ABSTRACT
A 53-year-old man with tuberous sclerosis complex presented with severe, acute, right lower quadrant pain. The patient was found to have ileocolonic intussusception and a cecal mass on imaging. Diagnostic colonoscopy revealed a 3-cm cecal lesion which was grossly equivocal for hamartoma, adenoma, or other neoplasm, biopsies of which revealed villous adenoma. Given the lesion was believed to represent the trigger point for intussusception, the patient was referred for surgical resection, the histopathology from which the lesion was identified to be invasive adenocarcinoma. The patient underwent hemicolectomy, with plans for routine postoperative colon cancer surveillance. This case is unique because previously published literature has not described adenocarcinoma in an adult with tuberous sclerosis complex and it calls attention to the need to maintain unsuspected cancer high on the differential in adults with intussusception.
INTRODUCTION
Intussusception is the telescoping of a portion of a bowel segment into the lumen of another. It is most frequently seen in children, where it is commonly idiopathic; in adults, intussusception is predominantly secondary to a pathologic lesion acting as a lead point (eg, stricture due to inflammatory bowel disease or previous surgical intervention, large polyp), with more than half of cases being caused by an underlying malignancy.1 We present a case of extensive ileocolonic intussusception in a patient with tuberous sclerosis complex (TSC), a neurocutaneous disorder caused by an autosomal dominant or sporadic mutation in the TSC1 or TSC2 gene. The expression of these genes is highly variable and leads to a wide range of presentations, but most notably, it is characterized by benign tumors called hamartoma, which can serve as a lead point for intussusception. In this case, however, the intussusception was because of a more sinister and unsuspected process.
CASE REPORT
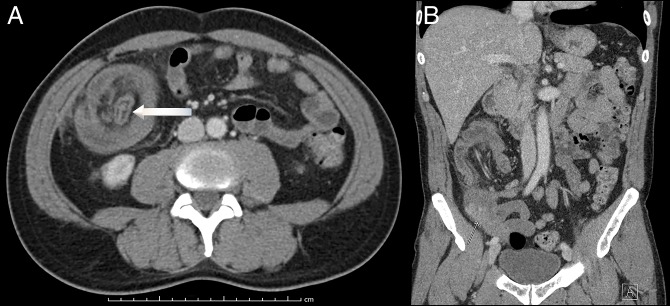
A 53-year-old man with TSC presented to the emergency department with 1 day of severe, acute, right lower quadrant pain. The pain was constant and nonradiating and had started without apparent provocation. On further questioning, he noted 4 months of intermittent abdominal distention and constipation. He denied recent fevers, weight loss, early satiety, nausea, and vomiting. He had no personal history of colonoscopy and no known family history of gastrointestinal diseases. Vital signs on presentation were normal except for tachycardia to 102 beats per minute. Physical examination revealed a mildly distended abdomen with tenderness to palpation in the right lower quadrant, without rebound. Laboratory studies, including complete blood count, serum electrolytes, and lactate, were within normal limits. Computed tomography of the abdomen and pelvis with intravenous contrast demonstrated ileocolonic intussusception that extended from the terminal ileum to the hepatic flexure, with adjacent fat stranding and increased soft tissue in the cecal wall concerning for possible polyp or another lesion (Figure 1).
Figure 1.
Abdominal and pelvic computed tomography (A) axial view showing intussusception (arrow) and (B) coronal view showing fat stranding and increased soft tissue in the cecal wall (arrow).
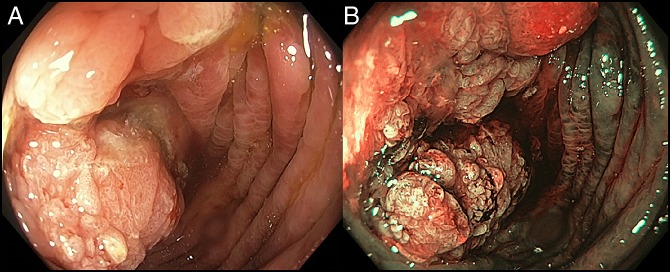
The patient was admitted to the hospital. After discussion with colorectal surgery regarding management approaches, including how to best evaluate for an underlying cause of intussusception, diagnostic colonoscopy was performed. This revealed a 3-cm “cauliflower”-like polypoid cecal lesion with surrounding dusky mucosa, visualized with white light and narrow-band imaging and 2 small (<5 mm) polyps, one in the transverse and one in the descending colon (Figure 2). Numerous biopsies of the cecal lesion were obtained and the polyps were resected in toto. On the basis of the radiographic, colonoscopic, and histopathologic features, a right hemicolectomy was performed during the index hospitalization.
Figure 2.
Endoscopy showing (A) a polypoid cecal lesion with white light and cecal lesion and (B) narrow-band imaging of cecal lesion.
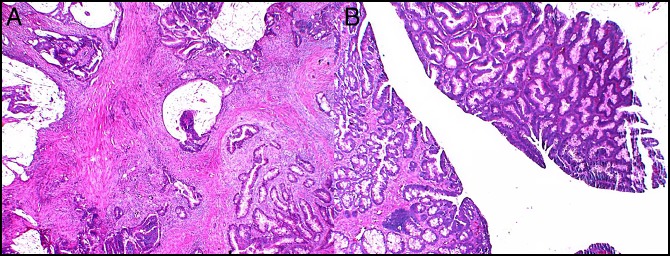
Biopsies of the cecal lesion revealed villous adenoma, whereas the full-thickness surgical specimen was positive for invasive cecal adenocarcinoma (Figure 3). The patient recovered uneventfully from a right hemicolectomy with primary anastomosis, and a decision was made by the tumor board to surveil the patient, according to the American Joint Committee on Cancer guidelines.
Figure 3.
Biopsy of the cecal lesion showing (A) villous adenoma and (B) cecal adenocarcinoma.
DISCUSSION
This present case highlights the importance of considering malignancy as the likely cause of intussusception, even if initial biopsies do not reveal carcinoma and/or the patient has a known benign underlying condition. Indeed, a high index of suspicion should be maintained, and prompt measures should be taken to rule out this possibility.
Definitive treatment of intussusception in adults (in the absence of an underlying causal systemic disorder, eg, celiac disease) is surgical resection, specifically given that more than 50% of cases are caused by malignancy, with adenocarcinoma being the most likely.1 Attempts at reduction before surgical intervention have been described but are of uncertain benefit; even if successful, colonoscopic evaluation and/or pathologic diagnosis would remain indicated to formulate an unequivocal treatment plan.2
In addition, notable about this case is the unclear association between TSC and malignancy. Although this disorder is often characterized by its multiorgan involvement and benign (ie, noncancerous) nature, it has also been associated with an 18-fold increase in malignancy in children, specifically of the brain, kidneys, and soft tissue, for unclear reasons.3 However, despite this increased likelihood of certain pediatric cancers (the underlying pathophysiology of which remains unknown), TSC has not been previously associated with adenocarcinoma in adults. Histopathology of hamartomatous lesions shows limited, if any, atypia or mitotic activity, and whereas gastrointestinal involvement of TSC is rare, the most common manifestation appears to be hamartomatous polyps in the rectosigmoid.4 Therefore, although there may be some as yet unknown genetic or other underlying association, in this case, the cecal adenocarcinoma was believed to most likely be sporadic. Last, although genetic testing should be considered in all cases of primary gastrointestinal adenocarcinoma, given the pathology findings, lack of family history, and associated costs, it was not recommended for this patient.
DISCLOSURES
Author contributions: A. Zhornitskiy and NB Marya wrote the manuscript and provided the images. JH Tabiban provided the images, revised the manuscript, and is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
REFERENCES
- 1.Marinis A, Yiallourou A, Samanides L, et al. Intussusception of the bowel in adults: A review. World J Gastroenterol. 2009;15(4):407–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Onkendi EO, Grotz TE, Murray JA, Donohue JH. Adult intussusception in the last 25 years of modern imaging: Is surgery still indicated? J Gastrointest Surg. 2011;15(10):1699–705. [DOI] [PubMed] [Google Scholar]
- 3.Narod SA, Stiller C, Lenoir GM. An estimate of the heritable fraction of childhood cancer. Br J Cancer. 1991;63(6):993–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gould SR. Hamartomatous rectal polyps are common in tuberous sclerosis. Ann N Y Acad Sci. 1991;615:71–80. [DOI] [PubMed] [Google Scholar]