Abstract
Objective:
Globally, indoor and outdoor pollutants are leading risk factors for death and reduced quality of life. Few theories explicitly address environmental health within the nursing discipline with a focus on harmful environmental exposures. The objective here is to expand the National Institutes of Health Symptom Science Model to include the environmental health concepts of environmental endotype (causative pathway) and environmental exposure.
Design:
Meleis’ research to theory strategy for theory refinement was used. Research workshop proceedings, environmental health nursing research expert consensus, panelist research trajectories, and review of the literature were utilized as data sources.
Results:
Ongoing emphasis on the physical environment as a key determinant of health and theoretical perspectives for including environmental exposures and endotypes in symptom science are presented. Definitions of these concepts, further developed, are provided. Recommendations to strengthen environmental health nursing research and practice through capacity building/infrastructure, methods/outcomes, translational/clinical research, and basic/mechanistic research are included.
Conclusion:
The revised model deepens theoretical support for clinical actions that include environmental modification, environmental health education, and exposure reduction. This modification will enable a middle-range theory and shared mental model to inspire the prioritization of environmental health in nursing leadership, research, practice, and education.
Keywords: Environmental Health Science, exposure, endotype, Symptom Science Model, environmental justice, nursing theory
Globally, indoor and outdoor pollutants are leading risk factors for death and reduced quality of life for a broad range of common diseases, including asthma, chronic obstructive lung disease (COPD), and cardiovascular events (Lim et al., 2012). In the United States, the Healthy People 2020 initiative includes the physical environment as a key social factor and a determinant of health (U.S. Office of Disease Prevention and Health Promotion, 2018). These physical factors that influence health include occupational hazards, climate change, natural and technological disasters, the built environment, and hazardous substance exposure in the air, water, soil, and food. The built environment includes “all of the physical parts of where we live and work”, such as housing, streets, building, transportations, parks, and infrastructure (CDC, 2011). While addressing the physical determinants of health across many sectors and disciplines, the historical foundation (and meta-paradigm) of the nursing discipline is based on the concepts of person, environment, health, and nursing. Furthermore, one of the four major contemporary nursing science priorities is determinants of health, which includes the physical and built environment (Eckardt et al., 2017). Environmental exposure as a substantial public health concern necessitates advancements in disciplinary theory, research, practice, education, and policy to address environmental determinants of health in nursing.
Several interdisciplinary theories inform environmental health nursing. Exemplars include Allostatic Load, Exposome, and Translational Research Framework for Environmental Health (McEwen, 1998; Pettibone et al., 2018; Wild, 2012). Allostatic Load, or the cumulative stress and biological response associated with maintaining homeostasis, provides a framework to integrate social stressors with environmental exposure variables in research (McEwen, 1998). Exposomic theory, informing the cumulative measurement of human environment exposures from conception, also resonates with the holistic and lifespan nature of environmental health nursing (Wild, 2012). Pettibone and colleagues (2018) describe a framework to translate research processes that is applicable to environmental health nursing research. Environment has also been included as a major concept in several nursing theories, such as the environment in the Florence Nightingale Theory of Nursing, Martha E. Rogers’s Science of Unitary Human Beings, Dorothy Johnson’s Behavioral System Model, and Betty Newman’s System Model (Smith & Parker, 2015). Although these theories discuss the effect of environment on symptom development and outcomes, they do not explain the essential nature of the concept of exposure (Thompson & Schwartz Barcott, 2017).
The NIH/NINR Symptom Science Model (NIH-SSM) guides intramural NIH/NINR program and much of biobehavioral nursing science (Cashion & Grady, 2015). Briefly, the NIH-SSM begins with a recognition of a complex symptom or cluster of symptoms, which can be further classified based on phenotype using biological and clinical data, and delineated by –’omics’ methods, which clarify targets for nursing intervention. Using Meleis’ (2012) criteria, strengths of the SSM model include contagiousness in the nursing discipline, clarity, consistency, elegant simplicity, logical coherence, useful diagram depiction, and applicability for nursing interventions in clinical practice. Symptom resolution is the key outcome of interest in nursing and is nested within three domains of nursing science including public health nursing: person, environment, and health/illness (Bender, Jason, Franck, & Lee, 2018). Symptoms are the main research, clinical, and policy concerns because they are the main reason people seek healthcare (Rutledge & McGuire, 2004). Further, symptoms are the main tenets of several nursing theories, such as Symptom Management Theory, Theory of Self-Efficacy, and Theory of Unpleasant Symptoms (Bender et al., 2018; Lenz & Pugh, 2018; Resnick, 2018). Symptoms have been clearly connected to the concept of environment or community.
In a series of environmental health nursing research workgroup meetings and workshops, a need and opportunity was identified to expand the scope of the NIH-SSM to enhance the model’s applicability by including environmental exposures. The revised model has implications for public health nursing research and practice, as well as the social significance to environmental determinants of health, the inclusion of causal network pathways, and the utility to nurses engaged in environmental policy interventions. The purpose here is to advance the National Institutes of Health Symptom Science Model to include environmental health. This theory revision includes the addition of environmental exposures and environmental endotype concepts to the model, which are defined and described in detail the results section. Environmental exposure in nursing has been defined in a previous concept analysis, and integrated with the NIH-SSM here (Thompson & Schwartz Barcott, 2017). The concept of environmental endotype is an existing concept in interdisciplinary work, and is further developed and integrated for nursing here (Carr, Zeki, & Kraft, 2017).
Methods
To advance the development of nurse scientists within environmental health research, the Alliance of Nurses for Healthy Environments (ANHE) Research Work Group created a workshop for regional and national conferences. ANHE is an affiliation of nurses working in environmental health, with the mission of promoting healthy people and healthy environments by educating and leading the nursing profession, advancing research, incorporating evidence-based practice, and influencing policy. The focus of this Research Work Group is to frame and support an agenda for enabling nurses to solve environmental challenges through the creation of new knowledge. The Research Work Group was created in 2008, at the same time as the formation of the Alliance of Nurses for Healthy Environments. The Research Work Group currently includes over 60 interdisciplinary affiliates. We meet monthly by webinar and electronic communication. The authorship team here began collaborating in detail on workshop planning, implementation, and dissemination since summer of 2018.
The Research Work Group members used Meleis’ (2012) research to theory strategy for theory refinement. Methods to develop the theory integrated monthly meeting proceedings and research workshops to refine the key concepts of symptom science, environmental endotypes and environmental exposures. Furthermore, the focus of these proceedings included detection of exposures, vulnerable global populations and environmental justice. We utilized environmental health nursing research expert consensus internal and external to the work group, panelist research trajectories and NINR priorities related to environmental exposure, environmental endotype, health, symptom science, and biomarker discovery.
Results
The revised NIH-SSM for Environmental Health, depicted in Figure 1, is a middle range theory and shared mental model for environmental health nursing leadership, research, practice, and education. This model adds two main concepts, environmental exposure and environmental endotype, to the NIH-SSM, which emphasizes the important effect that non-infectious exposures have on pathobiological processes and resulting symptoms. These two concepts, environmental exposure and environmental endotype, are discussed in detail below. Details about the components of the original NIH-SSM can be found in the article by Cashion & Grady (2015), are included in with the asthma example in the discussion section of this paper.
Figure 1 :
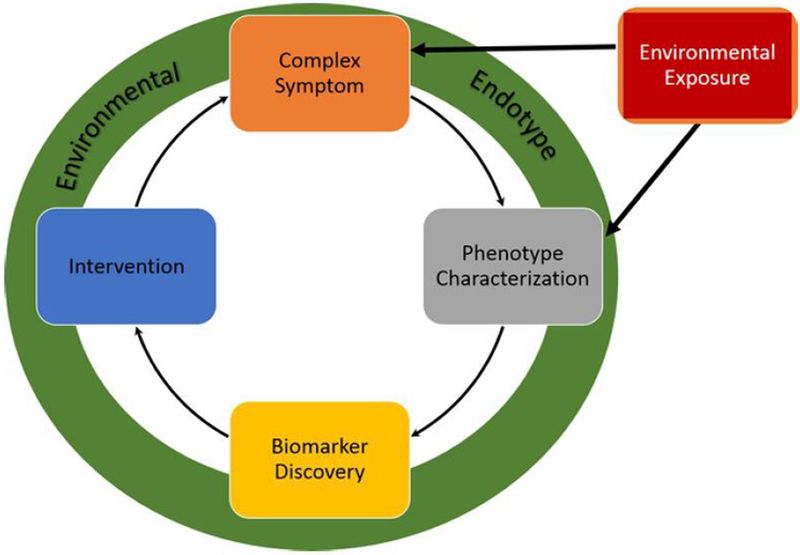
Symptom Science Model for Environmental Health
Environmental Exposure
The concept of exposure for nursing science includes three necessary attributes: first, there must be physical contact between the person and one or more agents in the same environment. Second, the agent has the potential to enter the body through one or more routes. Finally, the agent crosses a barrier or boundary to enter the body (Thompson & Schwartz Barcott, 2017). For the purposes of this NIH-SSM theory modification, environmental exposures are defined as non-infectious agents. While not all exposures cause symptoms or disease, environmental exposures are key contributors to symptom presentation and phenotype characterization in many conditions. Examples of environmental exposures associated with symptoms and disease include allergens, indoor chemical irritants, radiation, cigarette smoking exposure, outdoor dust and ambient pollutants. A specific example of the external exposure process would be fine particulate matter (<PM2.5) at high concentration in an area with high traffic and vehicle emissions above the regulatory standard. This exposure can be internalized via inhalation (the main route of exposure to PM2.5), where PM2.5 can then enter the upper airway passages and reach lower airway passages where it is deposited in lungs. These harmful environmental exposures can be reduced and mitigated to improve health outcomes through public health nursing interventions.
Environmental Endotype
Endotype is the pathobiological mechanism, or theorized causative pathway, of the symptom or disease (Bonnelykke & Ober, 2016). Environmental endotypes are causative pathways by which non-infectious environmental exposures cause and/or exacerbate disease phenotypes and symptom clusters (Carr, Zeki, & Kraft, 2017). While the concept of environmental endotype is most commonly used in precision studies of allergy and asthma, our innovative approach is to broaden the concept’s application to any symptom or disease attributed to environmental toxin causation. Nurses are generally familiar with the concept of environmental endotype, as we propose its novel use, in common poisonings. For example, in carbon monoxide poisoning, where carbon monoxide, the exposure, enters the body by inhalation and displaces oxygen from the hemoglobin in the blood causing diminished oxygenation, resulting in symptoms of somnolence, diminished awareness, and headache (Rose et al., 2017). We identify this causative pathway as one environmental endotype. The proposed SSM for Environmental Health includes this concept as the underlying pathway of focus.
Measuring Environmental Exposure
There are many different methods of measuring environmental exposure. These include outdoor, area, personal, and internal biomarker measurements. There are 187 hazardous air pollutants known to have detrimental health effects that are routinely monitored and controlled by the United States Environmental Protection Agency (EPA) (Strum & Scheffe, 2016). Of these, the six criteria air pollutants (particulate matter (PM), nitrogen dioxide (NO2), sulfur dioxide (SO2), carbon monoxide (CO), ozone (O3) and lead (Pb)) are continuously monitored across the United States and globally (EPA, 2018a). Common outdoor pollution sources include mobile sources, such as automobiles and trucks, industrial emissions, agricultural activity, and natural disasters, such as volcanic eruptions and forest fires (EPA, 2018a). Household combustion sources, such as wood stoves used for cooking and heating, also contribute to poor air quality (Institute of Medicine, 2011; World Health Organization [WHO], 2010). Natural biological sources include pollens and dust (EPA, 2018a). Most often, fixed government monitors are used for ambient monitoring, although outdoor household or specific building monitors may also be used (Szyszkowicz, Kousha, Castner, & Dales, 2018).
Indoor air quality area monitoring measures the levels of exposure in a household, school, workplace, or other building (Centers for Disease Control and Prevention [CDC], 2008). Area monitoring can be measured using subjective and objective methods. Subjectively, questionnaires can be used to recall potential specific exposures. Objectively, air sampling monitors may be placed in the home, school, and/or workplace.
Personal exposure monitoring can range from subjective responses to questionnaires to objective measures where external sensors are worn by people. The link between area concentrations of a given pollutant and body burden and the total amount of a particular chemical present in a human’s body, depend on personal susceptibility and behavior, but also on time-activity patterns of the individual (Shin, McKone, Sohn, & Bennett, 2014; Thompson & Schwartz Barcott, 2017). Thus, the extent to which area monitoring measures individual exposure depends on the route of entry, amount of time and type of activity performed in the area, diffusion of the exposure across the area (e.g. differences among floor, breathing zone, and ceiling level), seasonality, proximity of the monitor to exposure sources, and proximity to the individual in the area.
Biomarkers provide important estimates of internal dose of a specific pollutant. Matrices to collect biomarker samples include blood, urine, breastmilk, expelled air, nails, and saliva, among others (WHO, 2011). Selection of a matrix for biomarker assessment of environmental exposure requires that a researcher have an in depth understanding of how the chemical of interest is absorbed, metabolized, stored, and/or excreted. In addition, the age of research participants and their growth and development are a crucial point to consider when selecting a matrix for the biomarker of exposure (Rodriguez et al., 2016).
Measuring Environmental Endotype
Environmental endotype is quantified as a subtype of symptom clusters and diseases attributable to environmental exposures that are a known human health hazard. For example, an observed asthma exacerbation after cigarette smoke exposure can be detected with a quantifiable change in the innate immune response to the cigarette smoke. A potentially complex network of functions and pathways, the central causal mechanism that links exposure to symptom or disease response is most often oxidative stress, nitrosative stress, direct cellular damage, alterations in acid-base balance, or immune-mediated inflammatory responses (Carr et al., 2017). Genetic and personal vulnerability are additional internal attributes to the environmental endotype. Common examples of molecular mechanism measurements include DNA methylation, gene expression profiling, and allergen-specific immune response (IgE).
Ideally, quantifying environmental endotype involves the longitudinal response to environmental exposures (considering the magnitude, duration, and route of exposure) through the repeated measurement of subjective symptoms, objective physiology, and molecular profile changes (Agache & Akdis, 2019). Utility, sensitivity, and specificity of many measures are emergent as novel areas of scientific inquiry. To date, measures of environmental endotype have largely been quantified as clusters of measures in exploratory, inductive bioinformatics and machine learning approaches that classify and segregate subtypes of asthma and allergy based on common environmental triggers with linked (and often non-specific) physiologic and biomarker measures.
Environmental endotype is a patient-centered, precision health concept that mirrors and complements the toxin-focused concept of toxicodynamics (mechanism of action of toxicant’s adverse effects on biological target tissue and function). For example, rather than quantifying lead’s toxic effect on cognitive ability, the environmental endotype measure quantifies the individual cognitive decline relative to lead exposure in the context of all of the systems biology influences on cognitive ability.
Simple measurements of environmental endotype that are often used in nursing include patient diaries with self-report of environmental exposures documented temporally with symptoms such as migraine headache, autoimmune disease exacerbation, and chronic lung disease exacerbation (Ananthakrishnan, et al., 2018; Fraga, et al., 2013; Mimiya et al., 2017). The predictive utility, sensitivity and specificity of these diary-type patient reported outcome measures can also vary widely, and provide a promising area for future environmental health research, particularly in research augmented with phenotype and biomarker measurement.
Discussion
Our proposed revision to the NIH-SSM, which is called the SSM for Environmental Health, adds the important concepts of environmental exposure and environmental endotype to the model. This revision enables a shared mental model for nursing science that promises to inform precision prevention and environmental modification interventions (Castner, Gehrke, Shapiro, & Dannemiller, 2018; Castner, Gittere, & Seo, 2015). Enhancing the scope of the NIH-SSM with environmental health is coherent with the underlying values of the nursing discipline, allows for social significance to environmental determinants of health research, includes causal pathway conceptualization, and enhances utility to nurses engaged in policy interventions.
Asthma Example of NIH-SSM for Environmental Health
Table 1 includes the NIH-SSM concepts applied to environmental health nursing using asthma as an example. The existing NIH-SSM model begins with complex symptoms, a unique focus to the scientific and practice work of nursing (Cashion & Grady, 2015). Symptoms are often the key factors that drive patients to seek care, identify the status of their condition for self-care considerations, and inform clinician judgement and therapeutic decisions (Bime et al., 2012). The next NIH-SSM concept is phenotype identification. Phenotype includes all of the observable characteristics of the person (Cashion & Grady, 2015). This includes demographic, clinical, and physiologic measures. While asthma was traditionally viewed as one disease, subdivided into allergic and non-allergic, or adult and child onset, more recent evidence clarifies that asthma is a heterogeneous disease with multiple phenotypes (Wenzel, 2012). Clinical diagnoses may be included as well. Each of these phenotypes is linked to a unique biomarker or immune-modulated molecular signature, providing promising opportunities for precision prevention along with novel diagnostic, therapeutic, and clinical intervention targets (Wenzel, 2012). As this biomarker discovery leads to advances in medication therapies, such as the biologic treatment targeting specific immune processes in specific severe asthma phenotypes, the opportunity to advance precision prevention and risk reduction provide unique prospects that are key to nursing science and practice (Carr et al., 2017). Resulting clinical interventions can then be formulated and tested. In asthma, there are multiple environmental exposures that increase the risk of disease development and exacerbation, such as diesel fuel exhaust, mold, pollens, or dust. An environmental endotype is the process by which diesel exhaust exposure upregulates Th17 activity, with neutrophil recruitment and auto-inflammatory responses, triggering worsened shortness of breath, chest tightness, and wheeze symptom clusters (Brandt, et al., 2013).
Table 1.
NIH-SSM for Environmental Health Concepts Applied to Asthma
| Complex Symptoms | Phenotype Characterization | Biomarker Discovery | Intervention (Clinical Application) | Environmental Exposure | Environmental Endotype |
|---|---|---|---|---|---|
| • Wheeze • Dyspnea • Cough • Phlegm • Chest discomfort • Night-time symptom wakening • Activity limitation |
• Age of onset • Obesity • Atopy • Pulmonary function |
•
15‑F2t‑IsoP • IL-17A • IgE • FeNO • Cytokine/ Chemokine levels • Microbiome characterization • Endogenous and exogenous metabolites |
• Air filtration &
ventilation • Trigger reduction strategies • Policy change • Improved household ventilation • Workplace personal protective equipment use |
•
Pollens • Molds • Cigarette smoke • Air pollution • Wood or coal burning smoke, • Dust |
•
Innate Immune Pathway • Acquired Immune Pathway • Oxidative Stress • Nitrosative Stress • Acid-Base Alterations • Direct Cellular Damage • Metabolic pathway |
Note: Greyscale shading in columns with concepts Environmental Exposure and Environmental Endotype, depict the novel additions to the Symptom Science Model.
Coherence with Nursing Discipline Values
The value of environmental justice (EJ) underlies the SSM for Environmental Health. EJ is coherent with the ethical underpinnings of the nursing discipline and motivates nursing research (American Nurses Association, 2015). EJ is defined as “the fair treatment and meaningful involvement of all people regardless of race, color, national origin, or income, with respect to the development, implementation, and enforcement of environmental laws, regulations, and policies” (EPA, 2018b). Nurses have played an important role in developing EJ body of knowledge and linking it to health disparities (Adams et al., 2018; Amiri & Zhao, 2019a, 2019b; Flaskerud et al., 2002; Lee et al., 2015). EJ research aims to identify the relationship between the disproportionate burden of environmental risks associated with those under-represented in decision-making, racially diverse, marginalized, and disadvantaged populations. Populations that are disproportionally exposed to environmental hazards are more likely to experience health disparities and have more health problems. In the United States, poor and minority neighborhoods are disproportionately burdened with hazardous environmental exposures that impact health (Kravitz-Wirtz, Crowder, Hajat, & Sass, 2016). Racial disparities in particular have been noted across the socioeconomic strata. For example, African Americans are more likely than Caucasians to be exposed to higher levels of air pollution (Kravitz-Wirtz et al., 2016), run off from hazardous waste facilities, and higher levels of toxicants including phenols and polychlorinated biphenyl (Mortensen et al., 2014; Sicotte & Swanson, 2007).
The framework supports nursing’s focus on vulnerable populations. Across the lifespan, children and older adults are frequently identified as more vulnerable due to unique anatomical, physiological, immunological, and psychological characteristics, which result in alterations in toxicokinetic (how the body absorbs, distributes, biotransforms, and excretes the chemical) or toxicodynamic (the molecular, biochemical, and physiological effects of chemicals or their metabolites to the body) processes (Links, Schwartz, Simon, Bandeen-Roche, & Stewart, 2001; Simoni et al., 2015). Environmental exposures during early life can affect the risk of developing acute diseases, such as pneumonia, or chronic diseases, such as diabetes and asthma, at any point across the life span (Landrigan et al., 2016). In older adults, exposure to air pollution has been associated with increased rates of chronic obstructive pulmonary disease, chronic bronchitis, asthma, and emphysema, mortality, and hospital admissions/emergency-department visits (Polivka et al., 2018; Simoni et al., 2015). In addition, chronic exposure to air pollutants, such as particulate matter and heavy metals, has been linked to hypertension, stroke, Parkinson’s disease, Alzheimer’s disease, and cancers (Pope, Ezzati, & Dockery, 2009; Thurston et al., 2013). Depending on the environmental exposure, vulnerable groups also include pregnant women and those with occupational risk (e.g. factory or farmworkers) (Hoppin et al., 2012; Talaska, Thoroman, Schuman, & Kafferlein, 2014). Workplace condition may generate human exposure to chemicals (e.g., asbestos, formaldehyde, or lead), physical (e.g., noise or radiation), and biological agents (e.g., Ebola virus) over a period of time, which can affect normal physiological mechanism and impair health of the workers (Ministry of Labor, 2019). Further, exposure to environmental chemicals such as PM, lead, phthalate, and formaldehdye are linked to cognitive deficits and pregnancy outcomes through different mechanisms such as genotoxicity, oxidative stress, disruption of the protein, enzyme and hormonal activity, and DNA methylation (Duong, Steinmaus, McHale, Vaughan, & Zhang, 2011).
Policy
The revised SSM for Environmental Health includes policy interventions, in addition to clinical interventions. Environmental health nursing research has important policy implications (Behague, Tawiah, Rosato, Some, & Morrison, 2009). The evaluations of a variety of environmental pollutants’ impact on human health provide the bases for policy decision and policy change (Behague et al., 2009). Interdisciplinary work among public health professionals, nurses, and policy scholars could significantly improve evaluations of public health outcomes related to environmental risks, provide recommendations of preventative measurements to protect different populations and suggest environmental improvements to the population’s living, working, and recreational environment. In practice, open source informatics tools and databases that public health scholars use to establish the state of the science of environmental exposures could be integrated with existing EJ research to offer more comprehensive evaluation tools for policy makers.
Implications for Leadership, Research, Practice, and Education
The revised SSM for Environmental Health coalesces several implications and recommended areas for ongoing leadership in environmental health nursing research. Additional recommendations for priorities in environmental health nursing are listed in Table 2. Nursing has a rich history in environmental health research (Polivka & Chaudry, 2018), yet there remains an ongoing need to address analytic methods that account for different levels of analysis, including genomics, in exposure measurements and health outcomes in nursing research (Khoury et al., 2012; Lynch & Rebbeck, 2013). Nurses are trained as complex systems thinkers and problem-solvers. “Holistic” is a central concept to the nursing discipline, and holistic practice and research is coherent with the idea that multiple contextual levels of analyses and environmental factors impact health status (Eckardt et al, 2017; Khoury et al., 2012). Further, nursing practice dictates a necessary focus on patient symptom management (Bender et al., 2018; Schmid-Mohler, Caress, Spirig, & Yorke, 2019). The lived environment and exposures significantly contribute to symptoms as already discussed and understanding the environmental endotype of a given exposure provides the nurse substantial insight into symptom etiology impacting nursing management choices.
Table 2.
Future Environmental Health Nursing Priorities
| Topic | Recommendations |
|---|---|
| Capacity building & infrastructure | • Develop graduate minor, cognate,
certificate, or specialization in environmental health
nursing • Enhance the integration of environmental health into BSN, MSN essentials with corresponding education curricular development & certification • Support interdisciplinary, interprofessional education in environmental health • Increase funding for post-doctoral opportunities to integrate environmental exposure assessment in nursing research • Increase support and focus on environmental endotype research (causal pathways & interventions) • Structure additional training opportunities for biomarker & –omic research, including environmental exposure |
| Methods & outcomes | • Enhance utilization of multi-level
research designs & analysis • Validate subjective assessments (e.g. using questionnaires) with objective measures (e.g. exposures using personal monitoring) • Leverage existing datasets & data science opportunities to integrate the nursing perspective with environmental endotypes • Enhance design to address causation vs. correlation (consider Bradford Hill Criteria for observational study) |
| Translational & clinical research | • Intervene through environmental
modification to increase well-being, prevent & self-manage symptoms
and disease • Develop and implement best practices for biomarker report-back processes • Empower patients by providing them with environmental exposure data and tools, including report-back of research measures • Strengthen community-based and community-relevant environmental health research projects |
| Basic & Mechanistic Research | • Explore gene-environment interactions
in symptom science • Characterize environmental endotypes in symptom & disease development and exacerbation |
Because common exposure measurements can vary from outdoor ambient exposure to internal dose, statistical and computational advances in nursing research, such as multi-level modeling, will enable the future mathematical representation and testing the SSM for Environmental Health. Informatics and advanced analysis methods allow for complex conceptual and graphical diagrams of networks, functions, and pathways as concepts, such as those in the Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway system (Kanehisa Laboratories, 2018). Frequently in nursing theory, concepts are linked by propositions amenable to group differences or linear regression testing. In the SSM for Environmental Health, the environmental endotype is added as a novel feature to depict the causal network, function and pathway as a concept. Environmental exposure morbidity, mortality, and quality of life endotypes involve a complex interplay of causative factors at multiple levels of analysis (ambient, area, personal, and within-person) over time (Khoury et al., 2012; Lynch & Rebbeck, 2013). Ongoing training in systems theory and relevant quantitative applications are essential to advancing science in this domain. Implementation of the revised SSM model in public health nursing education with a focus on developing and evaluating novel interventions in the communities, especially EJ communities and vulnerable populations, can lead to novel, valuable, and personalized exposure mitigation practices, models, and policy changes.
Conclusion
The authors of this manuscript propose a revision of the NIH-SSM to include environmental exposure and environmental endotype. This revision will serve to strengthen nursing environmental research, practice, and education through the inclusion of factors that significantly impact symptom presentation and management. Future directions should include continued refinement of the model and expansion into emerging areas such as management of symptoms associated directly and indirectly with climate change (George, Bruzzese, & Matura, 2017).
Clinical Resources.
Alliance of Nurses for Healthy Environments: https://envirn.org/
WHO, Public Health, Environmental and Social Determinants of Health: http://www.who.int/phe/en/
National Institute for Environmental Health Sciences Brochures and Fact Sheets: https://www.niehs.nih.gov/health/materials/index.cfm
Agency for Toxic Substances and Disease Registry Patient Education and Care Instruction Sheets: https://www.atsdr.cdc.gov/emes/health_professionals/instruction_sheets.html
Acknowledgments:
The authors gratefully acknowledge Katie Huffling, Cara Cook, and the staff and conference organizers for Southern Nursing Research Society and Council for the Advancement of Nursing Science.
Funding: This work was supported, in part, by the Alliance of Nurses for Healthy Environments and committed support from the Environmental Health Study of [for] Western New York (also documented as The Tonawanda Health Study: An Epidemiologic Study of Health Effects and Coke Oven Emissions from Tonawanda Coke) through the US District Court for Western New York.
Dr. Rodriguez would like to acknowledge current funding from the National Institute of Environmental Health Sciences/Environmental Protection Agency (P50ES026071), the National Institute of Minority Health and Health Disparities (R01MD009746), and The HERCULES Exposome Research Center (P30 ES019776) and Center for Childrens Health, the Environment, the Microbiome and Metabolomics (CCHEM2; P50ES026071) pilot grant programs during completion of this manuscript.
Dr. Polivka would like to acknowledge funding from the National Institutes of Health, National Institute on Aging (R01AG047297).
JC acknowledges committed support from the University at Buffalo through NIH (#1UL1TR001412), committed salary support from the University at Buffalo School of Nursing, and committed support from the Environmental Health Study of [for] Western New York (also documented as The Tonawanda Health Study: An Epidemiologic Study of Health Effects and Coke Oven Emissions from Tonawanda Coke) through the US District Court for Western New York. Dr. Castner is President of Castner Incorporated with additional funding/consulting disclosures which are unlikely to be perceived as a conflict of interest available on request.
Footnotes
Conflict of Interest: The remaining authors declare no conflicts of interest.
Contributor Information
Jessica Castner, Castner Incorporated, Grand Island, New York.
Azita Amiri, The University of Alabama in Huntsville, College of Nursing, Huntsville, Alabama.
Jeannie Rodriguez, Emory University, Nell Hodgson Woodruff School of Nursing, Atlanta, Georgia.
Luz Huntington-Moskos, University of Louisville, School of Nursing, Louisville, Kentucky.
Lisa M. Thompson, Emory University, Nell Hodgson Woodruff School of Nursing, Atlanta, Georgia.
Shuang Zhao, The University of Alabama in Huntsville, Political Science and Atmospheric Science Departments, Huntsville, Alabama.
Barbara Polivka, University of Kansas Medical Center, School of Nursing, Kansas City, Kansas.
References
- Adams RJ, Ellis C, Magwood G, Kindy MS, Bonilha L, & Lackland DT. (2018). Addressing racial disparities in stroke: The wide spectrum investigation of stroke outcome disparities on multiple levels (WISSDOM). Ethn Dis, 28(1), 61–68. doi: 10.18865/ed.28.1.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. Silver Springs, MD: Author. [Google Scholar]
- Amiri A, & Zhao S. (2019a). Environmental justice screening tools: Implications for nursing. Public Health Nurs doi: 10.1111/phn.12593 [DOI] [PubMed]
- Amiri A, & Zhao S. (2019b). Working with an environmental justice community: Nurse observation, assessment, and intervention. Nurs Forum doi: 10.1111/nuf.12327 [DOI] [PubMed]
- Ananthakrishnan AN, Bernstein CN, Iliopoulos D, Macpherson A, Neurath MF, Ali RAR, … & Fiocchi C. (2018). Environmental triggers in IBD: a review of progress and evidence. Nature reviews Gastroenterology & hepatology, 15(1), 39. doi: 10.1038/nrgastro.2017.136 [DOI] [PubMed] [Google Scholar]
- Behague D, Tawiah C, Rosato M, Some T, & Morrison J. (2009). Evidence-based policy-making: the implications of globally-applicable research for context-specific problem-solving in developing countries. Social Science & Medicine, 69(10), 1539–1546. doi: 10.1016/j.socscimed.2009.08.006 [DOI] [PubMed] [Google Scholar]
- Bender M, Jason S, Franck L, & Lee KA. (2018). Theory of symptom management In Smith MJ & Iiehr PR. (Eds.), Middle Range Theory of Nursing (4th ed.). New York, NY: Springer Publishing Company. [Google Scholar]
- Bime C, Wei CY, Holbrook JT, Sockrider MM, Revicki DA, & Wise RA. (2012). Asthma symptom utility index: Reliability, validity, responsiveness, and the minimal important difference in adult asthmatic patients. Journal of Allergy and Clinical Immunology, 130(5), 1078–1084. doi: 10.1016/j.jaci.2012.07.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnelykke K, & Ober C. (2016). Leveraging gene-environment interactions and endotypes for asthma gene discovery. Journal of Allergy and Clinical Immunology, 137(3), 667–679. doi: 10.1016/j.jaci.2016.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt E, Kovacic M, Lee G, Gibson A, Acciani T, Le Cras T, Ryan P, Budelsky A, & Khurana Hershey G. (2013). Diesel exhaust particle induction of IL-17A contributes to severe asthma. Journal of Clinical Immunology, 132(5), 1194–1204. doi: 10.1016/j.jaci.2013.06.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr TF, Zeki AA, & Kraft M. (2017). Eosinophilic and noneosinophilic asthma. American Journal of Respiratory and Critical Care Medicine, 197(1), 22–37. doi: 10.1164/rccm.201611-2232PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cashion AK & Grady PA. (2015). The National Institutes of Health/National Institutes of Nursing Research Intramural Research Program and the development of the NIH Symptom Science Model. Nursing Outlook, 63(4), 484–487. doi: 10.1016/j.outlook.2015.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castner J, Gehrke GE, Shapiro N, & Dannemiller KC. (2018). Community interest and feasibility of using a novel smartphone-based formaldehyde exposure detection technology. Public Health Nursing. doi: 10.1111/phn.12384 [DOI] [PubMed]
- Castner J, Gittere S, & Seo JY. (2015). Criteria air pollutants and emergency nursing. J Emerg Nurs, 41(3), 186–192. doi: 10.1016/j.jen.2014.08.011 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention and US Department of Housing and Urban Development. (2008). Healthy housing inspection manual. Retrieved from https://www.cdc.gov/nceh/publications/books/inspectionmanual/healthy_housing_inspection_manual.pdf
- Centers for Disease Control and Prevention. (2011). Impact of the built environment on health. Retrieved from https://www.cdc.gov/nceh/publications/factsheets/impactofthebuiltenvironmentonhealth.pdf
- Duong A, Steinmaus C, McHale CM, Vaughan CP, & Zhang L. (2011). Reproductive and developmental toxicity of formaldehyde: a systematic review. Mutat Res, 728(3), 118–138. doi: 10.1016/j.mrrev.2011.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckardt P, Culley JM, Corwin E, Richmond T, Dougherty C, Pickler RH, … DeVon HA. (2017). National nursing science priorities: Creating a shared vision. Nursing Outlook, 65(6), 726–736. doi: 10.1016/j.outlook.2017.06.002 [DOI] [PubMed] [Google Scholar]
- Environmental Protection Agency. (2018a). Criteria air pollutants. Retrieved from https://www.epa.gov/criteria-air-pollutants
- Environmental Protection Agency. (2018b). Environmental Justice. Retrieved from https://www.epa.gov/environmentaljustice/learn-about-environmental-justice
- Flaskerud JH, Lesser J, Dixon E, Anderson N, Conde F, Kim S, … Verzemnieks I. (2002). Health disparities among vulnerable populations: evolution of knowledge over five decades in Nursing Research publications. Nurs Res, 51(2), 74–85. [DOI] [PubMed] [Google Scholar]
- Fraga MDB, Pinho RS, Andreoni S, Vitalle MSDS, Fisberg M, Peres MFP, … & Masruha MR. (2013). Trigger factors mainly from the environmental type are reported by adolescents with migraine. Arquivos de neuro-psiquiatria, 71(5), 290–293. [DOI] [PubMed] [Google Scholar]
- George M, Bruzzese JM, & Matura LA. (2017). Climate change effects on respiratory health: Implications for nursing. J Nurs Scholarsh, 49(6), 644–652. doi: 10.1111/jnu.12330. [DOI] [PubMed] [Google Scholar]
- Hoppin JA, Long S, Umbach DM, Lubin JH, Starks SE, Gerr F, … Sandler DP. (2012). Lifetime organophosphorous insecticide use among private pesticide applicators in the Agricultural Health Study. Journal of Exposure Science & Environmental Epidemiology, 22(6), 584–592. doi: 10.1038/jes.2012.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine, Committee on the effect of climate change on indoor air quality & public health. (2011). Climate change, the indoor environment, and health. Washington, D.C.: National Academies Press [Google Scholar]
- Kanehisa Laboratories. (2018). Kyoto Encyclopedia of Genes and Genomes (KEGG) Database (Release 88.2). Retrieved from https://www.kegg.jp/kegg/docs/relnote.html
- Khoury MJ, Coates RJ, Fennell ML, Glasgow RE, Scheuner MT, Schully SD, … Clauser SB. (2012). Multilevel research and the challenges of implementing genomic medicine. Journal of the National Cancer Institute Monographs, 2012(44), 112–120. doi: 10.1093/jncimonographs/lgs003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravitz-Wirtz N, Crowder K, Hajat A, & Sass V. (2016). The long-term dynamics of racial/ethnic inequality in neighborhood air pollution exposure, 1990–2009. Du Bois Review, 13(2), 237–259. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrigan PJ, Sly JL, Ruchirawat M, Silva ER, Huo X, Diaz-Barriga F, … Sly PD. (2016). Health consequences of environmental exposures: Changing global patterns of exposure and disease. Annals of Global Health, 82(1), 10–19. doi: 10.1016/j.aogh.2016.01.005 [DOI] [PubMed] [Google Scholar]
- Lee H, Kim S, DeMarco R, Aronowitz T, Mtengezo J, Kang Y, … Fitzpatrick JJ. (2015). Recognizing global disparities in health and in health transitions in the 21st century: what can nurses do? Appl Nurs Res, 28(1), 60–65. doi: 10.1016/j.apnr.2014.09.004 [DOI] [PubMed] [Google Scholar]
- Lenz R, & Pugh LC. (2018). Theory of unpleasant symptoms In Smith MJ & Iiehr PR. (Eds.), Middle range theory of nursing (4th ed.). New York, NY: Springer Publishing Company. [Google Scholar]
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, … Memish ZA. (2012). A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet, 380(9859), 2224–2260. doi: 10.1016/s0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Links JM, Schwartz BS, Simon D, Bandeen-Roche K, & Stewart WF. (2001). Characterization of toxicokinetics and toxicodynamics with linear systems theory: application to lead-associated cognitive decline. Environmental Health Perspectives, 109(4), 361–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch SM & Rebbeck TR. (2013). Bridging the gap between biological, individual, and macroenvironmental factors in cancer: A multilevel approach. Cancer Epidemiology Biomarkers & Prevention, 22(4), 485–495. doi: 10.1158/1055-9965.EPI-13-0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamiya H, Lix LM, Gardner W, Bartlett SJ, Ahmed S, & Buckeridge DL. (2017). Montreal Accord on Patient-Reported Outcomes (PROs) use series–Paper 5: patient-reported outcomes can be linked to epidemiologic measures to monitor populations and inform public health decisions. Journal of Clinical Epidemiology, 89, 142–147. doi: 10.1016/j.jclinepi.2017.04.018 [DOI] [PubMed] [Google Scholar]
- McEwen BS. (1998). Stress, adaptation, and disease. Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840, 33–44. [DOI] [PubMed] [Google Scholar]
- Meleis AI. (2012). Theoretical nursing: Development and progress. Philadelpha, PA: Wolters Kluwer. [Google Scholar]
- Ministry of Labor. (2019). Occupational Health Hazards and Illnesses. Retrieved from https://www.labour.gov.on.ca/english/hs/topics/health_hazards.php
- Mortensen ME, Calafat AM, Ye X, Wong LY, Wright DJ, Pirkle JL, … Moye J. (2014). Urinary concentrations of environmental phenols in pregnant women in a pilot study of the National Children’s Study. Environmental Research, 129, 32–38. doi: 10.1016/j.envres.2013.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Disease Prevention and Health Promotion. (2018). Leading health indiciators development and framework. Healthy People 2020. Retreived from https://www.healthypeople.gov/2020/leading-health-indicators/Leading-Health-Indicators-Development-and-Framework
- Pettibone KG, Balshaw DM, Dilworth C, Drew CH, Hall JE, Heacock M, … & Walker NJ. (2018). Expanding the concept of translational research: making a place for environmental health sciences. Environmental Health Perspectives, 126(7), 074501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polivka B, Folz R, Myers J, Barnett R, Antimisiaris D, Jorayeva A, & Beatty B. (2018). Identifying phenotypes and factors impacting outcomes in older adults with asthma: A research protocol and recruitment results. Research in Nursing and Health, 41(4), 336–345. DOI: 10.1002/nur.21880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polivka B, Chaudry R. (2018). A scoping review of environmental health nursing research. Public Health Nursing. 35, 10–17. DOI: 10.1111/phn.12373 [DOI] [PubMed] [Google Scholar]
- Pope CA, Ezzati Majid, & Dockery Douglas W. (2009). Fine-particulate air pollution and life expectancy in the United States. New England Journal of Medicine, 360(4), 376–386. doi: 10.1056/NEJMsa0805646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B. (2018). Theory of self-efficacy In Smith MJ & Iiehr PR (Eds.), Middle range theory of nursing (4th ed.). New York, NY: Springer Publishing Company. [Google Scholar]
- Rodriguez J, Huntington-Moskos L, Johnson A, Williams S, Gulledge E, Feeley C, & Rice M. (2016). Collecting biological measures for research with children and adolescents. Journal of Pediatric Health Care, 30(3), 279–283. doi: 10.1016/j.pedhc.2015.12.007 [DOI] [PubMed] [Google Scholar]
- Rose JJ, Wang L, Xu Q, McTiernan CF, Shiva S, Tejero J, & Gladwin MT. (2017). Carbon monoxide poisoning: Pathogenesis, management, and future directions of therapy. American Journal of Respiratory and Critical Care Medicine, 195(5), 596–606. doi: 10.1164/rccm.201606-1275CI [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutledge DM, & McGuire C. (2004). Evidence-based symptom management In Yarbro CH, Frogge MH, & Goodan M (Eds.), Cancer Symptom Management (pp. 3–14). Sudbury: Jones & Bartlett. [Google Scholar]
- Schmid-Mohler G, Caress A-L, Spirig R, & Yorke J. (2019). Introducing a model for emotional distress in respiratory disease: A systematic review and synthesis of symptom management models. Journal of Advanced Nursing, 0(0). doi: 10.1111/jan.13968 [DOI] [PubMed] [Google Scholar]
- Shin HM, McKone TE, Sohn MD, & Bennett DH. (2014). Tracking contributions to human body burden of environmental chemicals by correlating environmental measurements with biomarkers. PLoS One, 9(3), e93678. doi: 10.1371/journal.pone.0093678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sicotte D, & Swanson S. (2007). Whose risk in Philadelphia? Proximity to unequally hazardous industrial facilities. Social Science Quarterly, 88(2), 515–534. [Google Scholar]
- Simoni Marzia, Baldacci Sandra, Maio Sara, Cerrai Sonia, Sarno Giuseppe, & Viegi Giovanni. (2015). Adverse effects of outdoor pollution in the elderly. Journal of Thoracic Disease, 7(1), 34–45. doi: 10.3978/j.issn.2072-1439.2014.12.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strum M, & Scheffe R. (2016). National review of ambient air toxics observations. Journal of the Air & Waste Management Association, 66(2), 120–133. doi: 10.1080/10962247.2015.1076538 [DOI] [PubMed] [Google Scholar]
- Smith MC, & Parker ME. (2015). Nursing theories and nursing practice (4th ed.). Philadelphia, PA: F. A. Davis Company. [Google Scholar]
- Szyszkowicz M, Kousha T, Castner J, & Dales R. (2018). Air pollution and emergency department visits for respiratory diseases: A multi-city case crossover study. Environmental Research, 163, 263–269. doi: 10.1016/j.envres.2018.01.043 [DOI] [PubMed] [Google Scholar]
- Talaska G, Thoroman J, Schuman B, & Kafferlein HU. (2014). Biomarkers of polycyclic aromatic hydrocarbon exposure in European coke oven workers. Toxicology Letters, 231(2), 213–216. doi: 10.1016/j.toxlet.2014.10.025 [DOI] [PubMed] [Google Scholar]
- Thompson MR, & Schwartz Barcott D. (2017). The concept of exposure in environmental health for nursing. Journal of Advanced Nursing, 73(6), 1315–1330. doi: 10.1111/jan.13246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurston GD, Ito K, Lall R, Burnett RT, Turner MC, Krewski D, … Pope CA. (2013). NPACT Study 4. Mortality and long-term exposure to PM2.5 and its components in the American Cancer Society’s Cancer Prevent Study II cohort. Retrieved from www.healtheffects.org
- Wenzel SE. (2012). Asthma phenotypes: The evolution from clinical to molecular approaches. Nature Medicine, 18(5), 716–725. [DOI] [PubMed] [Google Scholar]
- Wild CP. (2012). The exposome: from concept to utility. International Journal of Epidemiology, 41(1), 24–32. doi: 10.1093/ije/dyr236 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2010). WHO guidelines for indoor air quality: Selected pollutants. Retrieved from http://www.who.int [PubMed]
- World Health Organization. (2011). Biomarkers and human biomonitoring. Retrieved from http://www.who.int/ceh/capacity/biomarkers.pdf


