Abstract
Botulinum toxin (Botox) was introduced for the management of internal anal sphincter (IAS) achalasia after a pull-through procedure in Hirschsprung disease (HD). We conducted a prospective evaluation of the efficacy and safety of this Botox treatment.
Our study group included 15 patients with HD (median age, 4.8 years; range, 1.7–7.4 years) who experienced persistent constipation after pull-through surgery. Rectal biopsy and colon study were performed before Botox injection to exclude agangliosis. Intersphincteric Botox injections (dose, 4 IU/kg) were performed at 3 sites, (3, 6, and 9 o’clock) under general anesthesia. Measured outcomes of efficacy included anorectal manometry, Wexner constipation score and the quality of life score for defecation, measured at baseline and at 2 weeks and 3 months after injection. The Holschneider incontinence score and an assessment of pain, bleeding, heating sensation, and swelling were also performed at follow-up as outcomes of safety.
There was no significant change in measured outcomes with Botox treatment. Botox did decrease the number of patients who experienced abdominal distension at 3 months, compared to 2-weeks, post-injection. No major complications were identified, with only 2 cases of anal bleeding that resolved spontaneously. Local tenderness at the injection site was reported by 4 patients, recovering without treatment.
The efficacy of Botox, injected into the IAS, for the treatment of achalasia is questionable on short-term follow-up. Larger studies with a longer follow-up period and the use of repeated injections are required to evaluate the evidence for this treatment.
Keywords: botulinum toxins, constipation, Hirschsprung disease, internal anal sphincter
1. Introduction
Although good clinical outcomes can generally be expected in patients with Hirschsprung disease (HD) after surgical correction, using pull-through procedure, obstructive gastrointestinal symptoms do develop in 10% to 30% of cases.[1–3] These patients experience persistent constipation, which is usually treated with laxatives or enemas; however, severe symptoms of abdominal distension, vomiting, and enterocolitis can also be presenting factor.[4] Internal anal sphincter (IAS) achalasia is present in all children with HD, with a myectomy normally performed as a treatment for severe obstructive symptoms. However, this treatment is not always successful and can result in irreversible sphincter injury and fecal incontinence.[5,6] To minimize these risks, intrasphincteric botulinum toxin (Botox) has been widely used to treat patients with obstructive symptoms after pull-through surgery for HD, since first being introduced by Langer and Birnbaum in 1997.[7] However, evidence regarding the efficacy and safety is still lacking for this procedure. Therefore, the aim of our study was to prospectively evaluate the efficacy and safety of Botox for the treatment of children with obstructive symptoms after pull-through surgery.
2. Materials and methods
Our study group was formed of patients with HD, 18 months to 18 years of age, who experienced persistent constipation after undergoing a pull-through procedure at our hospital and in whom symptoms of obstruction were not improved with application of laxative medication. Rectal biopsy, anorectal manometry, and colon barium study were performed before Botox injection to exclude the presence of aganglionosis. Patients were screened on the following exclusion criteria; a prior allergic reaction to Botox; a tendency to bleeding or current anticoagulant therapy; previous Botox application to another site within 3 months; any neuromuscular disease, such as myasthenia gravis; and possibility of pregnancy.
Botulinum toxin A vials produced by Allergan were used for treatment. Botox was used at a concentration of 100 U/mL mixed with normal saline, with an individual dosage of 4 IU/kg (up to 100 IU total) calculated from each patient's body weight. The procedure was performed under general anesthesia, with the patient in the lithotomy position. Botox was injected intramuscularly into the IAS, using a 26-gauge needle, at 3 sites in the sphincter, namely at 3, 6, and 9 o’clock. All patients were hospitalized for observation after the procedure and discharged on the next day.
Patients were prospectively evaluated through our out-patient clinic at 2-weeks (immediate follow-up) and at 3 months (short-term follow-up). Treatment efficacy was evaluated using anorectal manometry, the Wexner constipation score (WCS) and the quality of life (QOL) score for defecation, with the change in score at 2 weeks and 3 months after injection, from baseline, used for analysis, with a lower WCS and QOL representing a better outcome status. The development of abdominal distension and enteritis after injection were evaluated by the surgeon. Safety was evaluated using the Holschneider incontinence score (HIS) and by the presence of pain or discomfort, bleeding, heating sensation, and swelling around the anal sphincter at 2 weeks and 3 months after injection, with a higher HIS score indicative of better continence.
Continuous data are summarized as the median with the range or the mean with standard deviations, and categorical data are summarized as proportions and percentages. Dichotomous and trichotomous variables were analyzed with the Chi-square test. Continuous variables were assessed using the paired T test and analysis of variance respectively. P-value of less than .05 was considered statistically significant. All statistical analyses were performed with the SPSS version 21.0, software (SPSS Inc, Chicago, IL).
This prospective study was approved by our Institutional Review Board (IRB No.: 1410-085-618).
3. Results
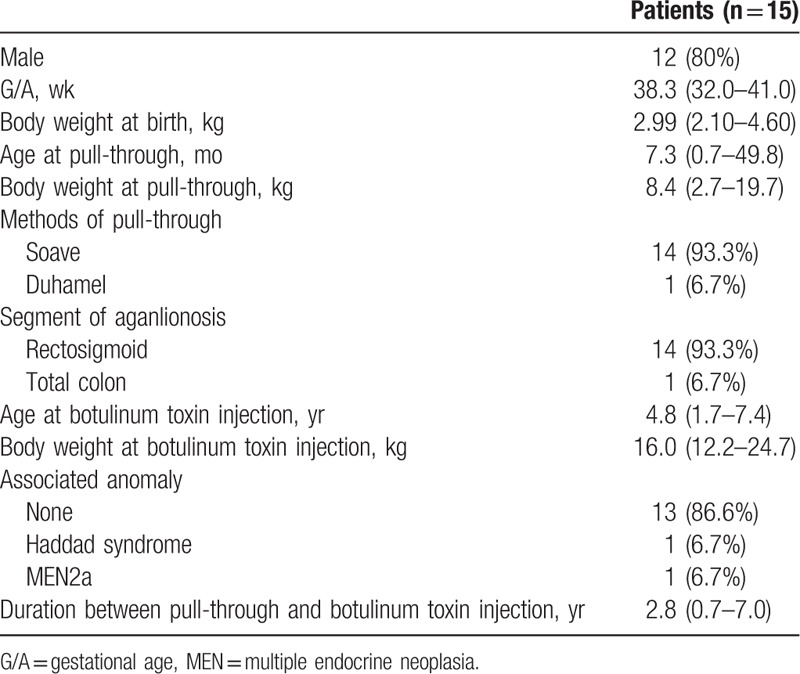
Fifteen patients with HD who underwent a pull-through procedure were included in our study group, with a median age at the time of surgery of 7.3 (range, 0.7–49.8) months, median age at the time of the Botox injection procedure of 4.8 (range, 1.7–7.4) years and body weight of 16.0 (range, 12.2–24.7) kg. With regard to the type of pull-through surgery performed, a Soave procedure was used in 14 cases (93.3%) and a Duhamel procedure in the remaining case. Aganglionic segments were identified in the rectosigmoid segment in 14 cases and in the entire colon in the remaining case. The median duration between the pull-through procedure and the Botox injection was 2.8 (range, 0.7–7.0) years. The relevant patient demographics are summarized in Table 1.
Table 1.
Patient demographics.
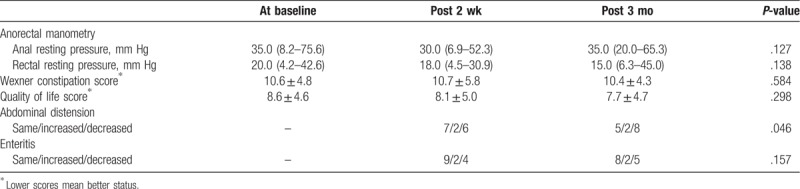
Rectal biopsies showed no residual aganglionosis in all patients. Colon study performed before Botox injection revealed no mechanical cause of obstruction. On pre-procedural anorectal manometry, the recto-anal inhibitory reflex was not present in all patients, with resting anal and rectal pressures of 35.0 mm Hg and 20.0 mm Hg, respectively. The mean WCS and QOL score before the procedure was 10.6 and 8.6, respectively.
After injection, there was a non-significant decrease in the resting anal and rectal pressure at 2 weeks (P = .127) and 3 months (P = .138). Even though decrease of WCS and QOL was observed in 11 (73.3%) and 10 (66.7%) patients, respectively, the mean WCS (P = .584) and QOL (P = .298) scores showed non-significant decrease as 10.4 and 7.7, respectively. Compared to baseline, a decrease in abdominal distention was identified in 6 patients at 2 weeks and 8 patients at 3 months. Moreover, enteritis resolved in 4 cases by week 2 and in another 5 cases by 3 months after injection. Outcome measurements, at baseline and at the 2-week and 3-month follow-up, are reported in Table 2.
Table 2.
Outcomes after botulinum toxin injection.
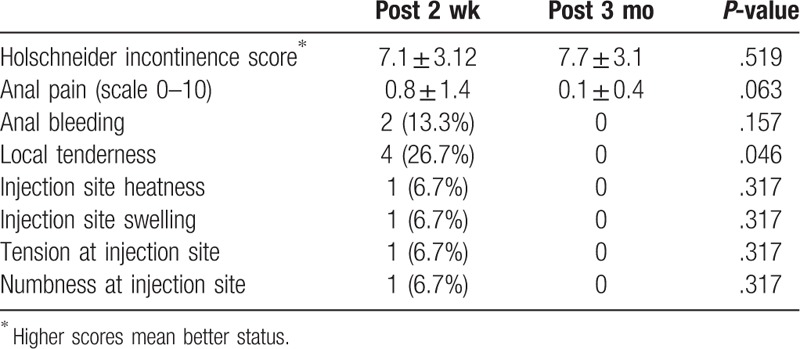
There was a nonsignificant change in incontinence at 2-weeks and 3-months after injection, with an increase in the HIS score from 7.1 at baseline to 7.7 at 3 months. The median anal pain score was 0.8/10 at 2 weeks, decreasing to 0.1/10 at the 3-month follow-up. Anal bleeding at the site of injection was observed in 2 patients, which resolved spontaneously without treatment. Local tenderness at the site of injection was reported in 4 patients, which resolved without treatment. Post-procedural side effects are listed in Table 3.
Table 3.
Post-injection complications.
4. Discussion
Symptoms of bowel obstruction, including fecal incontinence and enterocolitis can develop in patients with HD after a pull-through procedure. Inability of the IAS to relax may be the cause of these symptoms.[8] The severity of these obstructive symptoms can vary widely and patients may experience more than 1 symptom. Chronic obstruction may impair intestinal function and cause failure to thrive. Initial treatment of a chronic bowel obstruction after a pull-through procedure generally includes repeated mechanical evacuation and the use of enemas or laxatives.[9] In the absence of improvement in obstruction symptoms with this supportive therapy, posterior IAS myectomy has been the surgical treatment of choice over the past 50 years. However, this procedure carries the risk of permanent injury to the IAS, and possible fecal incontinence, as well as not always effective in relieving symptoms of obstruction.[5,6]
In 1997, the use of Botox injection into the IAS was introduced as a treatment for persistent obstructive symptoms after a pull-through surgery in patients with HD, which did not damage the IAS.[7] Promising results of Botox injection into the IAS have been reported for both short-term and longer-term follow-up in various small scale studies.[1,8,10–12] As an example, Minkes et al reported resolution of obstructive symptoms and a decrease in the IAS pressure at 1 month after Botox injection in 18 patients.[11] The success rate of Botox injection for the treatment of persisting obstructive from short-term follow-up has been reported to range between 62% and 89% (8,11,13,14), with successful long-term outcomes reported in >50% of cases.[8,13] Moreover, Chumpitazi et al reported that favorable outcomes were maintained for mean 17.1 months after the last Botox injection.[13] The maximal resting anal and rectal pressure was measured using anorectal manometry, with a decrease from pre-injection baseline having been reported on short- and long-term follow-up.[10,11] The hospitalization rate for enterocolitis in patients with HD has been reported to be significantly lower after Botox injection into the IAS.[13,14]
Our study is a prospective clinical trial with immediate (2 weeks) and short-term (3 months) post-procedural evaluations of treatment efficacy and safety. Overall, we did not find any significant benefit of Botox injection into the IAS, with no change in the constipation score (WCS), and nonsignificant improvements in the QOL score and resting anal and rectal pressures. Moreover, treatment did not change the degree of enteritis, although abdominal distension did decrease. Based on our findings, we can argue that Botox injection into the IAS is not an effective treatment for persistent constipation and does not improve QOL relative to defecation, although we did identify a benefit of the treatment in improving abdominal distension.
As per previous studies, we did not identify any significant complication related to the injection. Transient complications previously reported, and identified in our study, include anal pain,[11] fecal incontinence, which can occur in up to 10% of patients and can last a few days [8,13] and pain at the injection site. A previous study reported the absence of complications after a mean follow-up duration of 5 years.[14] None of the patients who developed complications in our study group required either medical or surgical treatment. Similarly, anal pain decreased from 2-weeks to 3-months, with 4 patients reporting pain at 2-weeks and 2 at 3-months; however, the level of pain was low overall, with a mean pain score of <1 out of 10. As well, bleeding at the injection site was identified in only 2 patients, which resolved spontaneously. The degree of local tenderness was higher immediately after injection, and improved without further management by the 3-month follow-up. Therefore, in agreement with previous studies, we can conclude from our findings that Botox injection into the IAS is a safe procedure.
Of note are findings from other studies that have reported a non-response rate to Botox injection as high as 37.5%,[15] with a high recurrence of obstructive symptoms.[9,12,16] In fact, in their case series, Ciamarra et al reported a relapse rate of 20% among patients who had an initial positive response to Botox injection, with these patients ultimately requiring a myectomy of the IAS.[9] Wester et al reported that repeated injections are needed due to the temporary effect of Botox if the use of laxatives and enemas is to be avoided over the longer term.[12]
In conclusion, Botox injection for the treatment of obstructive symptoms after a pull-through procedure in patients with HD is questionable over a short-term follow-up. Small sample size is a limitation of this study, and there could be type 2 errors. Larger studies with a longer follow-up period and the use of repeated injections are required to evaluate the evidence for this treatment.
Author contributions
Conceptualization: Joong Kee Youn, Hyun-Young Kim.
Data curation: Joong Kee Youn, Hyun-Young Kim, Ji-Won Han, Chaeyoun Oh, So-Young Kim, Sung-Eun Jung.
Formal analysis: Joong Kee Youn, Chaeyoun Oh.
Funding acquisition: Hyun-Young Kim.
Methodology: Joong Kee Youn, Hyun-Young Kim, Ji-Won Han, Chaeyoun Oh, Sung-Eun Jung.
Resources: So-Young Kim.
Supervision: Hyun-Young Kim.
Writing – original draft: Joong Kee Youn.
Writing – review and editing: Joong Kee Youn, Hyun-Young Kim, Ji-Won Han, Chaeyoun Oh, So-Young Kim, Sung-Eun Jung.
Footnotes
Abbreviations: Botox = botulinum toxin, HD = Hirschsprung disease, HIS = Holschneider incontinence score, IAS = internal anal sphincter, QOL = quality of life, WCS = Wexner constipation score.
How to cite this article: Youn JK, Han JW, Oh C, Kim SY, Jung SE, Kim HY. Botulinum toxin injection for internal anal sphincter achalasia after pull-through surgery in Hirschsprung disease. Medicine. 2019;98:45(e17855).
This research was supported by a grant (14172MFDS178) from the Ministry of Food and Drug Safety of Korea in 2016.
The authors have no conflicts of interest to disclose.
References
- [1].Chumpitazi BP, Nurko S. Defecation disorders in children after surgery for Hirschsprung disease. J Pediatr Gastroenterol Nutr 2011;53:75–9. [DOI] [PubMed] [Google Scholar]
- [2].Menezes M, Puri P. Long-term outcome of patients with enterocolitis complicating Hirschsprung's disease. Pediatr Surg Int 2006;22:316–8. [DOI] [PubMed] [Google Scholar]
- [3].Tariq GM, Brereton RJ, Wright VM. Complications of endorectal pull-through for Hirschsprung's disease. J Pediatr Surg 1991;26:1202–6. [DOI] [PubMed] [Google Scholar]
- [4].Langer JC. Persistent obstructive symptoms after surgery for Hirschsprung's disease: development of a diagnostic and therapeutic algorithm. J Pediatr Surg 2004;39:1458–62. [DOI] [PubMed] [Google Scholar]
- [5].Heikkinen M, Lindahl H, Rintala RJ. Long-term outcome after internal sphincter myectomy for internal sphincter achalasia. Pediatr Surg Int 2005;21:84–7. [DOI] [PubMed] [Google Scholar]
- [6].Wildhaber BE, Pakarinen M, Rintala RJ, et al. Posterior myotomy/myectomy for persistent stooling problems in Hirschsprung's disease. J Pediatr Surg 2004;39:920–6. [DOI] [PubMed] [Google Scholar]
- [7].Langer JC, Birnbaum E. Preliminary experience with intrasphincteric botulinum toxin for persistent constipation after pull-through for Hirschsprung's disease. J Pediatr Surg 1997;32:1059–61. [DOI] [PubMed] [Google Scholar]
- [8].Han-Geurts IJ, Hendrix VC, de Blaauw I, et al. Outcome after anal intrasphincteric Botox injection in children with surgically treated Hirschsprung disease. J Pediatr Gastroenterol Nutr 2014;59:604–7. [DOI] [PubMed] [Google Scholar]
- [9].Ciamarra P, Nurko S, Barksdale E, et al. Internal anal sphincter achalasia in children: clinical characteristics and treatment with Clostridium botulinum toxin. J Pediatr Gastroenterol Nutr 2003;37:315–9. [DOI] [PubMed] [Google Scholar]
- [10].Jiang da P, Xu CQ, Wu B, et al. Effects of botulinum toxin injection on anal achalasia after pull-through operations for Hirschsprung's disease: a 1-year follow-up study. Int J Colorectal Dis 2009;24:597–8. [DOI] [PubMed] [Google Scholar]
- [11].Minkes RK, Langer JC. A prospective study of botulinum toxin for internal anal sphincter hypertonicity in children with Hirschsprung's disease. J Pediatr Surg 2000;35:1733–6. [DOI] [PubMed] [Google Scholar]
- [12].Wester T, Granstrom AL. Botulinum toxin is efficient to treat obstructive symptoms in children with Hirschsprung disease. Pediatr Surg Int 2015;31:255–9. [DOI] [PubMed] [Google Scholar]
- [13].Chumpitazi BP, Fishman SJ, Nurko S. Long-term clinical outcome after botulinum toxin injection in children with nonrelaxing internal anal sphincter. Am J Gastroenterol 2009;104:976–83. [DOI] [PubMed] [Google Scholar]
- [14].Patrus B, Nasr A, Langer JC, et al. Intrasphincteric botulinum toxin decreases the rate of hospitalization for postoperative obstructive symptoms in children with Hirschsprung disease. J Pediatr Surg 2011;46:184–7. [DOI] [PubMed] [Google Scholar]
- [15].Koivusalo AI, Pakarinen MP, Rintala RJ. Botox injection treatment for anal outlet obstruction in patients with internal anal sphincter achalasia and Hirschsprung's disease. Pediatr Surg Int 2009;25:873–6. [DOI] [PubMed] [Google Scholar]
- [16].Foroutan HR, Hosseini SM, Banani SA, et al. Comparison of botulinium toxin injection and posterior anorectal myectomy in treatment of internal anal sphincter achalasia. Indian J Gastroenterol 2008;27:62–5. [PubMed] [Google Scholar]


