Abstract
Purpose: We describe the development, implementation, and outcomes of role-emerging (RE) clinical placements at Positive Living Niagara (PLN), a community-based HIV organization (CBHIVO), for two second-year, entry-level Master of Science (Physiotherapy) (MSc[PT]) students from McMaster University. Client Description: A national, not-for-profit organization, Realize, conducted outreach to identify CBHIVOs interested in developing physiotherapy (PT) student placements. Intervention: PLN responded to the outreach and worked with McMaster’s MSc(PT) programme and Realize to establish two part-time RE PT student placements. The placement description and expectations were developed collaboratively by PLN, Realize, and the MSc(PT) programme. All PT students participating in their third 6-week clinical placement were eligible to apply. A registered occupational therapist and physiotherapist and PLN’s programme services manager participated in a shared model to supervise the students’ clinical and administrative activities. Measures and Outcome: These first RE PT placements in a Canadian CBHIVO were completed between November and December 2016. The evaluation of the student and placement included a learning contract and the Canadian Physiotherapy Assessment of Clinical Performance. Over 6 weeks, the students collaborated with people living with HIV (PLWHIV) who were members of PLN to identify a role for physiotherapists at PLN and led two health promotion workshops for PLN’s members and staff. Implications: The RE PT placement identified future opportunities for physiotherapists at PLN. The experience also influenced one student’s decision to apply after graduation for a newly created PT position that included working with PLWHIV.
Key Words: case report, community health planning, HIV, internship, interprofessional
Abstract
Objectif : présenter la création, la mise en œuvre et les résultats de stages cliniques en milieux émergents (MÉ) au sein de Positive Living Niagara (PLN), un organisme communautaire voué au VIH (OCVIH) où ont séjourné deux étudiants à la maîtrise en physiothérapie de l’université McMaster. Description du client : un organisme à but non lucratif national, Realize, a demandé à des OCVIH s’ils aimeraient accueillir des stages en physiothérapie. Intervention : PLN a répondu et, conjointement avec le programme de maîtrise en physiothérapie de McMaster, a mis sur pied deux stages en physiothérapie à temps partiel en MÉ. PLN, Realize et le programme de maîtrise ont rédigé ensemble la description du stage et les attentes. Tous les étudiants en physiothérapie qui participaient à leur troisième stage clinique de six semaines étaient admissibles. Un ergothérapeute agréé, un physiothérapeute et le chef des services relatifs aux programmes de PLN ont participé à un modèle de supervision partagé des activités cliniques et administratives des étudiants. Mesures et résultats : Ces premiers stages de physiothérapie en MÉ tenus dans un OCVIH canadien ont eu lieu entre novembre et décembre 2016. L’évaluation de l’étudiant et du stage incluait un contrat d’apprentissage et l’évaluation du rendement clinique de la physiothérapie au Canada. Sur une période de six semaines, les étudiants ont collaboré avec des personnes vivant avec le VIH (PVVIH) membres de PLN pour déterminer le rôle des physiothérapeutes à PLN et ont dirigé deux ateliers de promotion de la santé pour les membres et le personnel de PLN. Conséquences : le stage en physiothérapie en MÉ a permis de relever de futures possibilités pour les physiothérapeutes à PLN. L’expérience a également incité un étudiant à postuler, après l’obtention de son diplôme, à un nouveau poste de physiothérapeute auprès de PVVIH.
Mots-clés : interprofessionnel, plan de santá communautaire, rapport de cas, stage, VIH
The majority of people living with HIV (PLWHIV) experience at least one impairment, activity limitation, or participation restriction.1 In addition, PLWHIV experience multiple morbidity: more than 30% of PLWHIV in Ontario report having at least one other chronic health condition.2 Studies have demonstrated that physiotherapy (PT) techniques, including joint and soft tissue mobilization, resistance and aerobic exercise, and self-management strategies, have positive effects on the complex comorbidities associated with HIV, including balance impairment, reduced cardiovascular fitness, and poor mood, as well as neuropathic pain.3–6
Two goals of the Ontario Advisory Committee on HIV/AIDS Strategy to 2026 are to reduce the incidence of HIV in Ontario and ensure that PLWHIV lead long, healthy lives, free from stigma and discrimination.7 In addition, Ontario’s Patients First Act, 2016,8 aims to improve the connections among primary care, hospitals, public health, and home and community care to enhance individual experiences with transitions among health care sectors. Thus, it is important to identify how rehabilitation professionals, including physiotherapists, can facilitate the goals of the Patients First Act for PLWHIV.
Training future physiotherapists and supporting them as they develop knowledge about and experience working with PLWHIV are important to maximize equitable access to rehabilitation services in the future. Role-emerging (RE) clinical placements are placements that give rehabilitation students clinical education opportunities at locations where there is no established rehabilitation programme or identified set of rehabilitation roles and responsibilities.9 These placements challenge rehabilitation students to learn how to develop programmes and contribute to health care in new ways.9 RE placements are well documented in the occupational therapy (OT) literature,9,10 but the concept is not as well established in the PT literature.10
Interprofessional education for health professional students in community-based HIV organizations (CBHIVOs) increases their awareness of other professionals’ roles in the context of a team and their comfort and compassion when discussing sensitive topics related to HIV.11 Solomon and Baptiste noted that an RE placement at a community health centre that serviced PLWHIV challenged a PT and an OT student to discern their distinct and complementary areas of practice and to advocate for their roles with other staff.12
Client Description
Realize is a national, not-for-profit organization whose vision is to help improve the daily lives of PLWHIV in direct and meaningful ways through rehabilitation care, support, and services. Realize has facilitated the placement of more than 30 OT students at CBHIVOs in Canada since 2013,13 but it has not facilitated placements for PT students.13
Developing the placement
In Fall 2015, Realize conducted outreach with various CBHIVOs in Canada to ascertain their interest in working with PT programmes to establish clinical placements. Positive Living Niagara (PLN) responded and worked with McMaster University’s MSc(PT) programme and Realize to establish two part-time RE clinical placements (2 days per week over 6 consecutive weeks) for PT students in 2016.
PLN provides support, education, and advocacy for HIV-positive individuals and their families and friends. It is located in southwestern Ontario. PLN and the students (CW, KR) who completed their placements gave their consent for this case report to be written and key learnings shared through publication. Because of the nature of its content, this case study was exempt from formal ethics review.
A working group, consisting of one representative each from McMaster’s MSc(PT) programme, PLN, and Realize, collaboratively developed a RE placements proposal, including the specific objectives for the pilot placements (described in Box 1). The working group consisted of the project coordinator, access to rehabilitation, at Realize (PA), the executive director of PLN (GW), and the director of clinical education for the MSc(PT) programme at McMaster (SW). Members of PLN are PLWHIV who are supported by PLN services. A member was not included as part of the working group primarily because of logistical constraints. However, the working group acknowledged the importance of hearing from PLN members to understand the diverse PT needs for PLWHIV in this community before developing a specific role for PT in PLN. As a result, we determined that students would meet with PLN members during their placement to help inform and develop an understanding of the diverse PT needs of PLWHIV in this community.
Box 1.
Placement Description and Objectives Posted When the Physiotherapy Students Were Submitting Their Clinical Placement Preferences
| Placement description | Placement objectives |
|---|---|
| In this RE placement, you will be working under the supervision of a registered occupational therapist, the staff of PLN, and a physiotherapist to develop group education sessions, complete some clinical assessments,* and identify future opportunities for physiotherapists in this setting. | The placement at PLN will be 2 days per week for 6 weeks. By the end of the placement, the student(s) will:
|
This objective was removed during the implementation phase (i.e., in the students’ first week at the placement) because of concerns about their limited time and storage of personal health information. Instead, students focused on meeting with PLN members to identify potential future roles for a physiotherapist at PLN.
RE = role emerging; PLN = Positive Living Niagara; PT = physiotherapy; PLWHIV = people living with HIV.
While planning the placements, the working group determined that one desired outcome was to have the students prepare a final report that discussed potential future roles for physiotherapists and PT student placements at PLN. Additional placement objectives were creating individualized PT assessments and follow-up treatments for a few members of PLN to help them achieve their personal health and wellness goals and delivering two educational sessions on topics agreed on with PLN members and staff. Of the goals established during the planning phase by the working group, one was identified during implementation as not being feasible (see “Implementing the placements” section).
Because PLN does not currently employ a physiotherapist or occupational therapist, the working group developed a model of supervision to support the students’ learning and the desired outcomes of the placements. To give students the widest range of opportunities and clinical experiences, the team agreed on a shared, inter-professional model of supervision. This model included primary supervision by an off-site (i.e., not employed by PLN) registered occupational therapist (NR) with experience in community-based rehabilitation. In addition, an off-site, registered physiotherapist (SW) came onsite to supervise member interviews when the occupational therapist was not available. The on-site programs and service manager at PLN was responsible for the site orientation, arranged shadowing opportunities with other PLN staff (i.e., case managers), and was the daily contact for the students to answer questions about the organization.
Because these placements were developed as a pilot project, the working group decided that the PT students would work at PLN 2 days per week (Tuesdays and Thursdays) for 6 consecutive weeks, then work at another clinical site for the remaining 3 days per week. This would then create a full-time placement (5 days per week for 6 weeks). The model of supervision and allocation of placement days discussed during the planning stages was the model actually implemented. Figure 1 depicts a general overview of the collaborative placement process.
Figure 1.
Overview of the collaborative placement process.
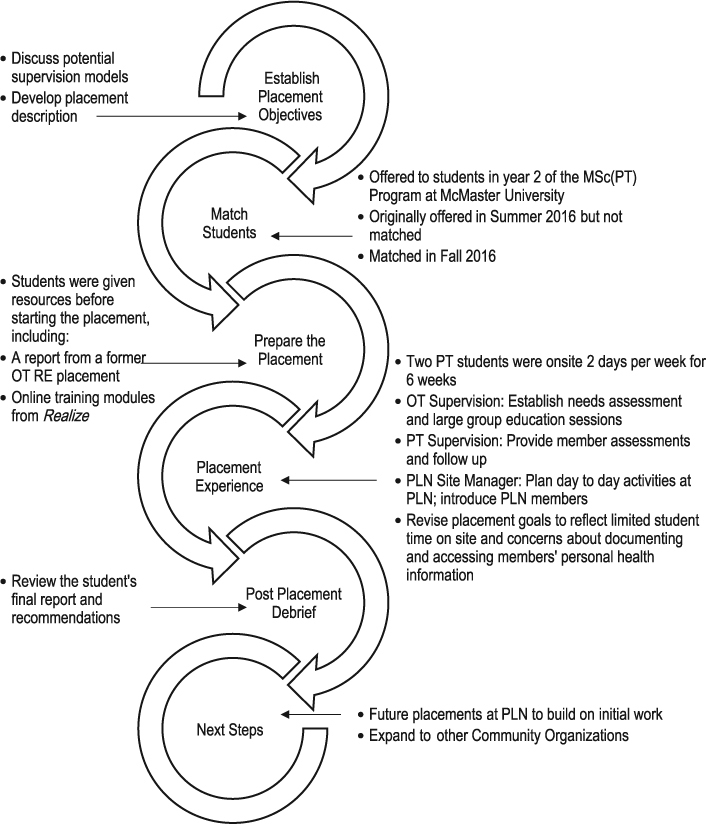
MSc(PT) = Master of Science (Physiotherapy); PT = physiotherapy; OT = occupational therapy; RE = role emerging; PLN = Positive Living Niagara.
Intervention
Matching the placement
The application and matching process for this placement was modified from the non-RE placements in the MSc(PT) programme at McMaster University. Consistent with all placements in the MSc(PT) programme at McMaster, students were required to submit their preferences ranked in order from 1st to 10th choice (student ranking). To be considered for the RE placement, students who were interested were also required to answer a series of questions (expression of interest). This modified application process required students to recognize that this placement would occur in a setting that did not traditionally employ a physiotherapist, involve working with individuals who had complex needs, and involve fewer hours of direct patient care than established PT placements.
The placement was initially offered to all students completing the first year of the MSc(PT) programme at McMaster (Summer 2016). At this initial offering, there were no students who submitted an expression of interest. In consultation with all stakeholders, the placement was offered again in Fall 2016 to all second-year students in the programme. Two second-year PT students ranked the placement highly and clearly articulated their personal goals for participating in this placement: (1) to learn about the health needs of PLWHIV and determine how PT can address these needs and (2) to advocate for the role of PT within CBHIVOs to improve functional performance and quality of life and to prevent future health concerns of PLWHIV.
Implementing the placement
Before starting the placement, the PT students were given background information about HIV; antiretroviral therapies and their side effects; and the associated social, cognitive, and physical conditions experienced by PLWHIV, using online learning modules (Evidence Informed HIV Rehabilitation, Realize), and the Canadian AIDS Treatment Information Exchange website which provides treatment and prevention information on HIV and hepatitis C (https://www.catie.ca/en/home). They were also given the final report from two OT students who had completed a placement at PLN. In addition, the director of clinical education (PT) met with the occupational therapist supervisor to review the evaluation expectations for the placement.
For the duration of the placement, the students shared office space with the home support staff at PLN. This location offered maximum opportunity to interact with PLN members and front-line staff with extensive knowledge of these members. The students could access private office space if needed, as well as PLN’s computer systems. The site manager was also located in the office for ease of communication with the students. PLN operates on an outreach model, so interactions with members take place in their homes and in PLN’s programming areas.
The placement occurred during the first placement of second year, after students had learned basic orthopedic, cardiorespiratory, and neurological PT practice in addition to basic research skills. To facilitate their orientation to PLN, the students met with the site manager on the first day and established further meetings as needed for formal updates. The students also met with different staff members (i.e., home support workers, case managers) during the first 2 days of the placement, and they discussed their proposed learning contracts and the consultative model with the occupational therapist supervisor.
After the first week of the placement, the students and team of supervisors realized that one of the original objectives of the working group – providing a few members with individualized PT assessments and treatments to help them reach their health and wellness goals – needed to be revised. This revision was due to the limited time students were onsite at the placement (only 12 days of placement over the 6 weeks). In addition, unanticipated challenges arose in relation to how the results of the proposed assessments and treatments completed would be stored in accordance with the standards of College of Physiotherapists of Ontario because PLN itself does not provide any direct patient care. Thus, the PLN supervisors, students, and staff decided that the students would meet with interested members to learn about the diverse PT needs of PLWHIV. These discussions would inform the students’ final report, which would discuss the possible long-term roles of a physiotherapist at PLN. The site manager facilitated this goal by approaching members and inquiring whether they would meet with the students and share their personal experiences of living with HIV. If a member or the students identified specific care needs or rehabilitation goals during the meetings, the students and supervisor would ask the member’s permission to refer them to a community service. The students also agreed to develop and deliver two general education sessions on topics that might interest the members.
The interviews gave the students the opportunity to not only explore members’ potential PT needs but also to identify their common needs. The students used these common needs to propose topics for and to develop the two educational sessions. These sessions enabled the students to enhance PLN staff’s knowledge of health promotion from a functional perspective, as well as to improve the members’ self-management skills. All PLN members, home support workers, and case managers received emails advertising session topics and timing.
The students planned their schedule and advised their supervisors when activities requiring profession-specific or direct supervision were needed. In general, the occupational therapist supervisor met with the students weekly to review progress on the final report and attended both educational sessions. The physiotherapist supervisor was onsite with the students 2–3 hours per week and attended the students’ meetings with the members. The students were expected to prepare for the education sessions and write their reports independently.
Measures and Outcomes
Measures
The placements were evaluated using a variety of measures. The students’ performance was measured using the typical evaluation processes at McMaster (i.e., a learning contract and the Canadian Physiotherapy Assessment of Clinical Performance [ACP]); PLN members provided feedback on the educational sessions; and the placement was evaluated by students and working group members (by means of questionnaires for education sessions and site evaluation forms).
Evaluation of the students’ performance
Learning contracts and the ACP were used to evaluate the students’ performance. A learning contract is a mandatory component of evaluating all clinical placements in McMaster’s MSc(PT) programme. Each student submitted a learning contract with two goals that were specific, measurable, attainable, realistic, and time related (SMART; available on request). The SMART goals for the students’ placements were established during the first week in collaboration with their supervisors.
The students were also evaluated using the ACP at mid-term (Week 3) and final evaluation (Week 6). The occupational therapist supervisor obtained feedback from the site manager and off-site physiotherapist and used it to complete each student’s assessments at mid-term and final evaluation. The occupational therapist supervisor also reviewed the ACP and learning contract evaluation with the students at both times. Despite being developed and tested for clinical placements that focus on direct patient care, the ACP was not modified for this RE placement. Instead, the director of clinical education (PT) developed a resource to describe how each section of the ACP could apply to the RE context.
Feedback on educational sessions
PLN members were also requested to complete feedback forms at the end of both educational sessions. These forms asked the participants to rank, out of 5 (0 = low, 5 = high), the helpfulness of the session, effectiveness of the group moderators, and consideration for future attendance. The forms also included space where attendees could add comments about what they liked most and least about the sessions, areas for improvement, and suggestions for future sessions.
Evaluation of the clinical placement by students and working group members
The students submitted a written evaluation of their placement using a standard placement site evaluation form and a written report submitted at the end of the placement. In addition, the students provided members of the working group (SW, NR) verbal feedback at the final evaluation. The perspective of the other working group members (PA, GW) was captured through post-placement discussion with the director of clinical education (PT).
Outcomes
The students successfully completed their learning contracts. Both students met the ACP expectations for students in the third 6-week clinical placement at McMaster. By the end of the 6 weeks, the students had also prepared and presented two educational sessions for PLN members and staff based on topics identified in meetings with members (“Promoting Your Health and Wellness through Physiotherapy and Exercise” and “Chronic Pain”). Both education sessions were well received by the member and staff attendees, with average ratings as follows: helpfulness of the group sessions, 4.7 out of 5; effectiveness of the group moderators, 4.9 out of 5; and consideration for future attendance, 4.9 out of 5. The written feedback noted that, in general, the attendees found the sessions informative and interactive.
Additional activities completed by the students during the placements included the development of a PT screening tool for PLN case managers to use in identifying a member’s need for PT; helping two members navigate access community services for the care or recreational opportunities identified during their interviews; and preparation of a final report that identified the potential future roles for a physiotherapist at PLN. In their final report, the students suggested the following future roles for a physiotherapist at PLN: help members navigate access to community resources, educate case managers about appropriate PT referrals, and develop a process to securely store personal health information for PLN members to subsequently enable future students to perform individualized PT assessments and treatment for members who cannot access PT services elsewhere.
In the following sections, we set out the views on the placement from the perspectives of three partners in the placements.
Perspective of the students
This placement experience afforded us the opportunity to see how physiotherapy services could not only help after injury or illness, but also in preventing functional decline and promoting activity and well-being. Despite understanding the physical implications of HIV/AIDS, we quickly learned the impact of the social determinants of health on well-being and the complexities of the lived experiences of PLWHIV. As the first PT students on placement in a community-based HIV organization, we were able to apply our current knowledge and problem solve through challenging and novel situations as well as lay the foundation for future students, and physiotherapists, to further the work done. This placement provided a meaningful and fulfilling experience, and we are excited to see future physiotherapy placement opportunities in community-based HIV organizations. (CW, KR)
Less than 1 year after graduation from the MSc(PT) programme, one student (CW) credits her experience during this placement with giving her the confidence to successfully apply for a newly created PT position at Casey House, Canada’s first and only stand-alone hospital for people with HIV/AIDS, in Toronto.
Perspectives of the occupational therapist and physiotherapist supervisors
The placement provided students with key insights around access to community-based rehabilitation services. Specifically, the students were challenged to address rehabilitation needs within existing systems and appreciate the context and lived experience of PLWHIV. The students also practised the skills of collaboration, negotiation, and active listening with a variety of partners. Future placements will build on the lessons learned from this experience in order to enhance the integration of student learning goals, with the needs of PLN and the MSc(PT) programme’s placement expectations at McMaster. Future placements can also establish a model of practice and evaluation both with members as individuals and members as organizations within and outside the health sector. (NR, SW)
Perspective of Positive Living Niagara
This experience offered an opportunity for students to understand the impact HIV has not just physically on an individual, but the social, emotional and economic impacts. The placement provided a glance into the complex lives that PLWHIV have and how they struggle to have their rehabilitation needs met. The impacts of stigma, sexual orientation, trauma history and lack of health provider knowledge and support could be seen first-hand. The placement demonstrated the need for physiotherapy within this population of individuals who have been on long-term antiretrovirals and who tend to suffer from early onset of and multiple musculoskeletal issues. For staff and members, it was an opportunity to see what PT could offer to them and how to use PT to improve the quality of life within this unique population. (GW)
Although the students, supervisors, and PLN brought their individual perspectives to the placement, they included some common themes. For example, the supervisors and PLN believed that the placement exposed the students to the barriers to accessing rehabilitation services experienced by PLWHIV. In addition, the students and PLN highlighted how the placement experience facilitated the students’ understanding of how the social determinants of health contributed to the complex lives of PLWHIV and affected their overall health and function.
Implications
Rehabilitation professionals, including physiotherapists, have experience working with individuals who have impairments, activity, and participation restrictions as a result of chronic conditions.14 However, in a national survey of rehabilitation professionals, including Canadian physiotherapists, occupational therapists, speech–language pathologists, and HIV specialists (e.g., physicians, nurses, social workers), only one-third who had served PLWHIV stated that they had received training in working with PLWHIV as part of their professional degree.15 In addition, less than 15% of their rehabilitation professional education was in the form of clinical placements or internships with an HIV focus or shadowing opportunities with health professionals in HIV care.15 Of the rehabilitation professionals who reported that they had served a PLWHIV, approximately 53% rated their profession as “very important” in the rehabilitation of this population.15 Worthington and colleagues suggested that this lack of training may contribute to gaps in service provision by rehabilitation professionals for PLWHIV and that further training opportunities in HIV care might ensure that rehabilitation professionals feel confident in addressing the needs of PLWHIV in the future.15
An interdisciplinary, RE clinical placement at PLN provided a bi-directional training opportunity that enhanced the skills and knowledge of two PT students as well as the other professionals with whom they interacted. The inter-professional nature of the student supervision and the clinical experience enabled the students to not only develop their own skills and knowledge but also understand how essential inter-professional and cross-sectoral teams are to maximizing care for individuals with complex chronic conditions. As a result of staffing changes, this placement has not yet been offered to other cohorts of students. However, each group is committed to working together to offer it in the future.
Despite the fact that this placement was only part time, it gave the students novel learning opportunities and influenced the decision of one student to apply for the newly established position of physiotherapist at Casey House in Toronto less than 12 months after graduation. This outcome reinforces the fact that RE placements not only positively contribute to students’ learning but may also positively influence future roles for the PT profession and models of practice.
Key Messages
What is already known on this topic
Studies have demonstrated that physiotherapy (PT) techniques have positive effects on the complex comorbidities associated with HIV, including balance impairment, reduced cardiovascular fitness and poor mood, and neuropathic pain.3–6 However, a national survey of rehabilitation professionals, including Canadian physiotherapists, occupational therapists, speech–language pathologists, and HIV specialists (e.g., physicians, nurses, social workers), reported that less than 15% of their rehabilitation professional education was in the form of clinical placements or internships with an HIV focus or shadowing opportunities with health professionals in HIV care.15
What this case study adds
We described a collaborative initiative to develop the first PT placements in a community-based HIV organization in Canada for second-year PT students at McMaster University. We offer a framework and considerations that other PT programmes and a community-based HIV organization could build on to establish additional placements.
References
- 1.Rusch M, Nixon S, Schilder A, et al. Impairments, activity limitations and participation restrictions: prevalence and associations among persons living with HIV/AIDS in British Columbia. Health Qual Life Outcomes. 2004;2:46 10.1186/1477-7525-2-46. Medline:15350202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kendall C, Wong J, Taljaard M, et al. A cross-sectional, population-based study measuring comorbidity among people living with HIV in Ontario. BMC Public Health. 2014;14(1):161 10.1186/1471-2458-14-161. Medline:24524286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pullen SD, Chigbo NN, Nwigwe EC, et al. Physiotherapy interventional as a complementary treatment for people living with HIV/AIDS. HIV AIDS (Auckl). 2004;6:99–109. 10.2147/HIV.S62121. Medline:24936132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Brien K, Tynan AM, Nixon S, et al. Effect of progressive resistance exercise in adults living with HIV/AIDS: systematic review and meta-analysis of randomized trials. AIDS Care. 2008;20(6):631–53. 10.1080/09540120701661708. Medline:18576165 [DOI] [PubMed] [Google Scholar]
- 5.O’Brien K, Nixon S, Tynan AM, et al. Aerobic exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst Rev. 2010;(8):CD001796 10.1002/14651858.CD001796.pub3. Medline:20687068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gale J. Physiotherapy intervention in two people with HIV or AIDS-related peripheral neuropathy. Physiother Res Int. 2003;8(4):200–9. Medline:14730724 [DOI] [PubMed] [Google Scholar]
- 7.Ontario Advisory Committee on HIV/AIDS. HIV/AIDS strategy to 2026: focusing our efforts: changing the course of the HIV prevention, engagement and care cascade in Ontario [Internet]. Toronto: Ministry of Health and Long-Term Care; 2017. [cited 2017 Oct 22]. Available from: http://www.health.gov.on.ca/en/pro/programs/hivaids/docs/oach_strategy_2026.pdf. [Google Scholar]
- 8.Toronto Central Local Health Integration Network. The Patients First Act Backgrounder. Toronto: The Network; 2016. [Google Scholar]
- 9.Dunbar SB, Simhoni O, Andersen LT. Classification of fieldwork experiences for the new millennium. Occup Ther Health Care. 2002;16(1):81–7. 10.1080/aJ003vl16n01_06. Medline:23952064 [DOI] [PubMed] [Google Scholar]
- 10.Jung B, Solomon P, Cole B. Developing emerging roles in clinical education In: Solomon P, Bapiste S, editors. Innovations in rehabilitation science: preparing the leaders for the future. Berlin: Springer; 2005. p. 39–58. [Google Scholar]
- 11.Mignano J, Sofolahan-Oladeinde Y, Hossain M, et al. Preparing the future: an interprofessional approach to prepare future health and service-delivery professionals to attain an AIDS-free generation. J Interprof Educ Pract. 2016;4:1–8. 10.1016/j.xjep.2016.04.001. [DOI] [Google Scholar]
- 12.Solomon P, Bapiste S, editors. Innovations in rehabilitation science: preparing the leaders for the future. Berlin: Springer; 2005. [Google Scholar]
- 13.Ahluwalia P. HIV and rehabilitation: evaluation of a community-based initiative and looking to future directions. Poster session presented at: Canadian Association of HIV Research Conference; 2017 April; Montreal. [Google Scholar]
- 14.Canadian Physiotherapy Association. Chronic disease. Ottawa: The Association; 2012. [cited 2017 Oct 23] Available from: https://physiotherapy.ca/sites/default/files/valuePT/cpa_valuept_chronicdisease-en.pdf. [Google Scholar]
- 15.Worthington CA, O’Brien K, Myers T, et al. HIV and rehabilitation training needs of health professionals in Canada: results of a national survey. J Res Interprof Pract Educ. 2014;4(1). 10.22230/jripe.2014v4n1a128. [DOI] [Google Scholar]


