ABSTRACT
Ischemic colitis is a common form of bowel ischemia typically associated with vasculopathy in advanced age. Although some predisposing factors can increase the risk of developing ischemic colitis, the disease is relatively uncommon in young adults. Furthermore, cases of ischemic colitis associated with pregnancy are exceedingly rare. We present a young woman with severe ischemic colitis after vaginal delivery that ultimately led to sigmoid resection due to persistent stricturing.
INTRODUCTION
Ischemic colitis is one of the most common forms of gastrointestinal injury that occurs because of an inadequate blood supply to the large bowel. Disease severity can vary depending on the degree and location of vascular compromise. Symptoms of nonocclusive disease are generally transient and resolve spontaneously, but severe stenosis or occlusive disease may require invasive interventions.1 Segmental disease involving the left colon is more common and has less complications, whereas bilateral and isolated right colon ischemia are associated with higher rates of surgery and greater morbidity and mortality.2 The etiology of ischemia can be multifactorial, but pathogenesis is most commonly due to underlying intestinal vasculopathy that can develop in advanced age.2 Consequently, colonic ischemia predominantly affects the elderly population. Although certain factors can predispose individuals at an earlier age, acute large bowel ischemia is uncommon in young patients and is exceedingly rare as a potential complication of pregnancy.
CASE REPORT
A 29-year-old primigravida with chronic hepatitis C infection from past illicit substance use underwent a vacuum-assisted vaginal delivery of a term pregnancy. The patient suffered a small second-degree perineal laceration during delivery which was successfully repaired. The estimated blood loss was less than 300 mL, and she remained hemodynamically stable throughout delivery.
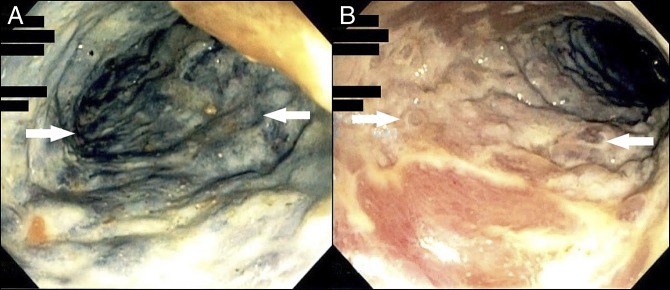
On postpartum day 0, a few hours after delivering, she developed severe left lower quadrant abdominal pain and bloody diarrhea. A complete blood count demonstrated a hemoglobin level of 11 g/dL, which was unchanged from the hemoglobin level of 11.1 g/dL before the onset of the symptoms. Her blood count remained stable on serial laboratory studies. Abdominal computed tomography (CT) demonstrated bowel wall thickening involving the left colon (distal transverse, descending, and sigmoid) suspicious for colitis (Figure 1).
Figure 1.
Coronal abdominal computed tomography showing colonic wall thickening involving the descending and sigmoid colon (white arrows), and an enlarged, heterogeneous-appearing uterus which is compatible with recent postpartum state is also evident (black arrow).
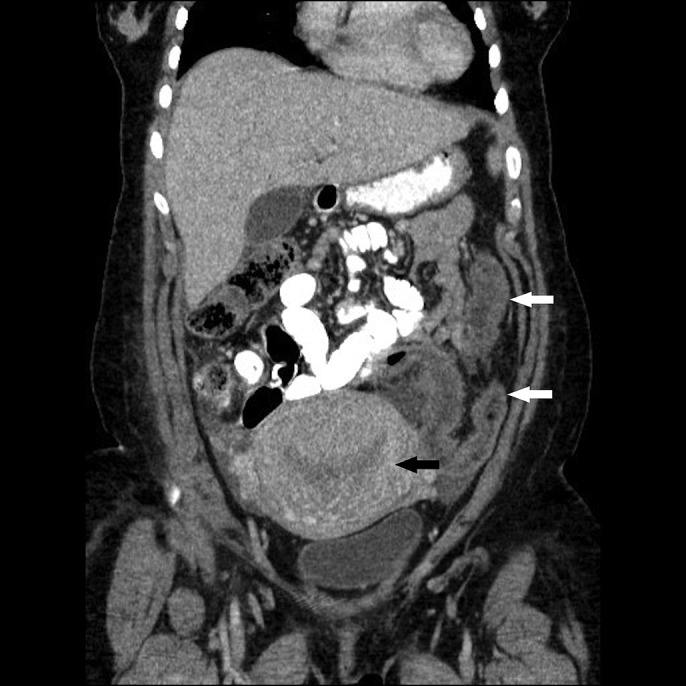
After consultation with a gastroenterologist, a flexible sigmoidoscopy was performed on postpartum day 1. This revealed extensive dusky and edematous mucosa, which is suggestive of ischemia and continuous inflammation from the rectum up to the descending colon with large areas of mucosal erythema and erosions (Figure 2). Histological examination of the biopsies found marked active colitis with ulcerative debris and gland dropout. No granulomas, dysplasia, or malignancy were identified, and comprehensive microorganism testing was negative. Because of the severity of large bowel injury, an evaluation by colorectal surgery was requested, and the patient was transferred to the intensive care unit for closer monitoring. Medical management in the critical care unit consisted of empiric intravenous antibiotics because of the concerns of potential infection from bacterial translocation, isotonic crystalloids for hydration, and analgesics. Because the patient made gradual clinical improvement with ongoing supportive care, no surgical intervention was pursued.
Figure 2.
Flexible sigmoidoscopy showing (A) extensive dusky discoloration and mucosal edema suggestive of ischemia (white arrows) and (B) areas of mucosal erythema, inflammation, and erosions (white arrows).
An extensive investigation into other potential etiologies including inflammatory bowel disease, vasculitides, cryoglobulinemia, and coagulopathies was unremarkable. The patient was hemodynamically stable throughout her hospital course. She had no known personal or family history of acquired or hereditary thrombophilia. She was not on any chronic medications, and she was not actively using illicit substances during pregnancy. On excluding all other possible causes, she was diagnosed with acute ischemic colitis. She was discharged on postpartum day 5 in stable condition but experienced recurrent symptoms a few days later, prompting readmission for intravenous hydration and pain control. Abdominal and pelvic CT showed findings of colitis that were unchanged from previous imaging. No vascular pathology or hemodynamically significant stenoses were detected.
Eight weeks after the initial onset of symptoms, surveillance colonoscopy discovered a tight stricture in the sigmoid colon that had formed because of recent ischemia (Figure 3). Efforts to dilate and traverse the stricture endoscopically were unsuccessful. A subsequent CT colonography demonstrated persistent abnormal circumferential wall thickening and luminal narrowing, extending from the splenic flexure to the juncture of the distal descending and sigmoid colon. The patient was referred for colorectal surgery and ultimately underwent a laparoscopic sigmoidectomy. Gross pathology of the surgical specimens showed ulceration and moderate inflammation of the mucosal surface associated with some crypt distortion and occasional crypt abscesses consistent with ischemia (Figure 4). Features suggestive of chronic inflammatory disease such as basal plasmacytosis, transmural lymphoid aggregates, granulomata, and pyloric or Paneth cell metaplasia were not evident. Two months after her surgery, flexible sigmoidoscopy showed a well-healed anastomosis and no sign of ongoing colitis.
Figure 3.
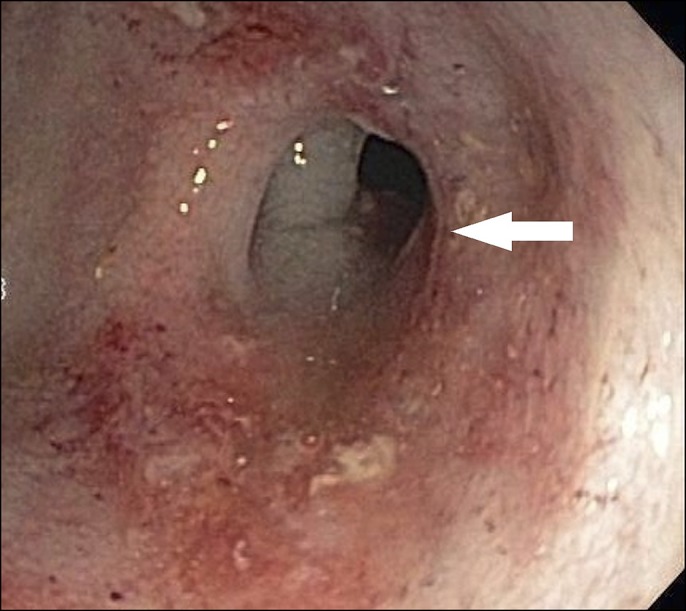
Surveillance colonoscopy showing a tight stricture in the sigmoid colon (white arrow) 40 cm from the anus with areas of local inflammation and friable mucosa.
Figure 4.
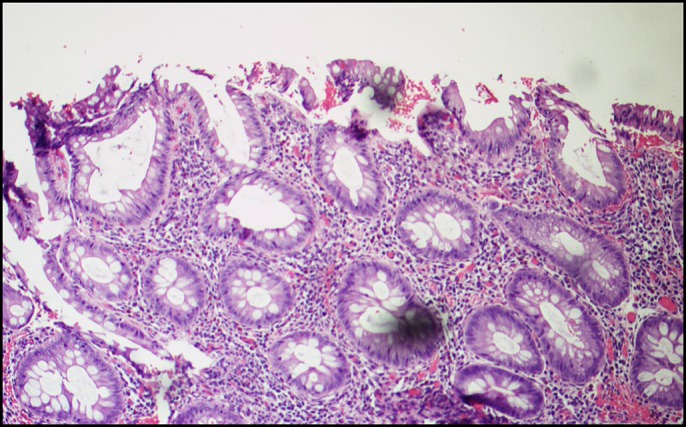
Histopathology showing ulceration and moderate acute inflammation of the mucosal surface associated with crypt distortion and occasional crypt abscesses.
DISCUSSION
The premise of this case is to discuss an unusual presentation of acute large bowel ischemia in a young pregnant patient, which was not due to an apparent vascular occlusion or other identifiable cause. To our knowledge, there have been no reported cases in the literature of intestinal ischemia specifically associated with pregnancy. The exact pathogenesis remains elusive because of limited clinical data and experience, but an estrogen-induced hypercoagulable state may have a significant role based on several documented cases of transient ischemic colitis in women taking oral contraceptives.2–4 The pathologic mechanism is thought to be the result of excess estrogen, causing an increased risk of thromboemboli formation within the small segmental colonic vasculature.2 Further studies are needed to definitively elucidate the underlying pathophysiologic processes. For now, physicians should stay mindful of the physiologic changes that occur during pregnancy. Although it is rare, we advise clinicians to consider acute intestinal ischemia in the differential when evaluating pregnant patients with abdominal pain and bloody diarrhea.
DISCLOSURES
Author contributions: B. Kim and H. Tayel reviewed the literature and wrote the manuscript. KJ Chaput reviewed the literature and approved the final version. B. Kim is article guarantor.
Financial disclosure: None to report.
Previous presentation: This case was presented at the Pennsylvania Society of Gastroenterology (PSG) Annual Scientific Meeting; September 14–16, 2018; Hershey, Pennsylvania; and the American College of Gastroenterology Annual Scientific Meeting; October 5–10, 2018; Philadelphia, Pennsylvania.
Informed consent was obtained for this case report.
Acknowledgments
The authors would like to acknowledge Dr Daniel Bowers and Dr Berhanu Bowers who supported patient care and served as advisors for the colorectal surgery and Dr Lisa M. Stoll and Dr Santo Longo who served as scientific advisers on pathology findings.
REFERENCES
- 1.Koutroubakis IE, Theodoropoulou A. Ischemic colitis: Clinical practice in diagnosis and treatment. World J Gastroenterol. 2008;14(48):7302–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Longstreth GF, Yao JF. Diseases and drugs that increase risk of acute large bowel ischemia. Clin Gastroenterol Hepatol. 2010;8:49–54. [DOI] [PubMed] [Google Scholar]
- 3.Choon SS, Young SP, Se HP, et al. A case of oral-contraceptive related ischemic colitis in young woman. Clin Endosc. 2011;44:129–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rasmussen DK, Segars LW. Case of ischemic colitis in a young adolescent associated with triphasic hormonal contraceptive therapy: A case report and review of the literature. W V Med J. 2011;107:22–5. [PubMed] [Google Scholar]