Abstract
We surveyed hospital epidemiologists and infection preventionists on their usage of and satisfaction with infection prevention–specific software supplementing their institution’s electronic medical record. Respondents with supplemental software were more satisfied with their software’s infection prevention and antimicrobial stewardship capabilities than those without. Infection preventionists were more satisfied than hospital epidemiologists.
Electronic medical records (EMR) are often augmented with supplemental infection prevention software (SIPS) that assists with the identification and monitoring of healthcare-associated infections and antibiotic-resistant bacteria, facilitates regulatory reporting and antimicrobial stewardship, and improves workflows.1 Hospital epidemiologists and infection preventionists making purchasing decisions about SIPS have little information available on the quality and effectiveness of these products beyond what is provided by the vendors. Additionally, cost and implementation complexity make trying multiple SIPS in a single facility impractical.
In order to address this lack of information about SIPS, we conducted a survey of hospital epidemiologists and infection preventionists related to their SIPS usage. The primary aims of this study were to (1) provide descriptive information about SIPS usage and (2) to compare the self-reported user satisfaction of hospital epidemiologists and infection preventionists using SIPS with those using EMR alone in terms of infection prevention and antimicrobial stewardship needs. Additionally, we assessed user-reported functionality, cost effectiveness, customizability, and information technology support requirements of SIPS.
METHODS
We surveyed hospital epidemiologists and infection preventionists belonging to 2 professional organizations, the Society for Healthcare Epidemiology of America (SHEA) Research Network2 and the Association for Professionals in Infection Control and Epidemiology (APIC). SHEA Research Network members were contacted directly with a personalized e-mail prompting them to follow a link to complete our survey. Members who did not complete the survey within 12 days were sent a personalized reminder e-mail. APIC members were contacted through an e-mail sent to their listserv. Data were collected between April 3 and April 19, 2013. Web-based survey software SurveyMonkey was used to collect data and send personalized e-mails. Survey responses were anonymized prior to analysis.
Respondents were first asked to identify the EMR and SIPS used by their facility. Respondents indicating that their facility used commercial SIPS were asked to complete a detailed 19-question survey (available as an online supplement) on their satisfaction with and usage of this software as well as questions about its capabilities, cost, implementation process, and customizability. These respondents are referred to as SIPS users. Respondents at facilities without commercial SIPS (ie, had only EMR software) or who had proprietary infection prevention software were asked to complete a 13-question survey on how well their software met infection prevention needs, how they transferred reporting data to the Centers for Disease Control and Prevention/National Healthcare Safety Network, and reasons for not purchasing SIPS. These respondents are referred to as non-SIPS users. Both surveys were developed and pretested by a focus group of 4 hospital epidemiologists/infection preventionists (A.D.H., M.Y.L., D.J.M., and M.-O.W.).
We report overall means, means stratified by SIPS usage and vendor, and respondent profession (hospital epidemiologist or infection preventionist) for survey questions that were scored using 10-point Likert items. Two-tailed Wilcoxon rank-sum tests were used to compare means between groups (SIPS vs non-SIPS or hospital epidemiologists vs infection preventionists). Data were analyzed with SAS 9.2 (SAS Institute).
RESULTS
We received a total of 98 completed responses to our survey, 56 from SHEA (out of 174 members of the SHEA Research Network) and 42 from APIC listserv members (the number of APIC listserv members who received the e-mail could not be determined). Out of all completed responses, 43 were from hospital epidemiologists and 55 from infection preventionists. Twenty-seven percent of respondents used Epic, 18% used Cerner, and 8% used MEDITECH. Thirty-eight percent of respondents used another EMR, and 9% used no EMR. The most commonly used SIPS were MedMined (26% of all respondents), TheraDoc (16%), and SafetySurveillor (14%). Fourteen percent of respondents used other commercial SIPS (including BD AICE by BD [previously by ICPA], BD Protect Infection Prevention by BD, Cerner Infection Control by Cerner, Midas+ Care Management by MidasPlus, QC PathFinder by Vecna Technologies, and VigiLanz by Vigilanz), 13% used proprietary software built at their institution, and 16% used no SIPS.
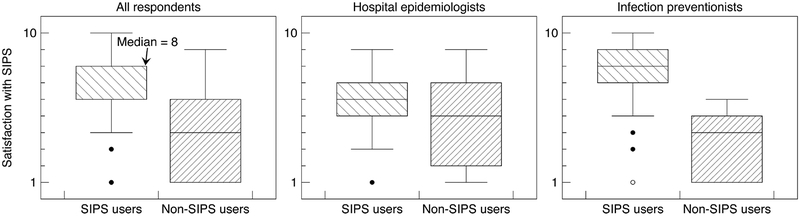
SIPS users reported higher satisfaction with their software’s infection prevention capabilities than non-SIPS users (Figure 1). For the question “What is your level of satisfaction with [your software] in terms of meeting your infection control needs?” responses were higher for SIPS users (mean, 7.0; standard deviation [SD], 2.3) than for non-SIPS users (mean, 4.1; SD, 2.5; P < .001). SIPS users reported a higher likelihood that they would be using the same infection prevention software in 2 years (mean, 7.4; SD, 3.0) than non-SIPS users (mean, 4.5; SD, 2.9; P < .001).
FIGURE 1.
User-reported satisfaction with infection control capabilities of software, as reported by supplemental infection prevention software (SIPS) users and non-SIPS users, for all respondents and stratified by respondent profession (1, low satisfaction; 10, high satisfaction). Whiskers represent the range of the responses with 1.5 interquartile ranges of the median. Circles represent responses outside this range.
There was some variation in the distribution of SIPS usage between hospital epidemiologists and infection preventionists. Specifically, 43% of infection preventionists who completed the survey reporting using MedMined (n = 24) compared with 2% of hospital epidemiologists (n = 1); 15% of infection preventionists (n = 8) and 14% of hospital epidemiologists (n = 6) reported using SafetySurveillor; 11% (n = 6) and 23% (n = 10), respectively, reported using TheraDoc; 20% (n = 11) and 42% (n = 18), respectively, reported using no SIPS or proprietary software; and 11% (n = 6) and 19% (n = 8), respectively, reported using other commercial SIPS.
Among SIPS users, infection preventionists indicated a higher level of satisfaction with their software meeting infection control needs (mean, 7.5; SD, 2.2) than hospital epidemiologists (mean, 5.8; SD, 2.2; P = .003). There was variation in user satisfaction among SIPS, but the low number of respondents in each strata when stratifying both by respondent profession and SIPS prevents comparing user-reported satisfaction among SIPS with hypothesis tests. Mean user-reported satisfaction among infection preventionists was 8.2 (SD, 1.9) for MedMined, 5.9 (SD, 2.7) for SafetySurveillor, 7.2 (SD, 1.8) for TheraDoc, 2.9 (SD, 1.7) for no SIPS or proprietary software, and 4.0 (SD, 2.4) for other commercial SIPS. Mean user-reported satisfaction among hospital epidemiologists was 9.0 (n = 1) for MedMined, 5.0 (SD, 3.0) for SafetySurveillor, 6.0 (SD, 1.2) for TheraDoc, 4.4 (SD, 2.8) for no SIPS or proprietary software, and 5.0 (SD, 2.8) for other commercial SIPS.
Most SIPS users thought that SIPS improved their daily workflow (mean, 7.0; SD, 2.6). Infection preventionists had more positive responses to this question (mean, 7.5; SD, 2.7) than hospital epidemiologists (mean, 6.0; SD, 2.2; P = .02). Among SIPS users, 49% used SIPS for antimicrobial stew-ardship. These respondents were substantially more satisfied with how their software met antimicrobial stewardship needs (mean, 6.5; SD, 2.4) than non-SIPS users were (mean, 2.8; SD, 1.7; P < .001).
SIPS users had a mean response of 7.0 (SD, 2.9) to the question, “Do you feel that [SIPS] was a cost-effective purchase, i.e. could the money be better used for something else in hospital epidemiology?” We did not observe any major differences in responses to this question for different individual SIPS, although small cell sizes made such comparisons difficult to compare. Nearly half of SIPS users did not know the annual cost of their SIPS (n = 25). Of those who did know, 18% (n = 5) reported costs ranging from $0 to $49,999; 32% (n = 9) reported costs ranging from $50,000 to $99,999; 18% (n = 5) reported costs ranging from $100,000 to $149,999; 14% (n = 4) reported costs ranging from $150,000 to $199,999; and 18% (n = 5) reported costs greater than $200,000 annually. No correlation was apparent between cost and user satisfaction.
DISCUSSION
We found that users of SIPS reported greater satisfaction with the infection prevention abilities of their software, indicating that commercial SIPS offered benefits over relying on the infection prevention capabilities of their EMR. SIPS users indicated a higher likelihood of continuing to use the same software 2 years from now than non-SIPS users. Infection preventionists reported greater satisfaction with SIPS than hospital epidemiologists, although this difference may be caused by differences in the distribution of SIPS vendors between these groups. Alternatively, the difference in satisfaction between hospital epidemiologists and infection preventionists may indicate differences in the implementation, daily responsibilities, frequency of use, or usability of SIPS features used by infection preventionists and hospital epidemiologists. It is also possible that hospital epidemiologists are generally less satisfied with software than infection preventionists.
While we report user-reported satisfaction for individual SIPS vendors, we urge caution in the interpretation of these data. Because of the small number of respondents for each vendor and limitations in this study design discussed below, it would be irresponsible to use these data to make comparisons between individual SIPS.
Like any voluntary survey, our study is limited by possible nonresponse bias. Additionally, the source population (SHEA and APIC members) may not be representative of all infection prevention software users, limiting generalizability of our findings. We also were not able to collect information detailing differences within individual SIPS or EMR products (eg, the presence of optional modules). Finally, we use survey responses as a proxy for performance and value of SIPS. Thus, these data may imperfectly represent the true utility of SIPS.
In conclusion, commercial infection prevention software used in addition to EMR was well liked by end users, with greater appreciation from infection preventionists than hospital epidemiologists. Further research is needed on the usage and effectiveness of SIPS.
Supplementary Material
ACKNOWLEDGMENTS
We would like to acknowledge the infection preventionists and Society for Healthcare Epidemiology of America Research Network members who responded to the survey.
Financial support. Support for D.J.M. was provided by K08 HS18111-01 AHRQ. Support for A.D.H. was provided by K24 5K24A1079040-02 NIH.
Footnotes
Potential conflicts of interest. M.-O.W. reports that he is a member of the advisory board for IC Net Systems (a paid position) and is a member of Epic’s Brain Trust for IC development (an unpaid position). All other authors report no conflicts of interest relevant to this article. All authors submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and the conflicts that the editors consider relevant to this article are disclosed here.
REFERENCES
- 1.Perl TM, Pottinger JM, Herwaldt LA. Chapter 6: basics of surveillance: an overview In: Lautenbach E, Woeltje K, eds. Practical Handbook for Healthcare Epidemiologists. 2nd ed Thorofare, NJ: Slack, 2004. [Google Scholar]
- 2.Lautenbach E Expanding the research agenda for infection prevention: the SHEA Research Consortium In: Society for Health-care Epidemiology of America Annual Scientific Meeting. Dallas: Society for Healthcare Epidemiology of America, April 1–4, 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.