ABSTRACT
Dietary modification has been the cornerstone of cardiovascular disease (CVD) prevention since the middle of the last century when the American Heart Association (AHA) first issued recommendations. For the vast majority of that time the focus has been on saturated fat, with or without concomitant guidance for total or unsaturated fat. Over the past few years there has been a renewed debate about the relation between dietary saturated fat and CVD risk, prompted by a series of systematic reviews that have come to what appears to be different conclusions. This triggered a robust discourse about this controversy in the media that in turn has led to confusion in the general public. The genesis of the different conclusions among the systematic reviews has been identified in several studies on the basis of isocaloric substitution analyses. When the data were analyzed on the basis of polyunsaturated fat replacing saturated fat, there was a positive relation between dietary saturated fat and CVD. When the data were analyzed on the basis of carbohydrate replacing saturated fat, there was a null relation between dietary saturated fat and CVD. When the substitution macronutrient was not taken into consideration, the differential effects of the macronutrient substitution went unrecognized and the relations judged as null. The lack of distinction among substituted macronutrients accounted for much of what appeared to be discrepancies. Dietary guidance consistent with replacing foods high in saturated fat with foods high in unsaturated fat, first recommended more than 50 y ago, remains appropriate to this day.
Keywords: dietary fat, cardiovascular disease, saturated fat, monounsaturated fat, polyunsaturated fat, macronutrients, dietary guidelines, total dietary fat, carbohydrate, protein
Introduction
Cardiovascular disease (CVD) is the leading cause of death globally, estimated to account for 32% of total mortality (1). In the United States this translates to 1 of every 3 deaths (2). The direct and indirect costs per year are estimated at approximately $320 billion. Although this number includes healthcare expenditures and lost productivity, it does not account for such factors as diminished quality of life. As with most chronic diseases, prevention is preferable to treatment.
Dietary modification has been the cornerstone of CVD prevention since the middle of the last century when the AHA first issued recommendations (3). For the vast majority of that time the focus has been on saturated fat, with or without concomitant guidance for total or unsaturated fat. Over the past few years there has been a renewed debate about the relation between dietary saturated fat and CVD risk, prompted by a series of systematic reviews that have come to what appears to be different conclusions (4–11). This triggered a robust discourse about this controversy in the media that in turn has led to confusion in the general public. Also triggered appears to be a shift in the perception of the CVD and saturated fat relation that, in turn, has impacted dietary patterns.
Consistent with decades of recommendations to limit dietary saturated fat there was a decline in intake (12). However, prospective observational studies and disappearance data suggest this decline abated, entered a period of relative stability, and is now increasing (13, 14). The trend is of concern because of all dietary factors associated with CVD risk, dietary fat type is considered to be the strongest modifiable factor (1). This guiding principle is reflected in the current recommendation to replace saturated fat with unsaturated fat, primarily polyunsaturated fat, from a range of entities (1, 15–17).
Evolution of Dietary Fat Guidance
Dietary guidelines for Americans
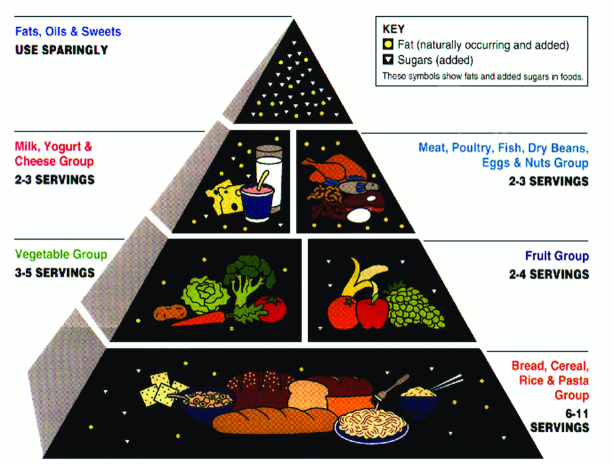
In 1977, the predecessor to the Dietary Guidelines for Americans, the US Dietary Goals, recommended that Americans “Reduce overall fat consumption from approximately 40 to 30% energy intake. Reduce saturated fat consumption to account for about 10% of total energy intake; and balance that with polyunsaturated and monounsaturated fat, which should account for about 10% of energy intake each” (18). Three years later, in 1980, the US Dietary Goals were replaced with the first edition of the Dietary Guidelines for Americans (19). The recommendation was to “Avoid too much fat, saturated fat, and cholesterol.” The second edition of the guidelines, issued in 1985, remained unmodified. The third edition of the guidelines, issued in 1990, shifted the tone but not the substance of the guideline, from negative to positive. The guideline wording was changed to “Choose a diet low in fat, saturated fat, and cholesterol.” In 1992, The US Food Guide Pyramid was released (Figure 1). Dietary fats and oils, grouped with sweets, were placed at the top, the narrowest part of the pyramid, accompanied by the words “Use Sparingly.” It was further specified that this advice included both naturally occurring and added fats and oils. Guidance for dietary fat, in the fourth edition of the guidelines, issued in 1995, remained the same.
FIGURE 1.
Food Guide Pyramid (1992) https://www.choosemyplate.gov/brief-history-usda-food-guides.
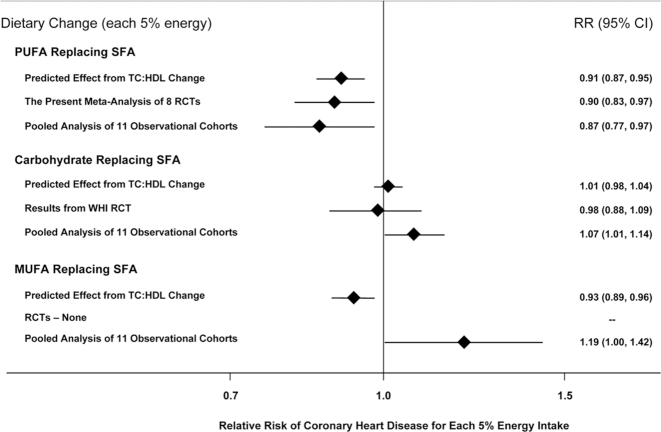
A substantial change in Dietary Guidelines for Americans with regard to dietary fat came in the fifth edition of the guidelines in 2000. The guidance was shifted from limiting total fat to “Choose a diet that is low in saturated fat and cholesterol and moderate in total fat.” This change occurred in response to the growing evidence that limiting dietary total fat promoted dyslipidemia, characterized by high triglyceride and low HDL cholesterol concentrations (20, 21). Nevertheless, consumers drove a demand for low-fat foods and the industry met the demands. This fueled the proliferation of items high in refined carbohydrate such as fat-free salad dressings and reduced-fat peanut butter that had the unanticipated consequence of decreasing unsaturated fat intake (20, 21). In the 2005 sixth edition of the Dietary Guidelines for Americans, the dietary fat guidance was worded somewhat differently and more expansively but was little changed in message. The recommendations were to “Consume less than 10% of calories from saturated fatty acids and less than 300 mg/d of cholesterol, and keep trans fatty acid consumption as low as possible”; “Keep total fat intake between 20 and 35% of calories, with most fats coming from sources of polyunsaturated and monounsaturated fatty acids, such as fish, nuts, and vegetable oils”; “When selecting and preparing meat, poultry, dry beans, and milk or milk products, make choices that are lean, low-fat, or fat-free”; and “Limit intake of fats and oils high in saturated and/or trans fatty acids, and choose products low in such fats and oils.” Around that time, a redesigned version of the Food Guide Pyramid was introduced, termed MyPyramid (Figure 2). It reflected the evolution in dietary fat guideline from low fat to moderate fat by including a separate sector for liquid vegetable oils while specifying preference to choosing lean meat, and non-fat and low-fat dairy products.
FIGURE 2.
Food Guide Pyramid (2005) https://www.choosemyplate.gov/brief-history-usda-food-guides.
Further refining the dietary fat guidance in 2010, the seventh edition of the Dietary Guidelines for Americans advised individuals to “Consume less than 10% of calories from saturated fatty acids by replacing them with monounsaturated and polyunsaturated fatty acids”; “Consume less than 300 mg/d of dietary cholesterol”; “Keep trans fatty acid consumption as low as possible by limiting foods that contain synthetic sources of trans fats, such as partially hydrogenated oils, and by limiting other solid fats”; and “Reduce intake of calories from solid fats and added sugars.” The term “solid fats,” referring to animal fat (diary and meat) and partially hydrogenated fat (shortening and margarine), was only used in the 2010 edition of the Dietary Guidelines for Americans. A year after the 2010 Dietary Guidelines for Americans were issued, the USDA replaced MyPyramid with MyPlate. My Plate initially contained 5 food groups: fruits, vegetables, grains, protein, and dairy (Figure 3).
FIGURE 3.
MyPlate (2011) https://www.choosemyplate.gov/.
The most recent 2015–2020 edition of the Dietary Guidelines for Americans departed from previous approaches with respect to dietary guidance by focusing on dietary patterns rather than individual components or nutrients of the diet. With respect to the major food sources of dietary fat, the guidelines recommended choosing “Fat-free or low-fat dairy, including milk, yogurt, cheese, and/or fortified soy beverages”; “A variety of protein foods, including seafood, lean meats and poultry, eggs, legumes (beans and peas), and nuts, seeds, and soy products”; and “Oils” and limiting “Saturated fats and trans fats, added sugars, and sodium.” However, still retained was the recommendation to limit saturated fat to 10% of energy in the absence of a recommendation for unsaturated fat. Consistent with the 2015–2020 Dietary Guidelines for Americans, the MyPlate website now has added a sixth group to the original 5 (fruits, vegetables, grains, protein, and dairy) – oils, further reinforcing the beneficial effects of liquid vegetable oils in the diet and to discourage the appearance of recommending low-fat diets. The evolution of the Dietary Guidelines for Americans has recently been summarized (22).
National Cholesterol Education Program (NCEP)
In 1988 the NCEP, under the auspices of the National Health, Lung and Blood Institute, introduced the Adult Treatment Panel (ATP) I Step 1 and Step 2 diets (23). Step 1 diet recommendations included limiting fat to <30% of energy, saturated fat to <10% of energy, and cholesterol to <300 mg/d. Step 2 diet recommendations included limiting fat to <30% of energy, saturated fat to <7% of energy, and cholesterol to <200 mg/d. Five years later, in 1993, the ATP II recommendations were updated but the diets remained essentially unchanged (24). In 2001, NCEP issued ATP III recommendations and retired the Step 1 and Step 2 diets. The Therapeutic Lifestyle Change diet was introduced in this version (25). The major change from prior ATP dietary recommendations was a shift from low-fat to moderate-fat intake (25–35% of energy). The recommendations for saturated fat and cholesterol were the same as the prior Step 2 diet; <7% of energy and <200 mg cholesterol/d. No update of the NCEP dietary recommendations has been issued since that time.
AHA
As previously noted, the AHA first issued dietary guidance in 1961, recommending a moderate-fat diet (25–35% of energy as fat), and replacing saturated fat with polyunsaturated fat (3). By the mid-1990s, consistent with the Dietary Guidelines for Americans and ATP I and ATP II diets, the AHA shifted their recommendations to limit total fat, with specific emphasis on saturated fat (26). Four years later there was a further shift in emphasis back to the original recommendation, focusing on replacing saturated fat with unsaturated fat (27). This recommendation was reinforced in 2006 (28). The dietary guidance included recommendations to balance calorie intake and physical activity to achieve or maintain a healthy body weight; consume a diet rich in vegetables and fruits; choose whole-grain, high-fiber foods; consume fish, especially oily fish, at least twice a week; and limit intake of saturated fat to <7% of energy, trans fat to <1% of energy, and cholesterol to <300 mg/d. This guidance was accompanied by recommendations to choose lean meats and vegetable alternatives; select fat-free (skim), 1%-fat, and low-fat dairy products; minimize intake of partially hydrogenated fats; minimize intake of beverages and foods with added sugars; choose and prepare foods with little or no salt; if consuming alcohol, to do so in moderation; and when eating food that is prepared outside of the home, to follow the AHA recommendations.
In 2013, the AHA and American College of Cardiology issued updated dietary pattern recommendations (15). These recommendations replaced those previously issued by NCEP. The recommendations include consume “a dietary pattern that emphasizes vegetables, fruits, and whole-grains; includes low-fat dairy products, poultry, fish, legumes, non-tropical vegetable oils, and nuts; and limits intake of sweets, sugar-sweetened beverages, and red meats.” It was further advised that individuals adapt this dietary pattern to appropriate calorie requirements, personal and cultural food preferences, and nutrition therapy for other medical conditions (including diabetes). For individuals with elevated low density lipoprotein cholesterol concentrations they further recommend “Aim for a dietary pattern that achieves 5% to 6% of calories from saturated fat.”
Major Sources of Fats and Oils in the US Diet
Dietary fats and oils come from both animal and plant sources. The fatty acid profile of dietary fats commonly consumed varies considerably. In general, fats of animal origin tend to be relatively high in saturated fatty acids and are solid at room temperature. Oils of plant origin tend to be relatively high in unsaturated fatty acids (MUFA and PUFA) and are liquid at room temperature. Notable exceptions include plant oils termed tropical oils (e.g., palm, palm kernel, coconut oils), and partially hydrogenated fat. Tropical oils are high in saturated fatty acids but remain liquid at room temperature because they contain a high proportion of SCFA. Partially hydrogenated vegetable oils are relatively high in trans fatty acids because of chemical changes induced during processing and tend to be solid at room temperature.
According to the 2013–2014 NHANES 24-h dietary recall data (29), the 10 major dietary sources of saturated fatty acids in US diets are regular cheese (7.73%), pizza (6.18%), burritos and tacos (4.51%), ice cream and frozen dairy desserts (4.35%), eggs and omelets (3.47%), cookies and brownies (3.19%), cakes and pies (2.98%), reduced 2% fat milk (2.96%), doughnuts, sweet rolls, and pastries (2.72%), and candy containing chocolate (2.61%). The 10 major dietary sources of monounsaturated fatty acids in US diets are nuts and seeds (7.96%), pizza (4.49%), eggs and omelets (3.97%), cheese (3.50%), cakes and pies (3.48%), burritos and tacos (3.36%), chicken (whole pieces 3.32%), cookies and brownies (3.03%), French fries and other fried white potatoes (2.97%), and potato chips (2.47%). The 10 major dietary sources of n–6 PUFA in US diets are nuts and seeds (7.08%), regular salad dressing and vegetable oils (6.87%), tortilla, corn, and other chips (4.14%), pizza (3.97%), eggs and omelets (3.49%), cookies and brownies (3.12%), cakes and pies (3.10%), chicken (whole pieces 2.95%), and mayonnaise (2.80%). The major sources of α-linolenic acid (18:3n–3) are salad dressing and vegetable oils (9.50%), pizza (4.43%), nuts and seeds (3.88%), mayonnaise (3.69%), French fries and other fried white potatoes (3.60%), cakes and pies (3.38%), cookies and brownies (3.24%), burritos and tacos (2.90%), eggs and omelets (2.70%), and pasta mixes dishes except macaroni and cheese (2.56%). The major sources of the n–3 fatty acid EPA are marine fish (45.02%) and shellfish (10.51%), and of DHA are fish (47.48%), and eggs and omelets (16.37%).
Dietary Fat and Cardiovascular Disease: Controversy
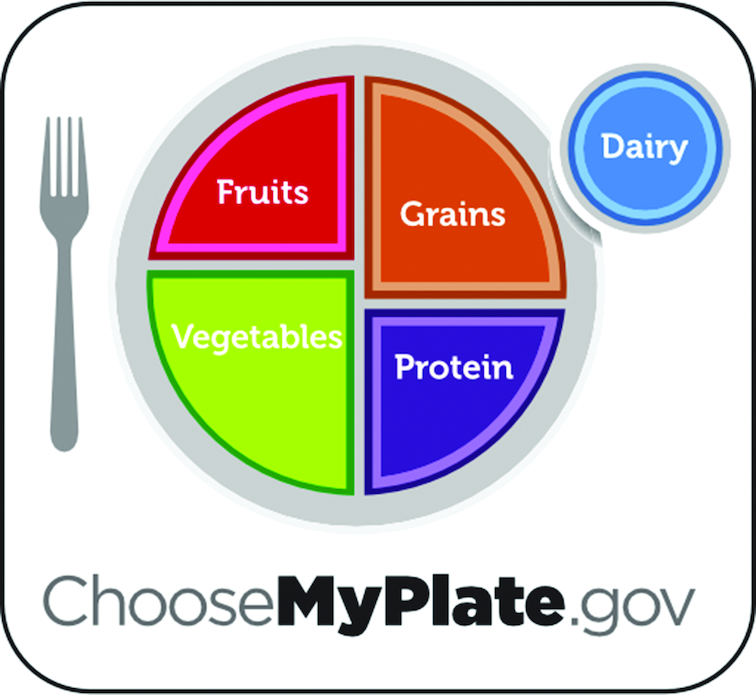
A range of headlines in the news media has elevated the topic of dietary fat and CVD risk, from “Butter is Back” (30) to “Once a Villain, Coconut Oil Charms the Health Food World” (31). These headlines were spawned by a number of relatively recent systematic reviews and meta-analyses that have questioned the relation between saturated fat intake and CVD events and mortality rates (4–7, 9, 10). In contrast, other systematic reviews and meta-analyses published during a similar period concluded that there was a positive association between saturated fat and CVD (1, 5, 8, 11). The difference between these 2 groups of systematic reviews on the topic of dietary fat and CVD risk can be attributed to whether a distinction was made in the data analysis plan between those studies in which the isocaloric replacement nutrient for SFA was PUFA or carbohydrate. This point is best demonstrated in the work based on isocaloric substitution analyses (5, 8, 32, 33). When the data were analyzed on the basis of PUFA replacing SFA, there was a positive relation between dietary SFA and CVD (Figure 4) (1, 8, 11). When the data were analyzed on the basis of carbohydrate replacing saturated fat, there was a null relation between dietary SFA and CVD (4, 6, 7, 9). When the substitution approach was not taken into consideration, the differential effects of the macronutrient substitution went unrecognized and the relations were judged as null. The lack of distinction among substituted macronutrients accounted for much of what appeared to be discrepancies among systemic reviews. Although humans can desaturate some stearic acid (18:0) to form oleic acid (18:1) (34), because the data for dietary fat and CVD are from studies in which foods, rather than purified fatty acids, were consumed, the differential effects of individual SFAs cannot be addressed with the current available data set.
FIGURE 4.
Effects on coronary heart disease risk of consuming PUFA, carbohydrate, or MUFA in place of saturated fatty acids. RCT, randomized controlled trials; TC, total cholesterol. Reproduced from (8).
Dietary Fat and Cardiovascular Disease: Present
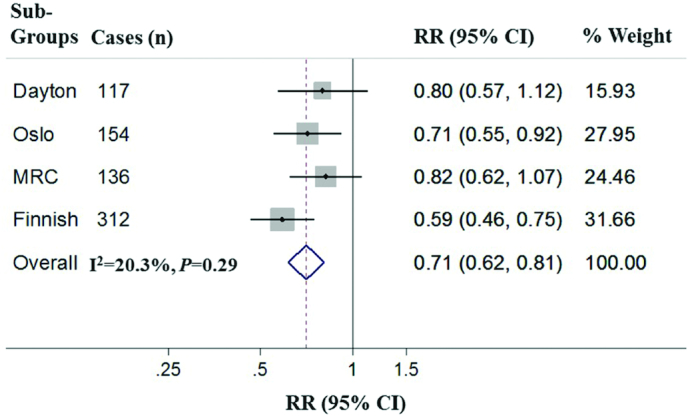
At the end of 2017, the AHA issued a Presidential Advisory entitled “Dietary Fats and Cardiovascular Disease” (1). A thorough review of the literature was conducted and summarized. “Core” studies were identified that meet pre-established criteria. These criteria specified that the trials “compared high saturated with high PUFA; did not include trans unsaturated fat as a major component; controlled the dietary intake of the intervention and control groups; had at least a 2 y sustained dietary intervention period; determined adherence using objective biomarkers (e.g., serum cholesterol or blood or tissue concentration of PUFA); and collected and validated information on cardiovascular or coronary disease events” (1). Four “core” studies met these criteria (35–38). A fixed-effects meta-analysis of the “core” studies demonstrated that replacing saturated fat with vegetable oil (primarily soybean oil) lowered coronary heart disease (CHD) by 29% (Figure 5). Because dietary cholesterol frequently occurs in foods high in saturated fat, it was noted that in many cases when replacing foods high in saturated fat with liquid vegetable oils, dietary cholesterol was reduced. The advisory concluded that the benefits of modifying dietary fat type were likely augmented by the consequent reduction in dietary cholesterol. Six additional “noncore” studies were identified (39–44). These studies were categorized as “noncore” because either SFA was replaced with a combination of PUFA and carbohydrate and/or they had insufficient duration, low adherence, few events, or other serious study design flaws. When these trials are included in meta-analyses, the effect of the “core” trials was somewhat diluted. For example, 2 systematic reviews that included noncore studies reported an overall pooled risk reduction of 19% by replacing SFA with PUFA (8, 9).
FIGURE 5.
Replacement of saturated fat with other types of fat or carbohydrate. Reused from Sacks et al. (1) with permission from the AHA, Inc.
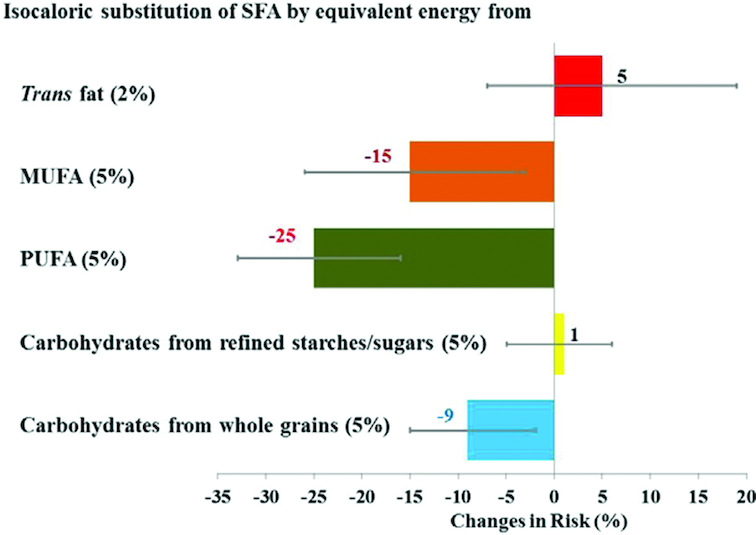
Prospective observational studies were also assessed by the AHA committee (1). A statistical framework for multivariable regression analysis that isolates effects of specific macronutrient exchanges was used to analyze the data (45). Comparisons were made between high SFA intake and high PUFA, MUFA, trans unsaturated fat, or carbohydrate, each independently. Replacement of 5% of energy from SFA with PUFA, MUFA, or unrefined carbohydrate was associated with a significantly lower CHD risk (25%, 15%, and 9%, respectively) (Figure 6) (33). In contrast, replacing saturated fats with refined carbohydrate or sugar was not significantly associated with CHD risk (1% higher incidence).
FIGURE 6.
Meta-analysis of core trials on replacing saturated with polyunsaturated fat. MRC, Medical Research Council. Reproduced from Sacks et al. (1) with permission from the AHA, Inc.
Conclusions
Recommendations for dietary fat have ebbed and flowed over the last half century, particularly with respect to CVD prevention and risk reduction. The majority of the data indicate that replacing food sources of saturated with unsaturated fat, particularly polyunsaturated fat, is associated with lower risk. Replacing food sources of saturated fat with refined carbohydrate has a null effect. Dietary guidance consistent with these conclusions, first formulated more than 50 y ago, remains appropriate to this day.
Acknowledgments
We thank Naglaa H El-Abbadi for analyses of the 2013–2014 NHANES for major sources of dietary fatty acids. AHL wrote, read, and approved the final manuscript.
Notes
Published in a supplement to Advances in Nutrition. This supplement was sponsored by the Harding-Buller Foundation of Ohio. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the sponsors. Publication costs for this supplement were defrayed in part by the payment of page charges. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of Advances in Nutrition.
Supported, in part, by the USDA (agreement No. 58-1950-4-401). Any opinions, findings, conclusions or recommendations expressed in this publication are those of authors, and do not necessarily reflect the view of the USDA.
Author disclosures: The author report no conflicts of interest.
Abbreviations used: ATP, Adult Treatment Panel; CHD, coronary heart disease, CVD, cardiovascular disease; NCEP, National Cholesterol Education Program.
References
- 1. Sacks FM, Lichtenstein AH, Wu JHY, Appel LJ, Creager MA, Kris-Etherton PM, Miller M, Rimm EB, Rudel LL, Robinson JG et al.. Dietary fats and cardiovascular disease. A Presidential advisory from the American Heart Association. Circulation. 2017;136:e1–e23. [DOI] [PubMed] [Google Scholar]
- 2. Benjamin EJ, for the AHA Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics–2017 update: a report from the American Heart Association. Circulation. 2017;135:e1–e458.28028067 [Google Scholar]
- 3. American Heart Association. Dietary fat and its relation to heart attacks and strokes. JAMA. 1961;175, 389–91. [PubMed] [Google Scholar]
- 4. Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659–69. [DOI] [PubMed] [Google Scholar]
- 5. Jakobsen MU, O'Reilly EJ, Heitmann BL, Pereira MA, Bälter K, Fraser GE, Goldbourt U, Hallmans G, Knekt P, Liu S et al.. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009;89(5):1425–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Skeaff CM, Miller J. Dietary fat and coronary heart disease: summary of evidence from prospective cohort and randomised controlled trials. Ann Nutr Metab. 2009;55:173–201. [DOI] [PubMed] [Google Scholar]
- 7. Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr. 2010;91:535–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7:e1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, Franco OH, Butterworth AS, Forouhi NG, Thompson SG et al.. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med. 2014;160:398–406. [DOI] [PubMed] [Google Scholar]
- 10. de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, Uleryk E, Budylowski P, Schünemann H, Beyene J et al.. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ. 2015;351:h3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Clifton PM, Keogh JB. A systematic review of the effect of dietary saturated and polyunsaturated fat on heart disease. Nutr Metab Cardiovasc Diseases. 2017;27(12):1060–80. [DOI] [PubMed] [Google Scholar]
- 12. Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among US adults, 1999–2012. JAMA. 2016;315:2542–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zong G, Li Y, Wanders AJ, Alssema M. Intake of individual saturated fatty acids and risk of coronary heart disease in US men and women: two prospective longitudinal cohort studies. BMJ. 2016;355:i5796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. USDA. Butter and margarine availability over the last century[Internet].2016. Available from: https://www.ers.usda.gov/amber-waves/2016/july/butter-and-margarine-availability-over-the-last-century/. [Google Scholar]
- 15. Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, Lee IM, Lichtenstein AH, Loria CM, Millen BE et al.. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63: 2889–934. [DOI] [PubMed] [Google Scholar]
- 16. Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, Mayer-Davis EJ, Neumiller JJ, Nwankwo R, Verdi CL, Urbanski P et al.. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2014;36:3821–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dietary Guidelines for Americans. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. [Internet]. 2015. Available from: http://health.gov/dietaryguidelines/2015-scientific-report/pdfs/scientific-report-of-the-2015-dietary-guidelines-advisory-committee.pdf. [Google Scholar]
- 18. Dietary Goals for Americans. [Internet]. 1977. Available from: https://health.gov/dietaryguidelines/dga2005/report/HTML/G5_History.htm. [Google Scholar]
- 19. Dietary Guidelines for Americans. 1980 Dietary Guidelines. [Internet]. 1980. Available from: https://health.gov/dietaryguidelines/1980.asp. [Google Scholar]
- 20. Lichtenstein AH, Ausman LM, Carrasco W, Jenner JL, Ordovas JM, Schaefer EJ. Short-term consumption of a low-fat diet beneficially affects plasma lipid concentrations only when accompanied by weight loss. J Arterioscler Thromb. 1994;14(11):1751–60. [DOI] [PubMed] [Google Scholar]
- 21. Lichtenstein AH, Van Horn L. Very low fat diets. Circulation. 1998;98(9):935–9. [DOI] [PubMed] [Google Scholar]
- 22. Jahns L, Davis-Shaw W, Lichtenstein AH, Murphy SP, Conrad Z, Nielsen F. The history and future of dietary guidance in America. Adv Nutr. 2018;9:136–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. [No authors listed]. Report of the National Cholesterol Education Program expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Arch Intern Med. 1988;148(1):36–69. [PubMed] [Google Scholar]
- 24. [No authors listed]. Summary of the second report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in Adults (Adult Treatment Panel II). JAMA. 1993;269(23):3015–23. [PubMed] [Google Scholar]
- 25. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–97. [DOI] [PubMed] [Google Scholar]
- 26. Krauss RM, Deckelbaum RJ, Ernst N, Fisher E, Howard BV, Knopp RH, Kotchen T, Lichtenstein AH, McGill HC, Pearson TA et al.. Dietary guidelines for healthy American adults. A statement for health professionals from the Nutrition Committee, American Heart Association. Circulation. 1996;94(7):1795–800. [DOI] [PubMed] [Google Scholar]
- 27. Krauss RM, Eckel RH, Howard B, Appel LJ, Daniels SR, Deckelbaum RJ, Erdman JW Jr, Kris-Etherton P, Goldberg IJ, Kotchen TA et al.. AHA dietary guidelines: revision 2000: a statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation. 2000;102(18):2284–99. [DOI] [PubMed] [Google Scholar]
- 28. Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B et al.. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96. [DOI] [PubMed] [Google Scholar]
- 29. National Health and Nutrition Examination Survey [Internet]. Available from: https://www.cdc.gov/nchs/nhanes/nhanes_products.htm, accessed 7 March, 2019. [Google Scholar]
- 30. Bittman M. Butter is back [Internet]. 2014. Available from: https://www.nytimes.com/2014/03/26/opinion/bittman-butter-is-back.html. [Google Scholar]
- 31. Clark M. Once a villain, coconut oil charms the health food world [Internet]. 2011. Available from: https://www.nytimes.com/2011/03/02/dining/02Appe.html. [Google Scholar]
- 32. Guasch-Ferré M, Babio N, Martínez-González MA, Corella D, Ros E, Martín-Peláez S, Estruch R, Arós F, Gómez-Gracia E, Fiol M et al.. Dietary fat intake and risk of cardiovascular disease and all-cause mortality in a population at high risk of cardiovascular disease. Am J Clin Nutr. 2015;102(6):1563–73. [DOI] [PubMed] [Google Scholar]
- 33. Li Y, Hruby A, Bernstein AM, Ley SH, Wang DD, Chiuve SE, Sampson L, Rexrode KM, Rimm EB, Willett WC et al.. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: a prospective cohort study. J Am Coll Cardiol. 2015;66(14):1538–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Emken EA, Adlof RO, Rohwedder WK, Gulley RM. Influence of linoleic acid on desaturation and uptake of deuterium-labeled palmitic and stearic acids in humans. Biochim Biophys Acta. 1993;1170(2):173–81. [DOI] [PubMed] [Google Scholar]
- 35. Controlled trial of soya-bean oil in myocardial infarction. Lancet. 1968;2:693–9. [PubMed] [Google Scholar]
- 36. Dayton S, Pearce ML. Prevention of coronary heart disease and other complications of arteriosclerosis by modified diet. Am J Med. 1969;46(5):751–62. [DOI] [PubMed] [Google Scholar]
- 37. Leren P. The Oslo Diet-Heart study: eleven-year report. Circulation. 1970;42(5):935–42. [DOI] [PubMed] [Google Scholar]
- 38. Turpeinen O, Karvonen MJ, Pekkarinen M, Miettinen M, Elosuo R, Paavilainen E. Dietary prevention of coronary heart disease: the Finnish Mental Hospital Study. Int J Epidemiol. 1979;8:99–118. [DOI] [PubMed] [Google Scholar]
- 39. Watts GF, Lewis B, Brunt JN, Lewis ES, Coltart DJ, Smith LD, Mann JI, Swan AV. Effects on coronary artery disease of lipid-lowering diet, or diet plus cholestyramine, in the St Thomas' Atherosclerosis Regression Study (STARS). Lancet. 1992;339:563–9. [DOI] [PubMed] [Google Scholar]
- 40. Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, Elwood PC, Deadman NM. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989;2:757–61. [DOI] [PubMed] [Google Scholar]
- 41. Houtsmuller AJ, van Hal-Ferwerda J, Zahn KJ, Henkes HE. Favorable influences of linoleic acid on the progression of diabetic micro- and macroangiopathy in adult onset diabetes mellitus. Prog Lipid Res. 1981;20:377–86. [DOI] [PubMed] [Google Scholar]
- 42. Rose GA, Thomson WB, Williams RT. Corn oil in treatment of ischaemic heart disease. BMJ. 1965;1:1531–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Frantz ID Jr, Dawson EA, Ashman PL, Gatewood LC, Bartsch GE, Kuba K, Brewer ER. Test of effect of lipid lowering by diet on cardiovascular risk: the Minnesota coronary survey. Arteriosclerosis. 1989;9(1):129–35. [DOI] [PubMed] [Google Scholar]
- 44. Ramsden CE, Zamora D, Leelarthaepin B, Majchrzak-Hong SF, Faurot KR, Suchindran CM, Ringel A, Davis JM, Hibbeln JR. Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis. BMJ. 2013;346:e8707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Willett WC. Nutritional epidemiology. 3rd ed New York (NY): Oxford University Press, 2013: pp. 1–16., 317–9. [Google Scholar]