Abstract
Objective To define the anatomy pattern and the incidence of Riché-Cannieu anastomosis, that is, median and ulnar communication in the palmar aspect of the hand.
Materials Methods A total of 80 anatomical dissections were performed on 60 hands of 30 cadavers from 1979 to 1982, and on 20 hands from 2012 to 2015. All of these procedures were performed at the Department of Anatomy of our institution. The incidence of Riché-Cannieu anastomosis and the innervation of the thenar muscles were studied.
Results Riché-Cannieu anastomosis was identified in every dissected hand (100%). The extramuscular Riché-Cannieu anastomosis was recorded in 57 hands, and the intramuscular, in 19 hands. The association of extra- and intramuscular Riché-Cannieu anastomoses occurred in four hands. The ulnar component always originated from the deep branch. The anastomotic branch arising from the median nerve originated from the motor thenar branch (recurrent branch) of the median nerve in most of the observations. The median-ulnar double innervation only to the deep head of the flexor pollicis brevis was identified in 29 of 80 hands. The double innervation only of the superficial head of the flexor pollicis brevis was found in 13 hands. In 12 hands, the deep head of the flexor pollicis brevis was absent. The double innervation of the superficial and deep heads of the flexor pollicis brevis occurred in 14 hands. The oblique head of the adductor pollicis received double innervation in 12 hands. The deep head of the flexor pollicis brevis and the oblique head of adductor pollicis were doubly-innervated in nine hands. The transverse head of the adductor pollicis received double innervation in two hands. Double innervation of the deep head of the flexor pollicis brevis and the transverse head of the adductor pollicis were found in one hand.
Conclusion According to the present study, Riché-Cannieu anastomosis should be considered a normal anatomical neural connection, not an anatomical variation. Knowledge of this anastomosis is essential because the presence of such neural communication may result in confusing clinical, surgical, and electromyographic findings in cases of median or ulnar damage or entrapment.
Keywords: neural conduction, median nerve, ulnar nerve, hand/innervation
Introduction
Riché-Cannieu anastomosis (RCA) is a neural connection between the deep branch of the ulnar nerve and branches of the median nerve in the thenar region. Axons derived from these two nerves may intersect and alter the motor innervation of the intrinsic muscles of the hand. The presence of such anastomoses may cause risk of iatrogenic injury during surgical procedures, and also make it difficult to interpret electrophysiological studies in the diagnosis of neuropathies. 1 These anatomical variations must be differentiated from incomplete nerve lesions, since, clinically, the innervation variations of these small muscles are very important in the sense that, even with a complete lesion of the median or ulnar nerves, some of these muscles may or may not be paralyzed, and this may lead to the erroneous conclusion that the nerve did not undergo a complete lesion. 2 Carpal tunnel syndrome, in particular, has been associated with exacerbated or diminished symptoms in the presence of these anastomoses. 3 4 There are three other types of anomalous neural connections between the medial and ulnar nerves in the upper limb: Martin-Gruber anastomosis (in the forearm, it communicates nerve fibers originating from the median nerve that go to the ulnar nerve), Marinacci anastomosis (also called reverse anastomosis of Martin-Gruber) and Berrettini anastomosis (communication between the common digital nerves of the ulnar and median nerves on the palmar surface of the hand).
Multiple aberrant connections between the median and ulnar nerves may occur in different combinations. 5
The RCA was first described by Riché 6 and Cannieu 7 as a palmar anastomosis between the recurrent branch of the median nerve and the deep branch of the ulnar nerve. Although it is generally believed to be present in a large part of the population, the defined parameters of anastomosis are difficult to classify and, thus, not very well described. 8
The cause, nature, incidence, and direction of the nerve fibers that make up the RCA is relatively unknown. It is believed that it can occur by an aberrant development in the early stage of embryogenesis. 9 Due to the similarity with Martin-Gruber anastomosis, a genetic basis was proposed for the development of RCA. Boland et al 9 considered it a family tendency for an autosomal dominant inheritance, and reported the case of a 21-year-old man whose father and brother also had the anastomosis.
The variety of clinical aspects observed in the isolated lesions of the median and ulnar nerves is not in agreement with the classic pattern of innervation of the muscles of the region of the thenar, as described in the classic treatises of anatomy. In the literature, many divergences are presented, which are accentuated when the authors use different methods of investigation, that is, electromyography, clinical examination, selective anesthetic block of the nerves, or anatomical dissections. Clinical reports and electromyographic studies suggest that the thenar muscles (near the anastomosis) may receive double innervation of the medial and ulnar nerves. The aim of the present study was to define the structure, function, incidence of RCA, and its clinical implications.
Materials and Methods
A total of 60y hands of 30 fresh adult cadavers were dissected between 1979 and 1982, and 20 hands between 2011 and 2015, totaling 80 hands. In all cases, both hands were studied. The dissection was performed using a magnifying glass (magnification of 2.5 times), and in the final phase, using a microscope (magnification of 10 to 16 times), to enable the dissection with special attention to the incidence of RCA. The age ranged from 17 to 68 years, and the sex distribution was of 36 men and 4 women. An initial pilot study, which consisted of the dissection of four hands of two fresh cadavers, was conducted so that the authors would become familiar with the anatomy of the palmar region of the hand, and it was not included in the present work. We investigated the anastomosis between the deep branch of the ulnar nerve and branches of the median nerve through the following technique of dissection: an incision proximal to the wrist fold was made in the interval between the radial flexor muscles of the carpus and the long palmar, extended distally in the palm of the hand. The palmar skin, the subcutaneous tissue and the palmar fascia were removed. The superficial and deep flexor tendons were sectioned 2 cm proximally to the flexor retinaculum and flexed distally. The median nerve was identified proximally to the transverse carpus ligament, the ligament was sectioned longitudinally on its ulnar side (damage to the thenar motor branch of the median nerve was avoided), and its branches were dissected distally. The ulnar nerve was also identified in the wrist, proximally to the Guyon canal, and its deep motor branch was followed distally until its communication with branches of the median nerve. The dissection was then performed using a microscope, with a 10 to 16-fold magnification and microsurgical tweezers. The terminal fascicles of these two nerves were dissected on the surface of these muscles or out of the thickness of their muscular mass, and the origin of the fascicles that penetrated the muscular bellies was observed, as well as the presence of a connection between them. Schematic drawings of the pieces were done, which were systematically photographed. The study was approved by the Ethics in Research Committee of Faculdade de Ciências Médicas e da Saúde, Pontifícia Universidade Católica de São Paulo (Committee Opinion no. 2.207.267).
Results
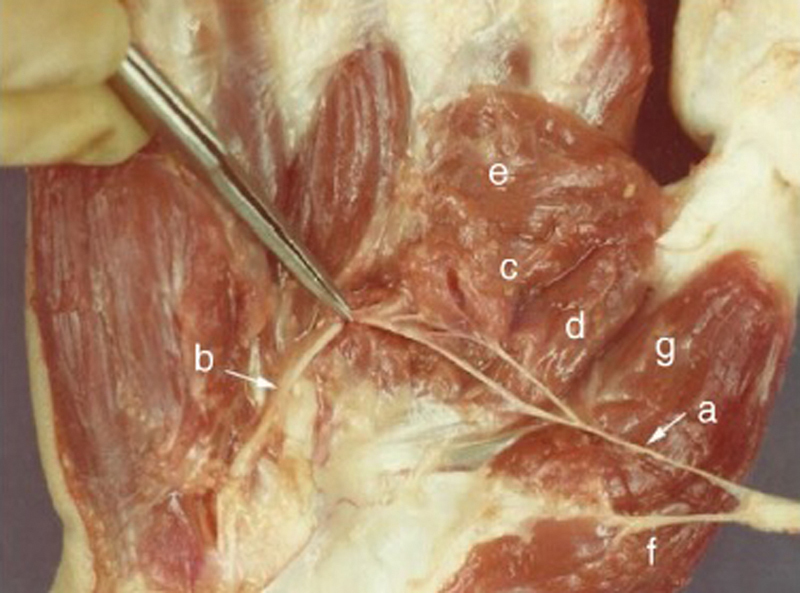
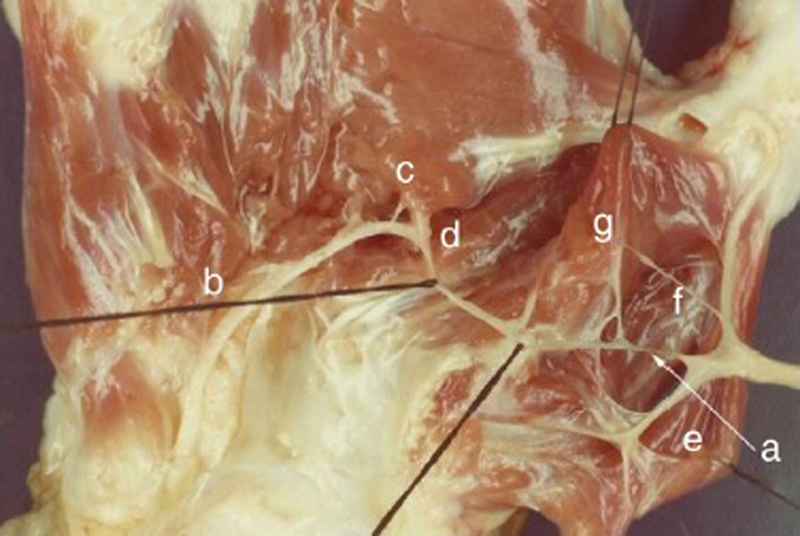
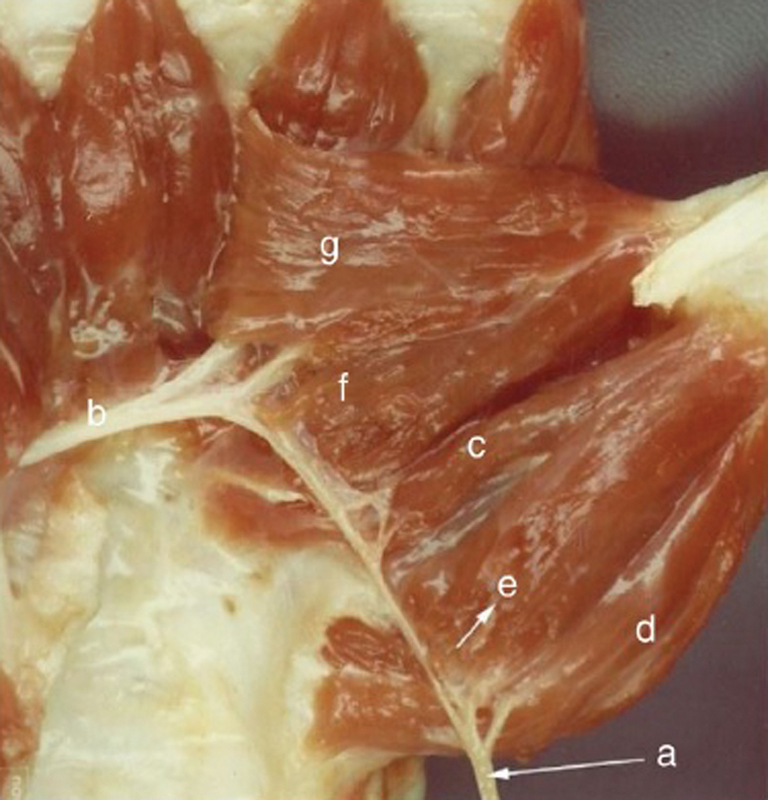
The RCA was identified in all of the 80 dissected hands (100%). In four hands, intra- and extramuscular communication was registered ( Fig. 1 ). Extramuscular RCA was identified in 57 hands ( Fig. 2 3 4 ), and intramuscular RCA, in 19 hands ( Fig. 5 ) ( Table 1 ). In every hand, we observed that the anastomotic branch of the ulnar nerve always originated from its deep branch, after penetrating between the oblique and transverse heads of the adductor muscle of the thumb ( Fig. 1 e 3 ).The anastomotic component of the median nerve was represented by fascicles originating from the recurrent branch of the median nerve in 35 observations ( Fig. 4 ). In 24 hands, the anastomotic fascicles originated from an isolated branch of the main trunk of medial nerve at the point of its division at the distal edge of the transverse carpal ligament ( Fig. 3 ). In 17 hands, the anastomotic branch originated from the radial collateral nerve of the thumb ( Fig. 5 ). In four observations, we identified the anastomotic branch originating from the common digital nerve, which branched into the ulnar collateral nerve of the thumb and radial collateral nerve of the index finger ( Fig. 6 ). In three hands, we identified that the fascicles deriving from the median nerve originated in two different places ( Fig. 7 ). We did not identify the branch of the anastomosis coming from the digital collateral branches of the index finger in our dissections ( Table 2 ). We noted that the branches originating from the median nerve were located laterally and dorsally to the flexor pollicis longus (FPL) tendon, circumvented it, and formed a loop positioned between the tendon and the first metacarpal.
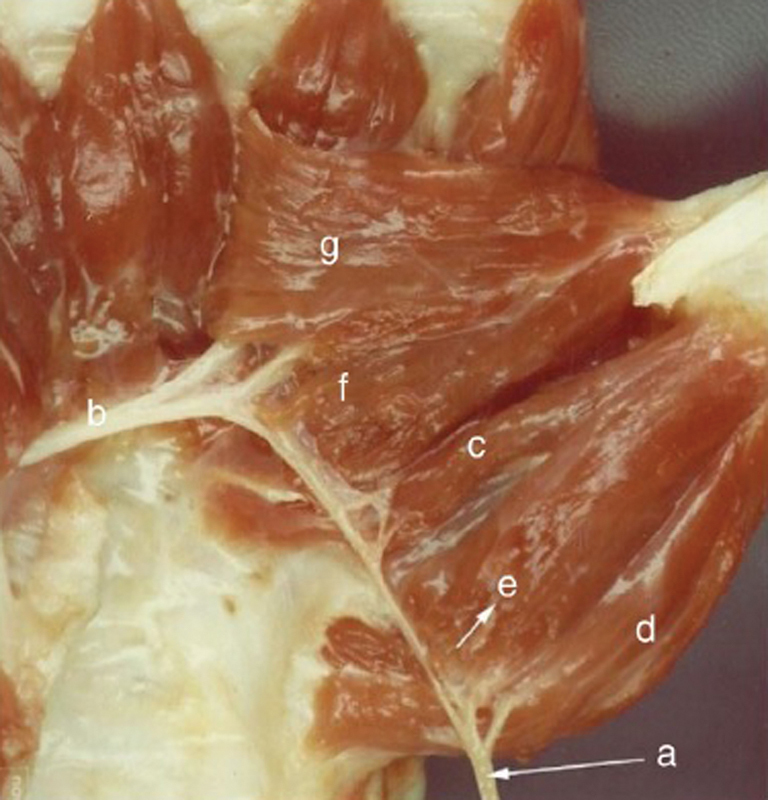
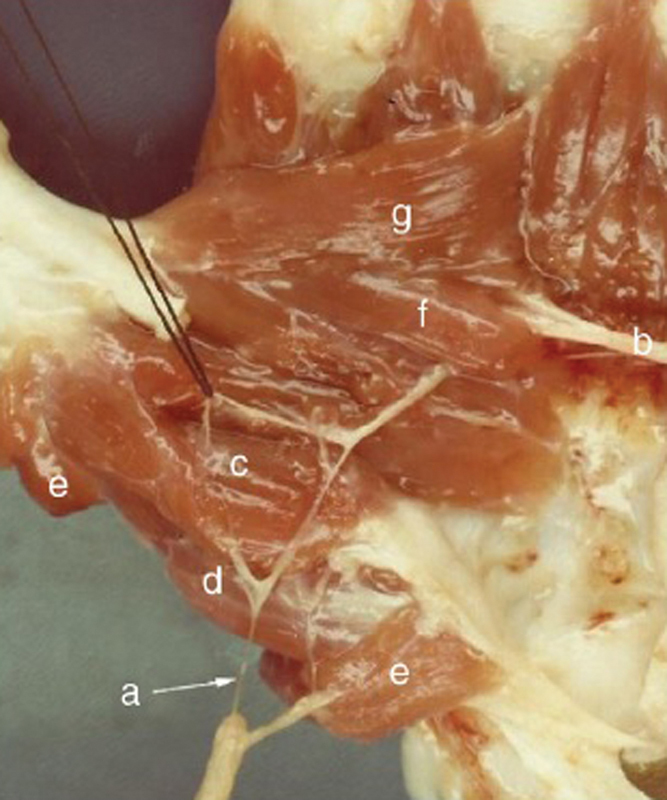
Fig. 1.
( a ) Recurrent branch of the median nerve; ( b ) deep branch of the ulnar nerve; ( c ) deep head of the flexor pollicis brevis (FPB, double innervation); ( d ) abductor pollicis brevis; ( e ) surface head of the FPB; ( f ) oblique head of the adductor pollicis; ( g ) transverse head of the adductor pollicis. Extramuscular anastomosis.
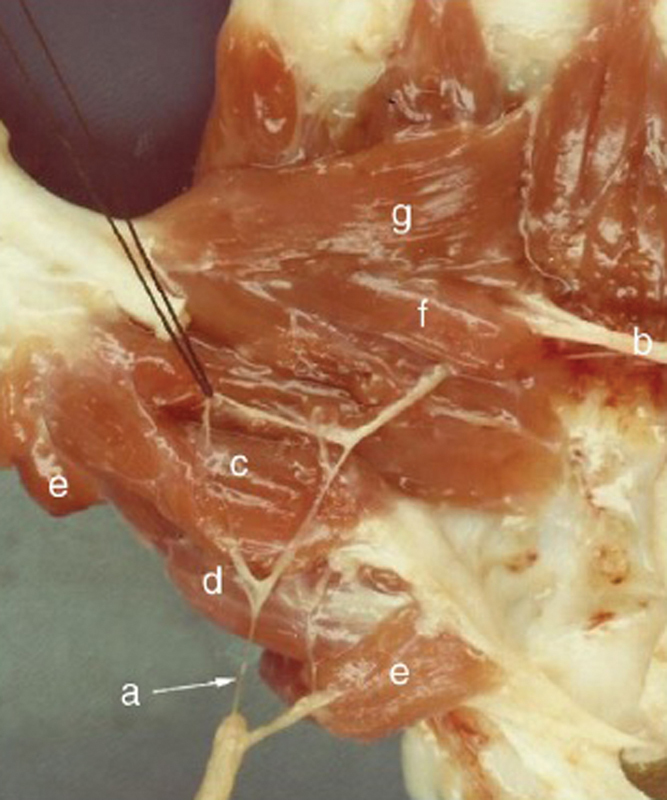
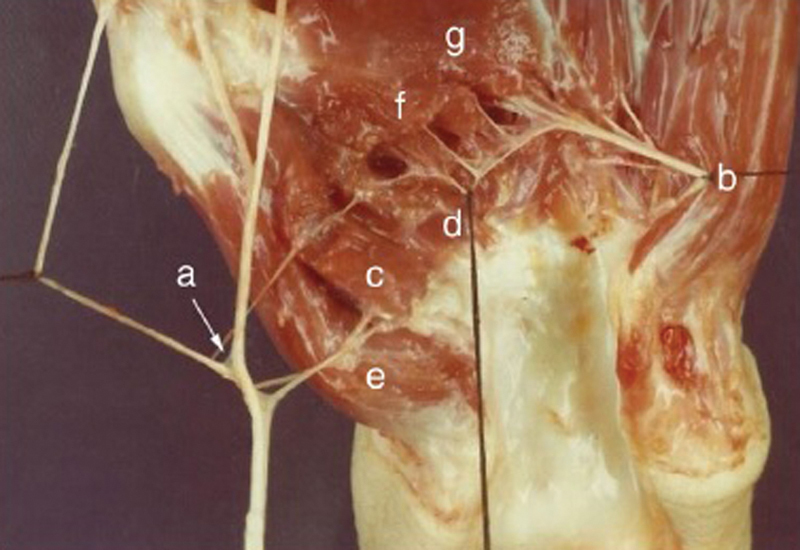
Fig. 2.
( a ) Isolated branch of the median nerve; ( b ) deep branch of the ulnar nerve; ( c ) superficial head of the FPB (double innervation); ( d ) opponent of the thumb; ( e ) abductor pollicis brevis; ( f ), oblique head of the adductor pollicis; ( g ) transverse head of the adductor pollicis. Extramuscular anastomosis.
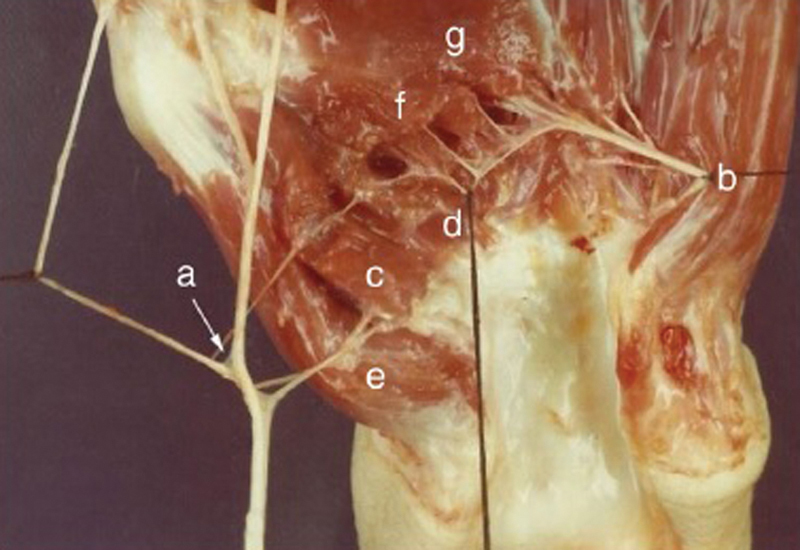
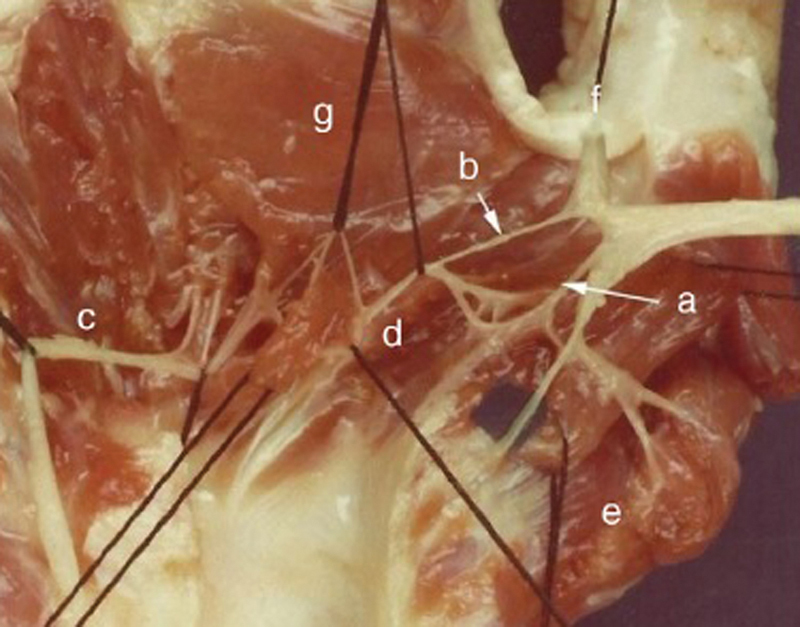
Fig. 3.
( a ) Radial collateral branch of the thumb; ( b ) deep branch of the ulnar nerve; ( c ) superficial head of the FPB (double innervation); ( d ) deep head of the FPB (double innervation); ( e ) adductor pollicis; ( f ) oblique head of the adductor pollicis; ( g ) transversal head of the adductor pollicis. Intramuscular anastomosis.
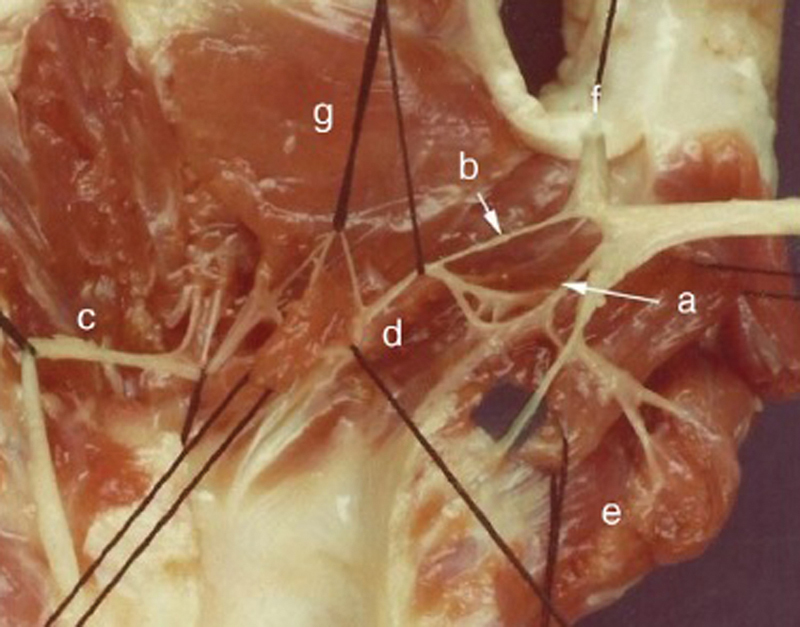
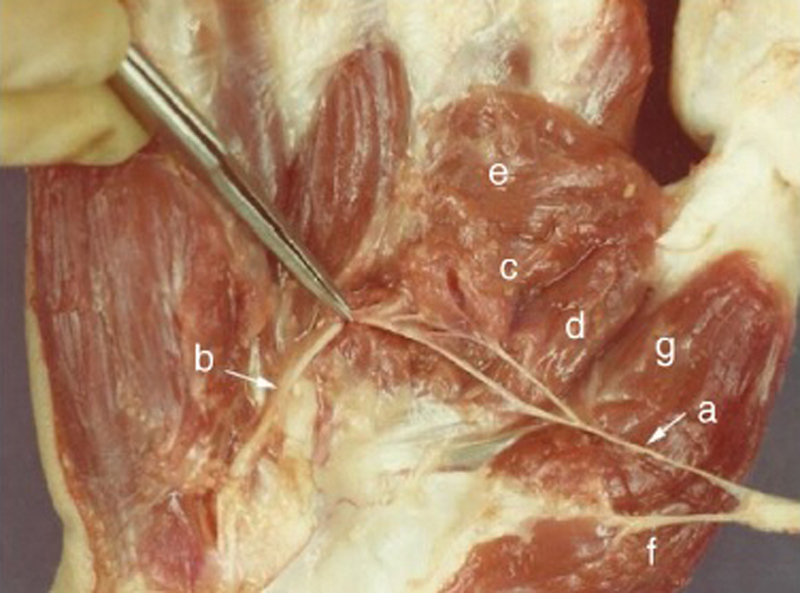
Fig. 4.

( a ) Common digital branch of the median nerve; ( b ) deep branch of the ulnar nerve; ( c ) deep head of FPB (double innervation); ( d ) superficial head of the FPB; ( e ) oblique head of the adductor pollicis (double innervation); ( f ) transverse head of the adductor pollicis. Extramuscular anastomosis.
Fig. 5.
Two branches of the median nerve; ( a ) recurrent branch of the median nerve; ( b ) radial collateral branch of the median nerve; ( c ) deep branch of the ulnar nerve; ( d ) deep head of the FPB (double innervation); ( e ) abductor pollicis brevis; ( f ) oblique head of the adductor pollicis; ( g ) transverse head of the adductor pollicis. Intramuscular anastomosis.
Table 1. Riché-Cannieu anastomosis according to the form of communication.
| Form of communication | Extramuscular | Intramuscular | Intra- and extramuscular | % total |
|---|---|---|---|---|
| Riché-Cannieu anastomosis | 57 (71%) | 19 (24%) | 4 (5%) | 100% |
Fig. 6.

( a ) Recurrent branch of the median nerve; ( b ) deep branch of the ulnar nerve; ( c ) deep head of the FPB (double innervation); ( d ) abductor pollicis brevis; ( e ) surface head of the FPB; ( f ) oblique head of the adductor pollicis; ( g ) transverse head of the adductor pollicis. Intramuscular and extramuscular anastomoses.
Fig. 7.
( a ) Isolated branch of the median nerve; ( b ) deep branch of the ulnar nerve; ( c ) oblique head of the adductor pollicis (double innervation); ( d ) deep head of the FPB; ( e ) transverse head of the adductor pollicis; ( f ) abductor pollicis brevis; ( g ) superficial head of the FPB. Extramuscular anastomosis.
Table 2. Riché-Cannieu anastomosis according to the origin of the nervous branches.
| Origin of the branches | Deep branch of the ulnar nerve | Recurrent branch of the median nerve | Isolated branch of the median nerve | Radial collateral branch of the thumb | First common digital nerve |
|---|---|---|---|---|---|
| Riché-Cannieu anastomosis | 80 (100%) | 35 (44%) | 24 (30%) | 17 (21%) | 4 (5%) |
The median-ulnar double innervation only of the deep head of the flexor pollicis brevis (FPB) muscle was identified in 29 out of 80 hands ( Fig. 1 ), and in 12 hands, the deep head of the FPB was absent ( Figs. 7 and 8 ). The double innervation only of the superficial head of the FPB muscle was found in 13 out of 80 hands ( Fig. 2 ). The double innervation of the superficial and deep heads of the FPB in the same hand was present in 14 cases. The oblique head of the adductor pollicis (AdP) received double innervation in 12 hands. ( Fig. 6 ). The deep head of the FPB muscle and the oblique head of the AdP were doubly innervated in nine hands. The transverse head of AdP received double innervation in two hands ( Fig. 8 ). The double innervation of the deep head of the FPB and the transverse head of the AdP were found in one hand.
Fig. 8.

( a ) Recurrent branch of the median nerve; ( b ) deep branch of the ulnar nerve; ( c ) transverse head ( c ) and oblique ( d ) of the adductor pollicis with double innervation; ( e ) abductor pollicis brevis; ( f ) opponent of the thumb; ( g ) superficial head of the FPB; deep head of the FPB (absent). Intramuscular and extramuscular anastomoses.
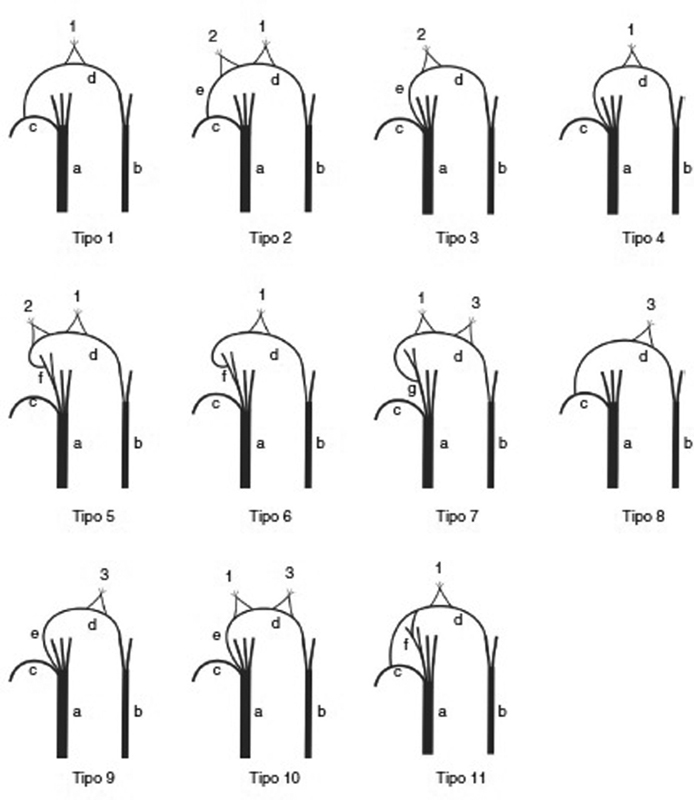
We identified 11 different RCA patterns in the 80 dissected hands ( Fig. 9 ).
Fig. 9.
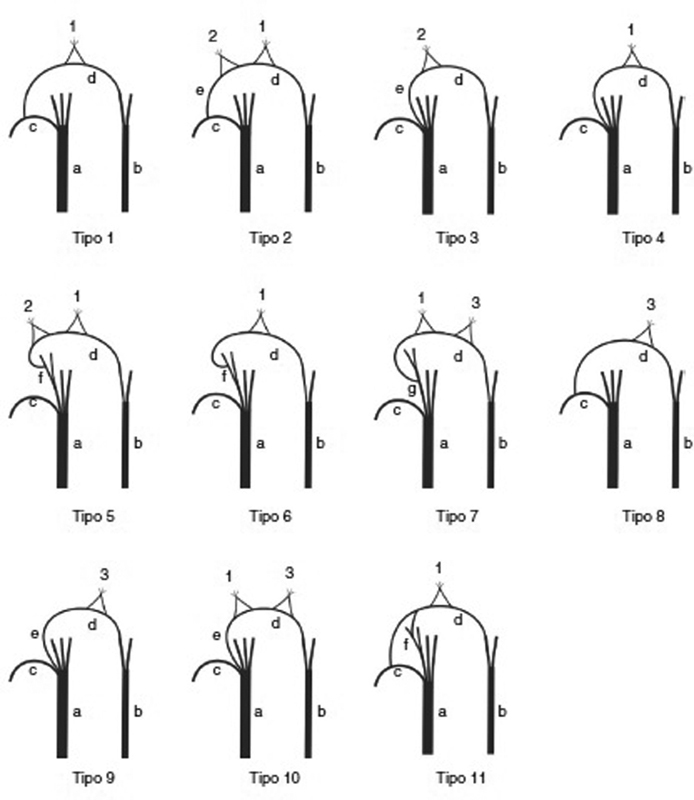
Schematic drawing of the different patterns of the Riché-Cannieu anastomosis. ( 1 ) Branches to the deep head of the FPB muscle; ( 2 ) branches to the superficial head of the FPB; ( 3 ) branches to the adductor muscle of the thumb. ( a ) Median nerve; ( b ) ulnar nerve; ( c ) recurrent branch of the median nerve; ( d ) deep branch of the ulnar nerve; ( e ) branch isolated from the main trunk of the median nerve; ( f ) digital radial collateral branch of the thumb; ( g ) first common digital branch of the median nerve.
Discussion
The incidence of RCA is a controversial issue due to a large discrepancy in the literature regarding prevalence rates. Cannieu 7 dissected 23 hands, and identified the anastomosis in 3 (13%). In the same year, Riché 6 described three types of connections. Type I: between the deep branch of the ulnar nerve and the recurrent branch of the median nerve destined for the two heads of the FPB muscle. Type II: between the deep branch of the ulnar nerve and the median nerve branch, within the muscular body of the transverse head of the AdP muscle. Type III: communication between these two nerves inside the muscular body of the lumbrical muscle. Forrest, 10 in a study combining electromyographic techniques and percutaneous nerve stimulation, concluded that the RCA may be much more common than we can imagine, and highlighted its relationship with the double innervation of the muscles of the thenar region. Harness e Sekeles 11 found RCA in 28 out of 35 dissected hands (77%). Souza 12 dissected 60 hands of corpses prepared in formaldehyde, and found RCA in 30 of them (50%). Kimura et al 13 identified, in an electrophysiological examination, the incidence of 83.3%, after analyzing 150 hands of non-selected participants. Falconer e Spinner 2 found this neural communication in 3 (30%) out of 10 dissected hands ( Table 3 ). Homma e Sakai 14 found RCA in 4 (66.6%) out of 6 dissected hands. Budak et al 15 registered only 1 (3.1%) out of 32 dissected hands. Ajmani 16 dissected 68 hands of 34 cadavers and identified RAC in 13 (18%) hands. Bölükbaşi et al 8 reported that they did not identify RCA in 216 hands of 108 medical students who were evaluated electrophysiologically. Roy et al, 1 in an extensive meta-analysis of nerve communications in the upper limbs, analyzed 501 cases in 6 studies, found a prevalence of 55.5% of RCA, and emphasized that the incidence rate of RCA could be increased if more accurate dissection techniques were used on fresh corpses. According to Yang et al, 5 the RCA was observed in 45 (50%) out of 90 upper limbs of cadavers ( Tablel 3 ). Harness and Sekeles 11 studied 19 laboratory-prepared specimens and 16 hands of fresh corpses, detected RCA in 27 (77.1%) out of 35 hands, and described that it is possible that fibers from the ulnar nerve through this anastomosis were so small that the nerve communication was not detected anatomically. They suggested that RCA could be identified in all dissected hands if more accurate dissecting techniques were used in fresh cadavers, since anastomosis was found in all of the 16 deceased cadavers that were dissected by them. Kimura et al 13 detected anastomosis in 125 (83.3%) out of the 150 hands of 85 unselected volunteer participants, and their results led them to assume that perhaps with more sensitive electrophysiological techniques, such as recording with the needle electrode, an even greater percentage of detection of this nerve connection would be identified. Our findings confirm these assumptions, since we identified this neural communication in all 80 (100%) dissected hands. We reached these results performing dissections in cadavers of newly-deceased persons under optical magnification (surgical microscope with a magnification of 10 to 16 times). In some pieces we identified that the anastomotic branch was so thin that it was only identified with a 16-fold magnification of its visualization, especially when the connection of the nerve fibers occurred within the muscular mass (intramuscular anastomoses). We agree with these authors that the high percentage of anatomical and electrophysiological evidence together with the clinical observations implies that the RCA should be regarded as a normal neural connection, not an anatomical variation.
Table 3. Summary of the literature involving different rates of occurrence of the Riché-Cannieu anastomosis.
| Year | Authors | Type of study | Cases | Riché-Cannieu anastomosis (%) |
|---|---|---|---|---|
| 1897 | Riché 6 | Anatomic | 03 out of 23 | 13 |
| 1971 | Harness and Sekeles 11 | Anatomic | 28 out of 35 | 77 |
| 1975 | Souza 12 | Anatomic | 30 out of 60 | 50 |
| 1983 | Kimura et al 13 | Electrophysiological | 125 out of 150 | 83.3 |
| 1985 | Falconer and Spinner 2 | Anatomic | 03 out of 10 | 30 |
| 1992 | Homma e Sakai 14 | Anatomic | 04 out of 6 | 66.6 |
| 1994 | Budak, Bolukbasi e Ozmenoglu 15 | Anatomic | 01 out of 32 | 3 |
| 1996 | Ajimani 16 | Anatomic | 13 out of 68 | 18 |
| 1999 | Bölükbaşi et al 18 | Electrophysiological | 0 out of 216 | 0 |
| 2016 | Roy et al 1 | Meta-analysis of 501 studies | 278 out of 501 | 55.5 |
| 2016 | Yang et al 5 | Anatomic | 45 out of 90 | 50 |
According to Chevrier, 17 the fascicles from the recurrent branch of the median nerve destined to the anastomosis originated laterally from the tendon of the FPL muscle and, when originating from the digital nerves of the thumb, were positioned medially to the tendon. Souza 12 found the RCA between the deep branch of the ulnar nerve and the recurrent branch of the median nerve in 50% of the cases, and between the deep branch of the ulnar nerve and the digital branches of the median nerve in 50% of the cases, and always laterally to FPL. Falconer and Spinner 2 found the RCA in three cases: in two of them it was positioned laterally and dorsally to the FPL, and the third arose from a separate branch of the median nerve; it was located dorsally and medially to the FPL. We did not identify the branch of the anastomosis from the digital collateral branches of the index finger in our dissections; the branches originating from the median nerve were located laterally to the FPL tendon; they circumvented it and formed a loop, which was positioned between the tendon and the first metacarpal. We recorded in our dissections that the anastomotic component of the median nerve was represented by fascicles originating from the recurrent branch in 35 observations. In 24 hands, the anastomotic fascicles originated directly from the main trunk of median nerve, in an isolated branch at the point of its ramification at the distal edge of the transverse carpal ligament.
In 17 hands, the anastomotic branch originated from the radial collateral nerve of the thumb. In four observations, we identified the anastomotic branch originating from the common digital nerve that branched into the ulnar collateral nerve of the thumb and the radial collateral of the index finger. In three hands, we identified that the fascicles originating from the median nerve did so in two different places. We did not identify the branch of the anastomosis originating from the digital palmar nerves of the index finger in our dissections, as described by Sarikcioglu and Sindel 18 and Paraskevas et al. 19
The double innervation of the thenar muscles suggests the incidence of RCA. Forrest 10 reported that the muscles located near the nerve connection may receive double innervation, and Harness and Sekeles 11 share the same opinion, saying that the terminal motor anastomoses between the median and ulnar nerves may be more frequent than it has been admitted. Our results corroborate these assertions, since we identified the median-ulnar double innervation of the deep head of the FPL muscle in 29 out of 80 hands. The superficial head of the FPL muscle was double-innervated in 13 out of 80 hands. Double innervation of the superficial and deep heads of the FPL in the same hand occurred in 14 cases. The oblique head of the AdP muscle received double innervation in 13 hands. The deep head of the FPL muscle and the oblique head of the AdP in the same hand were double-innervated in nine cases. The transverse head of the AdP received double innervation in three hands.
Communications between the median and ulnar nerves can cause changes in the clinical symptoms, especially in patients with carpal tunnel syndrome, since these variations may exacerbate or attenuate the clinical picture, causing motor and sensory alterations that differ from the usual pattern. Cliffton, 20 with electrophysiological methods, described a case in which all of the intrinsic muscles of the hand were innervated, despite complete injury of the ulnar nerve. He also described another case in which there was complete median nerve injury and all intrinsic muscles were functioning, despite the absence of sensation in the innervation area of the median nerve. In the first situation, all intrinsic muscles received innervation from the median nerve, and, in the second case, from the ulnar nerve. He attributed these variations to Martin-Gruber anastomosis (connection between the median and ulnar nerves in the forearm). However, we consider that this variation described by Cliffton 20 could be caused by RCA because this nervous communication is 3 times more frequent than Martin-Gruber anastomosis, and in the 80 dissected hands in our study, we did not identify any one in which all the muscles were innervated by a single nerve.
Komar et al 21 report a case with complete median nerve injury above the elbow, with incomplete paralysis of the median nerve in the hand and loss of sensation in the territory of sensory innervation of the median nerve. They reported that the electromyographic study suggested that there was transfer of nerve fibers from the ulnar to the median nerve on the forearm. Amoiridis 22 states that, in this case described by por Komar et al, 21 it is not a question of nerve communication in the forearm, since the stimulus in the wrist did not cause a response of the muscles of the thenar region. In this case, the transfer of fascicles from the ulnar to the median nerve likely occurred distally to the wrist by the RCA.
Saperstein and King 23 have described that the RCA can produce clinical and electrodiagnostic findings that confuse the examiner. They reported a case of deep branch neuropathy of the ulnar nerve complicated by the RCA. Its clinical presentation led to an initial diagnosis of motor neuron disease, and, after extensive electrophysiological studies, it became clear that it was ulnar neuropathy associated with RCA. Refaeian et al 3 reported two cases of carpal tunnel syndrome associated with RCA because, despite the absence of median nerve response to the electrophysiological stimulus, their patients had significant preservation of the function of the thenar muscles, without muscular atrophy. The stimulation of the ulnar nerve, both in the wrist and in the elbow, generated compound muscle action potentials that are easy to obtain from the thenar eminence, so they affirm that preservation of function and electrophysiological responses are better explained by the presence of RCA through nerve fibers originating from the ulnar nerve. Tamagawa et al 4 reported the case of a 72-year-old woman with dysesthesias in the left median nerve distribution area, followed by dysesthesias in the right ulnar distribution area. The clinical examination revealed weakness in the intrinsic muscles of the right hand, with atrophy of the thenar and hypothenar ipsilateral muscles, and emphasized that the paradoxical preservation of the left thenar muscles was a clinical challenge.
Through nerve conduction studies, they identified bilateral carpal tunnel syndrome and right cubital tunnel syndrome. Complementary studies with electromyography with needle recording indicated that there were transferences of nerve fibers from the ulnar to the median nerve, that is, RCA. Rovers et al 24 reported a case that presented progressive loss of force in the left hand without sensory changes. There was atrophy of the thenar region and the first dorsal interosseous. A serial electromyographic examination revealed that it was not, as suspected, motor neuron disease, but RCA associated with piso-hamate hiatus syndrome. The authors emphasize that attention is paramount, since the RCA can simulate the disease of the motor neuron.
Conclusion
We identified the RCA in 80 (100%) dissected hands. According to our study, RCA should be considered a normal anatomical neural connection, not an anatomical variation. Knowledge of this anastomosis and its anatomical patterns is essential because the presence of this neural communication can cause confounding clinical, surgical and electromyographic findings in the case of lesions or compressive syndromes of the median or ulnar nerves.
Conflitos de Interesse Os autores declaram não haver conflitos de interesse.
Trabalho desenvolvido na Faculdade de Ciências Médicas e da Saúde, Pontifícia Universidade Católica de São Paulo, Sorocaba, SP, Brasil. Publicado Originalmente por Elsevier Editora Ltda.
Study developed at Faculdade de Ciências Médicas e da Saúde, Pontifícia Universidade Católica de São Paulo, Sorocaba, SP, Brazil. Originally Published by Elsevier Editora Ltda.
Referências
- 1.Roy J, Henry B M, PĘkala P A et al. Median and ulnar nerve anastomoses in the upper limb: A meta-analysis. Muscle Nerve. 2016;54(01):36–47. doi: 10.1002/mus.24993. [DOI] [PubMed] [Google Scholar]
- 2.Falconer D, Spinner M. Anatomic variations in the motor and sensory supply of the thumb. Clin Orthop Relat Res. 1985;(195):83–96. [PubMed] [Google Scholar]
- 3.Refaeian M, King J C, Dumitru D, Cuetter A C. Carpal tunnel syndrome and the Riche-Cannieu anastomosis: electrophysiologic findings. Electromyogr Clin Neurophysiol. 2001;41(06):377–382. [PubMed] [Google Scholar]
- 4.Tamagawa C, Shiga K, Ohshima Y, Tokunaga D, Nakagawa M. [Riche-Cannieu anastomosis and a paradoxical preservation of thenar muscles in carpal tunnel syndrome: a case report] No To Shinkei. 2004;56(01):53–58. [PubMed] [Google Scholar]
- 5.Yang H, Gil Y, Kim S, Bang J, Choi H, Lee H Y. From the brachial plexus to the hand, multiple connections between the median and ulnar nerves may serve as bypass routes for nerve fibres. J Hand Surg Eur Vol. 2016;41(06):648–656. doi: 10.1177/1753193415622760. [DOI] [PubMed] [Google Scholar]
- 6.Riché D.Le nerf cubital et les muscles de l' eminence thenar Bull Mem Soc Anat Paris 1897;•••:251–252. [Google Scholar]
- 7.Cannieu A. Recherche sur l'innervation de l'eminence thenar par le cubital. J Med Mordeaux. 1896:377–379. [Google Scholar]
- 8.Bölükbaşi O, Turgut M, Akyol A.Ulnar to median nerve anastomosis in the palm (Riches-Cannieu anastomosis) Neurosurg Rev 199922(2-3):138–139. [DOI] [PubMed] [Google Scholar]
- 9.Boland R A, Krishnan A V, Kiernan M C. Riche-Cannieu anastomosis as an inherited trait. Clin Neurophysiol. 2007;118(04):770–775. doi: 10.1016/j.clinph.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 10.Forrest W J. Motor innervation of human thenar and hypothenar muscles in 25 hands: a study combining electromyography and percutaneous nerve stimulation. Can J Surg. 1967;10(02):196–199. [PubMed] [Google Scholar]
- 11.Harness D, Sekeles E.The double anastomotic innervation of thenar muscles J Anat 1971109(Pt 3):461–466. [PMC free article] [PubMed] [Google Scholar]
- 12.Souza O M.Contribuição ao estudo da inervação dos musculi hypotenaris et tenaris no homem [tese]São Paulo: Escola Paulista de Medicina;1975
- 13.Kimura I, Ayyar D R, Lippmann S M. Electrophysiological verification of the ulnar to median nerve communications in the hand and forearm. Tohoku J Exp Med. 1983;141(03):269–274. doi: 10.1620/tjem.141.269. [DOI] [PubMed] [Google Scholar]
- 14.Homma T, Sakai T. Thenar and hypothenar muscles and their innervation by the ulnar and median nerves in the human hand. Acta Anat (Basel) 1992;145(01):44–49. doi: 10.1159/000147340. [DOI] [PubMed] [Google Scholar]
- 15.Budak F, Bolukbasi O, Ozmenoglu M. Innervation anomalies in the upper and lower extremities. Norol Bil D. 1994;11(01):61–65. [Google Scholar]
- 16.Ajmani M L.Variations in the motor nerve supply of the thenar and hypothenar muscles of the hand J Anat 1996189(Pt 1):145–150. [PMC free article] [PubMed] [Google Scholar]
- 17.Chevrier G.Note sur l'anastomose de Riché et CannieuBull Mem Soc Anat Paris1904
- 18.Sarikcioglu L, Sindel M. A variant of the Cannieu-Riche communication: case report. Morphologie. 2002;86(273):35–37. [PubMed] [Google Scholar]
- 19.Paraskevas G, Ioannidis O, Martoglou S. Cannieu-Riche anastomosis of the ulnar to median nerve in the hand: case report. Chirurgia (Bucur) 2010;105(06):839–842. [PubMed] [Google Scholar]
- 20.Cliffton E E. Unusual innervation of the intrinsic muscles of the hand by median and ulnar nerve. Surgery. 1948;23(01):12–31. [PubMed] [Google Scholar]
- 21.Kómár J, Szegvári M, Gloviczky Z, Szántó A. [Traumatic section of the median nerve without complete motor paresis: the Martin-Gruber anastomosis (author's transl)] Nervenarzt. 1978;49(12):697–699. [PubMed] [Google Scholar]
- 22.Amoiridis G.Frequency of ulnar-to-median nerve anastomosis[letter]Electromyogr Clin Neurophysiol 199232(4-5):255–256. [PubMed] [Google Scholar]
- 23.Saperstein D S, King R B. Motor neuron presentation of an ulnar neuropathy and Riche-Cannieu anastomosis. Electromyogr Clin Neurophysiol. 2000;40(02):119–122. [PubMed] [Google Scholar]
- 24.Rovers J MP, Brekelmans G JF, Visser L H. Piso-hamate hiatus syndrome in a patient with Riche-Cannieu anastomosis. BMJ Case Rep. 2013;2013:1–5. doi: 10.1136/bcr-2013-008601. [DOI] [PMC free article] [PubMed] [Google Scholar]