In the United States, disparities in access to cancer screening, treatment, survivorship care, and survival have been well documented by patient race and/or ethnicity, socioeconomic status, and geographic region (1,2). Having health insurance coverage is one of the strongest predictors of patient access to high-quality care across the cancer control continuum, earlier stage diagnosis, and better survival (1,2). Because insurance coverage and benefit design are modifiable, they have been a major focus of health policy efforts to reduce disparities and improve population health. To date, most research evaluating the health effects of insurance coverage has measured coverage at only a single point in time. Little is known about health effects of insurance coverage disruptions, which are especially common in the poor and those with Medicaid coverage (3), the state-based health insurance programs for some low-income populations. Disruptions in insurance coverage may interfere with access to high-quality cancer care and adversely affect patient outcomes.
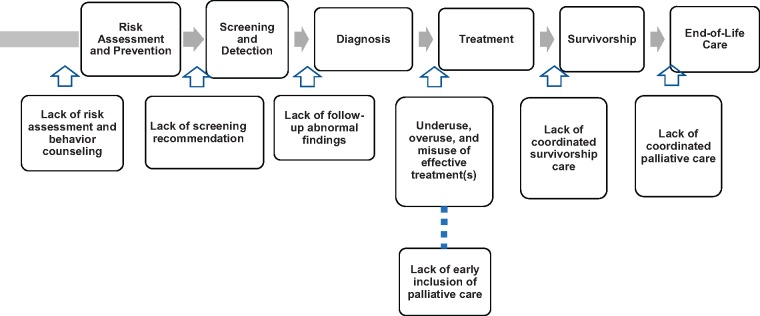
In this issue of the Journal, Keegan and colleagues used California Cancer Registry data linked to California Medicaid enrollment to evaluate the effects of Medicaid coverage continuity on stage at diagnosis for nine cancer sites in an important and relatively understudied population of cancer patients: those diagnosed as adolescents and young adults (AYAs) (4). This study adds to our understanding of the heterogeneity of Medicaid coverage and the importance of coverage continuity for cancer patients. The authors found that among newly diagnosed AYA cancer patients with Medicaid coverage from 2005 to 2014, nearly 50% either gained Medicaid coverage only at diagnosis or were discontinuously enrolled. The remaining 50% of patients with Medicaid coverage were continuously enrolled prior to and after cancer diagnosis. These distinctions in Medicaid coverage continuity were associated with substantial differences in late- stage disease at diagnosis. Compared with the privately insured, those enrolled in Medicaid only at cancer diagnosis were 2.2–2.5 times more likely to be diagnosed with late-stage disease; those discontinuously enrolled were 1.7–1.9 times more likely; and those continuously enrolled were 1.4–1.5 times more likely to be diagnosed with late-stage disease. Findings likely reflect greater problems with access to a usual source of care, prevention, screening, and symptom evaluation prior to cancer diagnosis among previously uninsured AYAs and those with disruptions in Medicaid coverage. Studies of older adult populations found that Medicaid coverage disruptions around cancer diagnosis were associated with later stage, lower rates of treatment, and poorer short-term survival (5,6). Taken together, these findings suggest that measurement of Medicaid coverage at a single point in time may underestimate its benefits in improving access to care for cancer patients. Evaluating the effects of Medicaid coverage disruptions on health care throughout the cancer control continuum will be important for future research (Figure 1).
Figure 1.
Medicaid insurance coverage disruptions and potential breakdowns in health care delivery across the cancer control continuum. Displays the cancer control continuum, including risk assessment and prevention, screening and detection, diagnosis, treatment, survivorship, and end-of-life care. Potential breakdowns are shown throughout the cancer control continuum that may be affected by Medicaid insurance coverage disruptions, from lack of risk assessment and behavior counseling to lack of screening recommendations, lack of follow-up of abnormal findings, underuse, overuse, and misuse of effective treatments, lack of coordinated survivorship care, and lack of coordinated palliative care. Adapted with permission from Yabroff et al. 2019 (18).
As noted by the authors, AYAs have the highest levels of uninsurance in the United States. The Affordable Care Act (ACA) enacted in 2010 contained multiple provisions to address the availability of insurance coverage, including incentives for states to expand Medicaid eligibility to 138% of the federal poverty level for low-income adults with and without children. As of November 2018, 36 states and the District of Columbia have adopted Medicaid expansion under the ACA (7). In the states that did not expand Medicaid eligibility, thresholds for Medicaid coverage are as low as 18% of the federal poverty level, equivalent to an annual income of $3740 for a family of three in 2017 (7). In many nonexpansion states, single adults are not eligible for Medicaid coverage, regardless of their income.
Accumulating evidence shows that cancer patients and survivors in Medicaid expansion states are more likely to be insured (8–11), have better access to care, and be diagnosed at an earlier stage than those in nonexpansion states (10,12). In addition, disparities in insurance coverage for newly diagnosed patients by race and/or ethnicity, rurality, and poverty either diminished or were eliminated only in Medicaid expansion states (8,12). Medicaid expansions might reduce the prevalence of Medicaid coverage disruptions by improving program infrastructure and eligibility recertification processes and minimizing the effects of income fluctuations on eligibility for low-income beneficiaries. Understanding mechanisms of these effects on disparities in cancer care and outcomes for AYA patients will be important for future research, especially with the recent emergence of work requirements for some state Medicaid programs, which might increase the risk of coverage disruptions.
The data for this study were from a single state and findings may not be generalizable to other states. Medicaid programs differ substantially across states in key aspects other than income eligibility thresholds, including the breadth and depth of covered services, requirements for patient copayments, frequency of eligibility recertification, levels of provider reimbursement, and differences in managed care plans. These factors likely play an important role in access to high-quality cancer care and better patient outcomes; however, linkages between population-based registries and Medicaid are not available for all states. Improving data infrastructure can stimulate research to identify modifiable Medicaid policies associated with reducing disparities and improving patient outcomes.
The ACA contained other provisions that can benefit AYA cancer patients, including introduction of the Marketplace, which allows individuals to enroll in private plans, and elimination of preexisting condition exclusions and of lifetime and annual coverage limits. The Dependent Coverage Expansion (DCE) allowed young adults to remain on parents’ private coverage up to age 26 years, which could minimize disruptions for some AYAs. The DCE is associated with improved access to preventive services and earlier stage at diagnosis in young adults aged 19–25 years compared with those aged 26–34 years (13–16). The importance of having a usual source of care, provider continuity, and stable private insurance coverage has been documented in other settings. Keegan et al. (4) did not evaluate the DCE in this study, and registry linkages for evaluating the effects of disruptions in private coverage may not be currently available. Nonetheless, understanding the effects of private coverage continuity will be important for future research, especially given the recent emergence of short-term plans (17), which are not required to cover preexisting conditions and frequently do not cover prescription drugs.
This novel study by Keegan and colleagues (4) highlights Medicaid coverage disruptions as a potentially modifiable lever for improving care for AYAs. It also highlights the need for ongoing improvements in health-care data infrastructure and research to identify additional levers to help improve access to high-quality care and reduce disparities for cancer patients in the United States.
Notes
Affiliation of authors: Surveillance and Health Services Research, American Cancer Society, Atlanta, GA (KRY, XH, LN, AJ).
Authors do not have any conflicts of interest.
References
- 1. Institute of Medicine. The Unequal Burden of Cancer. Washington, DC: National Academies of Science; 1999. [Google Scholar]
- 2. Institute of Medicine. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 3. Short PF, Graefe DR, Swartz K, Uberoi N.. New estimates of gaps and transitions in health insurance. Med Care Res Rev. 2012;696:721–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Keegan THM, Parsons HM, Chen Y, et al. Impact of health insurance on stage at cancer diagnosis among adolescents and young adults. J Natl Cancer Inst .2019;111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dawes AJ, Louie R, Nguyen DK, et al. The impact of continuous Medicaid enrollment on diagnosis, treatment, and survival in six surgical cancers. Health Serv Res. 2014;496:1787–1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bradley CJ, Gardiner J, Given CW, Roberts C.. Cancer, Medicaid enrollment, and survival disparities. Cancer. 2005;1038:1712–1718. [DOI] [PubMed] [Google Scholar]
- 7. Henry J Kaiser Family Foundation. Medicaid income eligibility limits for adults as a percent of the federal poverty level. https://www.kff.org/health-reform/state-indicator/medicaid-income-eligibility-limits-for-adults-as-a-percent-of-the-federal-poverty-level/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. 2019. Accessed April 5, 2019.
- 8. Jemal A, Lin CC, Davidoff AJ, Han X.. Changes in insurance coverage and stage at diagnosis among nonelderly patients with cancer after the Affordable Care Act. J Clin Oncol. 2017;3535:3906–3915. [DOI] [PubMed] [Google Scholar]
- 9. Davidoff AJ, Guy GP Jr, Hu X, et al. Changes in health insurance coverage associated with the Affordable Care Act among adults with and without a cancer history: population-based national estimates. Med Care. 2018;563:220–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Soni A, Simon K, Cawley J, Sabik L.. Effect of Medicaid expansions of 2014 on overall and early-stage cancer diagnoses. Am J Public Health. 2018;1082:216–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Soni A, Sabik LM, Simon K, Sommers BD.. Changes in insurance coverage among cancer patients under the Affordable Care Act. JAMA Oncol. 2018;41:122–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Han X, Yabroff KR, Ward E, Brawley OW, Jemal A.. Comparison of insurance status and diagnosis stage among patients with newly diagnosed cancer before vs after implementation of the patient protection and Affordable Care Act. JAMA Oncol. 2018;4(12):1713–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Han X, Yabroff KR, Robbins AS, Zheng Z, Jemal A.. Dependent coverage and use of preventive care under the Affordable Care Act. N Engl J Med. 2014;37124:2341–2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Robbins AS, Han X, Ward EM, Simard EP, Zheng Z, Jemal A.. Association between the Affordable Care Act dependent coverage expansion and cervical cancer stage and treatment in young women. JAMA. 2015;31420:2189–2191. [DOI] [PubMed] [Google Scholar]
- 15. Wallace J, Sommers BD.. Effect of dependent coverage expansion of the Affordable Care Act on health and access to care for young adults. JAMA Pediatr. 2015;1695:495–497. [DOI] [PubMed] [Google Scholar]
- 16. Han X, Zang Xiong K, Kramer MR, Jemal A.. The Affordable Care Act and cancer stage at diagnosis among young adults. J Natl Cancer Inst. 2016;1089:djw058. [DOI] [PubMed] [Google Scholar]
- 17. Pollitz K, Long M, Semanskee A, Kamal R.. Understanding Short-Term Limited Duration Health Insurance 2019. https://www.kff.org/health-reform/issue-brief/understanding-short-term-limited-duration-health-insurance/ Accessed April 5, 2019.
- 18. Yabroff KR, Gansler T, Wender RC, Cullen KJ, Brawley OW.. Minimizing the burden of cancer in the United States: goals for a high-performing health care system [published online ahead of print February 20, 2019]. CA Cancer J Clin. 2019. doi:10.3322/caac.21556. [DOI] [PubMed] [Google Scholar]