Summary
Objectives
To investigate the relationship between distance to water source, altitude and active trachoma in children in Rombo district, Tanzania.
Methods
In each of Rombo’s 64 villages, 10 balozis (groups of 8–40 households) were selected at random and all resident children aged 1–9 years were examined for clinical signs of active trachoma. The households of these children and village water sources were mapped using differentially corrected global positioning system data to determine each household’s altitude and distance to the nearest water supply.
Results
We examined 12 415 children and diagnosed 1171 cases of active trachoma (weighted prevalence = 9.1%, 95% CI: 8.0, 10.2%). Active trachoma prevalence ranged from 0% to 33.7% across villages. Increasing distance to the nearest water source was significantly associated with rising trachoma prevalence (age-adjusted odds ratio for infection (OR) for highest quartile compared to lowest = 3.56, 95% CI 2.47, 5.14, P for trend <0.0001). Altitude was significantly inversely associated with trachoma prevalence (age-adjusted OR for highest quartile compared to lowest = 0.55, 95% CI 0.41, 0.75, P for trend <0.0001). These associations remained significant after adjustment in multivariate analysis.
Conclusions
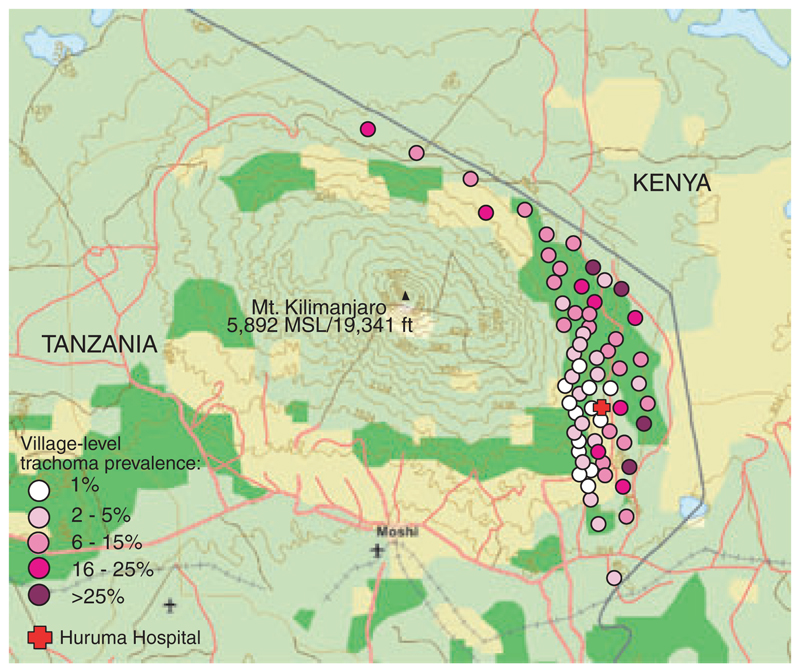
Trachoma is endemic in Rombo district, although the prevalence varies considerably between villages. Spatial mapping is a useful method for analysing risk factors for active trachoma.
Keywords: trachoma, water, altitude, Tanzania, survey
Introduction
Trachoma is the most common infectious cause of blindness (Resnikoff et al. 2004) and results from conjunctival infection with Chlamydia trachomatis. The infection is transmitted from person to person in infected secretions by direct contact, fomites (such as shared cloths and towels), eye-seeking flies and possibly through droplet spread. It is a disease of poor and marginalised people living in hot and dry regions.
Active trachoma is most commonly seen in young children. Its severity and frequency are thought to determine the risk of developing blinding complications later in life (Grayston et al. 1985; Beatty et al. 1994), although host factors are also likely to play a role (Mabey et al. 2003). The development of scarring, thickening of the conjunctiva and distortion of the eyelid may lead to inversion of the eyelashes so that they abrade the eye, leading to corneal opacity and eventual visual impairment or blindness (Grayston et al. 1985).
Lack of water is thought to be a risk factor for trachoma (West et al. 1989; Katz et al. 1996; Schemann et al. 2002) because hygiene practices such as face washing protect against disease (West et al. 1995; Ejere et al. 2004). In Southern Malawi (Tielsch et al. 1988), Nepal (West et al. 1989; Katz et al. 1996) and Tanzania (West et al. 1989), prevalence of trachoma was strongly associated with distance, or time taken to walk, to the nearest water supply. This is assumed to be related to the amount of water that individuals can carry home per trip. Cairncross (1999) has suggested that up to a particular threshold the distance or time to water source does not affect the amount of water brought into the household or its subsequent use, while above this level, distance to water source corresponds with a drop in the amount of water carried.
However, the precise role that water plays in transmission remains to be defined (Emerson et al. 2000). McCauley et al found that perceptions regarding the amount of water available and household priorities for water use, rather than the actual amount of water brought into the home, were the primary determinants of the cleanliness of children’s faces (McCauley et al. 1990,1992).
It therefore appears that it is mainly water use which affects trachoma transmission (West et al. 1989; Bailey et al. 1991), and this is related to water supply. To protect against trachoma, water must be used to improve hygiene, by washing faces and potential fomites. When water access is poor, face- and hand-washing decline (Gilman et al. 1993).
The relationship between trachoma and altitude has not previously been investigated. The prevalence of other infectious diseases, such as malaria, is related to altitude (Ellman et al. 1998), probably due to the decline in insect density at higher altitudes (Siziya et al. 1997; Bodker et al. 2003) and the temperature dependence of the parasite’s developmental cycle in the mosquito (Macdonald 1957; Attenborough et al. 1997). Since flies are mechanical vectors of ocular C. trachomatis (Emerson et al. 2004; Miller et al. 2004), a similar relationship between altitude and prevalence may exist for trachoma. Population density may also fall at higher altitude, and this is related to trachoma transmission (Mabey & Fraser-Hurt 2002).
The aim of this study was to investigate the relationship between distance to water source and altitude and active trachoma in children in Rombo district, Tanzania.
Methods
Rombo district contains 64 villages, each with 1500–9500 residents. We undertook a survey of all 64 villages between June and October 2002. For each village 10 balozis (groups of 8–40 households) were selected at random. All children aged 1–9 years resident in selected balozis were eligible for participation.
After collecting information on age, gender, educational attainment and ethnicity, each child was examined for clinical signs of trachoma by a trained trachoma grader, using binocular loupes (× 2.5) and the ‘WHO simplified system’ (Thylefors et al. 1987). With this system, ‘active trachoma’ is defined as the presence of TF (trachomatous inflammation – follicular) and/or TI (trachomatous inflammation – intense) in either eye. The occurrence of one or more flies making contact with the eyelid margin or tissue internal to the lid margin during the time taken to prepare for examination and examine the child (‘fly-eye’) was also recorded.
Good inter-observer agreement between examiners for clinical signs of trachoma was confirmed by comparing independent diagnoses on the same sets of children (k statistics for TF and TI each >0.80).
The geographical position of each household was recorded using a Trimble roving receiver device (Trimble Navigation Ltd, CA, USA). Water sources were located by questioning residents and their geographical positions recorded. Global Positioning System (GPS) data were differentially corrected using GPS Pathfinder Office (version 2.80, Trimble Navigation Ltd), at the Trimble reference station of the Joint Malaria Project, Kilimanjaro Christian Medical Centre, Moshi, Tanzania. For Kwalakamu village, more detailed information on households, such as housing type and roof type and on ‘crowding’ (mean number of individuals of all ages per bedroom for each household), was also collected.
Ethical approval for the project was granted by the ethics committees of the Kilimanjaro Christian Medical Centre and the London School of Hygiene & Tropical Medicine. Written informed consent was obtained from the parent or guardian of each enrolled child. Verbal consent to take GPS readings and gather attribute information on physical structures was obtained from each household head.
Children with active trachoma were supplied with a 6 weeks course of twice-daily 1% tetracycline eye ointment. Each community was provided with information regarding prevention of trachoma.
Statistical analysis
Maps were produced using ArcMap (version 3.1, Environmental Systems Research Institute), which also calculated straight-line distances from households to nearest water source. We assumed that villagers travelled to the nearest (by straight-line distance) water source.
Data were analysed using STATA version 8.0. Logistic regression was performed using the svy estimation commands for sample-survey data, to adjust for our sampling scheme and clustering of cases within households. Strata were villages, primary sampling units were balozis and sampling weights were ratios of village size to number of children sampled for each village.
For the subanalysis of Kwalakamu village the svy commands were again used, but only primary sampling units (balozis) were specified.
Results
About 5599 households contained eligible children. We interviewed respondents from 5587 (99.8%); for the remainder no responsible adult could be found, or the householder declined to participate. Of 12 545 children aged 1–9 years resident in these households, 12 415 (99.0%) were examined. The remaining 130 eligible children were either not traced at school or at home, or parental consent for ocular examination was refused. Of the 5587 households participating, 4901 were successfully mapped (87.7%). The primary reasons for households not being mapped were limitations of GPS equipment (location or weather preventing reading of satellite signals), and incorrect recording of household numbers. No household refused consent for mapping.
Among 12 415 children examined there were 1171 cases of active trachoma (unweighted district-level prevalence = 9.4%, 95% CI 8.9%, 9.9%, weighted prevalence = 9.1%, 95% CI 8.0%, 10.2%). Prevalence in individual villages varied substantially, ranging from 0.0% to 33.7% (Figure 1).
Figure 1.
Rombo district, Tanzania, showing the prevalence of active trachoma in children aged 1–9 years, by village. Background World Basemap from http://www.geographynetwork.com courtesy of ESRI. Copyright© ESRI. All rights reserved.
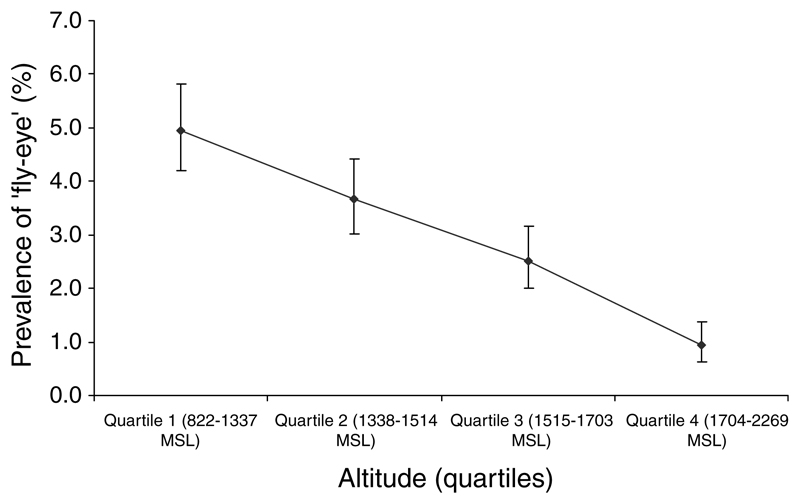
Prevalence of active trachoma decreased strongly with increasing age, but there was no relationship with gender (Table 1). Prevalence was substantially higher in Masai than in other ethnic groups. Children with a fly on their eye (‘fly-eye’-positive) were significantly more likely to have active trachoma (age-adjusted OR 3.98, 95% CI 2.98, 5.31). Prevalence of ‘fly-eye’ positivity was inversely correlated with altitude (Figure 2).
Table 1. Table showing the relationship between demographic characteristics and active trachoma.
| No. active trachoma cases | Number | Weighted† prevalence of active trachoma (95% CI) | Age-adjusted OR (95% CI) | |
|---|---|---|---|---|
| Overall | 1171 | 12 415 | 9.1% (8.0–10.2) | – |
| Age | ||||
| 1 year | 192 | 1338 | 13.8% (11.4–16.1) | 1.00 |
| 2 and 3 years | 433 | 2968 | 14.6% (12.5–16.6) | 1.07 (0.86–1.33) |
| 4 and 5 years | 269 | 2727 | 9.2% (7.7–10.7) | 0.63 (0.51–0.79) |
| 6 and 7 years | 174 | 2984 | 5.5% (4.3–6.7) | 0.37 (0.28–0.47) |
| 8 and 9 years | 100 | 2369 | 4.1% (3.1–5.1) | 0.27 (0.20–0.35) P for trend <0.0001 |
| Gender | ||||
| Male | 596 | 5739 | 9.3% (7.9–10.6) | 1.00 |
| Female | 575 | 5504 | 9.0% (7.8–10.1) | 1.07 (0.86-1.33) |
| Ethnicity | ||||
| Chagga | 1015 | 11 296 | 8.9% (7.8–10.1) | 1.00 |
| Kamba | 7 | 54 | 14.7% (3.9–25.5) | 1.79 (0.75-4.24) |
| Masai | 13 | 32 | 42.9% (30.9–54.9) | 6.99 (3.58–13.67) |
| Mpare | 76 | 497 | 14.1% (10.0–18.2) | 1.62 (1.12–2.35) |
| Msambaa | 33 | 294 | 9.1% (5.3–12.9) | 0.97 (0.59–1.57) |
| Other | 27 | 241 | 9.8% (3.8–15.9) | 1.05 (0.51–2.14) |
| Presence of ‘fly-eye’‡ | ||||
| No | 1062 | 12 072 | 8.4% (7.4–9.5) | 1.00 |
| Yes | 109 | 342 | 31.9% (25.9–37.9) | 3.98 (2.98–5.31) |
Refers to sampling weights, relating to number of children sampled per village and village size.
‘Fly-eye’ is defined as contact with the eyelid margin or tissue internal to the lid margin during the time taken to prepare for examination and examine the child. OR, Odds ratio.
Figure 2.
Relationship between altitude and the prevalence of ‘fly-eye’ in Rombo district, Tanzania. MSL, metres above sea level. Error bars are 95% confidence intervals.
There was a strong and highly significant association between active trachoma and distance to nearest water source (Table 2), which remained after adjustment for confounders (Table 3 – adjusted OR for last quartile compared to first = 2.99, 95% CI 2.09, 4.28). There was a statistically significant inverse association between active trachoma and altitude (Table 2), which remained after adjustment for confounders (Table 3 – adjusted OR for last quartile compared to first = 0.56, 95% CI 0.41, 0.76).
Table 2. The relationship between household altitude and distance to water and prevalence of active trachoma in 1–9-year-old children in Rombo district, Tanzania.
| No. trachoma cases | n | Weighted† prevalence (95% CI) | Age-adjusted OR (95% CI) | |
|---|---|---|---|---|
| Distance to water quartiles (metres)‡ | ||||
| 1 (0.0–79.0) | 130 | 2761 | 4.1% (2.9–5.3) | 1.00 |
| 2 (79.1–190.5) | 208 | 2760 | 7.0% (5.4–8.6) | 1.79 (1.29–2.47) |
| 3 (190.6–496.1) | 312 | 2756 | 10.9% (9.0–12.9) | 2.83 (2.00–4.01) |
| 4 (496.2–4855.7) | 358 | 2745 | 13.4% (11.1–15.7) | 3.56 (2.47–5.14) |
| Age-adjusted P for trend <0.0001 | ||||
| Altitude quartiles (MSL)‡ | ||||
| 1 (822.2–1337.3) | 371 | 2744 | 14.6% (11.9–17.3) | 1.00 |
| 2 (1337.4–1514.8) | 192 | 2758 | 6.0% (4.4–7.6) | 0.37 (0.26–0.53) |
| 3 (1514.9–1703.8) | 167 | 2755 | 6.0% (4.5–7.4) | 0.36 (0.26–0.50) |
| 4 (1703.9–2268.5) | 278 | 2765 | 9.0% (7.3–10.7) | 0.55 (0.41–0.75) |
| Age-adjusted P for trend <0.0001 | ||||
Refers to sampling weights, relating to number of children sampled per village and village size.
Altitude and distance refer to GPS measurements taken from each child’s household.
OR, odds ratio.
MSL, metres above sea level.
Table 3.
Multivariate adjusted association between household distance to water source, household altitude, age and presence of ‘fly-eye’ and prevalence of active trachoma in 1–9-year-old children in Rombo district, Tanzania
| Multivariate adjusted OR | |
|---|---|
| Distance to water quartiles (metres)‡ | |
| 1 (0.0–79.0) | 1.00 |
| 2 (79.1–190.5) | 1.67 (1.21–2.31) |
| 3 (190.6–496.1) | 2.52 (1.78–3.56) |
| 4 (496.2–4855.7) | 2.99 (2.09–4.28) |
| P for trend | <0.001 |
| Altitude quartiles (MSL)‡ | |
| 1 (822.2–1337.3) | 1.00 |
| 2 (1337.4–1514.8) | 0.40 (0.28–0.56) |
| 3 (1514.9–1703.8) | 0.42 (0.30–0.60) |
| 4 (1703.9–2268.5) | 0.56 (0.41–0.76) |
| P for trend | <0.001 |
| Age | |
| 1 year | 1.00 |
| 2 and 3 years | 1.05 (0.84–1.31) |
| 4 and 5 years | 0.66 (0.52–0.83) |
| 6 and 7 years | 0.36 (0.28–0.47) |
| 8 and 9 years | 0.29 (0.22–0.38) |
| P for trend | <0.001 |
| Presence of ‘fly-eye’ | |
| No | 1.00 |
| Yes | 3.21 (2.35–4.38) |
Altitude and distance refer to GPS measurements taken from the child’s household.
MSL, metres above sea level.
OR, odds ratio
Subanalysis – Kwalakamu village
Fifty-five cases of active trachoma were identified in children aged 1–9 years from a total of 246 children examined (prevalence = 22.4%, 95% CI 17.2%, 27.6%), which was higher than the weighted whole-district prevalence (9.1%, 95% CI 8.0%, 10.2%). Only age was significantly related to trachoma, although a weak association was evident between crowding and ‘fly-eye’ and active trachoma (Table 4). Prevalence increased with increasing distance to nearest water source and decreased with increasing altitude, although these associations did not reach statistical significance.
Table 4. Examination of potential confounders in Kwalakamu village, Rombo.
| Risk factor | No. trachoma cases | n† | Weighted§ prevalence (%) (95% CI) | Age-adjusted OR (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male | 22 | 118 | 18.6 (10.2–27.1) | 1.00 | ||||
| Female | 33 | 128 | 25.8 (12.3–39.3) | 1.79 (0.63–5.05) | ||||
| Age group | ||||||||
| <2 years | 8 | 29 | 27.6 (7.6–47.6) | 1.00 | ||||
| 2 and 3 years | 23 | 57 | 40.4 (25.9–54.8) | 1.78 (0.62–5.08) | ||||
| 4 and 5 years | 16 | 60 | 26.7 (11.8–41.5) | 0.95 (0.32–2.83) | ||||
| 6–9 years | 8 | 100 | 8.0 (2.5–13.5) | 0.23 (0.07–0.70) | ||||
| P for trend = 0.003 | ||||||||
| Crowding§§ | ||||||||
| 0.00–1.99 | 6 | 42 | 14.3 (0.0–29.6) | 1.00 | ||||
| 2.00–3.99 | 28 | 115 | 24.3 (12.6–36.1) | 1.93 (0.57–6.53) | ||||
| ≥4.00 | 21 | 88 | 23.9 (17.1–30.6) | 1.79 (0.51–6.32) | ||||
| Age-adjusted P for trend = 0.54 | ||||||||
| Number of children under 5 years per household | ||||||||
| 0–1 | 16 | 75 | 21.3 (9.4–33.3) | 1.00 | ||||
| 2 | 31 | 110 | 28.2 (20.8–35.6) | 1.20 (0.57–2.54) | ||||
| ≥3 | 8 | 60 | 13.3 (2.5–24.2) | 0.38 (0.15–0.94) | ||||
| Age-adjusted P for trend = 0.06 | ||||||||
| Presence of ‘fly-eye’ | ||||||||
| No | 43 | 212 | 20.3 (11.0–29.6) | 1.00 | ||||
| Yes | 12 | 34 | 35.3 (20.5–50.1) | 1.44 (0.50–4.13) | ||||
| House type | ||||||||
| Brick and/or wood | 27 | 125 | 21.6 (14.0–29.2) | 1.00 | ||||
| Mud only | 28 | 120 | 23.3 (9.9–36.8) | 1.03 (0.43–2.45) | ||||
| Presence of animals | ||||||||
| Outside house | 11 | 53 | 20.8 (9.4–32.1) | 1.00 | ||||
| Inside house | 41 | 185 | 22.2 (14.4–29.9) | 1.21 (0.67–2.20) | ||||
| No animals owned | 3 | 7 | 42.9 (29.1–56.6) | 3.32 (0.89–12.37) | ||||
| Distance to nearest water source ‡, quartiles (metres) | ||||||||
| 1 (151.9–502.0) | 11 | 54 | 20.4 (1.5–39.2) | 1.00 | ||||
| 2 (502.1–661.8) | 6 | 55 | 10.9 (5.7–16.1) | 0.47 (0.12–1.75) | ||||
| 3 (661.9–842.0) | 15 | 56 | 26.8 (17.8–35.8) | 1.77 (0.48–6.54) | ||||
| 4 (842.1–1235.8) | 17 | 52 | 32.7 (21.8–43.6) | 1.92 (0.54–6.82) | ||||
| Age-adjusted P for trend = 0.03 | ||||||||
| Altitudet ‡, quartiles (MSL) | ||||||||
| 1 (1393.0–1458.8) | 14 | 56 | 25.0 (21.3–28.7) | 1.00 | ||||
| 2 (1458.9–1480.7) | 18 | 54 | 33.3 (25.8–40.8) | 1.76 (1.11–2.80) | ||||
| 3 (1480.8–1591.3) | 7 | 54 | 13.0 (0.0–26.3) | 0.49 (0.13–1.78) | ||||
| 4 (1591.4–1599.3) | 10 | 53 | 18.9 (0.0–42.5) | 0.72 (0.13–3.98) | ||||
| Age-adjusted P for trend = 0.12 | ||||||||
Each risk factor is adjusted for the effect of each other risk factor in the table, plus adjustment for ethnicity and clustering of cases at the household level. Model adjusts for age group (divided as shown), distance to nearest water source and altitude.
Refers to sampling weights, relating to number of children sampled per village and village size.
Measured as number of individuals/number of bedrooms per household.
Total number of individuals does not always equal total number of individuals surveyed due to incomplete information on some variables for some surveyed children.
Altitude and distance refer to GPS measurements taken from the child’s household.
OR, odds ratio.
Discussion
In this cross-sectional survey of children in Rombo we found that the overall prevalence of active trachoma was 9.1% (95% CI 8.0, 10.2%). Prevalence had a strong dose-response relationship with distance to water source, and this association persisted after control for confounders. Prevalence fell with increasing altitude.
The association between active trachoma and distance to water found in this study is consistent with other studies (Marshall 1968; Assaad et al. 1969; West et al. 1989,1996; Cairncross & Cliff 1987; Tielsch et al. 1988; Katz et al. 1996; Hoechsmann et al. 2001). Although the exact reasons for this are debatable, it is widely accepted that the more difficult it is to access water, the higher the trachoma prevalence.
The relationship between altitude and trachoma prevalence has not previously been investigated, but an association is feasible. The prevalence of trachoma may fall with increasing altitude because population density [which is directly associated with trachoma transmission (Mabey & Fraser-Hurt 2002)] decreases, because rainfall increases and water supplies are more reliable at higher altitudes in Rombo (Majule 2003), or because fly densities decrease (Figure 2). Decreasing prevalence with altitude may also occur because (according to local anecdote) households of higher socio-economic status tend to reside higher up the slopes of Mt. Kilimanjaro. Many ‘down-slope’ communities are relatively new, comprising people who have moved from up-mountain because of lack of land, and therefore do not have the cohesiveness of more established villages. An investigation of the relationship between fly density, markers of socio-economic status and altitude in this district would be informative.
The use of spatial analysis has not yet been fully exploited within public health as a whole (Graham et al. 2004), but its application in research of trachoma (Polack et al. 2005) and other infectious diseases (Hay et al. 2001; Brooker 2002; Tatem & Hay 2004) is increasing. While many studies have examined the relationship between distance to water supply and trachoma prevalence, they have had to rely on reports of time to water source, which may be unreliable; GIS provides an alternative approach. This study was large, including more than 12 000 children, and benefited from a very high participation rate in the trachoma survey, minimising selection bias. The simplified WHO grading system is well established and examinations were conducted by experienced graders.
There were several limitations to this study. The trachoma prevalence survey was undertaken approximately 2 months before exposure data were collected. However, the exposures of altitude and distance to water were likely to have been stable over this time period and both exposure and outcome data were collected during the dry season. Only 87% of households had GPS data available. However, since data were absent due to equipment limitations or incorrect recording of household identification numbers, we expect that this was essentially random.
A number of different water sources may have been used by many households. Distance to water source may not directly translate into time to water source, or effort required to obtain water. Distance to nearest water source may therefore be an incomplete measure of the distance travelled to the water source, and this may have resulted in non-differential misclassification of distance to nearest water source, with consequent underestimation of the association with trachoma prevalence.
This study has provided the first evidence for an association between altitude and trachoma prevalence. There are a number of plausible explanations for this, including differences in socio-economic status, water availability and fly density with altitude. This study has also added support to the importance of distance to nearest water source for trachoma transmission.
Acknowledgements
The study was supported by grants from the International Trachoma Initiative and the Wellcome Trust/Burroughs Wellcome Fund. We gratefully acknowledge the support of the village chiefs, village executive officers, mabalozi leaders, parents and children of Rombo and the dedication of the project field teams. We also thank Andrea Le Fevre, James Lewis and Nick Grassly for comments, and Dr Chris Drakeley for his assistance with differential correction of GPS data.
References
- Assaad FA, Maxwell-Lyons F, Sundaresan T. Use of local variations in trachoma endemicity in depicting interplay between socio-economic conditions and disease. Bulletin of the World Health Organization. 1969;41:181–194. [PMC free article] [PubMed] [Google Scholar]
- Attenborough RD, Burkot TR, Gardner DS. Altitude and the risk of bites from mosquitoes infected with malaria and filariasis among the Mianmin people of Papua New Guinea. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1997;91:8–10. doi: 10.1016/s0035-9203(97)90373-4. [DOI] [PubMed] [Google Scholar]
- Bailey R, Downes B, Downes R, Mabey D. Trachoma and water use; a case control study in a Gambian village. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1991;85:824–828. doi: 10.1016/0035-9203(91)90470-j. [DOI] [PubMed] [Google Scholar]
- Beatty WL, Byrne GI, Morrison RP. Repeated and persistent infection with Chlamydia and the development of chronic inflammation and disease. Trends in Microbiology. 1994;2:94–98. doi: 10.1016/0966-842x(94)90542-8. [DOI] [PubMed] [Google Scholar]
- Bodker R, Akida J, Shayo D, et al. Relationship between altitude and intensity of malaria transmission in the Usambara Mountains, Tanzania. Journal of Medical Entomology. 2003;40:706–717. doi: 10.1603/0022-2585-40.5.706. [DOI] [PubMed] [Google Scholar]
- Brooker S. Schistosomes, snails and satellites. Acta Tropica. 2002;82:207–214. doi: 10.1016/s0001-706x(02)00012-8. [DOI] [PubMed] [Google Scholar]
- Cairncross S. Trachoma and water. Community Eye Health/International Centre for Eye Health. 1999;12:58–59. [PMC free article] [PubMed] [Google Scholar]
- Cairncross S, Cliff JL. Water use and health in Mueda, Mozambique. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1987;81:51–54. doi: 10.1016/0035-9203(87)90280-x. [DOI] [PubMed] [Google Scholar]
- Ejere H, Alhassan M, Rabiu M. Face washing promotion for preventing active trachoma. Cochrane Database of Systematic Reviews. 2004;3:CD003659. doi: 10.1002/14651858.CD003659.pub2. (Online) [DOI] [PubMed] [Google Scholar]
- Ellman R, Maxwell C, Finch R, Shayo D. Malaria and anaemia at different altitudes in the Muheza district of Tanzania: childhood morbidity in relation to level of exposure to infection. Annals of Tropical Medicine and Parasitology. 1998;92:741–753. doi: 10.1080/00034989858989. [DOI] [PubMed] [Google Scholar]
- Emerson PM, Cairncross S, Bailey RL, Mabey DC. Review of the evidence base for the ‘F’ and ‘E’ components of the SAFE strategy for trachoma control. Tropical Medicine and International Health. 2000;5:515–527. doi: 10.1046/j.1365-3156.2000.00603.x. [DOI] [PubMed] [Google Scholar]
- Emerson PM, Lindsay SW, Alexander N, et al. Role of flies and provision of latrines in trachoma control: cluster-randomised controlled trial. Lancet. 2004;363:1093–1098. doi: 10.1016/S0140-6736(04)15891-1. [DOI] [PubMed] [Google Scholar]
- Gilman RH, Marquis GS, Ventura G, Campos M, Spira W, Diaz F. Water cost and availability: key determinants of family hygiene in a Peruvian shantytown. American Journal of Public Health. 1993;83:1554–1558. doi: 10.2105/ajph.83.11.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AJ, Atkinson PM, Danson FM. Spatial analysis for epidemiology. Acta Tropica. 2004;91:219–225. doi: 10.1016/j.actatropica.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Grayston JT, Wang SP, Yeh LJ, Kuo CC. Importance of reinfection in the pathogenesis of trachoma. Reviews of Infectious Diseases. 1985;7:717–725. doi: 10.1093/clinids/7.6.717. [DOI] [PubMed] [Google Scholar]
- Hay SI, Rogers DJ, Shanks GD, Myers MF, Snow RW. Malaria early warning in Kenya. Trends in Parasitology. 2001;17:95–99. doi: 10.1016/s1471-4922(00)01763-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoechsmann A, Metcalfe N, Kanjaloti S, et al. Reduction of trachoma in the absence of antibiotic treatment: evidence from a population-based survey in Malawi. Ophthalmic Epidemiology. 2001;8:145–153. doi: 10.1076/opep.8.2.145.4169. [DOI] [PubMed] [Google Scholar]
- Katz J, West KP Jr, Khatry SK, et al. Prevalence and risk factors for trachoma in Sarlahi district, Nepal. The British Journal of Ophthalmology. 1996;80:1037–1041. doi: 10.1136/bjo.80.12.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mabey D, Fraser-Hurt N. Antibiotics for trachoma. Cochrane Database of Systematic Reviews. 2002:CD001860. doi: 10.1002/14651858.CD001860.pub2. (Online1) [DOI] [PubMed] [Google Scholar]
- Mabey DC, Solomon AW, Foster A. Trachoma. Lancet. 2003;362:223–229. doi: 10.1016/S0140-6736(03)13914-1. [DOI] [PubMed] [Google Scholar]
- Macdonald G. The Epidemiology and Control of Malaria. Oxford University Press; London: 1957. [Google Scholar]
- Majule AE. Impacts of Land Use/Land Cover Changes on Soil Degradation and Biodiversity on the Slopes of Mount Kilimanjaro, Tanzania. LUCID (Land Use Change Impacts & Dynamics) Working Paper Series Number 26. 2003 http://www.luci-deastafrica.org/publications/Majule_LUCID_WP26.pdf. [Google Scholar]
- Marshall CL. The relationship between trachoma and piped water in a developing area. Archives of Environmental Health. 1968;17:215–220. doi: 10.1080/00039896.1968.10665216. [DOI] [PubMed] [Google Scholar]
- McCauley AP, Lynch M, Pounds MB, West S. Changing water-use patterns in a water-poor area: lessons for a trachoma intervention project. Social Science and Medicine. 1990;31:1233–1238. doi: 10.1016/0277-9536(90)90129-g. [DOI] [PubMed] [Google Scholar]
- McCauley AP, West S, Lynch M. Household decisions among the Gogo people of Tanzania: determining the roles of men, women and the community in implementing a trachoma prevention program. Social Science and Medicine. 1992;34:817–824. doi: 10.1016/0277-9536(92)90368-z. [DOI] [PubMed] [Google Scholar]
- Miller K, Pakpour N, Yi E, et al. Pesky trachoma suspect finally caught. The British Journal of Ophthalmology. 2004;88:750–751. doi: 10.1136/bjo.2003.038661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polack SR, Solomon AW, Alexander ND, et al. The household distribution of trachoma in a Tanzanian village: an application of GIS to the study of trachoma. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2005;99:218–225. doi: 10.1016/j.trstmh.2004.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnikoff S, Pascolini D, Etya’ale D, et al. Global data on visual impairment in the year 2002. Bulletin of the World Health Organization. 2004;82:844–851. [PMC free article] [PubMed] [Google Scholar]
- Schemann JF, Sacko D, Malvy D, et al. Risk factors for trachoma in Mali. International Journal of Epidemiology. 2002;31:194–201. doi: 10.1093/ije/31.1.194. [DOI] [PubMed] [Google Scholar]
- Siziya S, Watts TE, Mason PR. Malaria in Zimbabwe: comparisons of IFAT levels, parasite and spleen rates among high, medium and lower altitude areas and between dry and rainy seasons. The Central African Journal of Medicine. 1997;43:251–254. [PubMed] [Google Scholar]
- Tatem AJ, Hay SI. Measuring urbanization pattern and extent for malaria research: a review of remote sensing approaches. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2004;81:363–376. doi: 10.1093/jurban/jth124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thylefors B, Dawson CR, Jones BR, West SK, Taylor HR. A simple system for the assessment of trachoma and its complications. Bulletin of the World Health Organization. 1987;65:477–483. [PMC free article] [PubMed] [Google Scholar]
- Tielsch JM, West KP, Jr, Katz J, et al. The epidemiology of trachoma in southern Malawi. The American Journal of Tropical Medicine and Hygiene. 1988;38:393–399. doi: 10.4269/ajtmh.1988.38.393. [DOI] [PubMed] [Google Scholar]
- West S, Lynch M, Turner V, et al. Water availability and trachoma. Bulletin of the World Health Organization. 1989;67:71–75. [PMC free article] [PubMed] [Google Scholar]
- West S, Munoz B, Lynch M, et al. Impact of face-washing on trachoma in Kongwa, Tanzania. Lancet. 1995;345:155–158. doi: 10.1016/s0140-6736(95)90167-1. [DOI] [PubMed] [Google Scholar]
- West SK, Munoz B, Lynch M, Kayongoya A, Mmbaga BB, Taylor HR. Risk factors for constant, severe trachoma among preschool children in Kongwa, Tanzania. American Journal of Epidemiology. 1996;143:73–78. doi: 10.1093/oxfordjournals.aje.a008659. [DOI] [PubMed] [Google Scholar]