Referrals for pediatric TGNC patients increased significantly over 3 years. Referrals were mostly for cross-sex hormones and/or blockers and surgery, and needs varied by age group.
Abstract
OBJECTIVES:
We characterized referral trends over time at a transgender clinic within an integrated health system in Northern California. We identified the transition-related requests of pediatric transgender and gender-nonconforming patients and evaluated differences in referrals by age group.
METHODS:
Medical records were analyzed for all patients <18 years of age in the Kaiser Permanente Northern California health system who were referred to a specialty transgender clinic between February 2015 and June 2018. Trends in treatment demand, demographic data, service requests, and surgical history were abstracted from medical charts and analyzed by using descriptive statistics.
RESULTS:
We identified 417 unique transgender and gender-nonconforming pediatric patients. The median age at time of referral was 15 years (range 3–17). Most (62%) identified on the masculine spectrum. Of the 203 patients with available ethnicity data, 68% were non-Hispanic. During the study period, the clinic received a total of 506 referrals with a significant increase over time (P < .001). Most referrals were for requests to start cross-sex hormones and/or blockers (34%), gender-affirming surgery (32%), and mental health (27%). Transition-related requests varied by age group: younger patients sought more mental health services, and older patients sought hormonal and surgical services. Eighty-nine patients underwent gender-affirming surgeries, mostly before age 18 and most frequently mastectomies (77%).
CONCLUSIONS:
The increase in referrals supports the need for expanded and accessible health care services for this population. The transition-related care of patients in this large sample varied by age group, underscoring the need for an individualized approach to gender-affirming care.
What’s Known on This Subject:
Pediatric patients are presenting to health care settings in increasing numbers for assistance with transition-related needs and mental health issues related to gender incongruence. These patients are at significantly increased risk for developing psychiatric diseases and risk-taking behaviors.
What This Study Adds:
Our findings highlight the growing demand for pediatric transgender and gender-nonconforming care. Patients most often sought medical and surgical interventions and mental health support. Findings underscore the need for expanded access and individualized services for pediatric transgender and gender-nonconforming patients.
Transgender and gender-nonconforming (TGNC) individuals are persons who experience an incongruence between their gender identity and their sex assigned at birth. TGNC persons often experience gender dysphoria, or distress that arises from the discordance between their sex assigned at birth and the gender with which they identify. Persons can identify on the masculine spectrum (eg, transmasculine), on the feminine spectrum (eg, transfeminine), or as gender nonbinary. Although the exact number of transgender individuals is unclear, a recent meta-analysis suggests a global prevalence of 4.6 per 100 000 individuals.1
Although the visibility of transgender persons and awareness of transgender health issues are increasing, this marginalized population faces health inequities. Transgender persons have higher rates of psychopathology such as depression, anxiety, suicidality, and self-harm compared with the general population.2–6 In addition, transgender persons often have poorer health outcomes that stem from social and structural factors such as homelessness, poverty, discrimination, and negative health care experiences.7–9
A weakness of transgender research is that studies have predominantly focused on the adult population. Clinical reports suggest that the number of pediatric TGNC patients presenting to health care settings has increased in the last decade,10,11 yet most studies have focused on psychiatric and medical comorbidities.12–14 One study evaluating psychological outcomes documented how children who were supported in their gender identity had comparable levels of depression as their cisgender (nontransgender) peers.15 Gender-affirming health services, such as cross-sex hormones and gender-affirming surgery, can have a protective effect on healthy development and can significantly reduce dysphoria and improve psychological functioning.13,16–19
The first study describing the demographics of pediatric TGNC patients in the United States was published in 2012 by Spack et al.12 Since this study, there has been evidence highlighting various changes in TGNC pediatric patient demographics and health care needs.10,11,14,20 Despite the rapidly evolving landscape of TGNC patient care, there is a scarcity of recent research examining the demand for and use of gender-affirming services among pediatric TGNC patients. To help expand health care capacity and inform service delivery, it is critical to understand the unique health care needs of this population. In this study, we characterized referral patterns over time at a specialty transgender clinic in Northern California, identified the types of transition-related services that TGNC children and their families most commonly sought, and evaluated differences in referrals by age group. Because insurance coverage and awareness of gender-affirming procedures have increased in recent years, we also characterized the number of patients who completed gender-affirming surgery either before or over the course of the study period.
Methods
Setting and Patients
Kaiser Permanente Northern California (KPNC) is a large, integrated health care system that serves >4.2 million members. In 2013, KPNC opened a specialty clinic in Oakland, California, as a referral hub for transition-related services for TGNC members throughout Northern California. Patients could be referred by any health care provider or by self-referral. A nurse coordinator completed intake for each referral via telephone and triaged patients to the KPNC facility closest to the patient’s home that had the appropriate services. To ensure culturally competent care, patients were triaged only to health care providers who were known to the clinic as transgender knowledgeable. Decisions around gender-affirming medical and surgical interventions were guided by a patient-directed care model informed by the World Professional Association for Transgender Health Standards of Care.2,21
Data Collection and Analysis
In February 2015, a pediatric referral database was established to track TGNC patients who were <18 years of age at the time of referral. All patients in this age group who were referred to the TGNC specialty clinic between February 2015 and June 2018 were included in this analysis. Age at referral, date of referral, sex assigned at birth, gender identity, and reasons for referral were abstracted from the pediatric referral database. Patients could have multiple referrals over the study period. We categorized referrals on the basis of the most common services that patients and their families requested: puberty suppression and/or cross-sex hormones; gender-affirming surgery; mental health assessment and/or treatment; or other, which included requests for facial hair removal, voice therapy, assistance with legal name change, and general resources. Mental health services included assessment for medical (eg, cross-sex hormones) and surgical interventions as well as ongoing therapy. Gender-affirming surgeries included mastectomy, hysterectomy, vaginoplasty, facial feminization surgery, phalloplasty and/or metoidioplasty, and mammoplasty. Referral categories were not mutually exclusive because each referral could include requests for multiple services (eg, patients could request to start cross-sex hormones, meet with a mental health provider, and start the process for gender-affirming surgery). Demographic information and surgical history were derived from the KPNC electronic health record. Information on ethnicity was only available with respect to whether the patient was non-Hispanic, and this information was available for 48.7% (n = 203) of the patient cohort. A smaller set of patients had additional ethnic information in their health record. However, this information was not included in our analysis because it was not standardized and was deemed to have uncertain significance in representing ethnic variation of the patient population.
Data were analyzed by using descriptive statistics. Testing of the linear trend in the number of referrals by year was done by orthogonal contrasts. Differences in services requested by age groups were evaluated by using χ2 tests. Analyses were completed by using Stata 14 (Stata Corp, College Station, TX). Study procedures were approved by the KPNC Institutional Review Board.
Results
Patient characteristics are described in Table 1. Between February 2015 and June 2018, 417 unique patients were referred to the clinic. The median age at time of first referral was 15 years (range 3–17), and 73% were assigned female sex at birth. Among all patients (N = 417), 62% identified on the masculine spectrum, 24% identified on the feminine spectrum, and 13% identified as gender nonbinary. The majority (44 of 56) of patients who identified as nonbinary were assigned female sex at birth. Gender identity was not available for 2 patients. Information on ethnicity was available for 203 patients, of whom 68% (n = 139) identified as non-Hispanic.
TABLE 1.
Characteristics of Pediatric Patients Referred to a Specialty Pediatric Transgender Clinic in Northern California Between February 2015 and June 2018 (N = 417)
| n (%) | |
|---|---|
| Age at first referral, y, median (range) | 15 (3–17) |
| Sex assigned at birth | |
| Male | 114 (27) |
| Female | 303 (73) |
| Gender identitya | |
| Transmasculine | 257 (62) |
| Transfeminine | 102 (24) |
| Gender nonbinary | 56 (13) |
| Ethnicitya | |
| Non-Hispanic | 139 (33) |
| Hispanic | 64 (15) |
| Surgery before age 18 | 57 (14) |
Totals may not add to 100% because of missing data.
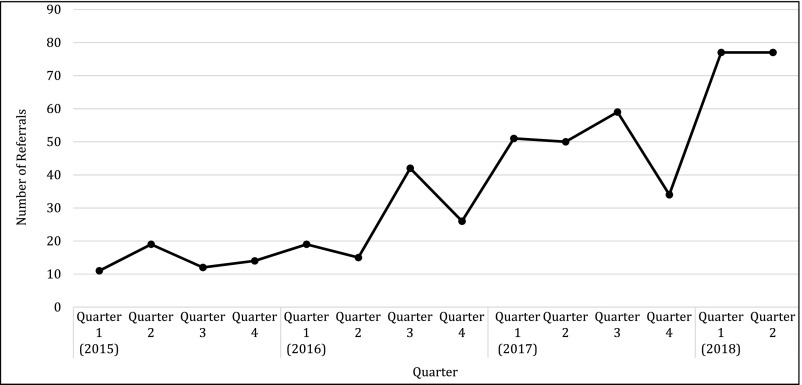
We observed a significant increase in the volume of pediatric referrals between 2015 and 2018 (test of linear trend P <.001). During this period, the clinic received a total of 506 referrals: 56 in 2015, 102 in 2016, 194 in 2017, and 154 in the first 6 months of 2018 (Fig 1). Average monthly referrals increased from 5.1 in 2015 to 25.7 in 2018, an increase of 504%. Of the 506 referrals, ∼34% were for puberty suppression or cross-sex hormones, 32% were for gender-affirming surgery, 27% were for mental health, and 16% were for other services (Table 2). Of the surgery referrals, 85% (139 of 164) were for mastectomy and 10% (17 of 164) were for vaginoplasty.
FIGURE 1.
Number of pediatric patients referred to a specialty transgender clinic in Northern California between February 2015 and June 2018. The volume of referrals increased significantly, from 56 in 2015 to 154 in year-to-date 2018 (linear test of trend P <.001).
TABLE 2.
Pediatric Referrals to a Specialty Transgender Clinic in Northern California Between February 2015 and June 2018 (N = 506)
| Referral Category | n (%) |
|---|---|
| Puberty suppression and/or cross-sex hormones | 173 (34) |
| Gender-affirming surgery | 164 (32) |
| Mental health | 137 (27) |
| Othera | 79 (16) |
| Gender-affirming surgeries requested | |
| Mastectomy | 139 (27) |
| Vaginoplasty | 17 (3) |
| Hysterectomy | 5 (1) |
| Facial feminization surgery | 5 (1) |
| Phalloplasty and/or metoidioplasty | 2 (<1) |
| Mammoplasty | 2 (<1) |
Totals may not add to 100% because of rounding. Categories are not mutually exclusive because patients could request multiple services in a single referral.
Other requests included facial hair removal, voice therapy, assistance with legal name change, and general resources.
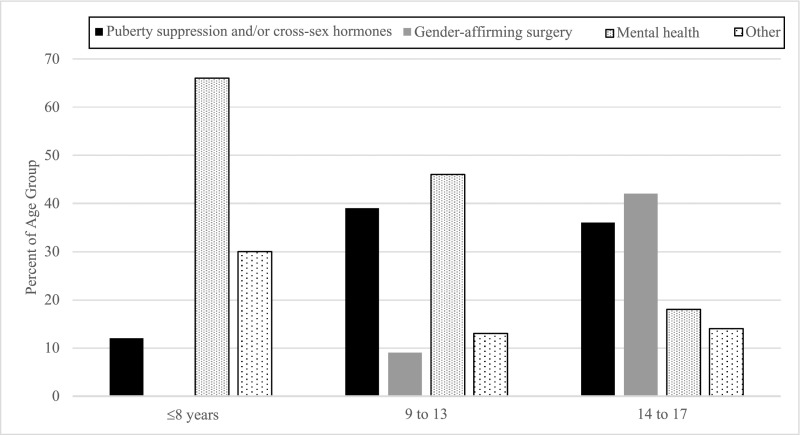
Transition-related services that patients and their families requested varied by age group (P < .001; Fig 2). Patients aged 8 years or younger were referred primarily for mental health services (66%; 33 of 50) and other requests, such assistance with legal name change and general resources (30%; 15 of 50). Most referrals for early adolescent patients between 9 and 13 years of age were for mental health services (46%; 38 of 82) and puberty suppression or cross-sex hormones (39%; 32 of 82). Adolescents aged 14 to 17 years were referred primarily for gender-affirming surgery (42%; 157 of 374). A total of 104 gender-affirming surgeries were documented in the electronic health record involving 89 unique patients (Table 3), of whom 64% (n = 57) had at least 1 surgery before the age of 18.
FIGURE 2.
Services requested varied by age group. Patients aged 8 years or younger were primarily referred for mental health services. Those in early adolescence (9–13 years old) mostly requested mental health services and puberty suppression or cross-sex hormones. The majority of patients in middle adolescence (14–17 years old) were referred for gender-affirming surgery and puberty suppression or cross-sex hormones. Referral categories are not mutually exclusive because patients could request multiple services. P <.001.
TABLE 3.
Gender-Affirming Surgeries Completed in Patients Referred to a Specialty Pediatric Transgender Clinic in Northern California (N = 104)
| n (%) | |
|---|---|
| Mastectomy | 80 (77) |
| Hysterectomy | 9 (9) |
| Vaginoplasty | 7 (7) |
| Facial feminization surgery and/or chondrolaryngoplasty | 4 (4) |
| Phalloplasty and/or metoidioplasty | 2 (2) |
| Mammoplasty | 2 (2) |
Includes those completed at age 18 or older.
Discussion
This study is among the first to evaluate specific transition-related health care needs and surgical use in a large sample of pediatric TGNC patients within an integrated health care system. Between 2015 and 2018, we noted a significant increase in referrals for pediatric patients seeking transition-related care. A large proportion of patients identified on the masculine spectrum, and although a majority of referrals were for medical and surgical transition, patients’ needs varied by age group. We also found that nearly two-thirds of patients referred to undergo phenotypic transition through surgery did so before the age of 18.
The increasing number of pediatric TGNC referrals we observed are reflective of trends described by others over the last decade. In a study involving pediatric TGNC patients at a pediatric endocrinology clinic over 13 years, 74% were referred within the last 3 years.14 Another study of 860 patients referred to a clinic in Amsterdam revealed an average increase in the number of patients referred each year between 1988 and 2016.20 In our cohort, nearly 10% of referrals were for patients 8 years or younger. These trends may reflect changing societal norms and broader acceptance of gender diversity as well as improved availability of TGNC-specific services. Spack et al12 documented a fourfold increase in the number of patients after the creation of a dedicated TGNC clinic in Boston, Massachusetts. The Gender Identity Development Service in the United Kingdom also had a similar growth in referrals for children and adolescents between 2011 and 2017.10 It is likely that as acceptance continues to progress and barriers to care are mitigated, the number of pediatric TGNC patients seeking transition-related care will grow.
We found a higher prevalence of patients who identified on the transmasculine spectrum, which is consistent with previous findings of a predominance of natal females among pediatric TGNC patients.2,10–12,14,20 Our study also reflects the increased rates of patients who identify as gender nonbinary.22 This is a reversal of the adult transgender population, which has been described as a 3:1 ratio of natal-male–to–natal-female individuals.1 The reasons for this shift in the sex ratio are presently unclear. It has been hypothesized that there may be decreased stigma for natal females who behave more typically “male” than for natal males who behave typically “female,” which may lower the barrier to seeking treatment for gender dysphoria.10
Although most referrals were for puberty suppression, cross-sex hormones, and surgery, we noted significant differences in transition-related needs across age groups. Patients 8 years or younger were most often referred for mental health support and other resources, whereas older patients were more likely to be referred for gender-affirming surgery. Patients in early puberty and/or early adolescence were more often referred for mental health and puberty suppression or cross-sex hormones. This finding is supported by literature that describes the development of increased comorbid psychiatric conditions in transgender children and adolescents. Puberty causes the development of secondary sex characteristics specific to a patient’s natal sex, which may cause worsening distress and dysphoria about gender. The burden of this dysphoria may be decreased by delaying puberty.5,15,16 Providers in our clinic initiate hormone blockers and cross-sex hormones when patients have started puberty, which is determined by either a score of 2 on the Tanner Scale during physical examination or laboratory confirmation. Decisions surrounding when to initiate blockers and/or cross-sex hormone therapy are made by the health care team on an individualized, patient-directed basis. The pediatric endocrinologist works in collaboration with the pediatric gender therapist in assessing the patient’s readiness to start medical transition. Age cutoffs are not used, but blocker monotherapy is generally avoided after age 14 because of concerns about effects on bone density.23
Notably, more than one-quarter of all referrals were for mental health services. Our findings support those of previous studies that highlight the importance of providing mental health services to TGNC youth.2,5,15,16 We were unable to collect data on comorbid psychiatric conditions, but others have documented a high prevalence of psychopathology in this population. Studies have found that TGNC youth often have higher rates of depression, anxiety, self-harm, and substance use compared with their cisgender counterparts.2,6,24–26 In a clinic-based sample of transgender youth in Los Angeles, 35% of patients had clinically significant depressive symptoms, 30% attempted suicide at least once, and 43% reported ever using illicit substances.26 The care of TGNC patients is often grounded in mental health providers trained as gender specialists. Beyond psychotherapy to alleviate distress, gender specialists play a critical role in educating patients and their families and in developing appropriate treatment goals, including assessing the appropriateness of medical and surgical transition. Affirmative approaches to care that support a child’s gender identity are essential because many mental health outcomes are likely tied to experiences of rejection and abuse.27,28 When children and adolescents are supported in their identity, mental health outcomes significantly improve.3,5,6,16,27–31
Some patients seek phenotypic transition through gender-affirming surgery. The majority of the of the procedures were for mastectomy, many of which were completed before patients turned 18. Guidelines acknowledge that this procedure may be appropriate in some patients before the age of 18 and do not require a specific time period during which patients should be on cross-sex hormones.21,32 In a study of TGNC patients in the Netherlands, Cohen-Kettenis and van Goozen33 found that patients who underwent gender-affirming surgery before adulthood had highly favorable outcomes. After a median follow-up of >2 years, patients had comparable dysphoria scores as cisgender controls, with many experiencing improved psychological functioning. Similar to decisions around blockers and cross-sex hormone therapy, decisions around gender-affirming surgeries were made by providers in our clinic on an individualized, patient-directed basis over specific age requirements. However, surgical interventions are irreversible and warrant careful consideration. The appropriateness of a patient’s psychological readiness for surgery should be assessed by a gender specialist in conjunction with the patient’s family and other health care providers. Appropriate staff and services are needed to support patients and their families in the decision-making process.
This study has several limitations. We were limited in our ability to capture sufficient information on sociodemographics. This prevented us from evaluating any relevant racial, ethnic, and other demographic variations in our cohort. We were also unable to differentiate between patients referred for puberty suppression and cross-sex hormones. Furthermore, because our data set only included information on the services that patients requested, we were unable to determine if patients ultimately received all the services related to the referral reason. Our use of referral data also limited our analysis to a select subset of individuals who were referred for care. Findings may not reflect the health care needs of TGNC patients who do not present for medical attention. Mental health accounted for a large proportion of the referrals we observed, but we were unable to distinguish whether patients were referred solely for assessment of readiness for medical and/or surgical interventions, for therapy and treatment, or for both. Lastly, all patients at KPNC have medical coverage including benefits for gender-affirming services, so findings may not be generalizable to the broader population of pediatric TGNC patients.
Conclusions
Our findings highlight the growing demand for TGNC care and support the need for expanded and accessible health care services for this medically underserved population. Within a short period of time, the volume of referrals we observed increased by threefold. As demand for TGNC services continues to grow, it will be important that health care providers are trained in the unique needs of TGNC patients so they can provide culturally competent care and help alleviate barriers to gender-affirming treatments. We found that patients and their families sought services around medical, surgical, and mental health interventions at rates that vary by age of the patient. This underscores the value of an individualized approach using a multidisciplinary model that provides colocated medical, surgical, and mental health care services. The findings of this study provide insight into the transition-related needs of pediatric TGNC patients, but more research is needed to identify the best interventions to mitigate dysphoria and improve long-term outcomes.
Acknowledgments
We thank the patients who contributed to our analysis. We also thank the members of the Proud Clinic at Kaiser Permanente Northern California: Yvette Fan, Jillian Goldstein, Lauren B. Hartman, Stephanie Hernandez, Terri Hupfer, Josephine S. Lau, Lisa K. Taylor, Amy Vallerie, and Susanne E. Watson. Thank you also to Miranda Weintraub at Kaiser Permanente Northern California graduate medical education and the Division of Research at Kaiser Permanente Northern California.
Glossary
- KPNC
Kaiser Permanente Northern California
- TGNC
transgender and gender-nonconforming
Footnotes
Dr Hojilla conceptualized and designed the study, designed the data collection instruments, collected data, conducted the initial analyses, and reviewed and revised the manuscript; Dr Handler collected data, conducted analyses, and reviewed and revised the manuscript; Dr Wellenstein collected data and reviewed and revised the manuscript; Ms Varghese collected data, conducted the analysis, and drafted the initial manuscript; Dr Satre provided feedback and revised the manuscript; Dr Zaritsky conceptualized and designed the study, collected data, supervised data collection, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Partly supported by the National Institutes of Health through the National Institute on Drug Abuse (T32 DA007250) and the National Institute on Alcohol Abuse and Alcoholism (K24 AA025703). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Arcelus J, Bouman WP, Van Den Noortgate W, et al. . Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry. 2015;30(6):807–815 [DOI] [PubMed] [Google Scholar]
- 2.Becerra-Culqui TA, Liu Y, Nash R, et al. . Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics. 2018;141(5):e20173845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Durwood L, McLaughlin KA, Olson KR. Mental health and self-worth in socially transitioned transgender youth. J Am Acad Child Adolesc Psychiatry. 2017;56(2):116–123.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diemer EW, Grant JD, Munn-Chernoff MA, Patterson DA, Duncan AE. Gender identity, sexual orientation, and eating-related pathology in a national sample of college students. J Adolesc Health. 2015;57(2):144–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reilly M, Desousa V, Garza-Flores A, Perrin EC. Young children with gender nonconforming behaviors and preferences. J Dev Behav Pediatr. 2019;40(1):60–71 [DOI] [PubMed] [Google Scholar]
- 6.Connolly MD, Zervos MJ, Barone CJ 2nd, Johnson CC, Joseph CLM. The mental health of transgender youth: advances in understanding. J Adolesc Health. 2016;59(5):489–495 [DOI] [PubMed] [Google Scholar]
- 7.Jaffee KD, Shires DA, Stroumsa D. Discrimination and delayed health care among transgender women and men: implications for improving medical education and health care delivery. Med Care. 2016;54(11):1010–1016 [DOI] [PubMed] [Google Scholar]
- 8.Bradford J, Reisner SL, Honnold JA, Xavier J. Experiences of transgender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. Am J Public Health. 2013;103(10):1820–1829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reisner SL, Vetters R, Leclerc M, et al. . Mental health of transgender youth in care at an adolescent urban community health center: a matched retrospective cohort study. J Adolesc Health. 2015;56(3):274–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Graaf NM, Carmichael P, Steensma TD, Zucker KJ. Evidence for a change in the sex ratio of children referred for gender dysphoria: data from the Gender Identity Development Service in London (2000–2017). J Sex Med. 2018;15(10):1381–1383 [DOI] [PubMed] [Google Scholar]
- 11.Aitken M, Steensma TD, Blanchard R, et al. . Evidence for an altered sex ratio in clinic-referred adolescents with gender dysphoria. J Sex Med. 2015;12(3):756–763 [DOI] [PubMed] [Google Scholar]
- 12.Spack NP, Edwards-Leeper L, Feldman HA, et al. . Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics. 2012;129(3):418–425 [DOI] [PubMed] [Google Scholar]
- 13.Wood H, Sasaki S, Bradley SJ, et al. . Patterns of referral to a gender identity service for children and adolescents (1976-2011): age, sex ratio, and sexual orientation. J Sex Marital Ther. 2013;39(1):1–6 [DOI] [PubMed] [Google Scholar]
- 14.Chen M, Fuqua J, Eugster EA. Characteristics of referrals for gender dysphoria over a 13-year period. J Adolesc Health. 2016;58(3):369–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Vries ALC, McGuire JK, Steensma TD, et al. . Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. 2014;134(4):696–704 [DOI] [PubMed] [Google Scholar]
- 16.de Vries ALC, Steensma TD, Doreleijers TA, Cohen-Kettenis PT. Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J Sex Med. 2011;8(8):2276–2283 [DOI] [PubMed] [Google Scholar]
- 17.Dhejne C, Lichtenstein P, Boman M, et al. . Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS One. 2011;6(2):e16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gómez-Gil E, Zubiaurre-Elorza L, Esteva I, et al. . Hormone-treated transsexuals report less social distress, anxiety and depression. Psychoneuroendocrinology. 2012;37(5):662–670 [DOI] [PubMed] [Google Scholar]
- 19.Rotondi NK, Bauer GR, Scanlon K, et al. . Prevalence of and risk and protective factors for depression in female-to-male transgender Ontarians: Trans PULSE Project. Canadian Journal of Community Mental Health. 2012;30(2):135–155 [Google Scholar]
- 20.Steensma TD, Cohen-Kettenis PT, Zucker KJ. Evidence for a change in the sex ratio of children referred for gender dysphoria: data from the Center of Expertise on Gender Dysphoria in Amsterdam (1988–2016). J Sex Marital Ther. 2018;44(7):713–715 [DOI] [PubMed] [Google Scholar]
- 21.Coleman E, Bockting W, Botzer M, et al. . Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgenderism. 2012;13(4):165–232 [Google Scholar]
- 22.Kaltiala-Heino R, Lindberg N. Gender identities in adolescent population: methodological issues and prevalence across age groups. Eur Psychiatry. 2019;55:61–66 [DOI] [PubMed] [Google Scholar]
- 23.Vlot MC, Klink DT, den Heijer M, Blankenstein MA, Rotteveel J, Heijboer AC. Effect of pubertal suppression and cross-sex hormone therapy on bone turnover markers and bone mineral apparent density (BMAD) in transgender adolescents. Bone. 2017;(95):11–19 [DOI] [PubMed] [Google Scholar]
- 24.Reisner SL, Biello KB, White Hughto JM, et al. . Psychiatric diagnoses and comorbidities in a diverse, multicity cohort of young transgender women: baseline findings from Project LifeSkills. JAMA Pediatr. 2016;170(5):481–486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olson-Kennedy J, Okonta V, Clark LF, Belzer M. Physiologic response to gender-affirming hormones among transgender youth. J Adolesc Health. 2018;62(4):397–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olson J, Schrager SM, Belzer M, Simons LK, Clark LF. Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. J Adolesc Health. 2015;57(4):374–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roberts AL, Rosario M, Corliss HL, Koenen KC, Austin SB. Childhood gender nonconformity: a risk indicator for childhood abuse and posttraumatic stress in youth. Pediatrics. 2012;129(3):410–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ryan C, Russell ST, Huebner D, Diaz R, Sanchez J. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nurs. 2010;23(4):205–213 [DOI] [PubMed] [Google Scholar]
- 29.Costa R, Dunsford M, Skagerberg E, et al. . Psychological support, puberty suppression, and psychosocial functioning in adolescents with gender dysphoria. J Sex Med. 2015;12(11):2206–2214 [DOI] [PubMed] [Google Scholar]
- 30.Shumer DE, Nokoff NJ, Spack NP. Advances in the care of transgender children and adolescents. Adv Pediatr. 2016;63(1):79–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olson KR, Durwood L, DeMeules M, McLaughlin KA. Mental health of transgender children who are supported in their identities [published correction appears in Pediatrics. 2018;142(2):e20181436]. Pediatrics. 2016;137(3):e20153223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hembree WC, Cohen-Kettenis PT, Gooren L, et al. . Endocrine treatment of gender-dysphoric/ gender-incongruent persons: an endocrine society clinical practice guideline [published correction appears in J Clin Endocrinol Metab. 2018;103(7):2758–2759]. J Clin Endocrinol Metab. 2017;102(11):3869–3903 [DOI] [PubMed] [Google Scholar]
- 33.Cohen-Kettenis PT, van Goozen SH. Sex reassignment of adolescent transsexuals: a follow-up study. J Am Acad Child Adolesc Psychiatry. 1997;36(2):263–271 [DOI] [PubMed] [Google Scholar]