthetists: assessment of the effects of age, sex, and GSTT1 gene polymorphism. J Biochem Mol Toxicol 2015; 29:234–239. [DOI] [PubMed] [Google Scholar]
- 4.Van der Wal RAB, Wallage J, Bucx MJL. Occupational stress, burnout and personality in anesthesiologists. Curr Opin Anaesthesiol 2018; 31:351–356. [DOI] [PubMed] [Google Scholar]
- 5.Volquind D, Bagatini A, Monteiro GM, et al. Occupational hazards and diseases related to the practice of anesthesiology. Braz J Anesthesiol 2013; 63:227–232. [DOI] [PubMed] [Google Scholar]
- 6.Doleman B, Blackwell J, Karangizi A, et al. Anaesthetists stress is induced by patient ASA grade and may impair nontechnical skills during intubation. Acta Anaesthesiol Scand 2016; 60:910–916. [DOI] [PubMed] [Google Scholar]
- 7.Caldiroli D, Molteni F, Sommariva A, et al. Upper limb muscular activity and perceived workload during laryngoscopy: comparison of Glidescope(R) and Macintosh laryngoscopy in manikin: an observational study. Br J Anaesth 2014; 112:563–569. [DOI] [PubMed] [Google Scholar]
- 8.Soder B, Johansson B, Soder PO. The relation between foetor ex ore, oral hygiene and periodontal disease. Swed Dent J 2000; 24:73–82. [PubMed] [Google Scholar]
- 9.Hammad MM, Darwazeh AM, Al-Waeli H, et al. Prevalence and awareness of halitosis in a sample of Jordanian population. J Int Soc Prev Community Dent 2014; 4:S178–S186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Suzuki N, Yoneda M, Takeshita T, et al. Induction and inhibition of oral malodor. Mol Oral Microbiol 2019; 34:85–96. [DOI] [PubMed] [Google Scholar]
- 11.Eismann H, Sieg L, Etti N, et al. Improved success rates using videolaryngoscopy in unexperienced users: a randomized crossover study in airway manikins. Eur J Med Res 2017; 22:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grundgeiger T, Roewer N, Grundgeiger J, et al. Body posture during simulated tracheal intubation: GlideScope((R)) videolaryngoscopy vs Macintosh direct laryngoscopy for novices and experts. Anaesthesia 2015; 70:1375–1381. [DOI] [PubMed] [Google Scholar]
- 13.Messadi DV, Younai FS. Halitosis. Dermatol Clin 2003; 21:147–155. [DOI] [PubMed] [Google Scholar]
- 14.Bornstein MM, Kislig K, Hoti BB, et al. Prevalence of halitosis in the population of the city of Bern, Switzerland: a study comparing self-reported and clinical data. Eur J Oral Sci 2009; 117:261–267. [DOI] [PubMed] [Google Scholar]
- 15.Liu XN, Shinada K, Chen XC, et al. Oral malodor-related parameters in the Chinese general population. J Clin Periodontol 2006; 33:31–36. [DOI] [PubMed] [Google Scholar]
- 16.Weinger MB, Herndon OW, Zornow MH, et al. An objective methodology for task analysis and workload assessment in anesthesia providers. Anesthesiology 1994; 80:77–92. [DOI] [PubMed] [Google Scholar]
- 17.Leedal JM, Smith AF. Methodological approaches to anaesthetists’ workload in the operating theatre. Br J Anaesth 2005; 94:702–709. [DOI] [PubMed] [Google Scholar]
- 18.Walker JD. Posture used by anaesthetists during laryngoscopy. Br J Anaesth 2002; 89:772–774. [PubMed] [Google Scholar]
- 19.Matthews AJ, Johnson CJ, Goodman NW. Body posture during simulated tracheal intubation. Anaesthesia 1998; 53:331–334. [DOI] [PubMed] [Google Scholar]
- 20.Benedetto WJ, Hess DR, Gettings E, et al. Urgent tracheal intubation in general hospital units: an observational study. J Clin Anesth 2007; 19:20–24. [DOI] [PubMed] [Google Scholar]
- 21.Griesdale DE, Bosma TL, Kurth T, et al. Complications of endotracheal intubation in the critically ill. Intensive Care Med 2008; 34:1835–1842. [DOI] [PubMed] [Google Scholar]
- 22.Griesdale DE, Liu D, McKinney J, et al. Glidescope(R) video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anaesth 2012; 59:41–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Latif RK, Akca O. Simulation based training of airway management with Macintosh blade and Glidescope video laryngoscope. Minerva Anestesiol 2011; 77:1–3. [PubMed] [Google Scholar]
- 24.Russell T, Khan S, Elman J, et al. Measurement of forces applied during Macintosh direct laryngoscopy compared with GlideScope(R) videolaryngoscopy. Anaesthesia 2012; 67:626–631. [DOI] [PubMed] [Google Scholar]
- 25.Sulser S, Ubmann D, Schlaepfer M, et al. C-MAC videolaryngoscope compared with direct laryngoscopy for rapid sequence intubation in an emergency department: a randomised clinical trial. Eur J Anaesthesiol 2016; 33:943–948. [DOI] [PubMed] [Google Scholar]
- 26.Riveros R, Sung W, Sessler DI, et al. Comparison of the Truview PCD and the GlideScope® video laryngoscopes with direct laryngoscopy in pediatric patients: a randomized trial. Can J Anaesth 2013; 60:450–457. [DOI] [PubMed] [Google Scholar]
- 27.Aziz MF, Healy D, Kheterpal S, et al. Routine clinical practice effectiveness of the Glidescope in difficult airway management: an analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology 2011; 114:34–41. [DOI] [PubMed] [Google Scholar]
- 28.Stroumpoulis K, Pagoulatou A, Violari M, et al. Videolaryngoscopy in the management of the difficult airway: a comparison with the Macintosh blade. Eur J Anaesthesiol 2009; 26:218–222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


