Abstract
The following report will discuss the diagnosis and management of non-specific abdominal pain in a 77-year-old woman who presented to a district general hospital in South London. CT imaging demonstrated ileo-colic intussusception with free air and fluid indicating perforation. The images of the specimen clearly show the ileal tumour within the intussusception. Thus, the patient underwent an emergency right hemicolectomy and formation of a double-barrelled ileostomy. Histology subsequently confirmed this was secondary to a colonic adenocarcinoma. This case report is unique as it highlights that intussusception in adults is very difficult to accurately diagnose based on clinical features (due to non-specific findings) and even with radiology can be challenging. This is also the first documented case of the site of perforation not being directly involved with the site of intussusception. The perforation site was in fact distal to the intussusception. At the time of surgery, it was noted that the patient had significantly faecal loading up to her rectum. The resulting closed loop was the cause of her perforation.
Keywords: general surgery, radiology, colon cancer
Background
Intussusception is a medical term from the Latin words ‘intus’ meaning within and ‘susceptio’ meaning take up, which came into discussion in the 17th century when the first case was documented by a Dutch physician in 1674.1 The word is used specifically to describe the telescoping of one portion of the intestine within another.
Intussusception can be categorised by the anatomical location of the defect. Enteroenteric intussusception, involving the small bowel only, is seen in half of all cases. The condition is rarely present in adulthood, with only 5% of cases of intussusception occurring in adults which accounts for less than 1% of all cases of bowel obstruction.2 Unlike in the younger population, adults present with vaguer symptoms and therefore diagnosis relies more heavily on imaging than examination alone.
There is a pathological abnormality of the bowel in the majority of adult cases which alters peristalsis and acts as a lead point which increases the likelihood of intussusception, which is in contrast to the cause in paediatric patients which is usually idiopathic. Such abnormalities include, but are not limited to, malignancy, Meckel’s diverticulum, polyps, postoperative adhesions and lipomas. The most common cause is malignancy and therefore definitive management with surgery is the gold standard however diagnosis can only be confirmed intraoperatively or by histological assessment. Perforation, ischaemia and bowel obstruction are life-threatening complications of intussusception however there is limited literature about this particularly in adults due to the rarity of cases.3
Case presentation
A 77-year-old woman who had been admitted under the emergency physicians for community-acquired pneumonia deteriorated acutely with abdominal pain. There was a 6-week history of colicky, centralised abdominal pain in the preceding weeks. She was nauseated and vomiting over the same period. She described a change in bowel habit to diarrhoea three to four times daily. She was tachypnoeic at 24 breaths/min, tachycardic at 120 beats/min and saturating at 99% on 2 L/min of oxygen. She was normotensive and apyrexial. Abdominal examination revealed umbilical and left-sided tenderness only. The abdomen was tympanic and had reduced bowel sounds. There was no organomegaly or hernias and the per-rectal examination revealed an empty rectum.
Investigations
The blood results demonstrated a white cell count of 8×109/L and a C-reactive protein of 203 mg/L. Serial blood gas analysis revealed worsening lactate from 0.6 mmol/L to 3.3 mmol/L even with fluid resuscitation. CT revealed features consistent with an ileocolic intussusception, with free fluid and air surrounding it, in keeping with a localised perforation (figures 1–3).
Figure 1.

CT abdominal pelvis coronal image—colocolic intussusception (red arrow) with surrounding free fluid.
Figure 2.

CT abdominal pelvis axial image—colocolic intussusception (red arrow) with surrounding free fluid.
Figure 3.

CT abdominal pelvis sagittal image—colocolic intussusception (red arrow) with surrounding free fluid.
DIFFERENTIAL DIAGNOSIS
On admission, the working diagnosis was obstructing colonic malignancy with possible perforation. However with the results of the CT report, this was modified to perforated intussusception.
TREATMENT
The patient was immediately commenced on intravenous amoxicillin, metronidazole and gentamicin to cover intra-abdominal sepsis. She was then taken to theatre for an exploratory laparotomy. This revealed a long segment intussusception of the terminal ileum, caecum and ascending colon with a distal perforation in the proximal transverse colon (figures 4–6). The distal colon and rectum were significantly faecally loaded. There was four quadrant-free faecal contamination within the peritoneum. The patient had an extended right hemicolectomy with formation of an end ileostomy and mucous fistula. The patient was transferred to the intensive care unit following which she was managed on a surgical ward. She made an uneventful recovery and was discharged to a nursing home. Histopathological analysis indicated a moderate and poorly differentiated adenocarcinoma arising at the ileocaecal junction. Final staging after CT chest was pT3 pN0 pM0.
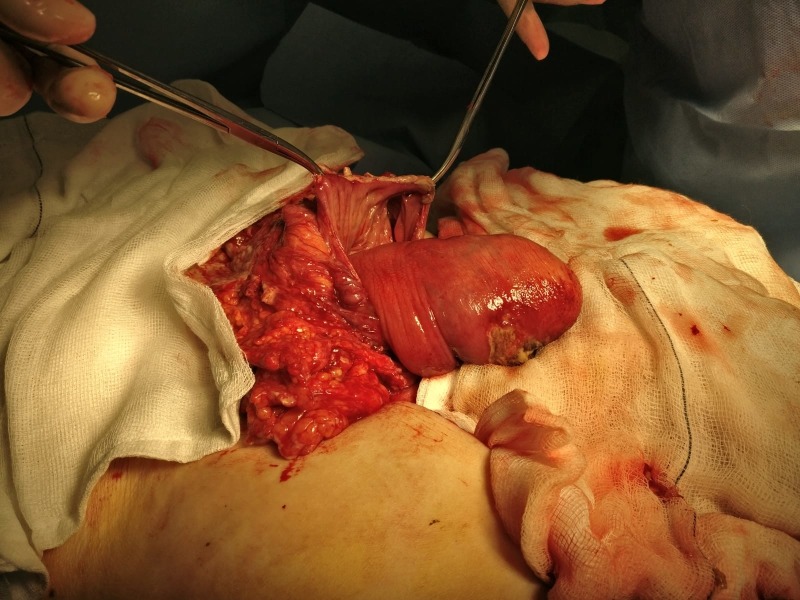
Figure 4.
Intraoperative findings, intussusception perforated through transverse colon (held by haemostats) with necrosis.
Figure 5.

Gross specimen—demonstrating colocolic intussusception into transverse colon.
Figure 6.

Division of intussusception in longitudinal axis demonstrating the tumour.
Outcome and follow-up
Postoperatively, the patient did not engage with medical input, physiotherapy or stoma care. The psychiatric team felt she was suffering from a hypoactive delirium which did not resolve during her stay.
In light of this and taking into account the patient’s comorbidities (including Alzheimer’s dementia, stage 2 chronic kidney disease, bipolar affective disorder and psychosis), a multidisciplinary team decision was made to further manage the patient conservatively and not with chemotherapy.
Of note is that she had a high-output stoma that was finally managed with loperamide, double strength St Mark’s solution and fluid restriction as per protocol. The patient’s discharge was delayed further due to social issues and so she remained in hospital for a total of 5 months. She was finally discharged to a nursing home with regular follow-up.
Discussion
A recently published meta-analysis of 1229 adult patients looked into the causes of intussusception and found the split in aetiology between malignant, benign and idiopathic was 32.9%, 37.4% and 15.1%, respectively.4 The most common site of intussusception overall was within the small bowel. However if the origin was malignant, the majority of cases were located in the colon. The most common method of treating the malignant intussusception was with an en bloc resection to minimise malignant seeding. The overall mortality for this cohort of patients was 5.2%.4 Many inflammatory processes have also been linked to intussusception of the bowel, including; coeliac disease, inflammatory bowel disease, appendicitis, pancreatitis and adenomatous polyps with 5%–16% of cases found to be idiopathic.5 6
The symptoms of intussusception are largely non-specific with the most common being abdominal pain, present in 70%–90% of cases. In addition to pain, rectal bleeding and vomiting are often present which can mimic the symptoms of obstruction.5–7 An abdominal mass can be palpated in between 20% and 40% of cases.7–9 The pain associated with this condition however is often colicky in nature. This non-specific, periodic pain makes diagnosis difficult to achieve where some studies report that less than 50% are diagnosed preoperatively.7 The classical symptoms of; abdominal pain, sausage-shaped abdominal mass and red jelly stools, as described in paediatric textbooks, is rarely seen in the adult population.8 The non-specific nature of presenting pain not only makes diagnosis difficult but may also cause the patient to delay their presentation to healthcare professionals. In fact in the case presented, the patient was having symptoms consistent with intussusception for a number of weeks before her surgery. A study reported that the mean time from onset of symptoms to presentation of confirmed cases of intussusception was 37.5 days.8 9
CT imaging is the mainstay of radiological imaging for intussusception however most patients will initially receive an abdominal radiograph that may show features similar to small bowel obstruction.10 The CT features of intussusception are typically described as a target or ‘sausage’ shaped lesion with surrounding fat stranding.11 CT scanning in cases of intussusception has been reported to have a sensitivity of 71.4%–87.5%.11
The management of intussusception is usually with surgery depending on the likely underlying aetiology. In patients with involvement of the colon and/or over the age of 60, the most appropriate management would be a resection. In contrast, younger patients with known underlying inflammatory conditions such as Crohn’s disease may benefit from a multidisciplinary treatment plan focusing on medical therapies to treat the underlying inflammation as well as limited resection.
This case report is not only unique as it discusses intussusception in an older patient but of note is that it is the first case of a perforation being distinctively separate and distal to the intussusception. The authors noted that at the time of surgery the patient was significantly faecally loaded in the rectum. This led to a closed-loop obstruction limited distally by faecal impaction and proximally by the tumour. The faecal impaction might have slowed peristalsis, thus exacerbating the intussusception and leading to distal perforation. The closed loop ultimately was the cause of the perforation which lead to the patient’s initial presentation.
Learning points.
Intussusception rarely presents in adults. When it does occur in this population the symptoms are non-specific, unlike in paediatric patients.
CT imaging is the gold standard of radiological imaging for the diagnosis of intussusception.
Surgery is the definitive form of management in large intestine intussusception due to the underlying cause being malignancy.
This is the first documented case of the perforation site being separate to the site of intussusception. This may have been due to a closed loop obstruction limited distally by faeces.
Footnotes
Contributors: KL, GJ, CC and DC have contributed to the planning, conduct and reporting of the work described in the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Davis CF, McCabe AJ, Raine PAM. The Ins and outs of intussusception: history and management over the past fifty years. J Pediatr Surg 2003;38:60–4. 10.1016/S0022-3468(03)00080-0 [DOI] [PubMed] [Google Scholar]
- 2.Marinis A, Yiallourou A, Samanides L, et al. . Intussusception of the bowel in adults: a review. World J Gastroenterol 2009;15:407–11. 10.3748/wjg.15.407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Segovia-Lohse HA. Adult intussusception with perforation and secondary peritonitis. Case report. Cir Cir 2011;79:252-55, 274-7. [PubMed] [Google Scholar]
- 4.Hong KD, Kim J, Ji W, et al. . Adult intussusception: a systematic review and meta-analysis. Tech Coloproctol 2019;23:315–24. 10.1007/s10151-019-01980-5 [DOI] [PubMed] [Google Scholar]
- 5.Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg 1997;173:88–94. 10.1016/S0002-9610(96)00419-9 [DOI] [PubMed] [Google Scholar]
- 6.Takeuchi K, Tsuzuki Y, Ando T, et al. . The diagnosis and treatment of adult intussusception. J Clin Gastroenterol 2003;36:18–21. 10.1097/00004836-200301000-00007 [DOI] [PubMed] [Google Scholar]
- 7.Reijnen HAM, Joosten HJM, de Boer HHM. Diagnosis and treatment of adult intussusception. The American 10.1016/0002-9610(89)90309-7 [DOI] [PubMed] [Google Scholar]
- 8.Yalamarthi S, Smith RC. Adult intussusception: case reports and review of literature. Postgrad Med J 2005;81:174–7. 10.1136/pgmj.2004.022749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azar T, Berger DL. Adult intussusception. Ann Surg 1997;226:134–8. 10.1097/00000658-199708000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aref H, Nawawi A, Altaf A, et al. . Transient small bowel intussusception in an adult: case report with intraoperative video and literature review. BMC Surg 2015;15:1–6. 10.1186/s12893-015-0020-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manouras A, Lagoudianakis EE, Dardamanis D, et al. . Lipoma induced jejunojejunal intussusception. World J Gastroenterol 2007;13:3641–4. 10.3748/wjg.v13.i26.3641 [DOI] [PMC free article] [PubMed] [Google Scholar]